Abstract
Background
Post traumatic stress disorder (PTSD) symptoms are related to a number of adverse consequences such as substance use and general medical conditions. The present longitudinal study seeks to find the longitudinal patterns of cannabis use as precursors of PTSD symptoms. Such information will serve as a guide for intervention programs for PTSD.
Methods
Growth mixture modeling was conducted to identify the cannabis use trajectory groups using a community sample of 674 participants (53% African Americans, 47% Hispanics of Puerto Rican decent; 60% females) from the Harlem Longitudinal Development Study. Logistic regression analyses were performed to examine the association between earlier trajectories of cannabis use (age 14 to 36) and later symptoms of PTSD (at age 36) for the full model including the entire sample (N=674) as well as the reduced model including only participants who had experienced a traumatic event (n=205).
Results
Five trajectory groups of cannabis use were obtained. The chronic use group (full model: Adjusted odds ratio, AOR=4.68, p<.01; reduced model: AOR=4.27, p<.05), the late quitting group (full model: AOR=6.18, p<.01; reduced model: AOR=6.67, p<.01), and the moderate use group (full model: AOR=3.97, p<.01; reduced model: AOR=3.32, p<.05) were all associated with an increased likelihood of having PTSD symptoms at age 36 compared with the no use group.
Conclusions
The findings provide information that PTSD symptoms in the mid 30s can possibly be reduced by decreasing membership in the chronic cannabis use trajectory group, the late quitting trajectory group, and the moderate cannabis use trajectory group.
Keywords: Post Traumatic Stress Disorder Symptoms, Cannabis Use, Trajectory Analysis, Longitudinal Study
Introduction
Numerous studies have shown the impact of the symptoms of post traumatic stress disorder (PTSD) on aspects of mental health such as suicide, depression, substance use, violence, and the inability to maintain relationships1, 2 as well as on aspects of physical health such as general health symptoms, general medical conditions, musculoskeletal pain, cardio-respiratory and gastrointestinal symptoms.3
One factor that may play a role in PTSD symptoms is substance use.4–7 The current research employs a theoretical approach based on Family Interactional Theory (FIT)8 and Life Course Models (LCM)9 of drug use that encompass the relationship between the developmental history of substance use and the risk for psychiatric disorders. According to FIT, the interactive relationships of behavioral factors change over time. Similarly, the LCM hypothesize that the development of the individual is the result of multiple interacting psychosocial and contextual factors. Both FIT and LCM postulate a developmental sequence of individual-level and contextual influences on substance use across the life span. Employing FIT and LCM to guide our study of the consequences of cannabis use, this research makes an innovative contribution to the substance use and psychiatric literature (i.e., PTSD).
In some research, cannabis use has not been considered as a risk factor for PTSD because the use of cannabis, in part, has been treated as a coping mechanism.10–12 Although cannabis use may occur after experiencing a traumatic event for its relief, some research has suggested cannabis use precedes PTSD.13 Using cross-sectional data, Khoury and colleagues have reported that lifetime cannabis dependence was associated with PTSD.5 Another cross-sectional study by Kingston and Raghavan6 reported that early initiation of substance use predicted exposure to traumatic experiences. A longitudinal study by Ullman et al.7 identified pathways from the use of illicit drugs (e.g., cannabis) to the traumatic event of sexual re-victimization in a community sample of female adult sexual assault victims. Characterizing the relationship between cannabis use and symptoms of PTSD may shed light on the developmental pathways from cannabis use to PTSD.
Research on PTSD has identified several associated factors that should be included as control variables in examining the connections between the trajectories of cannabis use and PTSD. The prevalence of PTSD differed by gender (females > males)14 and by race/ethnicity (Blacks > Hispanics).15 Johnson and her colleagues13 reported that alcohol dependence was associated with exposure to subsequent traumatic events for both males and females. Cigarette smoking16 and the use of illicit drugs7 have well established associations with PTSD. Some research has found a relationship between delinquency and trauma.17, 18 Low self-control19 as well as depression20 are well established as risk factors for PTSD. Early trauma-related experiences such as victimization were related to later PTSD.7, 21, 22
In contrast to the majority of earlier studies, we take into consideration the timing and intensity of changes in cannabis use across individuals using a statistical approach for obtaining trajectories from a person-centered analysis of longitudinal data.5 These trajectories reflect a latent or underlying heterogeneity among the members of the sample with regard to cannabis use. Some individuals may begin using cannabis at an early age and escalate rapidly. Other individuals may use cannabis moderately across several developmental stages. By identifying homogeneous subgroups of individuals who use cannabis, membership in each of the subgroups may assist in elucidating multiple pathways to PTSD symptoms.
Our previous research23 identified four trajectories of cannabis use: chronic use, increasing use, moderate use, and no or low use, extending from adolescence (mean age of 14) to early adulthood (mean age of 29). In the present study, we extend previous research23 which assessed the precursors of trajectories of cannabis use. The current analysis makes a substantial contribution over our previous research that assessed individuals to age 29. We have now added measures of cannabis use at two additional points in time (mean ages of 32 and 36) to examine the changes in the patterns of trajectories of cannabis use.
To our knowledge, no studies to date have used trajectory-based models to examine the relation between earlier trajectories of cannabis use and later PTSD symptoms beginning in early adolescence and extending to the fourth decade of life. Moreover, the present study adds to the literature by including several control variables (e.g., early trauma-related experiences) which may moderate the relation between trajectories of cannabis use and PTSD symptoms.
The present study is unique in four ways. First, we assess the associations with PTSD symptoms among relatively understudied minority groups (i.e., African Americans and Puerto Ricans) living in an urban area. Second, we follow our adolescent sample from mean age 14 to mean age 36, in contrast to the majority of prior research, which has been conducted using samples either of adolescents or young adults. Third, we identify the trajectories of cannabis use covering several developmental stages spanning a 22 year period as risk factors of PTSD symptoms. Fourth, when examining the relationship between trajectories of cannabis use and PTSD symptoms, we controlled for demographic factors, drug use, delinquency, self control, depressive symptoms, victimization and sexual assault.
We hypothesize that: 1) based on our previous research,23 there will be four cannabis use trajectory groups; 2) the higher level of cannabis use trajectory groups (e.g., the chronic cannabis use trajectory group, the increasing cannabis use trajectory group, and the moderate cannabis use trajectory group) compared to the no or low cannabis use trajectory group will be associated with an increased likelihood of having PTSD symptoms; and 3) the association between the trajectories of cannabis use and PTSD symptoms will be significant after controlling for a number of dimensions related to the use of cannabis and PTSD symptoms.
Methods
Participants
The current study included 674 African Americans and Puerto Ricans (53% African Americans, 47% Puerto Ricans) from a six wave survey, the Harlem Longitudinal Development Study.8, 24 Among the 674 participants, 60% of the participants were female (n=405). Data on the participants were first collected in 1990 (time 1; T1, N=1,332) when the participants were students attending schools in the East Harlem area of New York City. At T1, the questionnaires were administered in classrooms under the supervision of the study research staff with no teachers present. The mean age of the participants at T1 was 14 years (standard deviation; SD=1.3 years; inter-quartile range from 13 to 15 years). At time 2 (T2; 1994 – 1996; N=1,190), the National Opinion Research Center interviewed the participants in person or by phone. The mean age of the participants at this wave was 19 years (SD=1.5 years; inter-quartile range from 18 to 20 years). At time 3 (T3; 2000 – 2001; N=662 – due to budgetary limitations, we took a subsample of T2 participants), the Survey Research Center of the University of Michigan collected the data. The mean age of the participants at T3 was 24 years (SD=1.3 years; inter-quartile range from 23 to 25 years). At Time 4 (T4), Time 5 (T5), and Time (T6), the data were collected by our research group. At T4 (2004 – 2006; N=838), the mean age was 29 years (SD=1.4 years; inter-quartile range from 28 to 30 years). At T5 (2007 – 2010; N=816), the average age of the participants was 32 years (SD= 1.3 years; inter-quartile range from 31 to 34 years). At T6 (2011 – 2013; N=674), the average age of the participants was 36 years (SD= 1.4 years; inter-quartile range from 35 to 37 years).
The Institutional Review Board (IRB) of the New York University School of Medicine approved the study for T4, T5 and T6, and the IRBs of the Mount Sinai School of Medicine and New York Medical College approved the study’s procedures for data collection in the earlier waves. A Certificate of Confidentiality was obtained from the National Institute on Drug Abuse for T1–T4 and T6 and from the National Cancer Institute at T5. At each time wave, we obtained informed assent or consent from all of the participants. Additional information regarding the study methodology is available from a previous report.24
At T6, we attempted to follow-up all those who participated at T1. We compared the demographic variables for the 674 adults who participated at both T1 and T6 with the 658 who participated at T1 but not at T6. There were no significant differences between the T6 non-participants and the T6 participants in the proportion of African Americans and Puerto Ricans (χ2 (1) = 0.18, p=0.7), mean age at T1 (t=1.93, p=0.05), the frequency of cannabis use at T1 (t=−1.35, p=0.18), the frequency of illicit drug use other than cannabis at T1 (t=1.80, p=0.07), low self-control at T1 (t=0.44, p=0.66) and depressive symptoms at T1 (t=0.53, p=0.6). However, the percentage of males among T6 non-participants (53%) was significantly higher than the percentage of males who participated at T6 (40%) (χ2 (1) = 26.06, p<.001). The frequency of alcohol use at T1 among T6 non-participants (0.3) was higher than the frequency of alcohol use at T1 among T6 participants (0.2) (t = 3.67, p<0.001). The frequency of cigarette use at T1 among T6 non-participants (0.3) was higher than the frequency of cigarette use at T1 among T6 participants (0.2) (t=2.27, p<.05). The mean delinquency score at T1 among T6 non-participants (0.6) was higher than the mean delinquency score at T1 among T6 participants (0.5) (t=2.70, p<.01). We also compared the control variables (i.e., victimization and sexual assault at T2) for the 674 adults who participated at both T2 and T6 with the 516 who participated at T2 but not at T6. There were no significant differences between the T6 non-participants and the T6 participants in the mean scores of victimization at T2 (t=1.51, p=0.13) and sexual assault at T2 (t=0.58, p=0.56).
Measures
Control variables at T1
The participants were asked about their Gender (1=female, 2=male); Race/Ethnicity (1=African American, 2=Puerto Rican); Alcohol Use, a single item, i.e., “How often do you drink beer, wine, or hard liquor?” with a 5-point Likert scale that ranged from “none” to “three or more drinks every day”; Cigarette Use, a single item, i.e., “How many cigarettes do you smoke?” with a 6-point Likert scale that ranged from “none” to “more than one pack a day”; Illicit Drug Use Other Than Cannabis, a single item, i.e., “How often have you used cocaine, crack, ecstasy, etc.? with a 5-point Likert scale that ranged from “never” to “once a week or more”; Delinquency,25 a 10 item scale, e.g., “During the last 5 years, how often have you gotten into a serious fight?” with a 5-point Likert scale that ranged from “never” to “five or more times” (The alpha = 0.76); Low Self-control (Original), an 8 item scale, e.g., “Do you ignore rules when they get in the way?” with a 4-point Likert scale that ranged from “completely false” to “completely true” (The alpha = 0.77); and Depressive Symptoms,26 a 2 item scale, i.e., “Do you sometimes feel unhappy, sad, or depressed?” and “Do you sometimes feel hopeless about the future?” with a 4-point Likert scale that ranged from “not at all” to “extremely.” The correlation between the 2 items assessing depressive symptoms was 0.47 (p<.001).
Control variables at T2
The participants were also asked about their trauma-related experiences: Victimization,27 a 5 item scale, e.g., “How often has someone held a weapon (gun, club, or knife) to you?” with a 5-point Likert scale that ranged from “never” to “5 or more times” (The alpha = 0.70); and Sexual Assault, a single item, i.e., “During the past 5 years, have you been pushed by someone to have sex?” with answer options of “yes” or “no.”
Control variable at T6
The participants reported their age in years.
Cannabis use (T1–T6)
The participants reported their use of cannabis at each wave between T1 and T6. Participants were asked “How often have you ever used cannabis?” at T1 and “How often have you used cannabis in the past 5 years?” at T2 through T6. The answer options were never (0), a few times a year or less (1), about once a month (2), several times a month (3), once a week or more (4).
PTSD Symptoms at T6
PTSD symptoms were assessed by the PCL-S (PTSD Checklist for DSM-IV - Specific) measure. 28 First, participants were asked: “Have you ever experienced or witnessed or had to deal with an extremely stressful or traumatic event that bothered you for at least a month. The event included actual or threatened death or serious injury to you or someone else? (yes or no)” If the participant answered yes to the above question, s/he was asked about each of the 17 experiences.21 The participant rated each experience on a 5-point Likert scale: no (1), a little bothered (2), moderately bothered (3), quite a bit bothered (4), and extremely bothered (5). Each experience had a minimum score for PTSD symptoms.21 A participant was scored as having PTSD symptoms when the following four criteria were met: a) at least one question from 1 through 5 met or exceeded the minimum score, b) at least 3 questions from 6 through 12 met or exceeded the minimum score, c) at least 2 questions from 13 through 17 met or exceeded the minimum score, and d) the summed score of all 17 questions was ≥ 44.
Analytic procedure
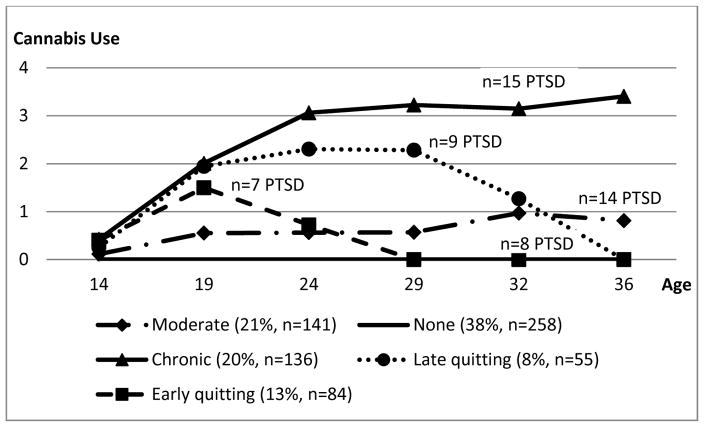
We used a growth mixture model to obtain the trajectories of cannabis use from T1 to T6 using Mplus software.29 An advantage of the growth mixture model is that it takes into consideration the timing, duration, and intensity of changes in cannabis use across individuals over a substantial part of the life span. Cannabis use at each point in time was treated as a censored normal variable. We applied the full information maximum likelihood approach for missing data.29 We used the optimal Bayesian Information Criterion (BIC) to estimate the number of trajectory groups. Each participant was assigned to the trajectory group with the largest Bayesian posterior probability (BPP) to produce Figure 1.
Figure 1.
Developmental Trajectories of Cannabis Use Extending from Adolescence to age 36
Note. Answer options for cannabis use: 0 = never; 1 = a few times a year or less; 2 = about once a month; 3 = several times a month; 4 = once a week or more
To examine the associations of membership in a trajectory group, we used logistic regression analyses30 with the indicator of PTSD symptoms as the dependent variable and the BPP of membership in each trajectory group and the control variables as the independent variables. The BPP of the no or low cannabis trajectory group was used as the reference variable. Gender, race/ethnicity, alcohol use, cigarette use, other illicit drug use, delinquency, low self-control, depressive symptoms at T1, victimization, sexual assault at T2 (as proxies of PTSD symptoms at T6), and age at T6 were used as control variables. The full model including the entire sample and the reduced model including only participants who had experienced a traumatic event were examined.
Results
We computed solutions for 2 through 6 trajectory groups. The BICs for each number of groups were: 2 (7813), 3 (7647), 4 (7598), 5 (7577), and 6 (7593). We chose the 5 trajectory group model because it had the smallest BIC (See Figure 1). After assigning each participant to the group with modal BPP, the mean BPP of the groups ranged from 78% to 98%, which indicated an adequate classification.
As shown in Figure 1, we labeled the five cannabis use trajectory groups as follows. The no cannabis use trajectory group had an estimated prevalence of 38% and included participants who reported no use of cannabis at each wave. The moderate cannabis use trajectory group included participants who reported no use of cannabis at age 14, but use of cannabis a few times a year thereafter. This group had an estimated prevalence of 21%. The chronic cannabis use trajectory group included participants who reported almost no use of cannabis at age 14, but use of cannabis monthly at age 19 (i.e., on average 2 use), and more than several times a month at ages 24, 29, 32, and 36. This group had an estimated prevalence of 20%. The early quitting trajectory group included participants who reported almost no use of cannabis at age 14, but use of cannabis from more than a few times a year (i.e., on average 1.5 use) to less than monthly at age 19, about a few times a year at age 24, and no use of cannabis at ages 29, 32, and 36. This group had an estimated prevalence of 13%. The late quitting trajectory group included participants who reported almost no use of cannabis at age 14, but use of cannabis about monthly (i.e., on average 2 use) at age 19, at least monthly but less than several times a month (i.e., on average 2.5 use) at age 24 and age 29, then use of cannabis from more than a few times a year to less than monthly at age 32, and finally no use of cannabis at age 36. This group had an estimated prevalence of 8%. Overall, the findings indicated at age 36, 41% of the participants continued to use cannabis, 21% of the participants quit their cannabis use, and 38% of the participants never used cannabis.
Table 1 contains the means, SDs, or percentages in each trajectory group for the variables in the study. Among the 674 participants, 205 (31%) answered yes to the screening question, and 53 (8%) were diagnosed as having PTSD at T6.
Table 1.
Means (standard deviation) or percentages in variables by cannabis use trajectory group
| No users (38%, n=258) | Chronic users (20%, n=136) | Late quitters (8%, n=55) | Moderate users (21%, n=141) | Early quitters (13%, n=84) | Whole sample (N=674) | |
|---|---|---|---|---|---|---|
| Control variables | ||||||
| African –American | 54% (n=139) | 56% (n=76) | 60% (n=33) | 46% (n=65) | 51% (n=43) | 53% (n=356) |
| Females | 74% (n=191) | 34% (n=46) | 49% (n=27) | 58% (n=82) | 70% (n=59) | 60% (n=405) |
| Alcohol use at T1 | 0.15 (0.29) | 0.30 (0.44) | 0.34 (0.55) | 0.25 (0.40) | 0.32 (0.42) | 0.24 (0.39) |
| Cigarette use at T1 | 0.08 (0.31) | 0.30 (0.76) | 0.32 (0.78) | 0.20 (0.55) | 0.36 (0.84) | 0.20 (0.60) |
| Illicit drug use other than cannabis at T1 | 0.02 (0.07) | 0.09 (0.38) | 0.05 (0.31) | 0.04 (0.25) | 0.06 (0.27) | 0.04 (0.25) |
| Delinquency at T1 | 0.35 (0.37) | 0.74 (0.69) | 0.62 (0.65) | 0.56 (0.58) | 0.67 (0.56) | 0.53 (0.56) |
| Low self-control at T1 | 2.02 (0.58) | 2.47 (0.60) | 2.24 (0.61) | 2.21 (0.61) | 2.30 (0.56) | 2.20 (0.61) |
| Depressive symptoms at T1 | 1.54 (0.85) | 1.66 (0.90) | 1.67 (0.75) | 1.58 (0.91) | 1.74 (0.95) | 1.61 (0.88) |
| Victimization at T2 | 0.26 (0.39) | 0.58 (0.63) | 0.65 (0.71) | 0.39 (0.55) | 0.45 (0.54) | 0.41 (0.54) |
| Sexual assault at T2 | 15% (n=38) | 24% (n=33) | 24% (n=13) | 22% (n=31) | 26% (n=22) | 20% (n=137) |
| Age at T6 | 35.98 (1.43) | 35.67 (1.38) | 35.92 (1.51) | 35.84 (1.37) | 36.20 (1.31) | 35.91 (1.40) |
| Outcome variable | ||||||
| Screening question | 23% (n=58) | 37% (n=48) | 38% (n=21) | 33% (n=47) | 37% (n=31) | 31% (n=205) |
| PTSD symptoms at T6 | 3% (n=8) | 11% (n=15) | 16% (n=9) | 10% (n=14) | 8% (n=7) | 8% (n=53) |
Note. T1= time 1 (mean age 14); T2=time 2 (mean age 19); T6=time 6 (mean age 36)
Answer options for alcohol use at T1 ranged: none (0), less than once a week (1), once a week to several times a week (2), 1 or 2 drinks a day (3), three or more drinks every day (4).
Answer options for cigarette use at T1 ranged: none (0), a few cigarettes or less a week (1), 1–5 cigarettes (2), about ½ a pack a day (3), about 1 pack a day (4), about 1 and ½ pack a day (5), more than one pack a day (6).
Answer options for illicit drug use other than cannabis at T1 ranged: never (0), a few times a year or less (1), about once a month (2), several times a month (3), once a week or more (4), once a week or more (5).
Answer options for delinquency at T1 ranged: never (0), once (1), twice (2), three or four times (3), five or more times (5).
Answer options for low self-control at T1 ranged: completely false (1), mostly false (2), mostly true (3), completely true (4).
Answer options for depressive symptoms at T1 ranged: not at all (0), a little (1), somewhat (2), extremely (3).
Answer options for victimization at T2 ranged: never (0), once (1), twice (2), three or four times (3), five or more times (4).
Answer options for sexual assault at T2 ranged: no (0), yes (1).
Table 2 presents: a) the odds ratios (OR) without the control variables and b) the adjusted odds ratios (AOR) of the BPP of each cannabis use trajectory group compared to the BPP of the no cannabis use trajectory group for PTSD symptoms at T6 after adjusting for the control variables. Membership in the cannabis use trajectory groups was significantly associated with PTSD symptoms at T6 with the exception of the early quitting trajectory group. A higher BPP for the chronic cannabis use trajectory group (full model: OR=4.52, p<.01, AOR=4.68, p<.01; reduced model: OR=3.12, p<.05, AOR=4.27, p<.05), for the late quitting trajectory group (full model: OR=7.29, p<.001, AOR=6.18, p<.01; reduced model: OR=6.10, p<.01, AOR=6.67, p<.01), and for the moderate cannabis use trajectory group (full model: OR=4.10, p<.01, AOR=3.97, p<.01; reduced model: OR=2.87, p<.05, AOR=3.32, p<.05) was associated with an increased likelihood of having PTSD symptoms at T6 compared with the BPP of the no cannabis use trajectory group. However, the BPP for membership in the early quitting trajectory group compared with the BPP of the no cannabis use trajectory group was not significantly associated with an increased likelihood of having PTSD symptoms at T6 for both full model and reduced model.
Table 2.
Odds ratios (OR) and adjusted odds ratios (AOR) for cannabis use trajectories (age 14 – 36) as related to the symptoms of post traumatic stress disorder (PTSD) at age 36
| Cannabis Use Trajectory (age 14 – 36) | PTSD symptoms (age 36) | |||
|---|---|---|---|---|
|
| ||||
| Full model (N=674) | Reduced model (n=205) | |||
|
| ||||
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | |
| Chronic users vs. no users | 4.52 (1.73, 11.83) ** | 4.68 (1.64, 13.39) ** | 3.12 (1.01, 8.77) * | 4.27 (1.28, 14.20) * |
| Late quitters vs. no users | 7.29 (2.37, 22.41) *** | 6.18 (1.89, 20.23) ** | 6.10 (1.69, 22.0) ** | 6.67 (1.62, 27.44) ** |
| Moderate users vs. no users | 4.10 (1.52, 11.02) ** | 3.97 (1.44, 10.98) ** | 2.87 (1.00, 8.32) * | 3.32 (1.07, 10.34) * |
| Early quitters vs. no users | 3.82 (0.99, 14.79) | 2.51 (0.60, 10.51) | 2.08 (0.50, 8.77) | 1.75 (0.36, 8.44) |
Note:
1. * p<0.05, ** p<0.01, *** p<0.001;
2. OR = Odds ratios without controls;
3. CI = Confidence interval;
4. AOR = Adjusted odds ratios including gender, race/ethnicity, alcohol use, cigarette use, other illicit drug use, delinquency, low self-control, depressive symptoms at age 14, victimization, sexual assault at age 19, and age at age 36 as controls. None of the control variables were statistically significant when examining the association between the trajectories of cannabis use and PTSD symptoms.
5. The full model used the entire sample (N=674).
6. The reduced model used only participants who had experienced a traumatic event (n=205).
Discussion
In our sample, 8% of the participants were diagnosed with PTSD symptoms. This is similar to findings from The National Comorbidity Survey Replication that reported 7% as the lifetime PTSD rate, using a nationally representative sample of 5,692 adults.31. In addition, PTSD United reported that an estimated 8% of Americans have PTSD at any given time.32
The findings indicated that: 1) there were two cannabis quitting trajectory groups (i.e., the early quitting trajectory group and the late quitting trajectory group); 2) the higher cannabis use trajectory groups (i.e., the chronic cannabis use trajectory group, the late quitting trajectory group, and the moderate cannabis use trajectory group) compared to the no cannabis use trajectory group were associated with an increased likelihood of having PTSD symptoms; and 3) the findings were maintained after control on a number of variables including demographic factors (gender, race/ethnicity, and age), substance use (alcohol use, cigarette use, and other illicit drug use), delinquency, low-self control, depressive symptoms in mid adolescence, victimization, and sexual assault in late adolescence.
The present results are consistent with those of Khoury et al.5 who reported that lifetime cannabis dependence was associated with a diagnosis of PTSD and also consistent with findings of other investigators6, 33 who reported that early initiation of substance use (e.g., cannabis use) was associated with exposure to traumatic experiences. Cannabis use may increase the risk of victimization or other traumatic events, and these experiences may increase the probability of experiencing PTSD.
In the present study, membership in the chronic cannabis use trajectory group and in the late quitting trajectory group showed a strong association with having PTSD symptoms at age 36. The relation between chronic cannabis use (as a risk factor to be exposed to a traumatic event) and the symptoms of PTSD may reflect the fact that cannabis using-individuals who are exposed to traumatic events may learn to regulate post traumatic stress symptoms by using cannabis. Therefore, the use of cannabis and PTSD symptoms may have a reciprocal association over time.34, 35 The participants who were in the late quitting trajectory group decreased their cannabis use by age 29 and then finally quit their cannabis use at age 36. This pattern is in accord with findings of Bachman and colleagues who reported that many individuals decrease their cannabis use from the mid-twenties to the early thirties.36
Lisdahl and Price found that increased cannabis use was associated with poorer cognitive functioning.37 Thus, individuals who use cannabis as compared with individuals who do not use cannabis may be more likely to be exposed to traumatic events since they may not realize the dangerous situations they may be in.
Another possible explanation of the relationship between cannabis use and PTSD symptoms is involvement in criminal activities. Indeed, a recent longitudinal study has found that the heavy chronic cannabis use trajectory group as compared with the no use of cannabis trajectory group was associated with an increased likelihood of shooting (or hitting) someone with a weapon.38 In such cases, the individual may be exposed to traumatic events.
Several psychological processes may also be involved to explain the relationship between the trajectories of cannabis use and PTSD symptoms. As noted in the Introduction section, there is evidence that the use of cannabis is related to delinquency and low self-control.39–42 Earlier delinquency, low self-control, depressive symptoms, victimization, and sexual assault have been found to be associated with later PTSD.7, 19–22, 43 However, the association between the trajectories of cannabis use and PTSD symptoms was significant with control on delinquency, low self-control, depressive symptoms, victimization, sexual assault, and demographic factors (gender, race/ethnicity, and age). Several other trait mechanisms could be examined in future research, including such traits as internalizing disorders and poor cognitive functioning.37
The participants in the early quitting trajectory group who quit using cannabis by age 29 did not statistically differ from the participants who were in the no cannabis use trajectory group in terms of having PTSD symptoms at age 36. This study shows the important role that early quitting plays in reducing the probability of PTSD symptoms. Such information will serve as a guide to intervention programs for PTSD.
Limitations
The sample consisted of inner city African American and Hispanic adults tracked from adolescence through their mid 30s. Further studies should include other ethnic groups. Our data are based on self-reports. However, studies have shown that the use of this type of self-report data yields reliable results.44 The absence of any generally accepted explanations of the causal or biological45, 46 mechanisms that link earlier trajectories of cannabis use to later PTSD symptoms is another limitation of this approach. Also, there is some controversy in the field as to the best criteria for deciding on the number of trajectory groups. We used the generally accepted convention of using the smallest BIC as the basis for estimating the number of trajectory groups. Lastly, PTSD symptoms were assessed only at the last time point. Future studies should assess the symptoms of PTSD at multiple time points as PTSD symptoms may present at one or more developmental stages.
Despite these limitations, the study supports and adds to the literature. Unlike most research that focuses on one point in time, we assess cannabis use over a span of up to 22 years. The prospective nature of the data allowed us to go beyond a cross-sectional analysis and to consider the temporal sequencing of variables. Trajectory analysis using a growth mixture model also allowed us to observe the patterns of cannabis use during significant developmental stages across the lifetime. In addition, the study contributes to a set of findings relating to different trajectories of cannabis use beginning in adolescence associated with adult PTSD symptoms in a sample of African American and Puerto Rican individuals living in an urban area of New York City.
Conclusions
The results underscore the value of a person-centered approach to understanding the relations between cannabis use and PTSD symptoms during the transition from adolescence to adulthood. The findings provide information that PTSD symptoms in the mid 30s can possibly be reduced by decreasing the chronic cannabis use trajectory group, the late quitting trajectory group, and the moderate cannabis use trajectory group. Future research with larger and more diverse samples of individuals at different developmental stages is necessary to examine further the association of the trajectories of cannabis use with PTSD symptoms.
Acknowledgments
Funding
This research was supported by the following grants from the NIH: DA05702 awarded to Dr. J.S. Brook and K01 DA041609 awarded to Dr. Lee, both from the National Institute on Drug Abuse.
Footnotes
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
References
- 1.Tanielian T, Jaycox LH. Post-Traumatic Stress Disorder Among Adults. 2008. The Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery (Santa Monica, CA: RAND Corporation, MG-720-CCF, 2008) [Google Scholar]
- 2.Vlahov D, Galea S, Ahern J, et al. Consumption of cigarettes, alcohol, and marijuana among New York City residents six months after the September 11 terrorist attacks. The American Journal of Drug and Alcohol Abuse. 2004;30(2):385–407. doi: 10.1081/ada-120037384. [DOI] [PubMed] [Google Scholar]
- 3.Pacella ML, Hruska B, Delahanty DL. The physical health consequences of PTSD and PTSD symptoms: a meta-analytic review. Journal of Anxiety Disorders. 2013;27(1):33–46. doi: 10.1016/j.janxdis.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 4.Messman-Moore TL, Ward RM, Brown AL. Substance use and PTSD symptoms impact the likelihood of rape and revictimization in college women. Journal of Interpersonal Violence. 2009;24(3):499–521. doi: 10.1177/0886260508317199. [DOI] [PubMed] [Google Scholar]
- 5.Khoury L, Tang YL, Bradley B, Cubells JF, Ressler KJ. Substance use, childhood traumatic experience, and posttraumatic stress disorder in an urban civilian population. Depression and Anxiety. 2010;27(12):1077–1086. doi: 10.1002/da.20751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kingston S, Raghavan C. The relationship of sexual abuse, early initiation of substance use, and adolescent trauma to PTSD. Journal of Traumatic Stress. 2009;22(1):65–68. doi: 10.1002/jts.20381. [DOI] [PubMed] [Google Scholar]
- 7.Ullman SE, Najdowski CJ, Filipas HH. Child sexual abuse, post-traumatic stress disorder, and substance use: Predictors of revictimization in adult sexual assault survivors. Journal of Child Sexual Abuse. 2009;18(4):367–385. doi: 10.1080/10538710903035263. [DOI] [PubMed] [Google Scholar]
- 8.Brook JS, Brook DW, Gordon AS, Whiteman M, Cohen P. The psychological etiology of adolescent drug use: a family interactional approach. Genetic, Social, and General Psychology Monographs. 1990;116:111–267. [PubMed] [Google Scholar]
- 9.Wright BRE, Caspi A, Moffitt TE, Silva PA. The effects of social ties on crime vary by criminal propensity: a life-course model of interdependence. Criminology. 2001;39(2):321–348. [Google Scholar]
- 10.Bonn-Miller MO, Babson KA, Vujanovic AA, Feldner MT. Sleep problems and PTSD symptoms interact to predict marijuana use coping motives: A preliminary investigation. Journal of Dual Diagnosis. 2010;6(2):111–122. [Google Scholar]
- 11.Potter CM, Vujanovic AA, Marshall-Berenz EC, Bernstein A, Bonn-Miller MO. Posttraumatic stress and marijuana use coping motives: the mediating role of distress tolerance. Journal of Anxiety Disorders. 2011;25(3):437–443. doi: 10.1016/j.janxdis.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buckner JD, Zvolensky MJ, Crosby RD, Wonderlich SA, Ecker AH, Richter A. Antecedents and consequences of cannabis use among racially diverse cannabis users: an analysis from ecological momentary assessment. Drug and Alcohol Dependence. 2015;147:20–25. doi: 10.1016/j.drugalcdep.2014.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson SD, Striley C, Cottler LB. The association of substance use disorders with trauma exposure and PTSD among African American drug users. Addictive Behaviors. 2006;31(11):2063–2073. doi: 10.1016/j.addbeh.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Dell’Osso L, Carmassi C, Massimetti G, Daneluzzo E, Di Tommaso S, Rossi A. Full and partial PTSD among young adult survivors 10 months after the L’Aquila 2009 earthquake: Gender differences. Journal of Affective Disorders. 2011;131(1):79–83. doi: 10.1016/j.jad.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 15.Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine. 2011;41(01):71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feldner MT, Babson KA, Zvolensky MJ. Smoking, traumatic event exposure, and post-traumatic stress: A critical review of the empirical literature. Clinical Psychology Review. 2007;27(1):14–45. doi: 10.1016/j.cpr.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martin D, Martin M, Dell R, Davis C, Guerrieri K. Profile of incarcerated juveniles: Comparison of male and female offenders. Adolescence. 2008;43(171):607–622. [PubMed] [Google Scholar]
- 18.Ford JD, Elhai JD, Connor DF, Frueh BC. Poly-victimization and risk of posttraumatic, depressive, and substance use disorders and involvement in delinquency in a national sample of adolescents. Journal of Adolescent Health. 2010;46(6):545–552. doi: 10.1016/j.jadohealth.2009.11.212. [DOI] [PubMed] [Google Scholar]
- 19.Walter KH, Gunstad J, Hobfoll SE. Self-control predicts later symptoms of posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy. 2010;2(2):97–101. [Google Scholar]
- 20.Campbell DG, Felker BL, Liu C-F, et al. Prevalence of depression–PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. Journal of General Internal Medicine. 2007;22(6):711–718. doi: 10.1007/s11606-006-0101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee JY, Brook JS, Finch SJ, Brook DW. Pathways from victimization to substance use: post traumatic stress disorder as a mediator. Psychiatry Research. 2016;237:153–158. doi: 10.1016/j.psychres.2016.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Komarovskaya I, Brown AD, Galatzer-Levy IR, et al. Early physical victimization is a risk factor for posttraumatic stress disorder symptoms among Mississippi police and firefighter first responders to Hurricane Katrina. Psychological Trauma: Theory, Research, Practice, and Policy. 2014;6(1):92–96. [Google Scholar]
- 23.Brook JS, Lee JY, Finch SJ, Seltzer N, Brook DW. Adult work commitment, financial stability, and social environment as related to trajectories of marijuana use beginning in adolescence. Substance Abuse. 2013;34(3):298–305. doi: 10.1080/08897077.2013.775092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee JY, Brook JS, Finch SJ, Brook DW. Trajectories of cigarette smoking beginning in adolescence predict insomnia in the mid thirties. Substance Use & Misuse. 2016;51(5):616–624. doi: 10.3109/10826084.2015.1126747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huizinga DH, Menard S, Elliott DS. Delinquency and drug use: temporal and developmental patterns. Justice Quarterly. 1989;6(3):419–455. [Google Scholar]
- 26.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behavioral Science. 1974;19(1):1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 27.Chavez EL, Oetting ER, Swaim RC. Dropout and delinquency: Mexican-American and Caucasian non-Hispanic youth. Journal of Clinical Child Psychology. 1994;23(1):47–55. [Google Scholar]
- 28.Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric properties of the PTSD Checklist—Civilian version. Journal of Traumatic Stress. 2003;16(5):495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- 29.Muthén L, Muthén B. Mplus user’s guide. 6. Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- 30.Cody R, Smith J. Applied Statistics and the SAS Programming Language. 5. NJ: Prentice-Hall, Inc; Upper Saddle River: 2005. [Google Scholar]
- 31.Gradus JL. Epidemiology of PTSD. U.S. Department of Veterans Affairs; [Accessed on May 9th, 2016]. PTSD: Center for PTSD. Available at http://www.ptsd.va.gov/professional/PTSD-overview/epidemiological-facts-ptsd.asp. [Google Scholar]
- 32.PTSD-United. [Accessed on May 9th, 2016];PTSD United: Anonymous Social Network. Available at http://www.ptsdunited.org/ptsd-statistics-2/
- 33.Pahl K, Brook JS, Lee JY. Joint trajectories of victimization and marijuana use and their health consequences among urban African American and Puerto Rican young men. Journal of Behavioral Medicine. 2013;36(3):305–314. doi: 10.1007/s10865-012-9425-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mitchell H, Zvolensky MJ, Marshall EC, Bonn-Miller MO, Vujanovic AA. Incremental validity of coping-oriented marijuana use motives in the prediction of affect-based psychological vulnerability. Journal of Psychopathology and Behavioral Assessment. 2007;29(4):277–288. [Google Scholar]
- 35.Cornelius JR, Kirisci L, Reynolds M, Clark DB, Hayes J, Tarter R. PTSD contributes to teen and young adult cannabis use disorders. Addictive Behaviors. 2010;35(2):91–94. doi: 10.1016/j.addbeh.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bachman J, O’Malley P, Johnston L, Bryant A, Merline A. The Decline of Substance use in young adulthood: Changes in Social Activities, Roles, and Beliefs. Mahwah, NJ: Lawrence Erlbaum Associates; 2002. [Google Scholar]
- 37.Lisdahl KM, Price JS. Increased marijuana use and gender predict poorer cognitive functioning in adolescents and emerging adults. Journal of the International Neuropsychological Society. 2012;18(04):678–688. doi: 10.1017/S1355617712000276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brook JS, Lee JY, Finch SJ, Brook DW. Developmental trajectories of marijuana use from adolescence to adulthood: Relationship with using weapons including guns. Aggressive Behavior. 2014;40(3):229–237. doi: 10.1002/ab.21520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.D’Amico EJ, Edelen MO, Miles JN, Morral AR. The longitudinal association between substance use and delinquency among high-risk youth. Drug and Alcohol Dependence. 2008;93(1):85–92. doi: 10.1016/j.drugalcdep.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 40.Mandara J, Rogers SY, Zinbarg RE. The effects of family structure on African American adolescents’ marijuana use. Journal of Marriage and Family. 2011;73(3):557–569. [Google Scholar]
- 41.Ellickson PL, Martino SC, Collins RL. Marijuana use from adolescence to young adulthood: multiple developmental trajectories and their associated outcomes. Health Psychology. 2004;23(3):299. doi: 10.1037/0278-6133.23.3.299. [DOI] [PubMed] [Google Scholar]
- 42.Ellickson PL, Martino SC, Collins RL. Marijuana use from adolescence to young adulthood: Multiple developmental trajectories and their associated outcomes. Health Psychology. 2004;23:299–307. doi: 10.1037/0278-6133.23.3.299. [DOI] [PubMed] [Google Scholar]
- 43.From internalizing to externalizing: Theoretical models of the processes linking PTSD to juvenile delinquency [computer program] Version. Hauppauge, NY: Nova Science Publishers; 2010. [Google Scholar]
- 44.Harrison L, Martin S, Enev T, Harrington D. Comparing drug testing and self-report of drug use among youths and young adults in the general population. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2007. [Google Scholar]
- 45.Neumeister A, Normandin MD, Pietrzak RH, et al. Elevated brain cannabinoid CB1 receptor availability in post-traumatic stress disorder: a positron emission tomography study. Molecular Psychiatry. 2013;18(9):1034–1040. doi: 10.1038/mp.2013.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Trezza V, Campolongo P. The endocannabinoid system as a possible target to treat both the cognitive and emotional features of post-traumatic stress disorder (PTSD) Frontiers in Behavioral Neuroscience. 2013;7:100. doi: 10.3389/fnbeh.2013.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]