Abstract
In the treatment of anterior shoulder instability, there are various conditions in which a sling effect is needed to enhance anterior stability. The traditional Latarjet procedure provides a sling effect but destroys the coracoacromial arch, which may result in superior instability. To preserve the coracoacromial arch and create a sling to enhance the anterior-inferior side of the shoulder, we introduce an arthroscopic technique to transfer the long head of the biceps (LHB) brachii. Indications of LHB transfer are patients younger than 45 years of age who participate in competitive sports, require forceful external rotation and abduction movement of the shoulder, and/or have capsule-ligament insufficiency, as well as patients 45 years o or older who have combined SLAP lesions (type II or IV). The main steps of this procedure include detaching the LHB, retrieving and braiding the LHB, creating a glenoid tunnel, placing a guide suture through the subscapularis and glenoid tunnel, passing the LHB through the subscapularis and into the glenoid tunnel, and suspension fixation of the LHB.
The Latarjet procedure, namely, transfer of the coracoid process along with the conjoined tendon, is a useful technique to treat anterior shoulder instability1, 2 and is especially indicated in patients with bony defects.3, 4 One of the main supposed mechanisms of the Bristow-Latarjet procedure to restore shoulder stability is the sling effect provided by the transferred conjoined tendon.4 However, during the classic or modified Latarjet procedure, the coracoacromial (CA) arch is destroyed,3, 5 which may result in superior instability,6, 7 especially in patients with severe rotator cuff tears.8, 9 In order to create a sling at the anterior-inferior side of the glenohumeral joint without disturbing the CA arch, we introduce a technique to transfer the long head of the biceps (LHB) brachii from the superior side of the glenoid to the anterior-inferior side.
The main indication of this technique is patients with anterior shoulder instability who require a sling effect to augment the shoulder at the anterior-inferior side. Detailed indications include patients younger than 45 years of age who participate in competitive sports, require forceful external rotation and abduction movement of the shoulder, and/or have capsule-ligament insufficiency, such as general laxity or capsule defect. Another special indication is patients 45 years or older who have combined SLAP lesions (type II or IV; Table 1). This technique can be used alone when specially indicated but is usually combined with other reconstructive procedures, such as Bankart repair, remplissage, or glenoid bone grafting. The contraindications of this procedure are over 50% rupture of the LHB and patients who do not require a sling effect to augment the shoulder.
Table 1.
Indications and Contraindications of Long Head of the Biceps (LHB) Transfer
| Indications | Younger than 45 years of age Participating in competitive sports Requiring forceful external rotation and abduction movement of the shoulder Having capsule-ligament insufficiency, such as general laxity or capsule defect 45 years or older having combined SLAP lesion (type II or IV) |
| Contraindications | Over 50% rupture of the LHB Not requiring a sling effect to augment the shoulder |
Surgical Technique
Patient Position, Portal Creation, and Arthroscopic Examination
General anesthesia and brachial plexus anesthesia are administered. The patient is placed in the lateral decubitus position with the arm in 30° abduction and with 10 pounds of traction. Routine portals for anterior shoulder dislocation, namely, posterior, anterior, and anterosuperior, are fashioned. Routine arthroscopic examination is performed to detect all pathologies (Table 2).
Table 2.
Step-by-Step Surgical Procedure
| 1. Hold the LHB in the joint with a suture, and then detach the LHB from the superior labrum. |
| 2. Pull the LHB out of the joint and bicipital groove to the anterior subdeltoid space and then out of the anterodistal portal. |
| 3. Braid the LHB with 3 high-strength sutures. |
| 4. Create a glenoid tunnel. |
| 5. Pass a guide suture through the glenoid tunnel from posterior to anterior and then through the subscapularis to the anterior side. |
| 6. Find the guide suture at the anterior side of the subscapularis and pull it laterally to near the bicipital groove. |
| 7. Put the braiding sutures through the loop of the guide suture and pull the braiding sutures through the subscapularis and glenoid tunnel and then out of the posterior portal using the guide suture. |
| 8. Pull the LHB through the subscapularis and into the glenoid tunnel. |
| 9. Tie the braiding sutures onto a miniplate placed over the posterior orifice of the glenoid tunnel. |
LHB, long head of the biceps.
Detaching the LHB
Under observation from the posterior portal, a folded no. 2 PE suture is passed through the proximal part of the biceps tendon with a suture passer placed through the anterosuperior portal. By passing the free ends of the suture into the folded end, the biceps tendon is held by the suture. Then the biceps tendon is cut at its conjunction with the superior labrum, proximal to the holding suture.
Extracting and Braiding the LHB
The arthroscope is placed in the anterior subdeltoid space via the anterosuperior portal. The anterolateral portal, which is located at the level of the coracoid process and approximately 2 cm lateral to the anterior midline of the arm, is fashioned under arthroscopic observation. Via the anterolateral portal, an obturator is placed to detect the biceps tendon and superior edge of the pectoralis major. The biceps tendon distal to the bicipital groove and proximal to the pectoralis major is exposed.
Then the anterodistal portal, which is located at the level of the proximal edge of the pectoralis major and just over the biceps tendon, is created. With instruments placed through the anterodistal portal, the biceps tendon is retrieved out of the joint and bicipital groove to the anterior subdeltoid space. By pulling the holding suture, the proximal end of the biceps tendon is pulled out of the anterodistal portal (Fig 1).
Fig 1.
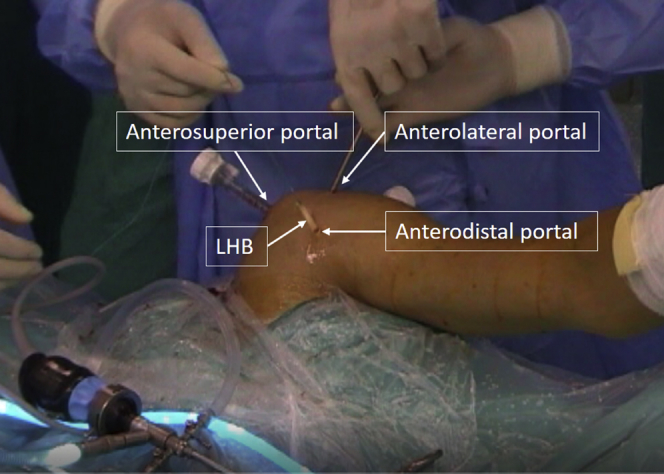
Outside view of left shoulder to show the anterosuperior, anterolateral, and anterodistal portals. The patient is placed in the lateral decubitus position. The long head of the biceps is extracted from the anterodistal portal.
Three no. 2 high-strength sutures (Ultrabraid; Smith-Nephew, Andover, MA) are used to braid the biceps tendon in a whipstitch style. The length of the tendon segment to be braided is 3 to 4 cm. Then the width of the braided tendon segment, which is usually 6 to 8 mm, is measured.
Creating a Glenoid Tunnel
The arthroscope is placed in the joint via the anterosuperior portal. Under observation, a customized glenoid guide is placed in the joint through the posterior portal. A 2.5-mm K-wire is drilled into the glenoid from posterior to anterior, 7 mm below the surface. The posterior entry point of the K-wire is located at the 2 to 4 o'clock position (left shoulder) without strict confinement, while the anterior exit point is located at the 4 to 5 o'clock position (left shoulder). The K-wire is overdrilled using a 4.5- or 5-mm cannulated drill to create a primary glenoid tunnel.
A 3.5 mm wide retrograde drill (FlipCutter; Arthrex, Naples, FL), with the same size as the biceps tendon when it is flipped, is placed through the glenoid tunnel from posterior to anterior in a nonflipped condition. Then the anterior part of the glenoid tunnel is enlarged to the expected size. The length of the enlarged part of the tunnel depends on the whole length, ensuring that a 5 mm long unenlarged part is left at the posterior side. Because the width of the glenoid is usually 25 to 30 mm, the length of LHB to be placed in the glenoid tunnel is usually 20 to 25 mm. When there is glenoid defect, the length of LHB in the glenoid tunnel is reduced accordingly (Fig 2).
Fig 2.
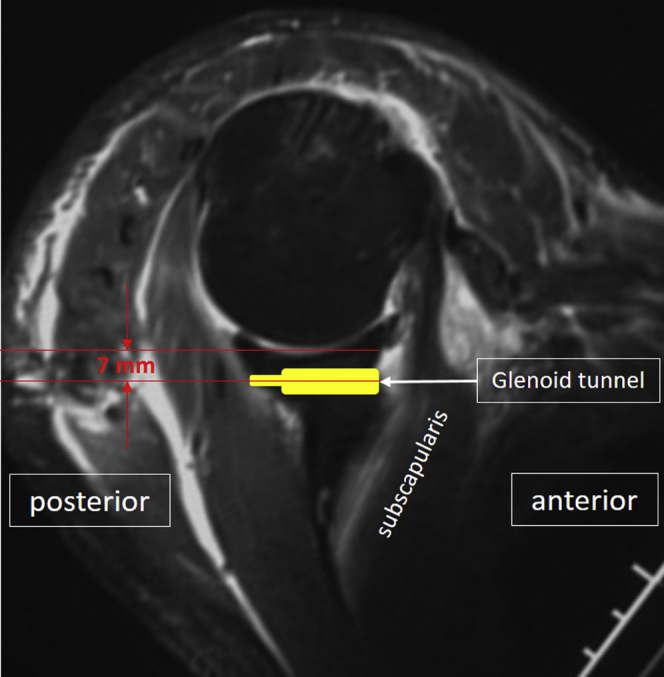
Illustration of left shoulder viewed from the superior side to show the shape and location of the glenoid tunnel. The center of the glenoid tunnel is located 7 mm below the glenoid surface. The size of the anterior part of the glenoid tunnel is equal to that of the long head of the biceps; the size of the posterior part of the glenoid tunnel is 4.5 or 5 mm.
Passing a Guide Suture Through the Glenoid Tunnel and Subscapularis
With the arthroscope placed in the joint through the anterosuperior portal for observation, a folded no. 2 PE suture, which will be used as a guide suture, is passed through the glenoid tunnel from posterior to anterior using a suture retriever, with the folded end of the suture at the anterior side. Using another suture retriever placed through the anterior portal, the guide suture is pulled into the joint space. Then the suture retriever in the glenoid tunnel is removed and passed through the posterior portal into the joint to hold the guide suture again. Then it is pushed anteriorly along the glenoid surface through the subscapularis at the 4:30 position along with the guide suture (Fig 3).
Fig 3.
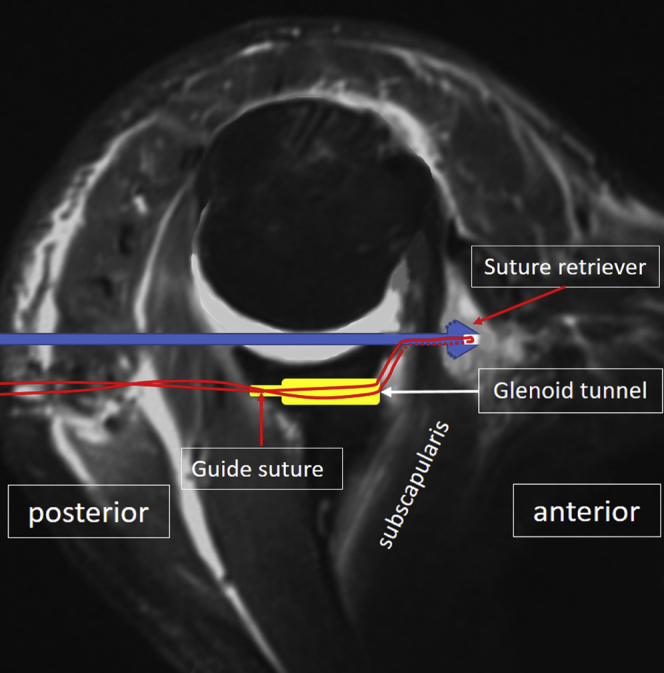
Illustration of left shoulder viewed from the superior side to show the passing of the guide suture through the glenoid tunnel and the subscapularis muscle. The guide suture is first passed through the glenoid tunnel to the anterior side of the glenoid and then passed through the subscapularis muscle with a suture retriever placed through the joint space.
Finding the Guide Suture at the Anterior Side of the Subscapularis
The arthroscope is placed through the anterolateral portal and pushed along the anterior side of the subscapularis in an inferior-medial direction. An obturator or switching stick is placed through the anterosuperior portal and used to separate the fibrous tissue in front of the scope until the suture retriever, which is passed through the joint and subscapularis, is touched and then exposed. Another suture retriever is used to replace the obturator or switching stick to hold the guide suture, which is found anterior to the subscapularis (Fig 4). The guide suture is then pulled to the anterosuperior portal.
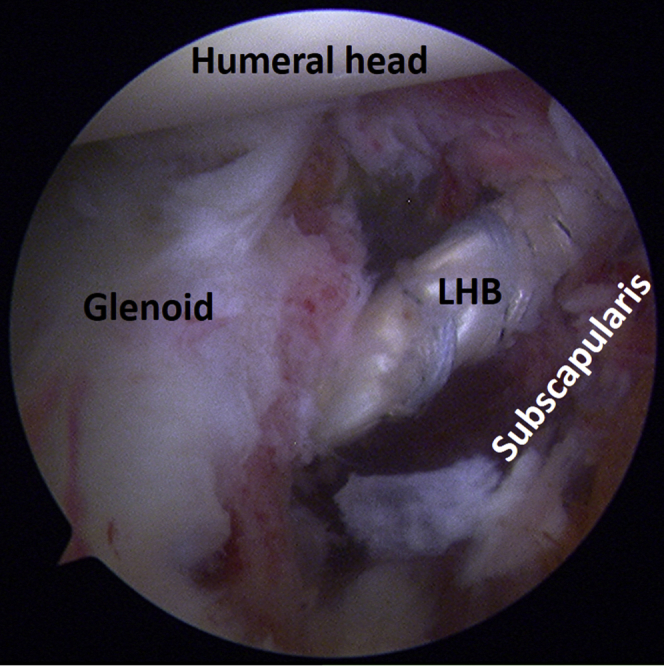
Fig 4.
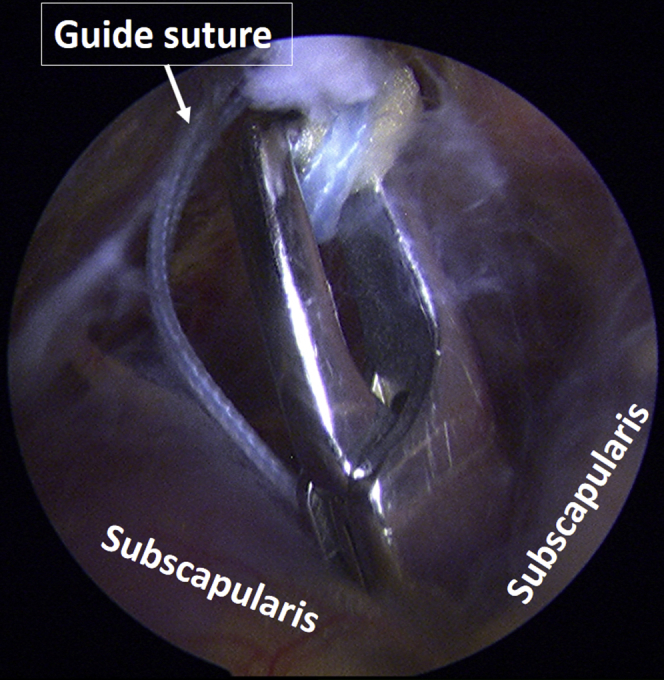
Finding the suture retriever and the guide suture at the anterior side of the subscapularis muscle. Arthroscopic view of left shoulder through anterolateral portal in the lateral decubitus position.
Passing the Braiding Suture Through the Subscapularis and Glenoid Tunnel
The braiding suture ends from the LHB are pulled through a cannula, which is pushed into the anterior subdeltoid space along the braiding sutures through the anterodistal portal. A suture retriever is placed through this cannula to pull the guide suture out of the anterodistal portal. Then all the suture ends are passed through the loop of the guide suture. By pulling the guide suture back, the suture ends from the LHB are pulled through the subscapularis and glenoid tunnel and out of the posterior portal.
Passing the LHB Through the Subscapularis and Into the Glenoid Tunnel
The arthroscope is placed in the joint through the anterosuperior portal. The anterior side of the glenoid is exposed to locate the braiding suture from the LHB. Then, under observation, the LHB is pulled through the subscapularis into the glenoid tunnel (Fig 5).
Fig 5.
Pulling the long head of the biceps into the glenoid tunnel. Arthroscopic view of left shoulder through anterosuperior portal in the lateral decubitus position.
Fixation of the LHB
The posterior portal incision is enlarged to 2 to 3 cm in length to allow insertion of the index finger of the operator. The soft tissue around the braiding suture is separated with the finger until the posterior orifice of the glenoid tunnel is touched and free of soft tissue. Then the 2 ends from each suture are passed through the middle 2 holes of a miniplate (EndoButton, Smith-Nephew) separately.
The miniplate is pushed along the sutures to the posterior orifice of the glenoid tunnel. All sutures are tied to their counter limbs on the miniplate. In this way, the LHB is fixed into the glenoid tunnel by suspension fixation on the miniplate over the posterior orifice (Figs 6 and 7).
Fig 6.
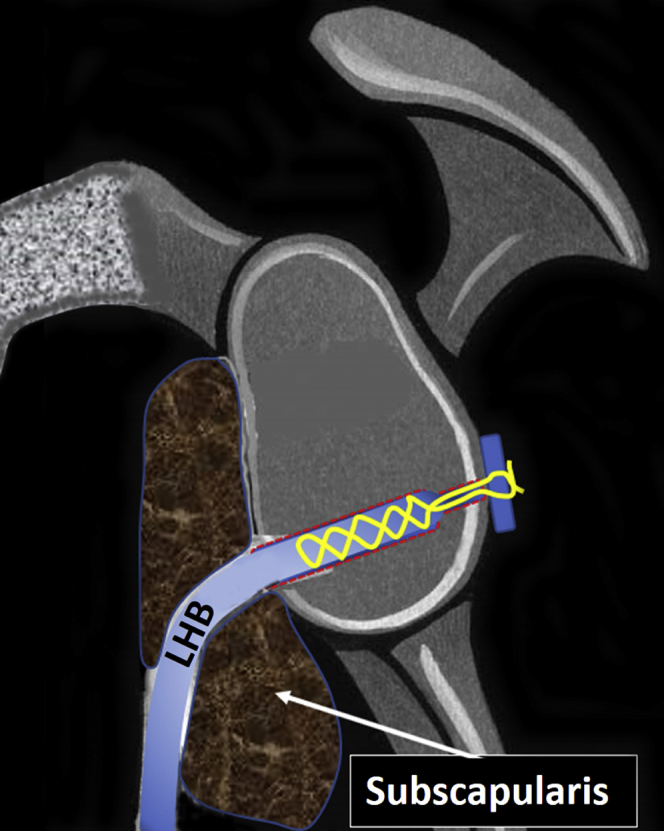
Illustration of left shoulder viewed from lateral side. Long head of the biceps fixation onto a miniplate placed over the posterior orifice of the glenoid tunnel.
Fig 7.

Posterior view of the left shoulder. Postoperative computed tomography showing the location of the miniplate for suspension fixation of the long head of the biceps.
Discussion
Anterior shoulder instability is a common clinical condition. For complicated anterior shoulder instability, the Latarjet procedure is an effective way to restore stability.10, 11, 12 However, during this procedure, the CA ligament is transected or detached, effectively destroying the CA arch. The role of the integrity of the CA arch in superior shoulder stability has been illustrated in several studies, with the finding that CA ligament resection or performing the Latarjet procedure resulted in increased superior shoulder translation in various joint configurations and loading conditions, regardless of whether or not the rotator cuff was intact.6, 7, 9, 13, 14, 15 Preservation of the CA arch during the Latarjet procedure is an ideal, but impossible, option.
The purpose of coracoid process transfer in the Latarjet procedure is to address the glenoid defect. A triple-block effect, which includes enlargement of the glenoid surface using the transferred coracoid process, repair of the capsule to CA ligament stump, and a sling effect of the conjoined tendon, is considered to be the functional mechanism to restore shoulder stability.4 There are several methods to correct the glenoid defect and create a sling simultaneously, without destroying or disturbing the CA arch. Among these methods, a modified Latarjet procedure along with CA arch reconstruction has been reported,16 while LHB transfer combined with glenoid bone grafting is another reasonable option.17
Studies have shown that several factors, including younger age, higher sports performance level, sports type requiring forceful external rotation and abduction movement of the shoulder, and structural defect of soft tissue and bone, predispose to a higher rate of failure.18 Theoretically, a sling effect is still required when risk factors other than severe glenoid defect exist.
A recent study showed that the sling effect depends on the loading of the transferred conjoined tendon.19 In cases of shoulder instability without severe glenoid defect, a bone block is unnecessary to restore shoulder stability when a sling effect exists.20 To create a sling effect alone, the Bristow procedure may be indicated21 because in this procedure only the tip of the coracoid process is removed along with the conjoined tendon. However, even in the Bristow procedure, caution should be taken regarding the length of the coracoid process to be removed. One study showed that the mean distance from the coracoid tip to the anterior and posterior CA ligament was 7.8 and 25.7 mm, respectively,22 and that, theoretically, a 17 mm long coracoid process removal destroys over 50% of the CA ligament. In one study that explored the effect of conjoined tendon transfer without coracoid bone fragment, Thomas et al. found that the same stability effect can be obtained compared with the Bristow procedure.23 This indicates the stability effect of a soft-tissue sling only.
To create a sling effect alone without intent to transfer any bony tissue, transferring the LHB instead of the conjoined tendon is a reasonable choice. A previous study indicated that the originally inserted LHB contributes to passive shoulder stability in all directions and in various degrees of arm abduction.24, 25, 26, 27 However, a biomechanical study is still needed to detect whether the LHB could enhance anterior-inferior stability when transferred to this position, although, theoretically, additional stabilizing structures at one site means additional stability. Compared with the conjoined tendon, the LHB is relatively thin (6-8 mm wide). Whether the same sling effect as conjoined tendon transfer can be obtained through LHB transfer still needs to be explored.
Furthermore, anterior shoulder instability is always combined with SLAP lesion.28, 29 LHB transfer in this condition may address the SLAP lesion and enhance anterior-inferior stability of the shoulder simultaneously.
Compared with conjoined tendon transfer, LHB transfer is simpler and less dangerous. The learning curve of the arthroscopic Bristow-Latarjet procedure is relatively long,30, 31 and many surgeons feel reluctant to split and manipulate through the subscapularis with the axillary nerve located nearby. In LHB transfer, a glenoid tunnel is created in a retrograde manner without risking the axillary nerve. The only dangerous maneuver is blind penetration of the subscapularis using the suture retriever, and with control of the direction and position of penetration, such danger can be minimized. The only maneuver at the anterior side of the subscapularis is location and retrieval of the guide suture, and this can be accomplished easily through the anterosuperior and anterolateral portals, without the far medial portal, which is required in the arthroscopic Latarjet procedure.32
The pearls and pitfalls of this LHB transfer procedure are illustrated in Table 3. The most important points in performing this procedure include creation of a suitable glenoid tunnel, appropriate penetration of the subscapularis, and reliable suspension fixation of the transferred tendon.
Table 3.
Pearls and Pitfalls
| 1. Make sure the LHB is fully detached from the superior labrum and separated from the neighboring tissue, otherwise outpulling will be hindered. |
| 2. In the anterior subdeltoid space, locating the superior edge of the pectoralis major first will facilitate locating the LHB distal to the bicipital groove. |
| 3. Measure the width of the glenoid to calculate the tunnel length and ensure a 5 mm long unenlarged part is left at the posterior side. Whole-tunnel enlargement will make suspension fixation with a miniplate impossible. |
| 4. Pass the guide suture through the subscapularis using a suture retriever along the glenoid surface to prevent too medial penetration. |
| 5. The penetrating point of the subscapularis should be located at the 4:30 position. Too inferior penetration may endanger the axillary nerve. |
| 6. Using an instrument to detect the hard point at the anterior side of the subscapularis will facilitate locating the subscapularis-penetrating suture retriever. |
| 7. When tying the braiding sutures onto the miniplate over the posterior orifice of the glenoid tunnel, make sure to push the miniplate tightly against the glenoid bone. |
LHB, long head of the biceps.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Funded by National Natural Science Foundation of China, grant nos. 31400800 and 31370945.
Supplementary Data
This operation is performed on the left shoulder. A folded suture is passed through the proximal part of the biceps tendon to hold it. The biceps tendon is cut at its conjunction with the superior labrum. The arthroscope is placed in the anterior subdeltoid space via the anterosuperior portal. The biceps tendon distal to the bicipital groove and proximal to the pectoralis major is exposed with instruments placed in through the anterolateral portal. The biceps tendon is retrieved out of the joint and bicipital groove to the anterior subdeltoid space and is pulled out of the anterodistal portal. Three no. 2 high-strength sutures are used to braid the biceps tendon in a whipstitch style. The arthroscope is placed in the joint via the anterosuperior portal. Under observation, a customized glenoid guide is placed in the joint through the posterior portal. A transverse glenoid tunnel, which is located 7 mm below the glenoid surface, is created sequentially with a 2.5-mm K-wire, a 4.5- or 5-mm cannulated drill, and a 3.5-mm-wide retrograde drill. A folded no. 2 PE suture, which will be used as a guide suture, is passed through the glenoid tunnel from the posterior to anterior side and then pulled into the joint. A suture retriever is placed into the joint and then used to pass the guide suture anteriorly through the subscapularis. The arthroscope is placed through the anterolateral portal and pushed along the anterior side of the subscapularis in an inferior-medial direction. With instruments placed through the anterosuperior portal, the guide suture is found and pulled to the anterosuperior portal. The LHB and the guide suture are rerouted through the same cannula, which is placed in the anterodistal portal. Using the guide suture, the suture ends from the LHB are pulled through the subscapularis and glenoid tunnel and out of the posterior portal. The arthroscope is placed in the joint through the anterosuperior portal. Under observation, the LHB is pulled through the subscapularis into the glenoid tunnel. At the posterior side, the 2 ends from each suture are passed through the middle 2 holes of a miniplate separately. The miniplate is pushed along the sutures to the posterior orifice of the glenoid tunnel. All sutures are tied to their counter limbs on the miniplate. In this way, the LHB is fixed into the glenoid tunnel by suspension fixation on the miniplate over the posterior orifice.
References
- 1.Hovelius L., Vikerfors O., Olofsson A., Svensson O., Rahme H. Bristow-Latarjet and Bankart: a comparative study of shoulder stabilization in 185 shoulders during a seventeen-year follow-up. J Shoulder Elbow Surg. 2011;20:1095–1101. doi: 10.1016/j.jse.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Burkhart S.S., De Beer J.F., Barth J.R., Cresswell T., Roberts C., Richards D.P. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy. 2007;23:1033–1041. doi: 10.1016/j.arthro.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 3.Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954;49:994–997. [PubMed] [Google Scholar]
- 4.Young A.A., Maia R., Berhouet J., Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg. 2011;20:S61–S69. doi: 10.1016/j.jse.2010.07.022. (2 Suppl) [DOI] [PubMed] [Google Scholar]
- 5.de Beer J.F., Roberts C. Glenoid bone defects—open Latarjet with congruent arc modification. Orthop Clin North Am. 2010;41:407–415. doi: 10.1016/j.ocl.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 6.Lee T.Q., Black A.D., Tibone J.E., McMahon P.J. Release of the coracoacromial ligament can lead to glenohumeral laxity: a biomechanical study. J Shoulder Elbow Surg. 2001;10:68–72. doi: 10.1067/mse.2001.111138. [DOI] [PubMed] [Google Scholar]
- 7.Su W.R., Budoff J.E., Luo Z.P. The effect of coracoacromial ligament excision and acromioplasty on superior and anterosuperior glenohumeral stability. Arthroscopy. 2009;25:13–18. doi: 10.1016/j.arthro.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Wiley A.M. Superior humeral dislocation. A complication following decompression and debridement for rotator cuff tears. Clin Orthop Relat Res. 1991;263:135–141. [PubMed] [Google Scholar]
- 9.Hockman D.E., Lucas G.L., Roth C.A. Role of the coracoacromial ligament as restraint after shoulder hemiarthroplasty. Clin Orthop Relat Res. 2004;419:80–82. doi: 10.1097/00003086-200402000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Bessiere C., Trojani C., Pélégri C., Carles M., Boileau P. Coracoid bone block versus arthroscopic Bankart repair: a comparative paired study with 5-year follow-up. Orthop Traumatol Surg Res. 2013;99:123–130. doi: 10.1016/j.otsr.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 11.Mizuno N., Denard P.J., Raiss P., Melis B., Walch G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg. 2014;23:1691–1699. doi: 10.1016/j.jse.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 12.Dumont G.D., Fogerty S., Rosso C., Lafosse L. The arthroscopic latarjet procedure for anterior shoulder instability: 5-year minimum follow-up. Am J Sports Med. 2014;42:2560–2566. doi: 10.1177/0363546514544682. [DOI] [PubMed] [Google Scholar]
- 13.Wellmann M., Petersen W., Zantop T., Schanz S., Raschke M.J., Hurschler C. Effect of coracoacromial ligament resection on glenohumeral stability under active muscle loading in an in vitro model. Arthroscopy. 2008;24:1258–1264. doi: 10.1016/j.arthro.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 14.Denard P.J., Bahney T.J., Kirby S.B., Orfaly R.M. Contact pressure and glenohumeral translation following subacromial decompression: how much is enough? Orthopedics. 2010;33:805. doi: 10.3928/01477447-20100924-02. [DOI] [PubMed] [Google Scholar]
- 15.Degen R.M., Giles J.W., Boons H.W., Litchfield R.B., Johnson J.A., Athwal G.S. A biomechanical assessment of superior shoulder translation after reconstruction of anterior glenoid bone defects: the Latarjet procedure versus allograft reconstruction. Int J Shoulder Surg. 2013;7:7–13. doi: 10.4103/0973-6042.109879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aurich M., Hofmann G.O., Gras F. Reconstruction of the coracoacromial ligament during a modified Latarjet procedure: a case series. BMC Musculoskelet Disord. 2015;16:238. doi: 10.1186/s12891-015-0698-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao J., Huangfu X., Yang X., Xie G., Xu C. Arthroscopic glenoid bone grafting with nonrigid fixation for anterior shoulder instability: 52 patients with 2- to 5-year follow-up. Am J Sports Med. 2014;42:831–839. doi: 10.1177/0363546513519227. [DOI] [PubMed] [Google Scholar]
- 18.Balg F., Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilization. J Bone Joint Surg Br. 2007;89:1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 19.Dines J.S., Dodson C.C., McGarry M.H., Oh J.H., Altchek D.W., Lee T.Q. Contribution of osseous and muscular stabilizing effects with the Latarjet procedure for anterior instability without glenoid bone loss. J Shoulder Elbow Surg. 2013;22:1689–1694. doi: 10.1016/j.jse.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 20.Kephart C.J., Abdulian M.H., McGarry M.H., Tibone J.E., Lee T.Q. Biomechanical analysis of the modified Bristow procedure for anterior shoulder instability: is the bone block necessary? J Shoulder Elbow Surg. 2014;23:1792–1799. doi: 10.1016/j.jse.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 21.Helfet A.J. Coracoid transplantation for recurring dislocation of the shoulder. J Bone Joint Surg Br. 1958;40:198–202. doi: 10.1302/0301-620X.40B2.198. [DOI] [PubMed] [Google Scholar]
- 22.Dolan C.M., Hariri S., Hart N.D., McAdams T.R. An anatomic study of the coracoid process as it relates to bone transfer procedures. J Shoulder Elbow Surg. 2011;20:497–501. doi: 10.1016/j.jse.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 23.Thomas P.R., Parks B.G., Douoguih W.A. Anterior shoulder instability with Bristow procedure versus conjoined tendon transfer alone in a simple soft-tissue model. Arthroscopy. 2010;26:1189–1194. doi: 10.1016/j.arthro.2010.01.033. [DOI] [PubMed] [Google Scholar]
- 24.Alexander S., Southgate D.F., Bull A.M., Wallace A.L. The role of negative intraarticular pressure and the long head of biceps tendon on passive stability of the glenohumeral joint. J Shoulder Elbow Surg. 2013;22:94–101. doi: 10.1016/j.jse.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 25.Rodosky M.W., Harner C.D., Fu F.H. The role of the long head of the biceps muscle and superior glenoid labrum in anterior stability of the shoulder. Am J Sports Med. 1994;22:121–130. doi: 10.1177/036354659402200119. [DOI] [PubMed] [Google Scholar]
- 26.Warner J.J., McMahon P.J. The role of the long head of the biceps brachii in superior stability of the glenohumeral joint. J Bone Joint Surg Am. 1995;77:366–372. doi: 10.2106/00004623-199503000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Pagnani M.J., Deng X.H., Warren R.F., Torzilli P.A., O'Brien S.J. Role of the long head of the biceps brachii in glenohumeral stability: a biomechanical study in cadavera. J Shoulder Elbow Surg. 1996;5:255–262. doi: 10.1016/s1058-2746(96)80051-6. [DOI] [PubMed] [Google Scholar]
- 28.Durban C.M., Kim J.K., Kim S.H., Oh J.H. Anterior shoulder instability with concomitant superior labrum from anterior to posterior (SLAP) lesion compared to anterior instability without SLAP lesion. Clin Orthop Surg. 2016;8:168–174. doi: 10.4055/cios.2016.8.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gaudelli C., Hébert-Davies J., Balg F. The impact of superior labral anterior to posterior lesions on functional status in shoulder instability: a multicenter cohort study. Orthop J Sports Med. 2014;2 doi: 10.1177/2325967114554195. 2325967114554195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cunningham G., Benchouk S., Kherad O., Lädermann A. Comparison of arthroscopic and open Latarjet with a learning curve analysis. Knee Surg Sports Traumatol Arthrosc. 2016;24:540–545. doi: 10.1007/s00167-015-3910-3. [DOI] [PubMed] [Google Scholar]
- 31.Castricini R., De Benedetto M., Orlando N., Rocchi M., Zini R., Pirani P. Arthroscopic Latarjet procedure: analysis of the learning curve. Musculoskelet Surg. 2013;97(Suppl 1):93–98. doi: 10.1007/s12306-013-0262-3. [DOI] [PubMed] [Google Scholar]
- 32.Lafosse L., Boyle S. Arthroscopic Latarjet procedure. J Shoulder Elbow Surg. 2010;19:2–12. doi: 10.1016/j.jse.2009.12.010. (2 Suppl) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This operation is performed on the left shoulder. A folded suture is passed through the proximal part of the biceps tendon to hold it. The biceps tendon is cut at its conjunction with the superior labrum. The arthroscope is placed in the anterior subdeltoid space via the anterosuperior portal. The biceps tendon distal to the bicipital groove and proximal to the pectoralis major is exposed with instruments placed in through the anterolateral portal. The biceps tendon is retrieved out of the joint and bicipital groove to the anterior subdeltoid space and is pulled out of the anterodistal portal. Three no. 2 high-strength sutures are used to braid the biceps tendon in a whipstitch style. The arthroscope is placed in the joint via the anterosuperior portal. Under observation, a customized glenoid guide is placed in the joint through the posterior portal. A transverse glenoid tunnel, which is located 7 mm below the glenoid surface, is created sequentially with a 2.5-mm K-wire, a 4.5- or 5-mm cannulated drill, and a 3.5-mm-wide retrograde drill. A folded no. 2 PE suture, which will be used as a guide suture, is passed through the glenoid tunnel from the posterior to anterior side and then pulled into the joint. A suture retriever is placed into the joint and then used to pass the guide suture anteriorly through the subscapularis. The arthroscope is placed through the anterolateral portal and pushed along the anterior side of the subscapularis in an inferior-medial direction. With instruments placed through the anterosuperior portal, the guide suture is found and pulled to the anterosuperior portal. The LHB and the guide suture are rerouted through the same cannula, which is placed in the anterodistal portal. Using the guide suture, the suture ends from the LHB are pulled through the subscapularis and glenoid tunnel and out of the posterior portal. The arthroscope is placed in the joint through the anterosuperior portal. Under observation, the LHB is pulled through the subscapularis into the glenoid tunnel. At the posterior side, the 2 ends from each suture are passed through the middle 2 holes of a miniplate separately. The miniplate is pushed along the sutures to the posterior orifice of the glenoid tunnel. All sutures are tied to their counter limbs on the miniplate. In this way, the LHB is fixed into the glenoid tunnel by suspension fixation on the miniplate over the posterior orifice.


