Abstract
Background
Nutrition labels are a low-cost tool with the potential to encourage healthy eating habits.
Objective
Investigate correlates of frequent Nutrition Facts use, describe the types of label information most often used, and measure how label use relates to dietary intake in young adults.
Design
Cross-sectional population-based study of young adults participating in Project EAT-IV (Eating and Activity in Teens and Young Adults).
Participants/Setting
Surveys and food frequency questionnaires were completed in 2015–2016 by young adults (N=1817, weighted sample: 49% women) ages 25–36.
Main Outcome Measures
Nutrition Facts use, frequency of using specific information on labels, dietary intake.
Statistical Analyses Performed
Relative risks and adjusted means were used to examine how demographic, behavioral, and weight-related factors were associated with Nutrition Facts use, and how label use related to dietary outcomes. Associations with p-values <0.05 were considered statistically significant.
Results
Almost a third (31.4%) of participants used Nutrition Facts labels ‘frequently.’ Use was significantly higher for women, for participants with high education and income, among those who prepared food regularly, were physically active, were classified as overweight, and were trying to lose, gain, or maintain weight. Label components used most often included total calories (73.1%), sugars (72.9%), serving size (68.9%), and the ingredient list (65.7%). Nutrition Facts users consumed significantly more fruits, vegetables, and whole grains and fewer sugar-sweetened beverages compared to non-frequent users. Nutrition Facts users ate significantly more frequently at sit-down restaurants but less frequently at fast-food restaurants compared to non-users.
Conclusions
While Nutrition Facts use was associated with markers of better dietary quality in a population-based sample of young adults, only a third of participants used labels frequently. Methods to improve label use should be studied, particularly through leveraging weight- or health-related goals (e.g., interest in making healthier food choices), and meeting consumer preferences concerning label content.
Keywords: Nutrition Facts, nutrition labels, diet, dietary intake, young adults
INTRODUCTION
Nutrition labels are an informational tool with the potential for encouraging healthful purchasing and eating habits. In the overall United States (U.S.) population, use of nutrition labels on packaged foods has been related to healthier dietary choices1; however, systematic reviews show that consumers may not frequently use nutrition labels to make food choices.1, 2 Nutrition Facts labels have been required on most packaged foods in the U.S. since the passage of the Nutritional Labeling and Education Act of 1990.3 In May 2016, the U.S. Food and Drug Administration (FDA) released rules to update the Nutrition Facts panel format and content to make labels more understandable, reflect scientific developments on the role of diet in disease risk, and update servings sizes to better align with actual dietary intake.4 In the context of this recent policy change, research on Nutrition Facts preferences, and how use relates to dietary quality is particularly timely and necessary.
Research examining characteristics of Nutrition Facts users and the relationship between Nutrition Facts use and self-reported dietary intake has suggested label use is related to markers of a healthy diet, but the specific outcomes and impact are less clear. Ollberding et al.5 found Nutrition Facts use among National Health and Nutrition Examination Survey (NHANES) 2005–2006 participants was associated with sociodemographic factors such as being female, white, having high education and income, being older, and living alone; greater use was associated with better dietary patterns including lower sugar, total and saturated fat, and energy consumption. Also in NHANES participants (2007–2010), Bleich and Wolfson6 found that Nutrition Facts use was related to female gender, high education, having white or Hispanic race/ethnicity, and engaging in weight loss activities such as physical activity and using commercial diets, but not weight status.
Measuring Nutrition Facts use in young adults is particularly crucial given the poor dietary quality exhibited by many young adults7, the importance of this period in the establishment of long-term dietary habits8 and chronic disease prevention9, and the potential secondary impact that dietary choices and habits of young adults may have on their own children10, 11. Previous studies in young adults have reported that females12–14 and those with higher nutrition knowledge or education12, 13 may be more likely to use Nutrition Facts. For dietary quality, researchers have found that self-reported general label use (not necessarily Nutrition Facts) was related to consuming more fruits and vegetables15–17 and fiber16, and less fried food18, but not dairy or calcium15. Significant gaps still remain, however, in understanding predictors of Nutrition Facts use besides basic sociodemographic characteristics, the types of information sought by consumers, and how nutrition label users compare on broad dietary outcomes such as restaurant visits, food groups and micronutrients, and compliance with the Dietary Guidelines for Americans.19 Better understanding the types of information that are of interest to consumers can inform future updates to label design and potentially encourage greater label use by aligning policies with consumer preferences.
The purpose of the current study was to investigate the correlates of Nutrition Facts use, the types of label information used most frequently, particularly in relation to the FDA’s 2016 updates to the Nutrition Facts Panel, and the relationship between Nutrition Facts use and measures of dietary intake in a population-based sample of young adults. Available data allowed for building on previous studies by considering a broader range of sociodemographic, weight-related, and behavioral correlates and a comprehensive set of dietary outcomes. This study aimed to better understand sociodemographic and behavioral factors to inform messaging and efforts to promote Nutrition Facts use and consuming a healthy diet in a population at risk of weight gain and poor dietary outcomes.
MATERIALS AND METHODS
Study Design and Sample
Young adults were surveyed as a part of Project EAT-IV (Eating and Activity in Teens and Young Adults), the fourth wave of a longitudinal cohort study measuring diet, physical activity, weight and related factors in adolescents and young adults. Students were initially recruited for Project EAT-I in 1998–1999 from 31 public middle schools and high schools in the Minneapolis-St. Paul metropolitan area of Minnesota. Those who participated in at least one of two prior follow-up surveys were mailed an invitation to participate in Project EAT-IV in 2015–2016 and offered a 50-dollar incentive. Of the original sample,20, 21 2,270 (58.4%) young adults had valid contact information at the start of EAT-IV recruitment, and 1,830 (66.1% of those with contact information) participated in the survey online or by mail. All participants with valid contact information were invited to participate, even if they had moved out of the state or country. The University of Minnesota Institutional Review Board approved the study protocol and all participants provided written informed consent.
Of 1,830 participants in Project EAT-IV, 99.3% (N=1,817) had complete information for the Nutrition Facts variable. Those with complete data on all dietary outcomes (N=1,367) did not differ from the larger sample on age or BMI category, but were more likely to be female, white, highly educated, high income, prepare food regularly, not single parents, and Nutrition Facts users compared to those with incomplete dietary data.
Survey Design
This cross-sectional analysis used data from Project EAT-IV, the fourth wave of a longitudinal cohort study. The Project EAT-IV survey was adapted from the original Project EAT survey21 and modified to ensure relevance for the current life stage of cohort participants using the life course perspective22 and formative focus groups with a separate sample of 35 young adults as a guide. Surveys assessed Nutrition Facts use, the frequency of looking at specific information on labels, sociodemographics, behavioral characteristics, and weight-related factors. Scale psychometric properties were examined in the full EAT-IV survey sample and estimates of item test-retest reliability, reported below, were determined in a subgroup of 103 participants who completed the EAT-IV survey twice within a period of one to four weeks. Dietary intake was assessed using a previously validated, semi-quantitative food frequency questionnaire.
Variables
Nutrition Facts use was assessed via a question modified from NHANES23: “How often do you use the Nutrition Facts panel (or other part of the food label: ingredient list, serving size information) before buying or choosing to eat a food product for the first time?” This was specifically adapted to ask “for the first time” to account for consumers who may use Nutrition Facts initially when choosing or purchasing a product, but not necessarily in subsequent purchases. Responses were listed on a 5-point Likert scale where 1=Never and 5=Always (test-retest r=0.83). For analysis, Nutrition Facts use was dichotomized similarly to a prior study24 by categorizing 4=Most of the time and 5=Always as being a label user, and all other responses (1–3) being considered label non-users.
Specific types of information of interest were assessed via a question adapted from NHANES23: “When you use the food label to decide about a food product, how often do you look for information about the following?” Total calories, calories from fat, total fat, trans fat, saturated fat, cholesterol, sodium, carbohydrates, fiber, sugars, serving size, and ingredient list were all then listed (test-retest ranging from 0.52 for cholesterol to 0.75 for sugars), and 5-point Likert scale responses were given for each where 1=Never and 5=Always. For analysis, each item was dichotomized by categorizing 4=Most of the time and 5=Always as looking at the information, and all other responses were considered as not looking at the information.
Food preparation was assessed via the question: “Who usually prepares food for your household? (Choose more than one if the task is split evenly.)” Those who selected “me” as an option were considered as preparing food regularly (test-retest agreement=91%).25 This item was skipped if participants indicated “I live alone” in response to an item in a prior question about living alone; thus, only participants who had reported not living alone and who answered this question directly were included in the analysis.
Moderate-to-vigorous physical activity (MVPA) was measured as a continuous variable using the Godin Leisure-Time Exercise Questionnaire26; the adapted questionnaire included relevant exercise examples and six response options ranging from 0 to 6 or more hours per week. This measure was validated against accelerometer-measured hours of activity in Project EAT-III (test-retest r=0.84).27
Height and weight were self-reported in feet and inches and pounds; BMI (body mass index) was calculated using the standard formula28; BMI<18.5 was considered underweight, BMI between 18.5 and 24.9 as normal weight, BMI between 25.0 and 29.9 as overweight, and BMI greater than 30 as obesity. A previous Project EAT study validated self-reported height and weight against objective measures, with correlations coefficients of 0.77–0.96.29 Weight goals were assessed by the question: “Are you currently trying to:” with possible answers of lose weight, stay the same weight, gain weight, and not trying to do anything about weight.
Sociodemographic Factors and Covariates
Gender, age, ethnicity/race, education, income, and living with a significant other or children in the past year were assessed via Project EAT survey measures20, 21 and reliability estimates have been previously reported30. Age was calculated using self-reported birth date and the survey completion date; for analysis, age was dichotomized into younger (ages 25–30) and older (ages 31–36). Education was assessed by the question: “what is the highest grade or year of school that you have completed?” (test-retest r=0.84). Household income was assessed by the question: “what was the total income of your household before taxes in the past year?” (test-retest r=0.94). Ethnicity/race was assessed by the question: “Do you think of yourself as white, black or African American, Hispanic or Latino, Asian-American, Hawaiian or Pacific Islander, or American Indian or Native American?, with respondents asked to check all that applied (k=0.70–0.83). Living with a significant other and children was assessed by the question: “During the past year, with whom did you live the majority of the time? (Mark all that apply); those who checked “my husband/wife”, “my partner of the opposite sex”, and “my partner of the same sex” were considered as living with a significant other, and those who checked “my child(ren), including any step-children or adopted children” were considered as living with children (percent agreement=100%).
Dietary Outcomes
Daily servings of fruits, vegetables, whole grains, fried potatoes, dairy, and sugar-sweetened beverages (i.e., sodas, sports drinks, punch, lemonade, sugared ice tea) were assessed using the Willett semi-quantitative food frequency questionnaire (FFQ).31 Daily servings were defined as one-half cup for fruits (excluding fruit juice) and vegetables (excluding French fries), 16 g for whole grains, and one cup for dairy. One serving of sugar-sweetened beverages was defined as the equivalent of one glass, bottle, or can. Protein was measured in grams.
Daily total energy intake (calories), fiber (grams), total fat (percent of total calories), saturated fat (percent of total calories), sodium (mg), and added sugars (percent of total calories) were also estimated from the FFQ. Nutrient intakes were developed based on a database from the Nutrition Questionnaire Service Center at the Harvard School of Public Health32, which utilized the United States Department of Agriculture’s Nutrient Database for Standard Reference. Reliability and validity of intake estimates is reported elsewhere.33, 34
Restaurant frequencies were assessed via questions asking participants how often they ate at different types of restaurants in the past month. This measure was adapted from a screener previously developed to assess restaurant use among adolescents.35 Restaurants listed included Traditional “burger-and-fries” fast food restaurant (such as McDonald’s or Wendy’s), Mexican fast food restaurant (such as Taco Bell or Chipotle), Fried Chicken (such as KFC), Sandwich or sub shop (such as Subway or Panera), Pizza place, Asian fast food restaurant (such as Panda Express) (test-retest ranging from r=0.52–0.71), Sit-down restaurant (where wait-staff brought food to the table) (test-retest r=0.73), or Other fast food or sit-down restaurant (with a blank listed to specify). Response categories included never/rarely (coded as 0 times), 1–3 times per month (coded as 2 times/month), 1–2 times per week (coded as 6 times/month), 3–4 times per week (coded as 14 times/month), 5–6 times per week (coded as 22 times/month), and 1 or more times per day (coded as 28 times/month). All restaurants excluding sit-down restaurants were grouped into a variable by summing the value of each individual variable, as a measure of frequency of eating any type of fast food in the past month. Reported fast food frequency ranged from 0–90 times per month.
Data analysis
Weighted chi-squared tests were used to examine differences in sociodemographic, behavioral, and weight-related characteristics by Nutrition Facts use. Since Nutrition Facts were used by almost a third of the study population, indicating that reading labels is relatively common, prevalence proportion ratios were used to cross-sectionally examine how demographic and behavioral factors (modeled as independent variables) were related to Nutrition Facts use. For predicting common outcomes, prevalence proportion ratios provide more conservative association estimates than odds ratios, which may overstate the prevalence proportion.36 Frequent Nutrition Facts use was defined as “most of the time” or “always.” Prevalence proportion ratios and confidence intervals were calculated from logistic regression using previously described methods.37, 38 Based on prior research in this cohort showing ethnic/racial differences in weight-related factors21, and broader research on socioeconomic and ethnic/racial disparities in health39, each model accounted for gender, age, ethnicity/race, education, and income. To reduce potential bias from related constructs, living situation, food preparation, physical activity, and weight status variables were analyzed in individual models.
Adjusted means accounting for gender, ethnicity/race, education, income, moderate-to-vigorous physical activity, and BMI were used to investigate how label use related to dietary outcomes (daily calories, servings of fruits, vegetables, whole grains, dairy, sugar-sweetened beverages, and monthly frequency of eating at fast-food and sit-down restaurants). Covariates were chosen based on putative or potential impact on dietary intake.20, 21, 40, 41 The response propensity method42 was used to weight data in all analyses since attrition did not occur randomly from the school-based sample. Response propensities, or likelihood of responding to EAT-IV, was estimated using a logistic regression of response at follow-up including predictor variables from EAT-I. The weighted sample was therefore more representative of and more generalizable to the adolescent population of the Minneapolis-St. Paul metropolitan area in 1998–1999. Descriptive statistics were used to examine the types of information used by those who reported looking at the Nutrition Facts label. All analyses were performed using SAS v. 9.4 (Cary, NC).43
RESULTS
Nutrition Facts prevalence and sample characteristics
The final weighted sample had a mean age of 31.0 ± 1.7 years and included 918 men and 887 women; 48.3% were white, 19.1% Asian American, 18.3% African American, 5.6% Hispanic, and 7.7% mixed or other. Participants had relatively high education and income; about a third had a high school degree or less, over a quarter had an associates or technical degree, and 43% had a bachelor’s degree or higher. For income, 44% had a household income of less than $50,000/year, 38% had an income between $50,000-$99,999/year, and 19% had income above $100,000/year. Almost a third (31.4%) of the sample reported using Nutrition Facts, which was defined as using them “most of the time” and “always” when buying or choosing a food product for the first time. Table 1 describes how the demographic and behavioral characteristics of young adults were related to Nutrition Facts use. Overall, unadjusted patterns showed that those who reported higher Nutrition Facts use were more likely to be female, white, have high education and income, prepare food regularly, engage in more hours of MVPA, have a weight status classified as overweight, and report wanting to lose weight.
Table 1.
Nutrition Facts usea by sociodemographic, weight-related, and behavioral characteristics in young adults (N = 1817).b
| Characteristics | % (n) | Label users % | Label non-users % | Unadjusted relative ratio, label usec |
|---|---|---|---|---|
| n = 567 (31.4) | n = 1239 (68.6) | |||
| Gender | ||||
| Men | 50.9 (918) | 26.1 | 73.9 | 1.00 (ref) |
| Women | 49.1 (887) | 36.9 | 63.1 | 1.17 (1.10, 1.25) |
| Age (years) | ||||
| 25–30 | 31.3 (566) | 32.8 | 67.2 | 1.00 (ref) |
| 31–36 | 68.7 (1240) | 30.7 | 69.3 | 0.97 (0.91, 1.04) |
| Ethnicity/race | ||||
| White | 48.3 (871) | 37.7 | 62.3 | 1.19 (1.12, 1.27) |
| Black | 18.3 (330) | 30.2 | 69.8 | 0.98 (0.91, 1.07) |
| Hispanic | 5.6 (101) | 25.7 | 74.3 | 0.92 (0.82, 1.04) |
| Asian | 19.1 (344) | 20.9 | 79.1 | 0.84 (0.78, 0.89) |
| Other | 7.7 (140) | 26.8 | 73.2 | 0.93 (0.84, 1.04) |
| Education | ||||
| High school graduate or less | 29.8 (536) | 20.7 | 79.3 | 0.81 (0.76, 0.86) |
| Associate/technical degree | 27.3 (492) | 29.2 | 70.9 | 0.95 (0.89, 1.02) |
| Bachelor degree or higher | 42.9 (772) | 40.5 | 59.5 | 1.27 (1.18, 1.35) |
| Income | ||||
| Low ($0–$49,999) | 43.6 (775) | 25.3 | 74.7 | 0.85 (0.80, 0.91) |
| Middle ($50,000–$99,999) | 37.5 (666) | 33.7 | 66.4 | 1.05 (0.98, 1.12) |
| High ($100,000+) | 18.9 (336) | 41.4 | 58.6 | 1.21 (1.10, 1.33) |
| Living situation | ||||
| Not living with children/SOd | 29.8 (538) | 30.1 | 69.9 | 0.97 (0.91, 1.04) |
| Living with SO, no children | 29.5 (532) | 35.4 | 64.6 | 1.09 (1.01, 1.17) |
| Living with SO and children | 34.9 (631) | 29.4 | 70.6 | 0.96 (0.90, 1.02) |
| Living with children, no SO | 5.8 (104) | 29.8 | 70.3 | 0.98 (0.86, 1.11) |
| Food preparation | ||||
| Does not prepare food regularly | 25.8 (413) | 21.9 | 78.1 | 1.00 (ref) |
| Prepares food at home regularly | 74.2 (1191) | 33.9 | 66.1 | 1.18 (1.11, 1.26) |
| Moderate-to-vigorous physical activity (mean hrs/wk, CI) | 100 (1817) | 5.2 (4.9, 5.5) | 3.9 (3.7, 4.1) | |
| Weight status | ||||
| Not overweight (<25 kg/m2) | 36.5 (645) | 33.0 | 67.0 | 1.03 (0.96, 1.10) |
| Overweight (25–29.99 kg/m2) | 33.0 (583) | 36.1 | 63.9 | 1.10 (1.03, 1.19) |
| Obesity (≥30 kg/m2) | 30.4 (537) | 25.3 | 74.7 | 0.88 (0.82, 0.94) |
| Weight goals | ||||
| Nothing in particular | 23.0 (415) | 20.1 | 79.9 | 0.81 (0.77, 0.87) |
| Lose weight | 51.9 (935) | 37.3 | 62.7 | 1.19 (1.12, 1.27) |
| Gain weight | 4.9 (88) | 26.5 | 73.5 | 0.93 (0.82, 1.06) |
| Stay the same weight | 20.2 (364) | 30.6 | 69.4 | 0.98 (0.91, 1.06) |
Nutrition Facts use was assessed via a question asking how often the participant used the Nutrition Facts panel when buying or eating a product for the first time.
Responses ranged from 1–5 where 1=Never and 5=Always; those responding “most of the time” and “always” were categorized as being frequent label users, and others as non-users.
Not all variable groups add up to 1817 participants due to missing data. All prevalence rates are weighted.
In the case of variables such as gender or age with two levels, the relative ratio compares the prevalence of Nutrition Facts use among the two groups (e.g. women compared to men). In the case of variables such as ethnicity/race with more than 2 levels, the relative ratio compares the prevalence of Nutrition Facts use among individuals in that group with those in all other groups (e.g. white vs. non-white).
SO = Significant Other
Correlates of Nutrition Facts use
In adjusted models, being a frequent Nutrition Facts user was again related to being female, higher education and income, preparing food regularly at home, engaging in more hours of MVPA, having a weight status classified as overweight, and having a specific weight goal (all p<0.05, see Table 2). Use was lower for the older age group (ages 31–36) and those of Asian ethnicity/race (both p<0.05). Factors that were strongly related to label use were desire to lose weight and high education. Desire to lose weight was associated with a 67% higher likelihood of Nutrition Facts use compared to not having a particular weight goal, and having a bachelor’s degree or higher was associated with a 58% higher likelihood of label use compared to low education.
Table 2.
Adjusted prevalence proportion ratios showing use of Nutrition Factsa by sociodemographic, weight-related, and behavioral factors in young adults (N = 1817).b
| Explanatory Variables | Prevalence Proportion Ratioc | Confidence Interval | P value |
|---|---|---|---|
| Gender | |||
| Men (ref.) | 1.00 | ||
| Women | 1.47 | 1.25, 1.77 | <0.001 |
| Age group | |||
| 25–30 (ref.) | 1.00 | ||
| 31–36 | 0.82 | 0.72, 0.93 | 0.003 |
| Ethnicity/race | |||
| White (ref.) | 1.00 | ||
| Black | 0.91 | 0.76, 1.09 | 0.320 |
| Asian | 0.57 | 0.45, 0.70 | <0.001 |
| Hispanic | 0.84 | 0.60, 1.13 | 0.277 |
| Other | 0.82 | 0.61, 1.06 | 0.136 |
| Education | |||
| High school graduate or less (ref.) | 1.00 | ||
| Associate/technical degree | 1.23 | 1.04, 1.44 | 0.016 |
| Bachelor degree or higher | 1.58 | 1.33, 1.89 | <.001 |
| Income | |||
| Low ($0–$49,999) (ref.) | 1.00 | ||
| Middle ($50,000–$99,999) | 1.20 | 1.04, 1.38 | 0.016 |
| High ($100,000+) | 1.31 | 1.10, 1.55 | 0.004 |
| Living situation | |||
| Not living with children/SO (ref.) | 1.00 | ||
| Living with SO, no children | 0.97 | 0.81, 1.15 | 0.728 |
| Living with SO and children | 0.85 | 0.71, 1.01 | 0.073 |
| Living with children, no SO | 0.94 | 0.68, 1.24 | 0.687 |
| Food Preparation | |||
| Does not prepare food regularly (ref.) | 1.00 | ||
| Prepares food at home regularly | 1.31 | 1.09, 1.60 | 0.003 |
| Moderate-to-vigorous physical activity (hrs/wk) | 1.07 | 1.05, 1.09 | <0.001 |
| Weight status | |||
| Non-overweight (ref.) | 1.00 | ||
| Overweight | 1.18 | 1.02, 1.37 | 0.025 |
| Obesity | 0.91 | 0.76, 1.07 | 0.256 |
| Weight goal | |||
| Nothing in particular (ref.) | 1.00 | ||
| Lose weight | 1.67 | 1.40, 1.99 | <0.001 |
| Stay the same | 1.36 | 1.14, 1.60 | 0.001 |
| Gain weight | 1.37 | 1.03, 1.73 | 0.036 |
Nutrition Facts use was assessed via a question asking how often the participant used the Nutrition Facts panel when buying or eating a product for the first time. Responses ranged from 1–5 where 1=Never and 5=Always; those responding “most of the time” and “always” were categorized as being frequent label users, and others as non-users.
Each model accounted for gender, age, ethnicity/race, education, and income. To reduce potential bias from correlated variables, weight status, weight goal, living situation, and health behavior variables were analyzed in individual models (e.g. Nutrition Facts use = gender + age + ethnicity/race + education + income + living situation + ε).
Since odds ratios may overestimate the prevalence proportion for common outcomes, prevalence proportion ratios were used to cross-sectionally examine how demographic and behavioral factors (modeled as independent variables) were related to Nutrition Facts use (modeled as dependent). Ratios and confidence intervals were calculated via logistic regression.
What Nutrition Facts users observe
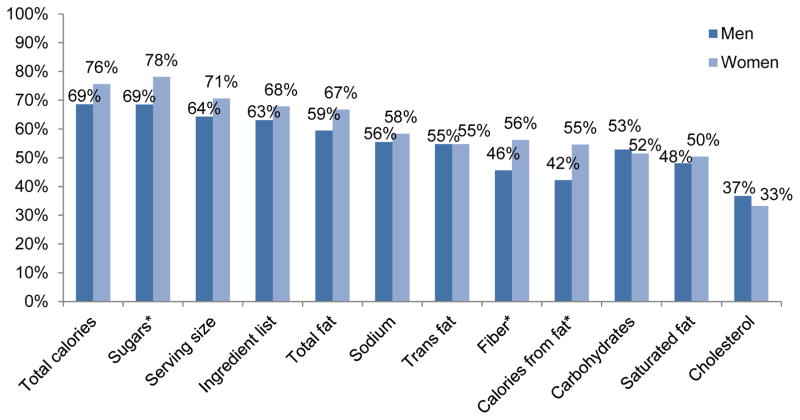
Overall, Nutrition Facts users reported looking at sugars (74.1%), total calories (72.9%), serving size (67.9%), and the ingredient list (65.8%) most often. Carbohydrates (52.1%), calories from fat (51.7%), saturated fat (49.4%), and cholesterol (34.7%) were observed by fewer Nutrition Facts users. Figure 1 shows the specific components of the Nutrition Facts panel that Nutrition Facts users reported observing, stratified by gender. Women were significantly more likely than men to look at information on sugars, fiber, and calories from fat.
Figure 1.
Percentage of Nutrition Facts users in the Project EAT-IV study (n ranges from 561–566 for each piece of dietary information) who reported using specific types of nutrition information on the label “most of the time” or “always”.
*indicates p<0.05 for the comparison between males and females
Associations with dietary intake
Table 3 describes observed associations between Nutrition Facts use and measures of dietary intake. Adjusted means showed Nutrition Facts use was related to eating more of healthful dietary components, including fruit, vegetables, whole grains, and fiber (all p<0.05). For example, Nutrition Facts users consumed almost one additional serving (1/2 cup) of vegetables per day than non-users. Compared to non-users, Nutrition Facts users also consumed a lower percentage of total calories from saturated fat, half the daily servings of sugar-sweetened beverages, three quarters the amount of added sugars, and fewer servings of fried potatoes (all p<0.05). Frequency of eating at restaurants also differed by label use; Nutrition Facts users reported eating at sit-down restaurants slightly more frequently than non-users, but ate at fast food restaurants less frequently than Nutrition Facts non-users (both p<0.05).
Table 3.
Adjusted dietary intake (mean servings/day, frequency) by Nutrition Facts use in young adults.a
|
|
||||
|---|---|---|---|---|
| Nutrition Facts Useb (mean ± SE) | ||||
|
| ||||
| Daily Dietary Outcomes | N | Label users | Non-users | p value |
| Fruit, excluding fruit juice (servings) | 1548 | 1.72 ± 0.13 | 1.46 ± 0.12 | 0.006 |
| Vegetables, excluding potatoes (servings) | 1548 | 3.80 ± 0.17 | 2.91 ± 0.16 | <0.001 |
| Whole grains (servings) | 1548 | 2.32 ± 0.14 | 1.94 ± 0.13 | <0.001 |
| Fried potatoes (servings) | 1534 | 0.12 ± 0.01 | 0.15 ± 0.01 | 0.002 |
| Dairy (servings) | 1548 | 1.37 ± 0.10 | 1.57 ± 0.10 | 0.007 |
| Protein (g) | 1548 | 91.2 ± 3.2 | 87.3 ± 2.98 | 0.121 |
| Sugar-sweetened beverages (servings) | 1547 | 0.29 ± 0.07 | 0.65 ± 0.06 | <0.001 |
| Fiber (gm) | 1514 | 0.51 ± 0.03 | 0.19 ± 0.03 | <0.001 |
| Saturated fat, % of total calories | 1548 | 10.9 ± 0.2 | 11.5 ± 0.2 | <0.001 |
| Sodium (mg) | 1548 | 2076 ± 75 | 2181 ± 69 | 0.064 |
| Added sugars, % of total calories | 1548 | 8.2 ± 0.5 | 11.1 ± 0.5 | <0.001 |
| Calories (Kcal) | 1548 | 1998 ± 65 | 2030 ± 59 | 0.519 |
|
| ||||
| Frequency in the past month | ||||
|
| ||||
| Fast-food frequency | 1759 | 12.2 ± 0.8 | 14.4 ± 0.7 | <0.001 |
| Sit-down restaurant frequency | 1757 | 2.4 ± 0.1 | 2.3 ± 0.1 | <0.001 |
Least squares means adjusted for gender, ethnicity/race, education, income, moderate-to-vigorous physical activity, and BMI.
Nutrition Facts use was assessed via a question asking how often the participant used the Nutrition Facts panel when buying or eating a product for the first time. Responses ranged from 1–5 where 1=Never and 5=Always; those responding “most of the time” and “always” were categorized as being frequent label users, and others as non-users.
DISCUSSION
The objectives of this study were to investigate the correlates of Nutrition Facts use, describe what label information is most often observed, and examine how label use related to dietary intake in a large population-based sample of young adults. Use was higher for women; for participants with a higher formal education and income; those who prepared food regularly at home; were physically active; had a weight status classified as overweight; and were trying to lose, gain, or maintain weight. Among Nutrition Facts users, men and women differed in terms of reported frequency of looking at specific label components; however, both men and women were most likely to look at total calories, sugars, and serving size. Nutrition Facts users differed from non-users across a variety of diet-related factors, such as consuming more vegetables, fewer added sugars, and eating less frequently at fast food restaurants.
The results of this study confirm and extend prior research showing that nutrition label use on packaged foods is higher for females1, 2, 44 and those with higher education5, 44 and income2, 5. Results on age have been mixed, with a few studies in young adult populations showing that older age is related to greater use13, 45, and one in adults showing that those 18–34 years old were less likely to use labels than those ages 35–54 or 55–855; other studies have found no association between age and label use12, 15. The Project EAT-IV sample only included young adults ages 25–36; thus, the finding that those in the 31–36-year-old age group used Nutrition Facts less frequently may be indicative of life situations that are more common in this age range, such as living with a significant other and/or children. The present study included a greater number of ethnic/racial groups than many prior studies in the US.5, 6, 16 In the adjusted analyses in Project EAT-IV, only young adults identifying as Asian American differed in terms of Nutrition Facts use, with a much lower prevalence of using labels compared to the reference group of white young adults. Notably, 40% of Asian American participants in this sample were born outside of the US, and over 62% self-identified as Hmong. The high proportion of immigrants and possibly refugees in this population subgroup may help to explain the finding that label use was substantially lower among Asian compared to white young adults. Many immigrants face substantial language and health literacy barriers46, and health literacy has been shown to differ by ethnicity/race and impact food label use in young adults45. Further, a prior study in this cohort found that compared to white participants, those of Hmong ethnicity were more involved in food purchasing and preparation while also reporting higher prevalence of dieting and unhealthy weight control practices47, suggesting that Hmong background may impact a variety of diet-related behaviors and practices.
Those living with both a significant other and child(ren) were marginally less likely to use Nutrition Facts compared to young adults living with neither a significant other nor child(ren). This somewhat aligns with previous research showing that individuals living alone were more likely to use Nutrition Facts compared to those in a household of more than one.5 However, the limited research on this topic has produced inconsistent findings.16, 48 The impact of parenthood on nutrition label use has rarely been studied; Kim, Imai, and Mathews49 reported that pregnant NHANES participants were more likely to use Nutrition Facts compared to non-pregnant counterparts after controlling for socioeconomic and perceived health and weight status. Understanding how parenthood and living situation impact label use is particularly important because previous studies have reported that parenthood may be related to poorer dietary behaviors50, 51, although other research has found that parents were more motivated to buy and prepare healthier foods52. Methods to make label use easy and understandable, such as providing front-of-pack labels53, have potential to improve Nutrition Facts use among this group. Supportive factors should also be further studied, particularly because of the strong influence that parents have on their own children’s dietary intake.10, 11
Higher moderate-to-vigorous physical activity was linked to greater Nutrition Facts use in this study, extending previous results showing that self-reported exercise was linked to label use.1, 54 Since healthy behaviors55 such as nutrition label use56 often cluster together, one potential way to increase label use might be to use engagement in physical activity or other healthy behaviors to promote label use. Particularly since men both have lower label use1, 2, 44 and higher activity levels57, leveraging Nutrition Facts as a way to ensure proper nutrient intake for physically active men could potentially promote healthier dietary patterns in a group that is motivated to be active but currently exhibits low label use.
Both overweight weight status and weight goals of wanting to lose, gain, or stay the same weight were related to higher Nutrition Facts use. No clear relationship between nutrition label use and weight status has been confirmed by prior research; while some studies have shown that nutrition label use was related to weight loss strategies6 and overweight54, 58, others have found no relationship between weight status and nutrition label use16, 59. Because there are many potential reasons for label use besides weight control, in future research it will be important to examine these variables in a comprehensive way, accounting for health, weight, and nutrition motivations. We found that Nutrition Facts use was more strongly related to weight goals than weight status in this sample, suggesting that label use may be more related to motivations rather than actual weight or physical characteristics. A notable concern when considering nutrition label use and weight status may be that of potential negative side effects among those with excessive weight concerns or at risk of eating disorders.60 Haynos and Roberto found that individuals with eating disorders were more likely to select fewer calories after exposure to menu labels61, and the potential impact of nutrition label use on body image, satisfaction, and healthy and unhealthy weight control behaviors should be further investigated.
Nutrition Facts users were most likely to report looking at sugars, total calories, serving size, and ingredient lists. These aspects are particularly poignant given the recent changes enacted by the FDA to highlight added sugars, enlarge total calories, and make serving sizes more reflective of servings sizes usually consumed62; the current study supports these aspects as highly desired and regularly used by Nutrition Facts users, with calories, sugars, and serving sizes being the most looked-at information. Since the survey for the present study was conducted prior to the 2016 FDA final rule concerning the Nutrition Facts label and because manufacturers are not yet required to comply, it is unlikely that participants were familiar with the new label. These results indicate that the FDA guidelines appear to align well with consumer preferences; however, consumer preferences and the impact of the newly-designed label should be tested using surveys and controlled trials, particularly those using objective measures of dietary intake. Additionally, use of interpretational aides and different label types such as front-of-pack53, exercise-equivalents63, or traffic light64 labels should be further tested, as these measures have shown promise at more effectively promoting healthier choices compared to simple textual calorie labels.
Nutrition Facts users reported eating differently than non-users on a number of different aspects, particularly in consuming more vegetables and fewer added sugars, and eating less frequently at fast food restaurants. This supports prior research in NHANES showing that sugar, fiber, and saturated and total fat differed among Nutrition Facts users5, although the present study did not find that daily energy intake differed. Notably, prior research has suggested that there may be qualitative differences in food choices of nutrition label users and non-users, such as increased vegetable and whole grain intake and healthier sides and beverages.24, 65 This study builds upon this research to show that in young adults, use of Nutrition Facts is related not only to factors present on Nutrition Facts labels, but also on dietary factors not included on labels, such as frequency of eating at fast food restaurants.
Strengths and limitations
This study had several strengths; first, it measured the relationship between Nutrition Facts use and rarely-studied characteristics including physical activity, meal preparation, and living with a significant other and children. Measuring these other behaviors and environmental factors are especially important when considering the contextual factors that likely impact dietary behaviors and routines. Second, this study included a comprehensive measure of dietary intake, including daily servings of relevant food groups and sugar-sweetened beverages, selected macro- and micronutrients, energy intake, and frequency of eating at fast-food and at sit-down restaurants. However, there were also several limitations. First, this study was cross-sectional, and was therefore unable to explore self-selection among Nutrition Facts users or the impact of using labels on long-term dietary intake. Second, although this study presented results from a large and diverse sample, participants were originally sampled from one geographic area and loss-to-follow-up was not completely at random; response weights were therefore used in analyses. The weighted sample was therefore more representative of and more generalizable to the adolescent population surveyed at baseline in the Minneapolis-St. Paul metropolitan area in 1998–1999. Last, this study used self-reported data for all measures including height, weight, sociodemographics, behavioral characteristics, and dietary intake.
CONCLUSIONS
Nutrition Facts use is associated with many positive dietary measures, but they are frequently used by only about a third of young adults. Future studies should focus on how and why consumers utilize the newly-designed Nutrition Facts panel, and investigate motivation to use labels and efficacy and acceptance of different label designs. Better understanding how nutrition label use might be leveraged with other related health behaviors, including physical activity and food preparation also has the potential to improve label use and dietary intake. Additionally, potential negative effects of nutrition label use on unhealthy weight control practices must be studied. More real-life studies measuring consumer use of labels while shopping for, preparing, and eating food are needed, particularly assessing how label use may relate to broad dietary outcomes.
RESEARCH SNAPSHOT.
Research question
What are the correlates of frequent Nutrition Facts use, what label information is most often used, and how does label use relate to dietary intake?
Key findings
In this cross-sectional study of 1817 young adults in Project EAT-IV, almost a third of participants used labels frequently; women and participants with specific weight goals and higher education were particularly likely to read labels. Label users looked at calories, sugars, and serving size most often. Label users and non-users differed on many dietary outcomes; label users reported consuming more vegetables, fewer added sugars, and eating less frequently at fast-food restaurants.
PRACTICE IMPLICATIONS.
What Is the Current Knowledge on this Topic?
Nutrition Facts label use is related to sociodemographic characteristics, and adults using Nutrition Facts seem to exhibit more positive dietary behaviors than those who do not use labels.
How Does this Research Add to Knowledge on this Topic?
This study extended previous work by showing in a young-adult population that specific weight goals and living with a significant other and children related to higher and marginally lower Nutrition Facts use, respectively. Men and women differed in observing specific items on labels, but both looked at calories, sugars, and serving size most often, seemingly aligning with the FDA’s recent updates to the Nutrition Facts label. Label users and non-users differed on many dietary outcomes, particularly consuming vegetables, added sugars, and eating at fast-food restaurants.
How Might this Knowledge Influence Current Dietetics Practice?
The Registered Dietitian Nutritionist should encourage Nutrition Facts use when choosing products and help support consumers in appropriately understanding this information. Young adults are an at-risk group undergoing transitions in dietary and health behaviors and habits. Individuals with low education, families with children, and males should particularly be supported and educated on label use and interpretation.
Acknowledgments
Funding: This study was supported by Grant Number R01HL116892 from the National Heart, Lung, and Blood Institute (PI: Dianne Neumark-Sztainer). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. M.J. Christoph is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under National Research Service Award (NRSA) in Primary Medical Care, grant no. T32HP22239 (PI: Borowsky). This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
The authors thank the Project EAT team and Jonathan Miller for feedback concerning the analysis and analytical methods.
Footnotes
Author Contributions: MJC conceptualized the study, performed the analysis, and drafted the manuscript. NL, ML, and DNS all reviewed, edited, and contributed to the proposal, analysis, and all manuscript drafts.
Conflict of interest disclosures: The authors report no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mary J Christoph, Postdoctoral Fellow, Division of General Pediatrics and Adolescent Health, University of Minnesota, 1300 2nd Street S., WBOB Suite 300, Minneapolis, MN, 55455, Phone: (612)-626-8984, Fax: (612)-626-7103.
Nicole Larson, Senior Research Associate, Division of Epidemiology and Community Health, University of Minnesota, 1300 2nd Street S., WBOB Suite 300, Minneapolis, MN 55414, Phone: (612)-625-5881, Fax: (612)-626-7103.
Melissa N. Laska, Associate Professor, Division of Epidemiology & Community Health, Director, Program in Public Health Nutrition, Co-Director, Obesity Prevention Center, University of Minnesota, 1300 2nd Street S., WBOB Suite 300, Minneapolis, MN 55454-1015, Phone: (612) 624-8832, Fax: (612) 624-0315.
Dianne Neumark-Sztainer, Professor and Division Head, Division of Epidemiology and Community Health, University of Minnesota, 1300 2nd Street S., WBOB Suite 300, Minneapolis, MN 55454, Phone: 612-624-0880, Fax: 612-626-7103.
References
- 1.Campos S, Doxey J, Hammond D. Nutrition labels on pre-packaged foods: a systematic review. Public Health Nutr. 2011;14:1496–1506. doi: 10.1017/S1368980010003290. [DOI] [PubMed] [Google Scholar]
- 2.Cowburn G, Stockley L. Consumer understanding and use of nutrition labelling: a systematic review. Public Health Nutr. 2007;8:21–28. doi: 10.1079/phn2005666. [DOI] [PubMed] [Google Scholar]
- 3.Nutrition Labeling and Education Act of 1990. HR 3562. Waxman HA, 1990.
- 4.U.S. Food and Drug Administration. Food Labeling: Revision of the Nutrition and Supplement Facts Labels. Final rule. 81 FR 33741. Published May 27, 2016. [PubMed] [Google Scholar]
- 5.Ollberding NJ, Wolf RL, Contento I. Food label Use and its relation to dietary intake among US Adults. J Am Diet Assoc. 2010;110:1233–1237. doi: 10.1016/j.jada.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Bleich SN, Wolfson JA. Differences in consumer use of food labels by weight loss strategies and demographic characteristics. BMC Public Health. 2015;15:1–8. doi: 10.1186/s12889-015-2651-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris KM, Gordon-Larsen P, Chantala K, Udry JR. Longitudinal trends in race/ethnic disparities in leading health indicators from adolescence to young adulthood. Arch Pediatr Adolesc Med. 2006;160:74–81. doi: 10.1001/archpedi.160.1.74. [DOI] [PubMed] [Google Scholar]
- 8.Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity. 2008;16:2205–2211. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- 9.Steffen LM, Van Horn L, Daviglus ML, et al. A modified Mediterranean diet score is associated with a lower risk of incident metabolic syndrome over 25 years among young adults: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Br J Nutr. 2014;112:1654–1661. doi: 10.1017/S0007114514002633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loth KA, MacLehose RF, Larson N, Berge JM, Neumark-Sztainer D. Food availability, modeling and restriction: How are these different aspects of the family eating environment related to adolescent dietary intake? Appetite. 2016;96:80–86. doi: 10.1016/j.appet.2015.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larsen JK, Hermans RC, Sleddens EF, Engels RC, Fisher JO, Kremers SP. How parental dietary behavior and food parenting practices affect children's dietary behavior. Interacting sources of influence? Appetite. 2015;89:246–257. doi: 10.1016/j.appet.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 12.Marietta AB, Welshimer KJ, Anderson SL. Knowledge, attitudes, and behaviors of college students regarding the 1990 Nutrition Labeling Education Act food labels. J Am Diet Assoc. 1999;99:445–449. doi: 10.1016/s0002-8223(99)00108-x. [DOI] [PubMed] [Google Scholar]
- 13.Misra R. Knowledge, attitudes, and label use among college students. J Am Diet Assoc. 2007;107:2130–2134. doi: 10.1016/j.jada.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Smith SC, Taylor JG, Stephen AM. Use of food labels and beliefs about diet - disease relationships among university students. Public Health Nutr. 2000;3:175–182. doi: 10.1017/s1368980000000203. [DOI] [PubMed] [Google Scholar]
- 15.Graham DJ, Laska MN. Nutrition label use partially mediates the relationship between attitude toward healthy eating and overall dietary quality among college students. J Acad Nutr Diet. 2012;112:414–418. doi: 10.1016/j.jada.2011.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li KK, Concepcion RY, Lee H, et al. An examination of sex differences in relation to the eating habits and nutrient intakes of university students. J Nutr Educ Behav. 2012;44:246–250. doi: 10.1016/j.jneb.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Cooke R, Papadaki A. Nutrition label use mediates the positive relationship between nutrition knowledge and attitudes towards healthy eating with dietary quality among university students in the UK. Appetite. 2014;83:297–303. doi: 10.1016/j.appet.2014.08.039. [DOI] [PubMed] [Google Scholar]
- 18.Jasti S, Kovacs S. Use of trans fat information on food labels and its determinants in a multiethnic college student population. J Nutr Educ Behav. 2010;42:307–314. doi: 10.1016/j.jneb.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015 – 2020 Dietary Guidelines for Americans. (8) 2015 Dec; Available at http://health.gov/dietaryguidelines/
- 20.Neumark-Sztainer D, Story M, Hannan PJ, Croll J. Overweight status and eating patterns among adolescents: where do youths stand in comparison with the Healthy People 2010 objectives? Am J Public Health. 2002;92:844–851. doi: 10.2105/ajph.92.5.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neumark-Sztainer D, Croll J, Story M, Hannan P, French S, Perry C. Ethnic/racial differences in weight-related concerns and behaviors among adolescent girls and boys: findings from Project EAT. J Psychosom Res. 2002:53. doi: 10.1016/s0022-3999(02)00486-5. [DOI] [PubMed] [Google Scholar]
- 22.Fine A, Kotelchuck M U.S. Department of Health and Human Services HRSA, Maternal and Child Health Bureau. Rethinking MCH: The life course model as an organizing framework. Version 1.12010. [Google Scholar]
- 23.Wojcicki JM, Heyman MB. Adolescent nutritional awareness and use of food labels: Results from the national nutrition health and examination survey. BMC Pediatr. 2012;12:55. doi: 10.1186/1471-2431-12-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Christoph MJ, Ellison B. A cross-sectional study of the relationship between nutrition label use and food selection, servings, and consumption in a university dining setting. J Acad Nutr Diet. 2017;117:1528–1537. doi: 10.1016/j.jand.2017.01.027. [DOI] [PubMed] [Google Scholar]
- 25.Harnack L, Story M, Martinson B, Neumark-Sztainer D, Stang J. Guess who's cooking? The role of men in meal planning, shopping, and preparation in US families. J Am Diet Assoc. 1998;98:995–1000. doi: 10.1016/S0002-8223(98)00228-4. [DOI] [PubMed] [Google Scholar]
- 26.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10:141–146. [PubMed] [Google Scholar]
- 27.Sirard JR, Hannan PJ, Cutler GJ, Graham DJ, Neumark-Sztainer D. Evaluation of two self-report measures of physical activity with accelerometry in young adults. J Phys Act Health. 2013;10:85–96. doi: 10.1123/jpah.10.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.US Centers for Disease Control and Prevention. Healthy weight: assessing your weight. Published May 15, 2015. [Google Scholar]
- 29.Himes JH, Hannan P, Wall M, Neumark-Sztainer D. Factors associated with errors in self-reports of stature, weight, and body mass index in Minnesota adolescents. Ann Epidemiol. 2005;15:272–278. doi: 10.1016/j.annepidem.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 30.Larson N, Neumark-Sztainer D, Story M, van den Berg P, Hannan PJ. Identifying correlates of young adults' weight behavior: survey development. Am J Health Behav. 2011;35:712–725. [PMC free article] [PubMed] [Google Scholar]
- 31.Hu FB, Rimm E, Smith-Warner SA, et al. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr. 1999;69:243–249. doi: 10.1093/ajcn/69.2.243. [DOI] [PubMed] [Google Scholar]
- 32.HSPH Nutrition Department’s File Download Site. Vol. 2017. Harvard School of Public Health Nutrition Department; [Google Scholar]
- 33.Feskanich D, Rimm EB, Giovannucci EL, et al. Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc. 1993;93:790–796. doi: 10.1016/0002-8223(93)91754-e. [DOI] [PubMed] [Google Scholar]
- 34.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol. 1992;135:1114–1136. doi: 10.1093/oxfordjournals.aje.a116211. [DOI] [PubMed] [Google Scholar]
- 35.Nelson MC, Lytle LA. Development and evaluation of a brief screener to estimate fast-food and beverage consumption among adolescents. J Am Diet Assoc. 2009;109:730–734. doi: 10.1016/j.jada.2008.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 37.Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43:962–970. doi: 10.1093/ije/dyu029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zou GY. Assessment of risks by predicting counterfactuals. Stat Med. 2009;28:3761–3781. doi: 10.1002/sim.3751. [DOI] [PubMed] [Google Scholar]
- 39.Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health. 2010:100. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed]
- 40.Donnelly JE, Herrmann SD, Lambourne K, Szabo AN, Honas JJ, Washburn RA. Does increased exercise or physical activity alter ad-libitum daily energy intake or macronutrient composition in healthy adults? A systematic review. PLoS ONE. 2014;9:e83498. doi: 10.1371/journal.pone.0083498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rolls BJ, Fedoroff IC, Guthrie JF. Gender differences in eating behavior and body weight regulation. Health Psychol. 1991;10:133–142. doi: 10.1037//0278-6133.10.2.133. [DOI] [PubMed] [Google Scholar]
- 42.Little R. Survey nonresponse adjustments for estimates of means. Int Stat Rev. 1986;54:139–157. [Google Scholar]
- 43.SAS Statistical Software [computer program] Cary, NC: SAS Institute, Inc; 2013. Vol Version 9.4. [Google Scholar]
- 44.Christoph MJ, An R, Ellison B. Correlates of nutrition label use among college students and young adults: a review. Public Health Nutr. 2016;19:2135–2148. doi: 10.1017/S1368980015003183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cha E, Kim KH, Lerner HM, et al. Health literacy, self-efficacy, food label use, and diet in young adults. Am J Health Behav. 2014;38:331–339. doi: 10.5993/AJHB.38.3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kreps GL, Sparks L. Meeting the health literacy needs of immigrant populations. Patient Educ Couns. 2008;71:328–332. doi: 10.1016/j.pec.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 47.Stang J, Kong A, Story M, Eisenberg ME, Neumark-Sztainer D. Food and weight-related patterns and behaviors of Hmong adolescents. J Am Diet Assoc. 2007;107:936–941. doi: 10.1016/j.jada.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 48.Blitstein JL, Evans WD. Use of Nutrition Facts panels among adults who make household food purchasing decisions. J Nutr Educ Behav. 2006;38:360–364. doi: 10.1016/j.jneb.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 49.Kim J, Imai S, Mathews H. Does pregnancy increase use and awareness of nutrition information in food labels? Matern Child Health J. 2017:1–9. doi: 10.1007/s10995-016-2245-0. [DOI] [PubMed]
- 50.Berge JM, Larson N, Bauer KW, Neumark-Sztainer D. Are parents of young children practicing healthy nutrition and physical activity behaviors? Pediatrics. 2011;127:881–887. doi: 10.1542/peds.2010-3218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Laroche HH, Hofer TP, Davis MM. Adult fat intake associated with the presence of children in households: findings from NHANES III. J Am Board Fam Med. 2007;20:9–15. doi: 10.3122/jabfm.2007.01.060085. [DOI] [PubMed] [Google Scholar]
- 52.Bassett-Gunter RL, Levy-Milne R, Naylor PJ, et al. Oh baby! Motivation for healthy eating during parenthood transitions: a longitudinal examination with a theory of planned behavior perspective. Int J Behav Nutr Phys Act. 2013;10:88. doi: 10.1186/1479-5868-10-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Graham DJ, Heidrick C, Hodgin K. Nutrition label viewing during a food-selection task: front-of-package labels vs Nutrition Facts labels. J Acad Nutr Diet. 2015;115:1636–1646. doi: 10.1016/j.jand.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 54.Christoph MJ, Ellison BD, Meador EN. The influence of nutrition label placement on awareness and use among college students in a dining hall setting. J Acad Nutr Diet. 2016;116:1395–1405. doi: 10.1016/j.jand.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 55.Laska MN, Pasch KE, Lust K, Story M, Ehlinger E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prev Sci. 2009;10:376–386. doi: 10.1007/s11121-009-0140-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim SY, Nayga RM, Capps O. The effect of food label use on nutrient intakes: an endogenous switching regression analysis. Journal of Agricultural and Resource Economics. 2000:215–231. [Google Scholar]
- 57.Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults' participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34:1996–2001. doi: 10.1097/00005768-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 58.Martinez OD, Roberto CA, Kim JH, Schwartz MB, Brownell KD. A Survey of undergraduate student perceptions and use of nutrition information labels in a university dining hall. Health Educ J. 2013;72:319–325. [Google Scholar]
- 59.Krukowski RA, Harvey-Berino J, Kolodinsky J, Narsana RT, DeSisto TP. Consumers may not use or understand calorie labeling in restaurants. J Am Diet Assoc. 2006;106:917–920. doi: 10.1016/j.jada.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 60.Laz TH, Rahman M, Berenson AB. Association of frequent use of food labels with weight loss behaviors among low-income reproductive-age women. J Am Coll Nutr. 2015;34:73–79. doi: 10.1080/07315724.2014.891957. [DOI] [PubMed] [Google Scholar]
- 61.Haynos AF, Roberto CA. The effects of restaurant menu calorie labeling on hypothetical meal choices of females with disordered eating. Int J Eat Disord. 2017;50:275–283. doi: 10.1002/eat.22675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.U.S. Food and Drug Administration. Changes to the Nutrition Facts Label. Available at https://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/LabelingNutrition/ucm385663.htm. Updated September 29, 2017.
- 63.Wolfson JA, Graham DJ, Bleich SN. Attention to Physical Activity-Equivalent Calorie Information on Nutrition Facts Labels: An Eye-Tracking Investigation. J Nutr Educ Behav. 2017;49:35–42. e31. doi: 10.1016/j.jneb.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 64.Roberto CA, Bragg MA, Seamans MJ, Mechulan RL, Novak N, Brownell KD. Evaluation of consumer understanding of different front-of-package nutrition labels, 2010–2011. Prev Chronic Dis. 2012;9:E149. doi: 10.5888/pcd9.120015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gruner J, Ohri-Vachaspati P. Food and beverage selection patterns among menu label users and nonusers: results from a cross-sectional study. J Acad Nutr Diet. 2017;117:929–936. doi: 10.1016/j.jand.2016.12.012. [DOI] [PubMed] [Google Scholar]