Abstract
Purpose
To evaluate healthy eating and physical activity intervention for immigrant families, derived through community-based participation.
Design
Healthy Immigrant Families study, randomized controlled trial with delayed-intervention control group, with families as the randomization unit.
Setting
US Midwest city.
Participants
Participants recruited by community partners from Hispanic, Somali, and Sudanese immigrant communities.
Intervention
Family health promoters from participating communities delivered 6 healthy eating modules, 4 physical activity modules, and 2 modules synthesizing information in 12 home visits (60–90 minutes) within first 6 months. Up to 12 follow-up phone calls to each participant occurred within second 6 months.
Measures
Primary measures were dietary quality measured with weekday 24-hour recall and reported as Healthy Eating Index score (0–100) and physical activity measured with accelerometers (14 wear days) at baseline, 6, 12, and 24 months.
Results
In total, 151 persons (81 adolescents and 70 adults; 44 families) were randomly assigned. At 12 months, significant improvement occurred in Healthy Eating Index score for adults in intervention compared with controls (change, +8.6 vs −4.4; P<.01) and persisted at 24 months (+7.4 from baseline; P<.01). No differences for adolescents and no significant differences occurred between groups and for physical activity.
Conclusions
This intervention produced sustained dietary quality improvement among adults but not adolescents. Program outcomes are relevant to communities working to decrease cardiovascular risk among immigrant populations.
Keywords: community-based participatory research, dietary quality, immigrant refugee health, physical activity
Purpose
Immigrants and their descendants will make up the majority of US population growth in the coming decades (1). Across many studies that have included a range of health measures, immigrants and refugees arrive to the United States healthier than the general population (2). However, residency in North America is associated with accumulation of cardiovascular risk, including increasing rates of obesity (3,4), hyperlipidemia (5), hypertension (6), diabetes mellitus (7), and cardiovascular disease (8,9). Furthermore, children of immigrants living in the United States may be at higher risk of obesity and its associated complications than persons who arrive to the country as adults.
Unhealthy dietary behaviors and low levels of physical activity are associated with each aforementioned risk factor (10–12). Populations that immigrate to high-income nations generally have less healthy behaviors than the nonimmigrant majority populations (13–16). Despite calls for intervention to address nutrition and physical activity among immigrant populations (17–19), few interventions have been reported. Systematic reviews published in 2010 (20) and 2013 (21) identified only 8 studies targeting dietary quality or obesity in the immigrant population; results from these studies suggest that tailored interventions may result in more success than general interventions applied to an immigrant population.
One barrier to designing healthy eating and physical activity interventions is that factors contributing to suboptimal behaviors among immigrant groups are multiple, complex, and not well understood (22,23). The identified factors include disproportionate social, economic, and environmental vulnerabilities that are compounded by the heterogeneous impacts of acculturation, low health literacy, and other migration-specific effects on health (24). Community-based participatory research is an intervention approach designed to collaboratively investigate health topics, in which community members and academic professionals partner in an equitable relationship through all research phases (25–27). Community-based participatory research has been effective in addressing health topics among immigrant and refugee populations (28–35). Although studies are underway (36,37), no results have been published of interventions of nutrition or physical activity, or both, for immigrant populations resulting from a community-based participatory research approach.
The Healthy Immigrant Families (HIF) study is a product of the Rochester (Minnesota) Healthy Community Partnership (RHCP), a CBPR partnership with a mission “to promote health and well-being among the Rochester population through community-based participatory research, education, and civic engagement to achieve good health for all” (38). Since its inception in 2004, RHCP effectively has designed and implemented several interventions with immigrant and refugee populations (28,39). Community and academic partners have conducted every aspect of research together.
The purpose of the HIF study is to leverage the experience of this CBPR partnership (40) to cocreate and evaluate a socioculturally appropriate intervention to enhance dietary quality and improve physical activity with and for immigrant and refugee families living in Rochester, Minnesota. Social cognitive theory (41) formed the conceptual base of intervention development. The theory acknowledges the interaction between individual factors (eg, self-efficacy to eat a healthful diet) and social environmental factors (eg, social support) on behavior change. Low self-efficacy is an important barrier to eating a healthful diet (42) and to being physically active (43). Furthermore, a socially supportive family environment has important positive influence on health behaviors among families of low socioeconomic position (44).
We have previously reported the results of formative research to inform intervention development (45–47). We have detailed previously the accounts of participatory recruitment processes (48), study methods (49), baseline measurements (49), association of distress with health behaviors (50), and training of interventionists (51) for the trial. Herein, we report the results of the HIF study.
Methods
The study design was a randomized controlled trial with families as the unit of randomization and a delayed-intervention control group. The assessments were done at baseline and at 6, 12, and 24 months after intervention initiation (Figure). The Mayo Clinic institutional review board and the Rochester School District approved the trial on behalf of community partners. The trial is registered at ClinicalTrials.gov No. NCT01952808.
Study Setting and Participants
Participants were recruited by RHCP partners from the Hispanic, Somali, and Sudanese communities in Rochester, Minnesota. These partners completed RHCP-developed human subjects protection training (52) before recruitment, which was accomplished through in-person contact and word of mouth with adult members of households throughout the community. Partners identified families who may meet eligibility criteria, explained the study, and gauged interest in participation. Partners obtained permission from an adult family member of an interested household (man or woman) to forward their contact information to a study staff member. A language-congruent study staff member then called the family and performed a telephone screen. Eligible families (all adult and adolescent members) were invited to a study event at a community partner location, where full eligibility screening and informed consent were conducted. Additional details of the community-led recruitment processes for this trial are described elsewhere (48).
Because this was a family-based intervention, eligibility criteria were available for both families and individuals. Eligibility criteria for families were a household with at least 1 adult and at least 1 adolescent aged 10 to 18 years (ie, no less than 2 participants per family). Adolescents were targeted instead of younger children on the basis of perceived need in the community and the enhanced rigor of assessment tools for the primary outcomes among adolescents compared with younger children. Inclusion criteria for individual participants (adults and adolescents) included 1) not planning to move from the area for the next 2 years, 2) willing and able to participate in all study aspects, and 3) able to provide oral informed consent or assent. The 4 individual exclusion criteria were self-reported pregnancy, self-reported insulin-dependent diabetes mellitus, self-reported diagnosis of cancer within the past 3 years, and a “yes” answer to the question “Do you know of any reason why you should not do physical activity?”
Randomization and Blinding
Each participant completed consent, enrollment, randomization, and baseline measurements at a community setting from February through March 2014. Randomization of family clusters (stratified as Hispanic, Somali, or Sudanese community) was achieved with software that allocated participants to either an early- or delayed-intervention group. Randomization status was revealed to participants and research staff only after completion of baseline measurements. Intervention group assignments could not be masked to interventionists and participants because of the logistical needs for coordination among families. However, group assignments were masked to data managers and analysts throughout the study.
Intervention
HIF work groups with community and academic membership developed the intervention framework and content over 2 years. Details of participatory intervention development and implementation of this trial are described elsewhere (49). The study team of community and academic partners created an intervention manual with 12 content modules: 6 for healthful eating (increasing fruit and vegetable consumption, healthful beverages, reducing dietary fats, healthful snacks, portion control, and smart shopping strategies), 4 to address physical activity (increasing physical activity, muscle strength and flexibility, reducing screen time, and overcoming barriers to physical activity), and 2 to synthesize and reinforce the content (exercise/food/work-life balance and celebrating accomplishments). Physical activity content was adapted from Active Living Every Day (53), an evidence-based guide to incorporating more physical activity into busy lifestyles and from the LEARN Program for Weight Management (54). Nutrition content was partially adapted from the Simply Good Eating for English Language Learners (55) curriculum for immigrants and refugee families with low English language literacy. Newsletters were written to underscore the central messages of each module and to incorporate success stories from community members.
Language-congruent family health promoters were trained to deliver the intervention to participants within a participant’s respective community. A working group of multidisciplinary health professionals derived the family health promoter training curriculum, which included the following constructs: community-based participatory research partnership orientation, HIF project orientation, protecting human research participant training, principles of community-based participatory research, social cognitive theory theory–based behavior change principles, motivational interviewing principles, family-focused communication, physical activity principles, nutrition principles, mastery of intervention guide content, and training on the intervention delivery. Approximately 250 hours of training were conducted with each family health promoter, which included practicing all of the modules with families and role playing, including a combined 64 sessions under direct observation (51).
The family health promoters delivered the intervention through 12 home visits (30-90 minutes each) over 6 months, followed by phone calls every 2 weeks (up to 12 calls total) during the next 6 months. At each visit, family health promoters assessed content knowledge and current behaviors related to each module topic, delivered the information, engaged in an interactive activity (eg, working with food models), discussed barriers and potential solutions with the family, and engaged in individual (with each participating adult and adolescent) and family goal setting. Family health promoters included counseling strategies consistent with social cognitive therapy, including role-modeling, feedback, reinforcement, and social support to enrich self-efficacy and behavior change. Furthermore, family health promoters modeled healthful behaviors with the families. An important aspect of this intervention involved family health promoters working with participants to adapt solutions for each family.
Following the completion of home visits, family health promoters began biweekly 15-minute telephone calls to each family (up to 12 calls within 6 months). During these calls with an adult family member, family health promoters obtained a verbal progress report regarding the family’s diet and physical activity relative to their stated goals. They ended each call with a content summary related to 1 of the 12 modules.
Treatment Adherence
A content module was considered to be successfully delivered if it was provided to at least 1 participating adult and 1 adolescent family member. Participants were categorized as receiving adequate intervention dose after they received at least 9 of the 12 home visits and 9 of the 12 phone calls (75% each). A telephone call was counted toward the total if completed by 1 adult participating family member.
Measures
Primary Outcomes
Dietary quality was assessed by a single 24-hour dietary recall collected from each participant through the Automated Self-Administered 24-hour recall system (ASA24), a National Cancer Institute Web-based tool (56). Respondents were guided through the recall interview with a modified version of the US Department of Agriculture (USDA) Automated Multiple-Pass Method. This tool performs well relative to true dietary intake and to traditional interviewer-administered dietary recalls (57,58). The ASA24-Kids system was used for adolescent participants. Recalls were supervised by study staff trained in use of the instrument, including a registered dietician. The tool was available in English and Spanish. Study staff and interpreters completed the recall with participants who spoke other languages. Many ethnic foods are included in the tool, and language-congruent study team members who were experienced with the tool assisted participants with food substitutions when needed. ASA24 data files produced nutrient estimates for each participant based on the USDA Food and Nutrient Database for Dietary Studies, from which we calculated the Healthy Eating Index-2010, as well as intake of fruits, vegetables, and sugar. The Healthy Eating Index, derived directly from the ASA24, is a valid and reliable measure of overall diet quality according to the 2010 Dietary Guidelines for Americans (59). The Healthy Eating Index is reported on a linear scale of 0 to 100, where a higher score reflects a more healthful diet.
Physical activity was measured for each participant with the Kinetic Activity Monitor accelerometer (Kersh Health) (60,61). Participants were instructed to wear the accelerometer at the waist for 14 consecutive days while awake. No feedback was provided to participants from the accelerometer. An assessment was considered valid when participants wore the accelerometer at least 12 hours per day for 5 days. The data collected included sedentary time, as well as time spent performing mild, moderate, and vigorous physical activity.
Secondary Outcomes
Weight was measured to the nearest 0.1 kg with a single digital floor scale (Model 876; Seca) and height to the nearest 0.1 cm with a single stadiometer (Model 213; Seca). Overweight was a body mass index (BMI) of 25.0 to 29.9 kg/m2 for adults and in the 85.0 to 94.9 percentile for adolescents; obesity was a BMI of 30.0 kg/m2 or greater for adults and in the 95.0 percentile for adolescents (62,63). Waist circumference was measured twice to the nearest 0.1 cm with a tape measure at the narrowest part of the torso between the ribs and the iliac crest after removing excess clothing and smoothing the remaining clothes. A third measurement was taken when the difference between the 2 measures exceeded 2.0 cm; the average of the 2 closest measurements was used in the analysis. Systolic and diastolic blood pressures were measured with a mechanical device on the right arm after each participant sat quietly for 5 minutes (64). The average of 2 blood pressure readings (1 minute apart) was used for analysis. Health-related quality of life was measured by single-item linear analog scale assessments of physical and emotional health (65).
Treatment Fidelity
To document fidelity of intervention delivery, family health promoters electronically recorded assessments immediately after each encounter with a family (module delivery and telephone call) using a checklist of key delivery points for each module and call. Protocol deviations were also recorded. These assessments were reviewed with study team members throughout the intervention interval, and difficult scenarios were incorporated into regular directly observed role playing sessions that continued throughout the intervention. Additional details of treatment fidelity assessment among family health promoters for this study have been described elsewhere (51).
Sample Size Considerations
Preliminary data indicated that a moderate effect size could be detected in the outcome variables (40), where a moderate effect size is defined as a half standard deviation difference between groups (66). The study had power to detect at least a moderate effect size for the primary outcomes of dietary quality and physical activity between the 2 groups. A sample of 64 persons per group (128 persons total) provided 80% power for a 2-sample t test to detect differences in the mean changes from baseline of 50% times the standard deviation of dietary improvement or physical activity with a 2-sided alternative and a 5% Type I error rate. Additional persons were accrued to account for cancellation, protocol violations, and incomplete cases.
Analysis
Primary analyses of dietary and physical activity data were compared between groups with a single 2-sample, 2-sided t test and 5% type I error rate. The supplementary analysis of primary outcomes included repeated measures analysis of variance modeling to assess effect of baseline measures and clustering on subsequent values. We used the individual person as the analysis unit because of the impractically large sample size that would have been required use of a family as the unit. Therefore, we adjusted for the clustering nature of our sample by including the family as an effect. Analyses of secondary outcomes were conducted either with 2-sample t tests supplemented by mixed effects modeling when the studied variable was continuous in nature or with Fisher exact test comparing relative incidence rates of each outcome supplemented by logistic regression to assess the effect of covariates on univariate results, with the family as an effect in the model. We performed additional subgroup analysis to evaluate outcomes separately for adults and adolescents. Missing data were managed with simple imputation methods, including last, minimum, average, or maximum value carried forward, followed by multiple imputation methods to assess the robustness of study results when data were missing. All analyses were performed using statistical software (SAS version 9.3; SAS Institute Inc).
Results
Participants
Target enrollment was achieved with 151 persons (81 adolescents and 70 adults) from 44 families undergoing randomization. Of these, 25 families (76 persons) were in the early-intervention group and 19 families (75 persons) were in the delayed-intervention (control) group. No significant demographic differences or baseline differences were found between the 2 groups for any primary or secondary outcome measure, with the exception of more Hispanic adolescents in the early intervention group (23 in the early intervention group versus 15 in the delayed intervention group; P=.04) (49). Baseline characteristics of the study population are shown in Table 1.
Table 1.
Baseline Characteristics of the Healthy Immigrant Families Study Population of 151 Persons
| Characteristica | Adolescentsb (n=81) | Adults (n=70) |
|---|---|---|
| Age, mean (SD), y | 13.5 (2.5) | 39.1 (10.9) |
| Female sex | 41 (51.6) | 50 (71.4) |
| Ethnicity/race | ||
| Hispanic | 37 | 43 |
| Somali | 40 | 24 |
| Sudanese | 4 | 3 |
| Born in United States | 36 (44.4) | 7 (10.0) |
| Time living in United States, mean (SD), y | 6.8 (4.5) | 13.8 (8.4) |
| English as the language at home | 39 (48.1) | 17 (24.3) |
| Limited English language proficiency | 10 (12.3) | 32 (45.7) |
| Marital status of married | NA | 50 (71.4) |
| Education status | NA | (n=65) |
| ≤8th grade | 31 (47.7) | |
| Some high school | 5 (7.7) | |
| High school graduation | 26 (40.0) | |
| College or graduate degree | 3 (4.6) | |
| Work status | NA | (n=68) |
| Full time | 23 (33.8) | |
| Part time | 8 (11.8) | |
| Unemployed | 37 (54.4) | |
| Mean annual family income | NA | (n=59) |
| $0–$9,999 | 21 (35.6) | |
| $10,000–$19,999 | 4 (6.8) | |
| $20,000–$29,999 | 10 (16.9) | |
| $30,000–$39,999 | 14 (23.7) | |
| $40,000 and higher | 10 (16.9) | |
| Health insurance | NA | (n=64) |
| None | 22 (34.4) | |
| Medicaid/Medicare | 27 (42.2) | |
| Private | 14 (21.9) | |
| Household size, mean (SD), No. of persons | NA | 5.6 (2.3) |
| Dietary quality | ||
| HEI score (range 0–100), mean (SD) | 51.9 (11.4) | 57.1 (13.5) |
| Vegetables, mean (SD) cup equivalents | 1.3 (0.9) | 1.7 (1.5) |
| Fruit, mean (SD), cup equivalents | 1.8 (1.5) | 1.4 (1.2) |
| Sugar, mean (SD), g | 139.8 (114.4) | 97.6 (55.0) |
| Physical activity | ||
| Moderate to vigorous, mean (SD), min/d | 64.7 (30.2) | 43.1 (35.4) |
| Sedentary, mean (SD), min/d | 795.3 (163.2) | 714.2 (181.4) |
| Biometric data | (n=65) | |
| BMI, mean (SD), kg/m2 | 23.8 (5.4) | 30.2 (6.8) |
| Normal weightc | 44 (54.3) | 13 (20.0) |
| Overweightd | 14 (17.3) | 21 (32.3) |
| Obesee | 23 (28.4) | 31 (47.7) |
| Systolic blood pressure, mean (SD), mm Hg | 111.1 (10.0) | 122.1 (14.7) |
| Diastolic blood pressure, mean (SD), mm Hg | 65.4 (7.7) | 76.3 (9.0) |
| Waist circumference, mean (SD), cm | 80.9 (12.6) | 98 (13.3) |
| Abdominal obesityf | NA | 42 (60.0) |
| Quality of lifeg | ||
| Physical well-being | 3.5 (1.2) | 3 (1.0) |
| Mood | 3.5 (1.2) | 3.3 (1.2) |
Abbreviations: BMI, body mass index; HEI, Healthy Eating Index; NA, not applicable.
Values are presented as number and percentage of persons unless specified otherwise.
Aged 10 to 18 years.
BMI <85.0 percentile for adolescents or <25 kg/m2 for adults.
BMI 85.0–94.9 percentile for adolescents or 25.0–29.9 kg/m2 for adults.
BMI ≥95.0 percentile for adolescents or ≥30.0 kg/m2 for adults.
Waist circumference >88.0 cm for women and >102.0 cm for men.
All domains reported as mean (SD) on 5-point Likert scale, with 1 being the lowest response option and 5 the highest.
Of the 25 families allocated to the early-intervention arm, 23 (92%) received the intervention (2 families were lost to follow-up before intervention initiation). Of the initial 151 persons, loss to follow-up was 16 (11%) at 6 months, 28 (19%) at 12 months (the primary end point), and 48 (32%) at 24 months (Figure). The family health promoters completed documentation for 294 (98%) of the 301 sessions. Visits lasted a mean (SD) period of 50.7 (12.2) minutes (range, 20–90 minutes). For treatment adherence, 100% of the participating families met the predefined criteria for treatment adherence, and every family had at least 1 individual receive the entire intervention (12 visits). Most visits included at least 1 adult (91%) and 1 adolescent (88%). The mean treatment fidelity related to intervention delivery was between 82% and 89% for each domain (51).
For all data reported, we found no statistically significant differences between the 3 racial/ethnic groups. Therefore, all data are reported in aggregate.
Dietary Quality
At baseline, moderate dietary quality was demonstrated with the Healthy Eating Index. Mean (SD) scores were 57.1 (13.5) for adults and 51.9 (11.4) for adolescents (Table 1). At 12 months, a significant improvement was seen in the Healthy Eating Index score for adults in the intervention group compared with controls (change of +8.6 vs −4.4, P<.01) that persisted at 24 months (+7.4 from baseline, P<.01). This change was mediated by statistically significant improvements in so-called empty calories (reduction of calories from solid fats, alcoholic beverages, and added sugars) (P<.05), increased greens and beans (P≤.005), and decreased refined carbohydrates (P<.05), as well as nonsignificant increases in overall intake of fruits and vegetables at 12 months. Similarly, 47% of adults achieved the goal of no sugar-sweetened beverages (eg, regular soda, sports drink, fruit drink) at 12 months, compared with 10% of controls (P<.005) (Table 2).
Table 2.
Healthy Immigrant Families Study Outcomes
| Outcome | Control Group
|
Intervention Group
|
6-mo P Value |
0–12 mo P Value |
||
|---|---|---|---|---|---|---|
| Change 0–6 mo |
Change 0–12 mo |
Change 0–6 mo |
Change 0–12 mo |
|||
| Adult Participants | ||||||
| Dietary quality | ||||||
| HEI score (range 0–100), mean (SD) | 0.9 (16.9) | −4.4 (21.0) | 5.6 (12.4) | 8.6 (13.3) | .17 | .004 |
| Fruit and vegetables, mean (SD), cup equivalents | 0.1 (2.4) | 0.0 (3.4) | 0.1 (2.7) | 0.9 (2.4) | .92 | .39 |
| Sugar, mean (SD), g | −18.3 (58.2) | −26.4 (51.7) | −13.2 (45.2) | −5.0 (61.3) | .52 | .09 |
| Physical activity | ||||||
| Moderate to vigorous, mean (SD), min/d | 8.7 (19.1) | −8.0 (15.8) | 15.1 (81.2) | −3.7 (35.1) | .65 | .12 |
| Sedentary, mean (SD), min/d | −38.0 (150.1) | 19.8 (125.8) | −43.5 (211.6) | −48.9 (183.6) | .81 | .19 |
| Biometric data | ||||||
| BMI, mean (SD), kg/m2 | −0.9 (1.5) | 0.6 (1.7) | −1.3 (1.3) | 0.2 (1.6) | .29 | .24 |
| Waist circumference, mean (SD), cm | −3.6 (6.3) | 1.5 (5.8) | −0.9 (5.9) | 0.6 (7.0) | .20 | .60 |
| Systolic blood pressure, mean (SD), mm Hg | −3.0 (9.6) | −2.7 (13.5) | 0.5 (12.1) | 0.7 (11.3) | .11 | .13 |
| Diastolic blood pressure, mean (SD), mm Hg | −2 (7.2) | −1.2 (9.9) | −0.8 (8.0) | 0.3 (9.1) | .41 | .48 |
| Quality of life | ||||||
| Physical well-being | — | 0.0 (1.2) | — | 0.4 (0.9) | — | .25 |
| Mood | — | −0.2 (1.6) | — | 0.3 (1.0) | — | .27 |
| Adolescent Participants | ||||||
| Dietary quality | ||||||
| HEI score (range, 0–100), mean (SD) | −0.8 (14.2) | 1.4 (13.2) | 2 (13.1) | −0.2 (10.9) | .54 | .73 |
| Fruits and vegetables, mean (SD), cup equivalents | −0.9 (2.0) | 0.3 (2.6) | 0.2 (2.0) | 0.2 (1.8) | .07 | .96 |
| Sugar, mean (SD), g | −11.5 (72.4) | 0 (90.4) | −3.7 (51.4) | −12.1 (60) | .96 | .62 |
| Physical activity | ||||||
| Moderate to vigorous, mean (SD), min/d | 9.3 (39.5) | −16.2 (44.1) | 12 (26.9) | −4.3 (23.7) | .83 | .56 |
| Sedentary, mean (SD), min/d | −1.6 (171.8) | 73.5 (179.5) | −11.7 (116.6) | 55.5 (131.5) | .71 | .91 |
| Biometric data | ||||||
| BMI, mean (SD) | −0.1 (3.9) | 0.5 (1.7) | 1.6 (1.9) | 0.5 (1.6) | .89 | .97 |
| Systolic blood pressure, mean (SD), mm Hg | 0.3 (7.5) | 0.5 (8.4) | −0.9 (10.7) | 2.6 (9.3) | .63 | .28 |
| Diastolic blood pressure, mean (SD), mm Hg | 0.1 (9.8) | −0.3 (10) | −2.2 (7.8) | 0.3 (8.9) | .23 | .65 |
| Quality of life | ||||||
| Physical well-being | — | 0.4 (1.3) | — | −0.1 (1.8) | — | .23 |
| Mood | — | 0.1 (1.8) | — | 0.2 (1.5) | — | .88 |
Abbreviations: BMI, body mass index; HEI, Healthy Eating Index.
Finally, improvement in Healthy Eating Index score for adults was replicated in the delayed-intervention group at 12 months (+9.8 from baseline, P≤.01) (Table 3). Adolescents had nonsignificant improvements in Healthy Eating Index score, fruit and vegetable consumption, and sugar intake at 6 months in the intervention group compared with controls (Table 2). However, these findings were not sustained at 12 months.
Table 3.
Results of 24-Month Measures for Healthy Immigrant Families, Adult Participants
| Outcome | Delayed-Intervention Group
|
Early-Intervention Group
|
||
|---|---|---|---|---|
| Change From 12 to 24 mo |
P Value | Change From 0 to 24 mo |
P Value | |
| Dietary quality | ||||
| HEI score (range, 0–100), mean (SD) | 9.8 | .01 | 7.4 | .006 |
| Fruit and vegetables, mean (SD), cup equivalents | 1.3 | 0.1 | ||
| Sugar, mean (SD), g | 16.2 | .29 | −14.4 | .34 |
| Physical activity | ||||
| Moderate to vigorous, mean (SD), min/d | 2.5 | .28 | 8.1 | .04 |
| Sedentary, mean (SD), min/d | 11.5 | .76 | 14.1 | .78 |
| Biometric data | ||||
| BMI, mean (SD), kg/m2 | −0.4 | .33 | 0.2 | .60 |
| Waist circumference, mean (SD), cm | −1.7 | .31 | 1.4 | .43 |
| Systolic blood pressure, mean (SD), mm Hg | 2.9 | .15 | −0.7 | .69 |
| Diastolic blood pressure, mean (SD), mm Hg | −0.3 | .87 | −2.5 | .13 |
| Quality of life | ||||
| Physical well-being | 0.3 | .38 | 0.4 | .12 |
| Mood | −0.2 | .33 | 0.5 | .11 |
Abbreviations: BMI, body mass index; HEI, Healthy Eating Index.
Physical Activity
At baseline, data from accelerometers were collected for 148 participants (98%). Accelerometers were worn for a mean (SD) time of 11.9 (4.8) hours per day for 11.4 (6.4) days, and the predetermined threshold for valid data was achieved by 117 participants (77%). Baseline physical activity values were relatively high: Mean (SD) time spent per day in moderate to vigorous physical activity was 64.7 (30.2) minutes for adolescents and 43.1 (35.4) minutes for adults (Table 1).
No statistically significant differences were seen at 6 months and 12 months between the intervention group and controls for moderate to vigorous physical activity or sedentary time among adults or adolescents (Table 2). Nonsignificant trends toward improvements in physical activity measures were found for adults and adolescents compared with controls at 6 months, but these findings were not sustained at 12 months.
Secondary Outcome Measures
Baseline biometric measurements showed that 37 adolescents (45.7%) and 52 adults (80.0%) were overweight or obese (Table 1). At 6 months and 12 months, no significant differences were found in BMI, waist circumference, or blood pressure in the intervention group compared with control group overall or for participants who were overweight or obese at baseline (Table 2).
For quality-of-life measures, nonsignificant trends toward improvement in physical well-being and mood were found among adults at 12 months in the intervention group compared with controls and were sustained at 24 months (Tables 2 and 3). Adolescents showed no significant changes in either of these domains following the intervention (Table 2).
Discussion
In this intervention of healthful eating and physical activity derived through a community-based participatory research approach with and for immigrant families, intervention participants had sustained improvements in dietary quality among adults but not among adolescents. No significant improvements occurred in physical activity level among adults or adolescents. A key finding is the high rate of intervention adherence and study retention among participating families, demonstrating the feasibility of conducting a randomized controlled trial in these immigrant communities. Other strengths are high intervention fidelity among family health promoters and community leadership through every study phase, which highlights the fact that rigorous study procedures can be sustained by incorporating participatory approaches in research. This trial is among the first reported community-based interventions to use a community-based participatory research approach to address decreases in dietary quality and physical activity in populations after immigration to the United States.
Among adults in the intervention group, dietary quality improved in a substantive and consistent manner at 12 months compared with controls and the improvement was sustained through the 24-month measures—a finding replicated in the delayed-intervention control group. This change was mediated by improvements in intake of empty calories, of fruits and vegetables, and of refined carbohydrates. This clinically significant behavior change reflects the content of the intervention modules and the goals established by most of the families.
Physical activity is associated with positive physical and mental health, thus we find it disappointing that the intervention did not improve physical activity levels. In looking to explain this lack of effect, we found that in contrast to seeking to improve their dietary quality, most participating families and individuals in this study did not cite improvement of physical activity as a goal. In addition, baseline objective levels of physical activity were high (49), creating a potential ceiling effect. These baseline findings are similar to data among racial/ethnic minority groups in the United States, in which physical activity level objectively measured with an accelerometer is higher than physical activity levels in the general population (67,68). These 2 factors—physical activity improvements as lower priorities for participating families and high baseline objective levels of physical activity—likely accounted for the lack of improvement in physical activity in this study.
Obesity is an important health problem among immigrant populations, and 80% of adults in the present study were overweight or obese at baseline. The difference in BMI reduction between intervention adults and control adults did not achieve statistical significance. However, the relatively large effect at 6 months suggests a possibility of clinically meaningful reduction in BMI among adults as a result of the intervention that was not sustained at 12 or 24 months. Although this study was not intended as a weight-loss intervention, future research is warranted to test the addition of dietary weight-loss principles (eg, calorie restriction, tracking daily intake, planning meals, managing urges for overeating) to the existing intervention modules, to promote weight loss and weight-loss maintenance among immigrants who are overweight or obese. Past research findings suggest that these interventions may be most successful when they are implemented within 10 years of immigration to the United States (3).
For adolescents in the early-intervention arm, no improvement was seen for either primary outcome. This result may reflect factors of intervention dose and implementation audience strategy. Delivery of each module required participation of at least 1 adult and 1 adolescent. While treatment fidelity related to delivery of the intervention was high, most participating families included more than 1 adolescent, such that individual participation in modules was inconsistent for the specific study adolescents compared with the enrolled study adults (51). Family health promoters reported difficulties with adolescents being unable to participate in counseling sessions because of after-school activities. For this reason, the modules tended to be delivered for the more engaged adult audience members. Furthermore, analysis of baseline data showed a positive association between mood and healthful behaviors (50), suggesting that mood management strategies should be included as a component of future interventions with adolescent participants. Future development of family-based interventions among these immigrant populations will require more intentional engagement of adolescents during the planning and implementation phases.
Limitations
The study has several important limitations. Although the randomized study design was optimal, a risk existed of indirect intervention dissemination to the control group through social networks among these immigrant communities in a single small city, a phenomena common to behavior-change interventions (69). The observed improvements for several variables among the control group, despite no significant improvement in secular trends, suggest that intervention diffusion to the control group occurred in this study. For logistical reasons in this community-based study, only a single 24-hour dietary recall measure was obtained for each participant at every measurement point. Therefore, only group-level changes can be inferred from these data. For practical reasons, individuals were used as the unit of analysis even though families were used as the unit of randomization. These individuals may not represent the results of the entire family, and results for individuals within the same family may be correlated. Although the analyses were adjusted for a family effect, the study results would have been more robust with a larger sample size, thereby allowing the use of families as the unit of analysis. Finally, although treatment conditions were masked to the investigators and data analysts, it was not practical to maintain blinding for the interventionists (family health promoters) with direct participant contact.
Significance
Healthy Immigrant Families is a multicomponent intervention, cocreated by community and academic partners, that resulted in the successful enrollment and study completion of adult and adolescent immigrants and produced sustained improvement of dietary quality among adults, but not among adolescents, in Rochester, Minnesota. It was feasible to conduct a randomized controlled trial in the participating immigrant groups, indicating substantial community support for our approach. Program outcomes are relevant to other communities working to reduce the accumulation of cardiovascular health risk among these adult and adolescent immigrant populations.
Figure.
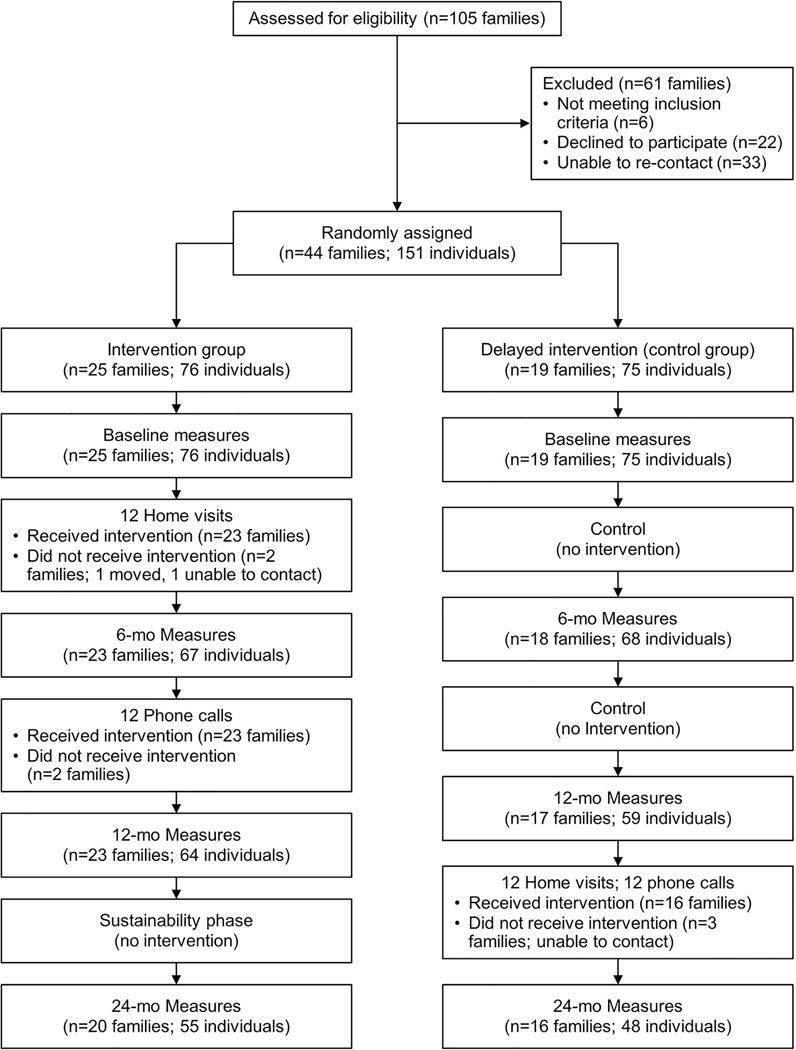
Flowchart of Healthy Immigrant Families Study Overview.
So What? Implications for Health Promotion Practitioners and Researchers.
What Is Already Known on this Topic?
Immigrants to the United States often have escalating cardiovascular risk after arrival. Barriers to healthy eating and physical activity are important contributors to this risk.
What Does This Article Add?
This multicomponent intervention, cocreated by community and academic partners, resulted in the successful enrollment and study completion of adult and adolescent immigrants and produced sustained improvement of dietary quality among adults but not among adolescents.
What Are the Implications for Health Promotion Practice or Research?
Outcomes are relevant to other communities working to reduce the accumulation of cardiovascular health risk among these adult and adolescent immigrant populations.
Acknowledgments
The authors thank the RHCP partners who contributed to the organization, implementation, and dissemination of this work.
This publication was supported by National Institutes of Health (NIH) Grant No. R01 HL 111407 from the National Heart, Lung, and Blood Institute; by National Center for Advancing Translational Science Grant No. UL1 TR000135; and by the Mayo Clinic Office of Health Disparities Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The funding bodies had no role in study design; in the collection, analysis, and interpretation of data; writing of the manuscript; and in the decision to submit the manuscript for publication.
Abbreviations
- ASA24
Automated Self-Administered 24-hour dietary recall
- BMI
body mass index
- HIF
Healthy Immigrant Families
- RHCP
Rochester Healthy Community Partnership
- USDA
US Department of Agriculture
Footnotes
Declaration of Conflicting Interests: J. A. Levine provides advice to Kersh Health, inventor of the accelerometer used in this study, without financial gain. The other authors declare that they have no conflict of interest.
Publisher: To expedite proof approval, send proof via email to scipubs@mayo.edu.
This trial was registered at ClinicalTrials.gov No. NCT01952808.
References
- 1.Passel JS, Cohn D. US population projections: 2005–2050. Washington, DC: Pew Research Center; c2008. [Google Scholar]
- 2.Singh GK, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. Am J Public Health. 2001 Mar;91(3):392–9. doi: 10.2105/ajph.91.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goel MS, McCarthy EP, Phillips RS, Wee CC. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004 Dec 15;292(23):2860–7. doi: 10.1001/jama.292.23.2860. [DOI] [PubMed] [Google Scholar]
- 4.Kaplan MS, Huguet N, Newsom JT, McFarland BH. The association between length of residence and obesity among Hispanic immigrants. Am J Prev Med. 2004 Nov;27(4):323–6. doi: 10.1016/j.amepre.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 5.Koya DL, Egede LE. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007 Jun;22(6):841–6. doi: 10.1007/s11606-007-0163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steffen PR, Smith TB, Larson M, Butler L. Acculturation to Western society as a risk factor for high blood pressure: a meta-analytic review. Psychosom Med. 2006 May-Jun;68(3):386–97. doi: 10.1097/01.psy.0000221255.48190.32. [DOI] [PubMed] [Google Scholar]
- 7.Creatore MI, Moineddin R, Booth G, Manuel DH, DesMeules M, McDermott S, et al. Age-and sex-related prevalence of diabetes mellitus among immigrants to Ontario, Canada. CMAJ. 2010 May 18;182(8):781–9. doi: 10.1503/cmaj.091551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lear SA, Humphries KH, Hage-Moussa S, Chockalingam A, Mancini GB. Immigration presents a potential increased risk for atherosclerosis. Atherosclerosis. 2009 Aug;205(2):584–9. doi: 10.1016/j.atherosclerosis.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 9.Lutsey PL, Diez Roux AV, Jacobs DR, Jr, Burke GL, Harman J, Shea S, et al. Associations of acculturation and socioeconomic status with subclinical cardiovascular disease in the multi-ethnic study of atherosclerosis. Am J Public Health. 2008 Nov;98(11):1963–70. doi: 10.2105/AJPH.2007.123844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. American College of Sports Medicine; American Heart Association Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007 Aug 28;116(9):1081–93. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 11.Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, et al. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study) Lancet. 2006 Jul 22;368(9532):299–304. doi: 10.1016/S0140-6736(06)69075-2. [DOI] [PubMed] [Google Scholar]
- 12.Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, et al. American Heart Association Nutrition Committee Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006 Jul 4;114(1):82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]; Errata. Circulation. 2006 Dec 5;114(23):e629. [Google Scholar]; Circulation. 2006 Jul 4;114(1):e27. [Google Scholar]
- 13.Centers for Disease Control and Prevention. Prevalence of fruit and vegetable consumption and physical activity by race/ethnicity: United States. MMWR Morb Mortal Wkly Rep. 2005;56:301–4. [PubMed] [Google Scholar]
- 14.Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Prev Med. 2000 Jan;18(1):46–53. doi: 10.1016/s0749-3797(99)00105-1. [DOI] [PubMed] [Google Scholar]
- 15.Sternfeld B, Ainsworth BE, Quesenberry CP. Physical activity patterns in a diverse population of women. Prev Med. 1999 Mar;28(3):313–23. doi: 10.1006/pmed.1998.0470. [DOI] [PubMed] [Google Scholar]
- 16.Gadd M, Sundquist J, Johansson SE, Wandell P. Do immigrants have an increased prevalence of unhealthy behaviours and risk factors for coronary heart disease? Eur J Cardiovasc Prev Rehabil. 2005 Dec;12(6):535–41. doi: 10.1097/01.hjr.0000174829.25388.ed. [DOI] [PubMed] [Google Scholar]
- 17.Kandula NR, Kersey M, Lurie N. Assuring the health of immigrants: what the leading health indicators tell us. Annu Rev Public Health. 2004;25:357–76. doi: 10.1146/annurev.publhealth.25.101802.123107. [DOI] [PubMed] [Google Scholar]
- 18.Singh GK, Kogan MD, Yu SM. Disparities in obesity and overweight prevalence among US immigrant children and adolescents by generational status. J Community Health. 2009 Aug;34(4):271–81. doi: 10.1007/s10900-009-9148-6. [DOI] [PubMed] [Google Scholar]
- 19.Davidson EM, Liu JJ, Bhopal RS, White M, Johnson MR, Netto G, et al. Consideration of ethnicity in guidelines and systematic reviews promoting lifestyle interventions: a thematic analysis. Eur J Public Health. 2014 Jun;24(3):508–13. doi: 10.1093/eurpub/ckt093. [DOI] [PubMed] [Google Scholar]
- 20.Renzaho AM, Mellor D, Boulton K, Swinburn B. Effectiveness of prevention programmes for obesity and chronic diseases among immigrants to developed countries: a systematic review. Public Health Nutr. 2010 Mar;13(3):438–50. doi: 10.1017/S136898000999111X. [DOI] [PubMed] [Google Scholar]
- 21.Nierkens V, Hartman MA, Nicolaou M, Vissenberg C, Beune EJ, Hosper K, et al. Effectiveness of cultural adaptations of interventions aimed at smoking cessation, diet, and/or physical activity in ethnic minorities: a systematic review. PLoS One. 2013 Oct 7;8(10):e73373. doi: 10.1371/journal.pone.0073373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunn JR, Dyck I. Social determinants of health in Canada’s immigrant population: results from the National Population Health Survey. Soc Sci Med. 2000 Dec;51(11):1573–93. doi: 10.1016/s0277-9536(00)00053-8. [DOI] [PubMed] [Google Scholar]
- 23.Malmusi D, Borrell C, Benach J. Migration-related health inequalities: showing the complex interactions between gender, social class and place of origin. Soc Sci Med. 2010 Nov;71(9):1610–9. doi: 10.1016/j.socscimed.2010.07.043. [DOI] [PubMed] [Google Scholar]
- 24.Caperchione CM, Kolt GS, Tennent R, Mummery WK. Physical activity in culturally and linguistically diverse migrant groups to Western society: a review of barriers, enablers and experiences. Sports Med. 2009;39(3):167–77. doi: 10.2165/00007256-200939030-00001. [DOI] [PubMed] [Google Scholar]
- 25.Horowitz CR, Robinson M, Seifer S. Community-based participatory research from the margin to the mainstream: are researchers prepared? Circulation. 2009 May 19;119(19):2633–42. doi: 10.1161/CIRCULATIONAHA.107.729863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shalowitz MU, Isacco A, Barquin N, Clark-Kauffman E, Delger P, Nelson D, et al. Community-based participatory research: a review of the literature with strategies for community engagement. J Dev Behav Pediatr. 2009 Aug;30(4):350–61. doi: 10.1097/DBP.0b013e3181b0ef14. [DOI] [PubMed] [Google Scholar]
- 27.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 28.Wieland ML, Weis JA, Olney MW, Aleman M, Sullian S, Millington K, et al. Screening for tuberculosis at an adult education center: results of a community-based participatory process. Am J Pub Health. 2011 Jul;101(7):1264–7. doi: 10.2105/AJPH.2010.300024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wieland ML, Weis JA, Yawn BP, Sullivan SM, Millington KL, Smith CM, et al. Perceptions of tuberculosis among immigrants and refugees at an adult education center: a community-based participatory research approach. J Immigr Minor Health. 2012 Feb;14(1):14–22. doi: 10.1007/s10903-010-9391-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johnson CE, Ali SA, Shipp MP. Building community-based participatory research partnerships with a Somali refugee community. Am J Prev Med. 2009 Dec;37(6 Suppl 1):S230–6. doi: 10.1016/j.amepre.2009.09.036. [DOI] [PubMed] [Google Scholar]
- 31.Gregg J, Centurion L, Maldonado J, Aguillon R, Celaya-Alston R, Farquhar S. Interpretations of interpretations: combining community-based participatory research and interpretive inquiry to improve health. Prog Community Health Partnersh. 2010 Summer;4(2):149–54. doi: 10.1353/cpr.0.0116. [DOI] [PubMed] [Google Scholar]
- 32.Lam TK, McPhee SJ, Mock J, Wong C, Doan HT, Nguyen T, et al. Encouraging Vietnamese-American women to obtain Pap tests through lay health worker outreach and media education. J Gen Intern Med. 2003 Jul;18(7):516–24. doi: 10.1046/j.1525-1497.2003.21043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cristancho S, Garces DM, Peters KE, Mueller BC. Listening to rural Hispanic immigrants in the Midwest: a community-based participatory assessment of major barriers to health care access and use. Qual Health Res. 2008 May;18(5):633–46. doi: 10.1177/1049732308316669. [DOI] [PubMed] [Google Scholar]
- 34.Martinez IL, Carter-Pokras O. Assessing health concerns and barriers in a heterogeneous Latino community. J Health Care Poor Underserved. 2006 Nov;17(4):899–909. doi: 10.1353/hpu.2006.0129. [DOI] [PubMed] [Google Scholar]
- 35.Lauderdale DS, Kuohung V, Chang SL, Chin MH. Identifying older Chinese immigrants at high risk for osteoporosis. J Gen Intern Med. 2003 Jul;18(7):508–15. doi: 10.1046/j.1525-1497.2003.20331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tovar A, Vikre EK, Gute DM, Kamins CL, Pirie A, Boulos R, et al. Development of the live well curriculum for recent immigrants: a community-based participatory approach. Prog Community Health Partnersh. 2012 Summer;6(2):195–204. doi: 10.1353/cpr.2012.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Renzaho AM, Halliday JA, Mellor D, Green J. The Healthy Migrant Families Initiative: Development of a culturally competent obesity prevention intervention for African migrants. BMC Public Health. 2015 Mar 19;15:272. doi: 10.1186/s12889-015-1628-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rochester Community Health Partnership [Internet] Rochester (MN): c2016. [cited 2016 Dec, 9]. Available from: www.rochesterhealthy.org. [Google Scholar]
- 39.Njeru JW, Patten CA, Hanza MM, Brockman TA, Ridgeway JL, Weis JA, et al. Stories for change: development of a diabetes digital storytelling intervention for refugees and immigrants to Minnesota using qualitative methods. BMC Public Health. 2015 Dec 29;15:1311. doi: 10.1186/s12889-015-2628-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wieland ML, Weis JA, Palmer T, Goodson M, Loth S, Omer F, et al. Physical activity and nutrition among immigrant and refugee women: a community-based participatory research approach. Womens Health Issues. 2012 Mar;22(2):e225–32. doi: 10.1016/j.whi.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004 Apr;31(2):143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 42.Sheeshka JD, Woolcott DM, Mackinnon NJ. Social Cognitive Theory as a framework to explain intentions to practice healthy eating behaviors. J Appl Soc Psych. 1993;23(19):1547–73. [Google Scholar]
- 43.Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc. 2002 Dec;34(12):1996–2001. doi: 10.1097/00005768-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 44.Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, Sallis JF. Physical activity social support and middle- and older-aged minority women: results from a US survey. Soc Sci Med. 1999 Sep;49(6):781–9. doi: 10.1016/s0277-9536(99)00137-9. [DOI] [PubMed] [Google Scholar]
- 45.Tiedje K, Wieland ML, Meiers SJ, Mohamed AA, Formea CM, Ridgeway JL, et al. A focus group study of healthy eating knowledge, practices, and barriers among adult and adolescent immigrants and refugees in the United States. Int J Behav Nutr Phys Act. 2014 May 16;11:63. doi: 10.1186/1479-5868-11-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wieland ML, Tiedje K, Meiers SJ, Mohamed AA, Formea CM, Ridgeway JL, et al. Perspectives on physical activity among immigrants and refugees to a small urban community in Minnesota. J Immigr Minor Health. 2015 Feb;17(1):263–75. doi: 10.1007/s10903-013-9917-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mohamed AA, Hassan AM, Weis JA, Sia IG, Wieland ML. Physical activity among Somali men in Minnesota: barriers, facilitators, and recommendations. Am J Mens Health. 2014 Jan;8(1):35–44. doi: 10.1177/1557988313489132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hanza MM, Goodson M, Osman A, Porraz Capetillo MD, Hared A, Nigon JA, et al. Erratum to: Lessons learned from community-led recruitment of immigrants and refugee participants for a randomized, community-based participatory research study. J Immigr Minor Health. 2016 Oct;18(5):1246. doi: 10.1007/s10903-016-0414-2. [DOI] [PubMed] [Google Scholar]
- 49.Wieland ML, Weis JA, Hanza MM, Meiers SJ, Patten CA, Clark MM, et al. Healthy immigrant families: participatory development and baseline characteristics of a community-based physical activity and nutrition intervention. Contemp Clin Trials. 2016 Mar;47:22–31. doi: 10.1016/j.cct.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morrison EJ, Clark MM, Wieland ML, Weis JA, Hanza MM, Meiers SJ, et al. Relationship between negative mood and health behaviors in an immigrant and refugee population. J Immigr Minor Health. 2017 Jun;19(3):655–64. doi: 10.1007/s10903-016-0506-z. Epub 2016 Sep 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bronars CA, Hanza MM, Meiers SJ, Patten CA, Clark MM, Nigon JA, et al. Treatment fidelity among family health promoters delivering a physical activity and nutrition intervention to immigrant and refugee families. Health Educ Behav. 2017 Apr;44(2):262–70. doi: 10.1177/1090198116650668. Epub 2016 Jul 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hawley NC, Wieland ML, Weis JA, Sia IG. Perceived impact of human subjects’ protection training on community partners in community-based participatory research. Prog Community Health Partnersh. 2014 Summer;8(2):241–8. doi: 10.1353/cpr.2014.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Blair SN, Dunn AL, Marcus BH, Carpenter RA, Jaret P. Active living every day. 2nd. Champaign (IL): Human Kinetics; 2011. [Google Scholar]
- 54.Brownell KD. The LEARN program for weight management. 10th. Dallas (TX): American Health Publishing Company; c2004. [Google Scholar]
- 55.University of MN Extension. Simply good eating for English language learners [Internet] 2009:416. cited 2017 Jun 8. Available from: https://www.extension.umn.edu/family/health-and-nutrition/toolkits-and-resources/simply-good-eating-for-english-language-learners/docs/full-version-ell.pdf.
- 56.National Cancer Institute. [Internet] ASA24: automated self-administered 24-hour dietary assessment tool. [Last updated 2016 Dec 6 cited 2016 Dec 9]. Available from: http://appliedresearch.cancer.gov/asa24.
- 57.Kirkpatrick SI, Subar AF, Douglass D, Zimmerman TP, Thompson FE, Kahle LL, et al. Performance of the automated self-administered 24-hour recall relative to a measure of true intakes and to an interviewer-administered 24-h recall. Am J Clin Nutr. 2014 Jul;100(1):233–40. doi: 10.3945/ajcn.114.083238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Thompson FE, Dixit-Joshi S, Potischman N, Dodd KW, Kirkpatrick SI, Kushi LH, et al. Comparison of interviewer-administered and automated self-administered 24-hour dietary recalls in 3 diverse integrated health systems. Am J Epidemiol. 2015 Jun 15;181(12):970–8. doi: 10.1093/aje/kwu467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guenther PM, Kirkpatrick SI, Reedy J, Krebs-Smith SM, Buckman DW, Dodd KW, et al. The healthy eating index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014 Mar;144(3):399–407. doi: 10.3945/jn.113.183079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Redfield MM, Anstrom KJ, Levine JA, Koepp GA, Borlaug BA, Chen HH, et al. NHLBI Heart Failure Clinical Research Network Isosorbide mononitrate in heart failure with preserved ejection fraction. N Engl J Med. 2015 Dec 10;373(24):2314–24. doi: 10.1056/NEJMoa1510774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zakeri R, Levine JA, Koepp GA, Borlaug BA, Chirinos JA, LeWinter M, et al. Nitrate’s effect on activity tolerance in heart failure with preserved ejection fraction trial: rationale and design. Circ Heart Fail. 2015 Jan;8(1):221–8. doi: 10.1161/CIRCHEARTFAILURE.114.001598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Physical status: the use and interpretation of anthropometry Report of a WHO Expert Committee. World Health Organization; Geneva: 1995. (WHO Technical Report Series No. 854). [PubMed] [Google Scholar]
- 63.Dietz WH, Bellizzi MC. Introduction: the use of body mass index to assess obesity in children. Am J Clin Nutr. 1999 Jul;70(1):123S–5S. doi: 10.1093/ajcn/70.1.123s. [DOI] [PubMed] [Google Scholar]
- 64.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003 May 21;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]; Erratum. JAMA. 2003 Jul 9;290(2):197. [Google Scholar]
- 65.Singh JA, Satele D, Pattabasavaiah S, Buckner JC, Sloan JA. Normative data and clinically significant effect sizes for single-item numerical linear analogue self-assessment (LASA) scales. Health Qual Life Outcomes. 2014 Dec 18;12:187. doi: 10.1186/s12955-014-0187-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cohen J. Statistical power analysis for the behavioral sciences. New York: Academic Press; 1969. [Google Scholar]
- 67.Ham SA, Ainsworth BE. Disparities in data on healthy people 2010 physical activity objectives collected by accelerometry and self-report. Am J Public Health. 2010 Apr 1;100(Suppl 1):S263–8. doi: 10.2105/AJPH.2009.180075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Whitt-Glover MC, Taylor WC, Floyd MF, Yore MM, Yancey AK, Matthews CE. Disparities in physical activity and sedentary behaviors among US children and adolescents: prevalence, correlates, and intervention implications. J Public Health Policy. 2009;30(Suppl 1):S309–34. doi: 10.1057/jphp.2008.46. [DOI] [PubMed] [Google Scholar]
- 69.Hunter RF, McAneney H, Davis M, Tully MA, Valente TW, Kee F. “Hidden” social networks in behavior change interventions. Am J Public Health. 2015 Mar;105(3):513–6. doi: 10.2105/AJPH.2014.302399. [DOI] [PMC free article] [PubMed] [Google Scholar]


