Abstract
In 2018, World Kidney Day (WKD) and International Women’s Day coincide. The WKD editorial focuses on women’s kidney health. The European Renal Association–European Dialysis and Transplant Association (ERA-EDTA) Registry Annual Report 2015 summary provides an excellent snapshot of renal replacement therapy (RRT) epidemiology and women in Europe. The WKD editorial reports a lower incidence of RRT in women in major registries and potential limitations to women’s access to transplantation. What is the situation in Europe? In Europe, the incidence of RRT is also lower in women: 38% of incident RRT patients are women. Does it represent milder chronic kidney disease (CKD) in women or barriers to RRT access? The question arises from the higher prevalence of CKD Stages G3–G5 in women than in men. However, in some European countries, such as Spain, non-dialysis CKD Stages G4–G5 is less frequent in women than in men, recapitulating the difference in RRT incidence. In the ERA-EDTA Registry, the incidence of transplantation as a first modality on Day 1 was slightly higher for women and survival on RRT was similar for women and men in the first 3 months, but an intergender gap favouring women increased as RRT vintage increased. However, women on RRT are worse off regarding survival when compared with women in the general population than men on RRT compared with men in the general population. In conclusion, the ERA-EDTA Registry Annual Report 2015 and European epidemiology data suggest a lower incidence of end-stage kidney disease in women, no gender differences in access to transplantation and better RRT survival in women.
Keywords: access to health care, chronic kidney disease, dialysis inequality, epidemiology, gender, mortality, public heath, transplantation
Introduction
Two years ago, upon publication of the European Renal Association–European Dialysis and Transplant Association (ERA-EDTA) Registry Annual Report 2012 [1], we commented on the inequalities in the incidence of renal replacement therapy (RRT) across different European countries [2]. Unfortunately, these inequalities persist in the Annual Report 2015 [3]. The incidence rates of RRT per million population (pmp) ranged from 24 (unadjusted) in Ukraine to 285 (adjusted) in Israel, a >10-fold difference. Both extremes are bad news: RRT may not be offered to all in need in some countries and prevention of end-stage renal disease (ESRD) may be facing hurdles in others.
This issue of the journal also contains the editorial written by an International Society of Nephrology World Kidney Day committee on women and kidney disease, in a year in which World Kidney Day (WKD) and International Women’s Day coincide [4]. The editorial focuses on women’s issues in the context of kidney disease across the globe, from unique risks for kidney diseases to pregnancy to access to and dosing of dialysis and/or transplantation. A key aspect is access to and results of RRT in women as compared with men. Specifically, it reports on the lower incidence of RRT in women than in men exemplified by statistics in Africa and Japan [5, 6] indicating that there are no explanations for this finding. One distinct possibility is that women are discriminated against when resources do not allow providing RRT to every person in need. Indeed, lack of access to RRT is the most frequent cause of death in ESRD patients worldwide [7]. It also reports that data from the USA, France, China and India indicate that women have lower kidney transplant rates than men, are less likely to be registered on national transplant waiting lists and have longer time from dialysis initiation to listing [4].
In Europe, the European Society of Paediatric Nephrology/ERA-EDTA Registry reported that girls have a 23% lower probability of receiving pre-emptive transplantation than boys [4, 8]. Despite a faster progression towards ESRD in girls than in boys overall, medical factors explained only 70% of the gender difference [8]. This begs several questions. What is the situation among European women overall? Is the incidence of RRT different in men and women in Europe? Are there country-specific differences? If they do exist, are they due to a decreased incidence or progression rate of chronic kidney disease (CKD) in women or to barriers to RRT access in women? Is access to transplantation lower in European women than in European men? Are RRT outcomes different in European women and men?
Incidence and prevalence of RRT in Europe by gender
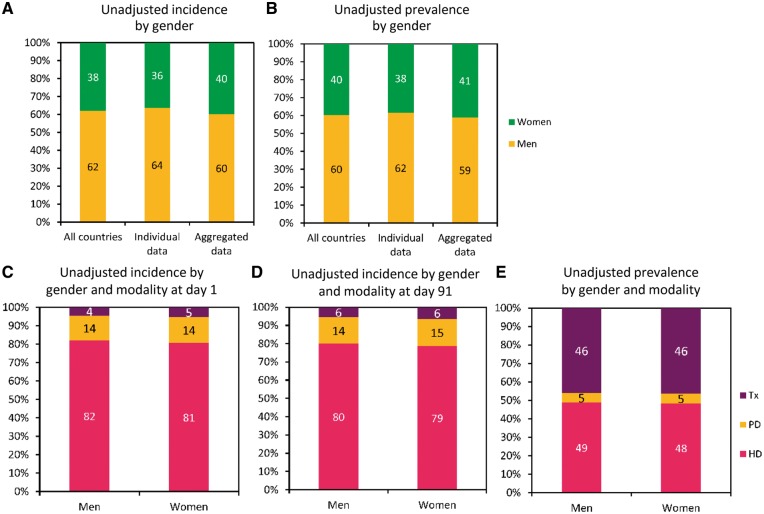
Data on the incidence of RRT in Europe confirm African, Japanese and US Renal Data System (USRDS) 2017 data [4, 9] of a lower incidence of RRT in women (Figure 1A). In Europe, 38% (unadjusted) of incident RRT patients in 2015 were women, while in the USA 42% were women in 2016 [3, 9]. The gender distribution of unadjusted prevalence in Europe was similar to the incidence data, with 40% of prevalent patients being women (Figure 1B). Are women discriminated against in RRT access in Europe?
Fig. 1.
Unadjusted incidence and prevalence of RRT by gender, according to the ERA-EDTA Registry Annual Report 2015. (A) Incidence of RRT (%). (B) Prevalence of RRT (%). (C) Incidence (%) of treatment modality at Day 1. (D) Incidence (%) of treatment modality at Day 91. (E) Prevalence (%) of established therapy. (C–E) Based on data from registries providing individual patient data as reported in Kramer et al. [3]. Reproduced with permission of Kramer et al.
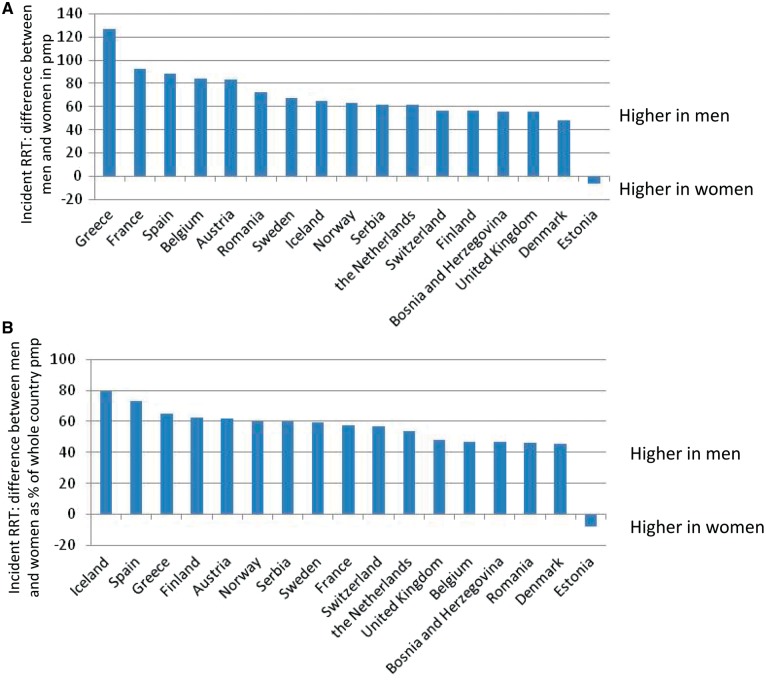
Access to the more detailed information in the full ERA-EDTA Registry Annual Report 2015 provides some additional clues. In most individual countries, the adjusted incidence of RRT was lower in women than in men and the gap ranged from 48 (Denmark) to 127 (Greece) pmp (Figure 2A) [10]. The only exception was Estonia, a country where a total of 114 patients started RRT in 2015. In relative terms, the absolute pmp gap represented 45% (Denmark) to 80% (Iceland) of the total adjusted RRT incidence in pmp, except for Estonia (Figure 2B). When expressed in relative terms, the figures are quite consistent across European countries with different cultures, socio-economic levels, health care systems and absolute incidence of RRT. Available data from countries not providing individualized data showed similar trends, with the exception of the Sfax region of Tunisia, where the incident rates pmp at Day 1, adjusted for age and gender, were high and very similar for men (241 pmp) and women (231 pmp). Again, in this region the total number of persons initiating RRT was relatively low (193 persons). In adults, the lower incidence of RRT in women is consistent across age ranges and countries, with only a handful of exceptions that could be related to the low number of patients in these categories (n < 25 per gender and age range: Estonia, 20–44 and 65–74 years; Castilla–Leon and Northern Ireland, 20–44 years) [10]. Thus gender differences on RRT incidence exist: they are consistent across countries and regions with different cultures, health care systems, gross domestic product and absolute incidence of RRT and are independent of age. In this regard, there is wide variability in the differences between women and men at the age of RRT initiation [10]. The age gap ranges from a median of 4 years older in women in French-speaking Belgium to a younger age in women in Scandinavian countries (Iceland, Finland, Sweden, Norway and Denmark), which is up to 3 years younger in women than in men. The reasons for these differences and regional clustering in Scandinavia should be explored, but the fact that these differences exist argue against systemic discrimination based on a woman's age regarding access to RRT.
Fig. 2.
Differences between men and women in incident rates of RRT at Day 1, adjusted for age and gender, according to the ERA-EDTA Registry Annual Report 2015 [10]. (A) Difference in the incidence of RRT between men and women expressed in pmp (men pmp − women pmp). (B) Difference in the incidence of RRT between men and women expressed as a percentage of the whole country (men and women) pmp {100 × [(men pmp − women pmp)/(all pmp)]}. Data from countries and regions providing individualized data. For countries not providing whole-country data (Spain, Belgium), the mean value of the different regions was calculated.
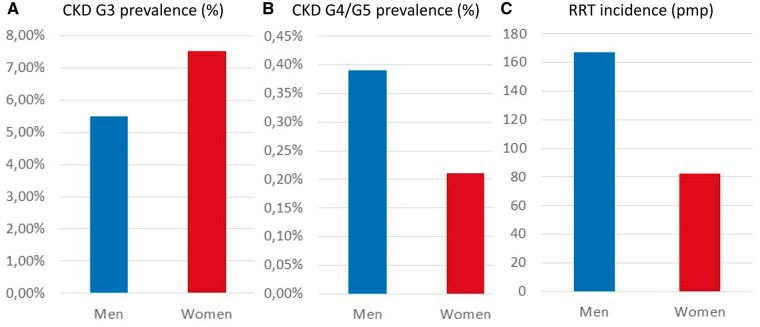
Beyond gender-based discrimination in access to RRT, gender differences in the prevalence and severity of CKD or response to therapy may also account for the lower incidence of RRT in women. As editorialized, certain kidney diseases, such as lupus nephritis, are more common in women [4]. However, what is known about gender differences in the overall prevalence of CKD in Europe? A recent manuscript collected epidemiological information on CKD in Europe [11]. The prevalence of CKD Stages G3–G5 was higher in European women [11], consistent with worldwide data showing a higher prevalence of CKD Stages G1–G5 and G3–G5 in women than in men [12]. These data may be interpreted as consistent with the existence of bias against providing RRT to women. However, analysis of available European data from countries with free, unlimited access to both primary and specialty care, such as Spain, provided additional information and clues [13]. While the 2004–8 Spanish epidemiological study confirmed the higher prevalence of CKD Stages G3–G5 in women than in men (7.71% versus 5.88%) of the general adult population, it also showed that severe CKD, that is, Stages G4–G5, are less frequent in women (0.21% versus 0.39%) (Figure 3A and B) [13]. This is consistent with the reported incidence of RRT in Spain in 2015 of 82 and 167 pmp for women and men, respectively (Figure 3C) [14].
Fig. 3.
Prevalence of different CKD categories and incidence of RRT by gender in Spain. Prevalence of CKD categories (A) G3 and (B) G4/G5 according to the 2004–8 EPIRCE Spanish epidemiological study of the adult general population [13]. (C) Incidence of RRT in 2015 in Spain according to gender [14].
There are several potential explanations for the divergent epidemiology of CKD Stages G3–G5, representing mainly Stage G3, and of Stage G4–G5 in Spain, which should be explored. They include different rates of progression in women and men, either spontaneously or as a consequence of therapeutic intervention or of dietary or health habits. In this regard, gender differences for the rate of CKD progression have been described. A recent review concluded that among higher-income countries, gender differences in the ESRD population require further study [15]. This echoed a meta-analysis of 68 published studies disclosing that men with non-diabetic CKD have a faster loss of glomerular filtration rate than women [16]. Similar results were obtained when diabetics and non-diabetics were included and progression from CKD Stages G3–G5 to ESRD was assessed [17]. Autosomal dominant polycystic kidney disease is influenced by gender [18]. Kidney cysts and loss of kidney function progress faster in men and liver cysts progress faster in women. In contrast, there are contradictory data for gender-specific progression of diabetic kidney disease [19]. Male sex has been associated with faster progression, although the impact is not as strong as in non-diabetic CKD [19]. In a recent meta-analysis of data from >5 million persons, women had a higher risk of ESRD, leading the authors to assume that women may have an accelerated progression of CKD [20].
The ERA-EDTA Registry does not provide a breakdown of causes of RRT by gender. This is an opportunity for further research that would allow understanding whether gender differences in RRT incidence are limited to one or several causes.
Access to transplantation in Europe by gender
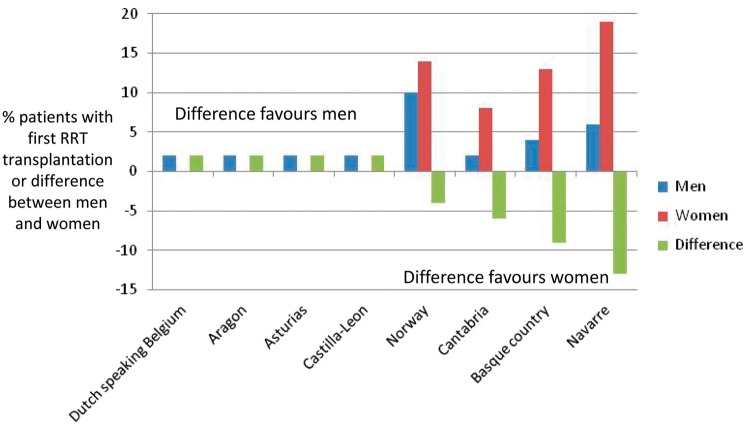
In USRDS 2017 data [9], there was a slightly lower incidence of transplantation as a percentage of RRT modalities in women (2.4%) than in men (2.6%). However, the situation was different in European countries providing individualized data. The unadjusted incidence of modality at Day 1 suggested a slight predominance of women having transplantation as the first modality (Figure 1C) [3]. Treatment modality at Day 1 also displayed large country-to-country differences. However, among countries that provided individual data, no systematic bias against transplantation first in women was apparent in any specific country [10]. An assessment of individual countries or regions with the largest gender gap in the percentage of patients on transplantation as a first therapy disclosed a number of regions with large gaps favouring women, ranging from a 4% difference in Norway to a 6–13% difference in the Spanish regions of Navarre, Basque country and Cantabria, while in regions where transplantation first favoured men, the difference did not exceed 2% (Figure 4). By Day 91, gender differences in transplantation could no longer be appreciated in the whole population (Figure 1D), as was the case for the prevalence of transplantation (Figure 1E).
Fig. 4.
Percentage of patients with first treatment modality transplantation unadjusted at Day 1, according to the ERA-EDTA Registry Annual Report 2015 [10]. The top four countries or regions with the largest differences favouring either women or men are depicted. Data from countries and regions providing individualized data. The small number of patients in some regions adds a caution note to interpretation of the data.
Gender and survival on RRT
The WKD editorial remarks that mortality rates are similar in men and women on dialysis, but the incident rates of some dialysis-associated complications and morbidity are higher in women, including hospitalization rates, 30-day readmissions, anaemia, nutrition and quality of life issues, while the prevalence of arteriovenous fistula was lower among women than men on haemodialysis [3, 21–23]. Furthermore, evaluation of the dialysis dose by Kt/Vurea may result in underdialysis in women [3, 24]. Despite the negative odds associated with these features, survival for women on RRT in Europe was similar to men for the first 3 months but was higher from then on, and increasing RRT vintage was associated with a widening survival gap favouring women (Figure 5) [10]. However, as compared with the general population, the gap in life expectancy between sexes at any age range was considerably shorter in persons on RRT. Thus survival on RRT was better in women, but women on RRT are worse off when compared with women in the general population than when men on RRT are compared with men in the general population [10]. Thus a wider margin for improvement in survival exists for women than for men on RRT.
Fig. 5.
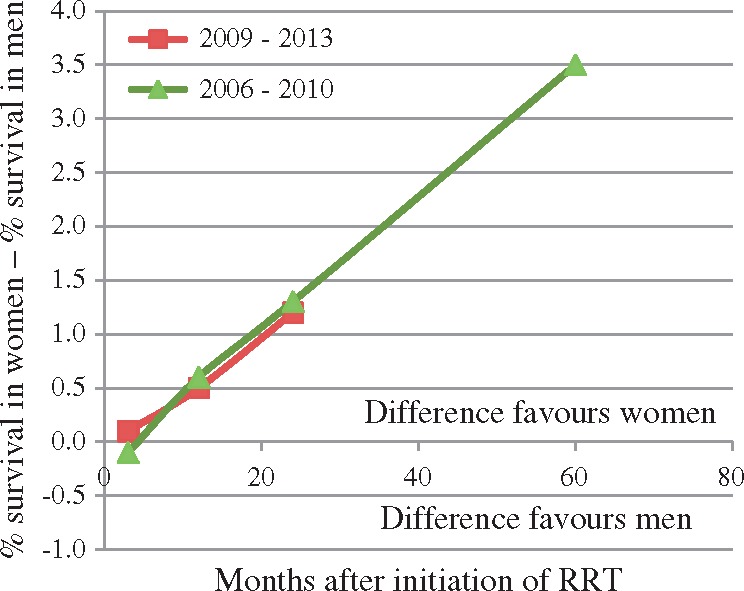
Difference in survival probability between men and women expressed as a percentage survival difference over time in incident RRT patients from Day 1, adjusted for age, gender and primary renal disease, according to the ERA-EDTA Registry Annual Report 2015 [10]. Data from countries and regions providing individualized data.
Limitations of ERA-EDTA Registry data
The ERA-EDTA Registry continues to have a number of limitations, including blackouts from large countries such as Germany and large parts of Italy [2, 3]. Additionally, some countries or regions do not provide individualized data so some epidemiological gender-related features could not be appropriately explored in those countries. The possibility of a systematic bias arises and data from countries providing individualized data may not apply to countries not providing those data. Thus large swaths of Eastern Europe do not provide individualized data and they include some of the countries with the lowest incidence of RRT, such as Ukraine, Russia and Belarus.
Conclusion
In conclusion, the ERA-EDTA Registry is a key resource to explore potential gender differences in the incidence of and access to RRT. The lower incidence of RRT in European women compared with men may be caused by a slower progression of CKD. If this is so, the contributing factors should be unraveled as they may provide clues to improve CKD outcomes across the board. This may be related not only to sex hormones, but also to other factors such as compliance with diet, medication or healthy living standards. In support of this hypothesis, at least for Spain, the gender epidemiology of CKD Stages G4–G5 is similar to the gender epidemiology of RRT incidence. Alternatively, limitations in access to RRT may exist for women. Regarding access to transplantation for European countries providing individualized data to the ERA-EDTA Registry, and this may represent a bias, no differences were observed in access to transplantation as a first RRT modality or in the prevalence of transplantation between men and women. Finally, despite the better survival of European women on RRT as compared with men, RRT has a greater adverse impact on survival for women than for men and research should focus on how to improve outcomes of women on RRT.
Funding
Funding was provided by grant support from the ISCIII and FEDER funds (PI16/02057), Sociedad Española de Nefrologia, ISCIII-RETIC REDinREN RD016/009, Joan Rodes (to BFF), Comunidad de Madrid CIFRA2 B2017/BMD-3686.
Conflict of interest statement
None declared.
References
- 1. Pippias M, Stel VS, Abad Diez JM. et al. Renal replacement therapy in Europe: a summary of the 2012 ERA-EDTA Registry Annual Report. Clin Kidney J 2015; 8: 248–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gonzalez-Espinoza L, Ortiz A.. 2012 ERA-EDTA Registry Annual Report: cautious optimism on outcomes, concern about persistent inequalities and data black-outs. Clin Kidney J 2015; 8: 243–247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kramer A, Pippias M, Noordzij M. et al. The European Renal Association – European Dialysis and Transplant Association (ERA-EDTA) Registry Annual Report 2015: a summary. Clin Kidney J 2018; 11: 108--122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Piccoli GB, Alrukhaimi M, Liu Z-H. et al. Women and kidney disease: reflections on World Kidney Day 2018. Clin Kidney J 2018; 11: 7--11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Saran R, Robinson B, Abbott KC. et al. US Renal Data System 2016 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2017; 69(3 Suppl 1): A7–A8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Halle MP, Takongue C, Kengne AP. et al. Epidemiological profile of patients with end stage renal disease in a referral hospital in Cameroon. BMC Nephrol 2015; 16: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ortiz A, Covic A, Fliser D. et al. Epidemiology, contributors to, and clinical trials of mortality risk in chronic kidney failure. Lancet 2014; 383: 1831–1843 [DOI] [PubMed] [Google Scholar]
- 8. Hogan J, Couchoud C, Bonthuis M. et al. Gender disparities in access to pediatric renal transplantation in Europe: data from the ESPN/ERA-EDTA Registry. Am J Transplant 2016; 16: 2097–2105 [DOI] [PubMed] [Google Scholar]
- 9. https://www.usrds.org/2017/view/Default.aspx (7 December 2017, date last accessed)
- 10. https://www.era-edta-reg.org/files/annualreports/pdf/AnnRep2015.pdf (7 December 2017, date last accessed)
- 11. Brück K, Stel VS, Gambaro G. et al. CKD prevalence varies across the European general population. J Am Soc Nephrol 2016; 27: 2135–2147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mills KT, Xu Y, Zhang W. et al. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int 2015; 88: 950–957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Otero A, de Francisco A, Gayoso P. et al. Prevalence of chronic renal disease in Spain: results of the EPIRCE study. Nefrologia 2010; 30: 78–86 [DOI] [PubMed] [Google Scholar]
- 14. http://www.senefro.org/contents/webstructure/reerOviedo2016.pdf (11 December 2017, date last accessed)
- 15. Carrero J-J, Hecking M, Ulasi I. et al. Chronic kidney disease, gender, and access to care: a global perspective. Semin Nephrol 2017; 37: 296–308 [DOI] [PubMed] [Google Scholar]
- 16. Neugarten J, Acharya A, Silbiger SR.. Effect of gender on the progression of nondiabetic renal disease: a meta-analysis. J Am Soc Nephrol 2000; 11: 319–329 [DOI] [PubMed] [Google Scholar]
- 17. Tsai W-C, Wu H-Y, Peng Y-S. et al. Risk factors for development and progression of chronic kidney disease: a systematic review and exploratory meta-analysis. Medicine 2016; 95: e3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gansevoort RT, Arici M, Benzing T. et al. Recommendations for the use of tolvaptan in autosomal dominant polycystic kidney disease: a position statement on behalf of the ERA-EDTA Working Groups on Inherited Kidney Disorders and European Renal Best Practice. Nephrol Dial Transplant 2016; 31: 337–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maric C. Sex, diabetes and the kidney. Am J Physiol Renal Physiol 2009; 296: F680–F688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shen Y, Cai R, Sun J. et al. Diabetes mellitus as a risk factor for incident chronic kidney disease and end-stage renal disease in women compared with men: a systematic review and meta-analysis. Endocrine 2017; 55: 66–76 [DOI] [PubMed] [Google Scholar]
- 21. Sehgal AR. Outcomes of renal replacement therapy among blacks and women. Am J Kidney Dis 2000; 35(Suppl): S148–S152 [DOI] [PubMed] [Google Scholar]
- 22. Adams SV, Rivara M, Streja E. et al. Sex differences in hospitalizations with maintenance hemodialysis. J Am Soc Nephrol 2017; 28: 2721–2728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ethier J, Mendelssohn DC, Elder SJ. et al. Vascular access use and outcomes: an international perspective from the dialysis outcomes and practice patterns study. Nephrol Dial Transplant 2008; 23: 3219–3226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Depner TA. Prescribing hemodialysis: the role of gender. Adv Ren Replace Ther 2003; 10: 71–77 [DOI] [PubMed] [Google Scholar]