Abstract
Background:
Scarring airway stenosis is commonly seen in China as compared to other developed countries, due to the high prevalence of tuberculosis. Nowadays, interventional bronchoscopy treatment has been widely used to treat this disease in China. This study demonstrated the characteristics of scarring airway stenosis in Chinese adults and retrospectively evaluated the efficacy of interventional bronchoscopy treatment of this disease.
Methods:
Patients with scarring airway stenosis from 18 tertiary hospitals were enrolled between January 2013 and June 2016. The causes, site, and length of scarring airway stenosis were analyzed, and the efficacy of the interventional bronchoscopy treatment was evaluated.
Results:
The final study cohort consisted of 392 patients. Endotracheobronchial tuberculosis (EBTB) was the most common cause of scarring airway stenosis (305/392, 77.8%) in Chinese adults with a high rate of incidence in young women. The left main bronchus was most susceptible to EBTB, and most posttuberculosis airway scarring stenosis length was 1.1–2.0 cm. The average clinical success rate of interventional bronchoscopy treatment for scarring airway stenosis in Chinese patients is 60.5%. The stent was inserted in 8.7% scarring airway stenosis in China.
Conclusions:
Scarring airway stenosis exhibits specific characteristics in Chinese patients. Interventional bronchoscopy is a useful and safe treatment method for the disease.
Keywords: Adults, Airway Stenosis, Bronchoscopy, Endotracheobronchial Tuberculosis, Stents
INTRODUCTION
Scarring airway stenosis, which is the benign type of airway stenosis,[1] is not a common disease in developed countries; postintubation stenosis, burn injuries, and secondary healing after surgery are the typical causes.[1] However, scarring airway stenosis with specific characteristics is commonly observed in China because of the high prevalence of tuberculosis.
For scarring airway stenosis, surgical resection was previously the gold standard;[2] however, interventional bronchoscopy treatments, such as balloon dilation, cryotherapy, laser therapy, and silicone stenting, have now been widely used to treat the disease,[3,4] benefitting a large number of patients. In this study, we demonstrated the characteristics of scarring airway stenosis in Chinese adults and retrospectively evaluated the efficacy of interventional bronchoscopy treatment of this disease.
METHODS
Ethical approval
The Institutional Review Board of Beijing Tian Tan Hospital, Capital Medical University, approved this study (Approval ID: JS2013-007-02), and the institutional review board of each hospital approved the analysis of clinical and radiological data of patients.
Patients
A retrospective study was conducted by Beijing Tian Tan Hospital, Capital Medical University. Scarring airway stenosis patients from 18 tertiary hospitals who underwent interventional bronchoscopy treatment were admitted between January 2013 and June 2016.
The interventional bronchoscopy treatment indications for scarring airway stenosis patients were those who could not receive surgery or those who could receive surgery but refused and prefer interventional bronchoscopy treatment.
The study excluded patients who were followed up for <3 months after the last interventional bronchoscopy treatment or lost to follow-up after treatment. Children and adolescents <18-year-old were also excluded from the study.
Evaluation methods
Location of stenosis
The stenosis sites were divided into 5 locations: (I) trachea, (II) left main bronchus, (III) right main bronchus, (IV) right middle bronchus, and (V) lobe bronchus.
Type of stenosis
In the article “A Proposed Classification System of Central Airway Stenosis” from Freitag et al., there are two major groups of stenosis: structural and dynamic (functional).[1] According to this classification, scarring airway stenosis in this study was also divided into two groups. The structural group includes all those in which shrinking and scarring predominate. Other stenoses caused by exophytic or intraluminal benign or malignant tumors; extrinsic compression; and distortion, kinking, bending, or buckling are all excluded. The dynamic group are malacic conditions of scarring airway stenosis, including those in which the cartilages are damaged.
Assessment of airway stenosis degree
The airway stenosis was described according to the Myer–Cotton stenosis grading system.[5,6] The classification is based on the cross-sectional area of the stenosis and divided into four grades: Grade I lesions have <50% obstruction, Grade II lesions have 51–70% obstruction, Grade III lesions have 71–99% obstruction, and Grade IV lesions have no detectable lumen or complete stenosis.
Assessment of the length of scarring airway stenosis
Chest contrast-enhanced computed tomography (CT) with 1.25 mm collimation, including transverse and coronal planes, was performed on all patients to assess the length of scarring airway stenosis. The length of scarring airway stenosis = number of layers from the proximal to distal regions of airway stenosis × 1.25 mm.
Assessment of dyspnea index
Patients' dyspnea index at baseline and after interventional bronchoscopy treatment was assessed. The Medical Research Council (MRC) Dyspnea Scale was used for assessing the dyspneic extent of airway stenosis patient (Grade 1, breathlessness upon strenuous exercise; Grade 2, hurrying on the elevation or a slight hill; Grade 3, walking slower than individuals of the same age because of breathlessness or having to stop for breath even while walking at own pace; Grade 4, having to stop after walking <100 m or after a few minutes; and Grade 5, breathlessness prevents leaving the house or while dressing).
The criteria to decide on interventional bronchoscopy treatment modalities
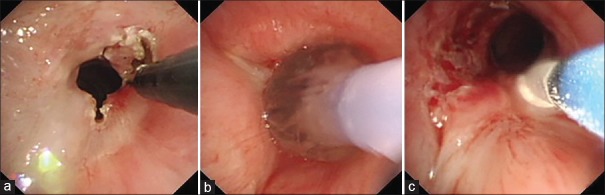
The interventional bronchoscopy treatment modalities included electronic knife or laser cutting, balloon dilation, cryotherapy, and stent insertion. According to the location, type, degree, and length of airway stenosis, the treatment of scarring airway stenosis usually needs to combine 2 or 3 modalities. In general, for structural scarring airway stenosis, electronic knife or laser was used first to release scar tissue [Figure 1a], then balloon dilation was done to expand the stenosis segment [Figure 1b], and cryotherapy was given at last to reduce the restenosis of scar [Figure 1c]. If all these treatments failed, stent insertion would be done. For dynamic scarring airway stenosis, because of the damage of cartilage, airway patency usually could not be maintained after using those interventional bronchoscopy methods mentioned above; thus, stent (including T tube) had to be used. Stent removal would be attempted on stable cases or cases with severe stent-related complications.
Figure 1.
Interventional bronchoscopy treatment for structural scarring airway stenosis. a: Scar tissue was released by electrical knife. b: Balloon dilation was done to expand the stenosis segement. c: Cryotherapy was done to reduce the restenosis of scar.
Assessment of efficacy
Efficacy was defined as the improvement in dyspnea index and/or decrease of airway stenosis grading. Invalidation was defined as no improvement in dyspnea index and no reduction in the grading of airway stenosis.
Follow-up and study endpoint
All patients underwent bronchoscopy examination 2–4 weeks after first interventional bronchoscopy treatment for the evaluation of the treatment effect. If the bronchoscopy treatment was effective, it would be continued, and clinical success was defined as the absence of an identified airway restenosis after three times continuous bronchoscopy examination (stable course).
If the bronchoscopy treatment was invalidated after first intervention, another two attempts were made. If the treatment proved to be effective after three repeated interventions, it would be continued. However, if it persistently failed after three repeated attempts, the bronchoscopy treatment would be stopped and patients would be recommended for surgical treatment or tracheotomy. The bronchoscopy treatment effect was defined as a clinical failure.
If severe bronchoscopy-related complications such as life-threatening bleeding occurred during the repeated therapeutic bronchoscopy, the treatment would be ceased and the effect defined as a clinical failure. For patients received stent insertion, if stent-related complications which could not be handled by interventional bronchoscopy treatment occurred, such as severe granulation tissue formation or repeated migration, stent would be removed and the effect also defined as a clinical failure.
Statistical analysis
Statistical analysis was conducted using SPSS software (version 12.0; SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to tabulate the demographic characteristics of the study population. All data are presented as mean ± standard deviation (SD).
RESULTS
Baseline characteristics of the study participants
The final study cohort consisted of 392 patients (106 males and 286 females) ranging in age from 18 to 83 years (median, 28 years).
The causes of the scarring airway stenosis were endotracheobronchial tuberculosis (EBTB) (n = 305, 77.8%), stenosis after intubation (n = 53, 13.5%), stenosis after tracheostomy (n = 19, 4.8%), anastomotic stenosis after surgical resection (n = 8, 2.0%), radiation-induced scarring stenosis (n = 4, 1.0%), and stenosis after trauma (n = 3, 0.8%).
Characteristics of endotracheobronchial tuberculosis scarring airway stenosis in Chinese adults
The cohort consisted of 305 patients (265 females and 50 males) ranging in age from 18 to 67 years (median, 27 years).
The localization of posttuberculosis scarring airway stenosis is summarized in this study. The stenosis involved trachea in 18 patients (5.9%), left main bronchus in 212 (69.5%), right main bronchus in 37 (12.1%), right middle bronchus in 32 (10.5%), and the lobe bronchus in 6 (2.0%).
With respect to the type of stenosis, the structure stenosis is in 270 cases (88.5%), and the dynamic stenosis is in 35 cases (11.5%). These 35 dynamic stenosis cases who could not be evaluated for stenosis length by preoperative CT scan due to complete airway occlusion or collapse were excluded, and the regions of 270 structure stenosis were available for the analysis of stenosis length. The average stenosis length is 1.6 ± 0.8 cm (range 0.2–5 cm). The stenosis length ≤1 cm is observed in 51 patients (18.9%), 1.1–2.0 cm in 184 (68.1%), 2.1–3.0 cm in 21 (7.8%), and >3 cm in 14 (5.2%).
Efficacy of interventional bronchoscopy treatment for scarring airway stenosis in Chinese patients
During the process of repeated therapeutic bronchoscopy, no severe life-threatening bronchoscopy-related complications occurred.
Figure 2 shows the treatment outcomes of 392 patients with scarring airway stenosis who underwent therapeutic bronchoscopy. After three repeated therapeutic bronchoscopy treatment interventions, 250 patients exhibited an effect whereas 142 patients showed an invalid clinical outcome. In 250 patients who were treated effectively, 237 had stable clinical course and 13 presented severe complications (all occurred after stent insertion, including 8 severe granulation tissue formation and 5 repeated stent migration) during the therapeutic bronchoscopy treatment. Finally, 155 patients demonstrated clinical failure.
Figure 2.
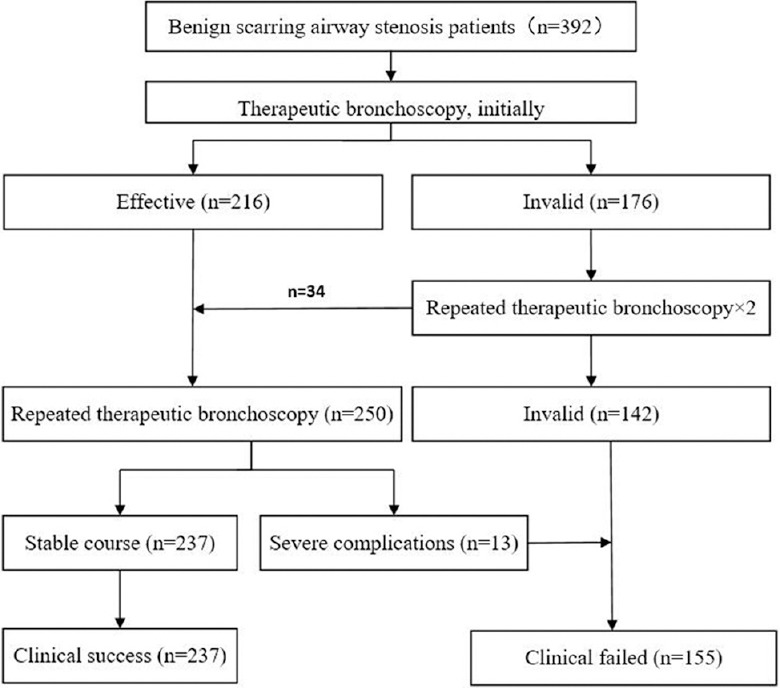
Treatment schematic representation of patients with scarring airway stenosis.
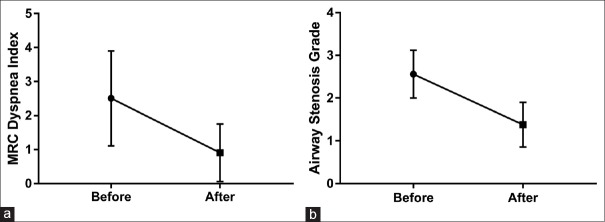
The results showed 60.5% (237/392) clinical success rate and 39.5% (155/392) clinical failure rate. For patients treated successfully, the average MRC dyspnea index decreased from 2.5 to 0.9, and the airway stenosis degree decreased from 2.6 to 1.4 [Figure 3]. The average times of interventional bronchoscopy treatment were 4.8.
Figure 3.
Difference before and after interventional bronchoscopy in Medical Research Council Dyspnea Grade (a) and airway stenosis grade (b). MRC: Medical research council.
Usage of stent in scarring airway stenosis treatment in China
In the present study, 34/392 (8.7%) patients received stent insertion (17 silicone stent, 15 fully covered metallic stent, and 2 T tubes). 13/34 (38.2%) stents had to be removed after an average of 56 days due to severe complications. 8/34 (23.5%) patients underwent stent removal due to severe granulation tissue formation (3 silicone stents and 5 fully covered metallic stents), and 5/34 (14.7%) showed stent migration (2 silicone stents and 3 fully covered metallic stents).
Stent removal was attempted on 21 stable cases. 10/34 (29.4%) stents could be removed after an average of 112.9 days (range, 25–357 days; 4 silicone stents and 6 fully covered metallic stents) while 11 stents (11/34, 32.4%) had to be left in the airway (9 silicone stents and 2 T tubes) without obvious complications [Figure 4].
Figure 4.
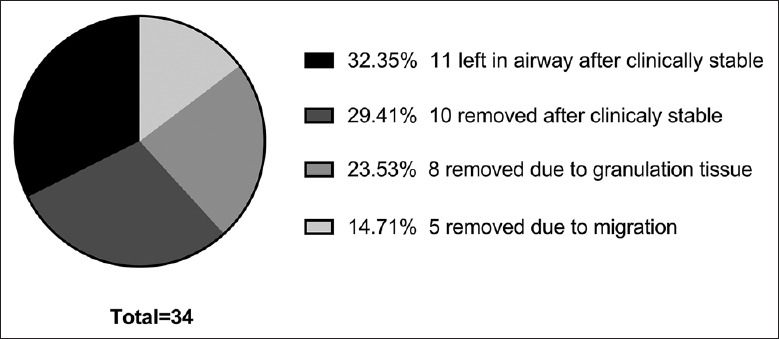
Final efficacy of stent used for scarring airway stenosis treatment.
DISCUSSION
Scarring airway stenosis is a specific type of benign airway stenosis. Interventional bronchoscopy treatment could rapidly and efficiently relieve the airway obstruction and improve clinical symptoms.[7,8] In western countries, scarring airway stenosis results mainly from intubation, tracheotomy, burn injuries, secondary healing after surgery, or trauma.[9] However, some differences are observed with respect to the characteristics and treatment efficacy of this disease between developed and developing countries. In this study, the characteristics of scarring airway stenosis in Chinese adults and the efficacy of interventional bronchoscopy treatment in China were described.
The results showed that EBTB was the most common cause of scarring airway stenosis in Chinese adults (77.8%), which was predisposed toward a high rate of incidence in young women (86.9%); this phenomenon was also observed in a previous study.[10] The high incidence of EBTB in young women may be attributed to the narrow bronchus and weak ability to clear sputum due to which the tubercle bacilli easily attaches to the bronchial wall. The left main bronchus was most susceptible to EBTB; this may be because, compared to the right main bronchus, the left is slender and tilted, thereby allowing easy attachment of the tubercle bacilli.
According to bronchoscopic features, EBTB could be classified into 7 subtypes: fibrostenotic, edematous–hyperemic, actively caseating, tumorous, ulcerative, granular, and nonspecific bronchitic type.[11] Studies showed that posttuberculosis scarring airway stenosis could be caused not only by fibrostenotic type but also other types such as actively caseating, edematous–hyperemic, and tumorous type.[12,13] In these cases, specific measures are essential for preventing or minimizing the bronchial stenosis. For active endobronchial tuberculosis patients, the primary goal of treatment is the eradication of tubercle bacilli, and progression to airway stenosis may be prevented if the therapy is initiated at the earliest. Early treatment with steroid therapy is effective in particular groups of EBTB; however, to consider the therapeutic effect of steroid on the alleviation of bronchial stenosis in EBTB, the interval between symptom-onset and treatment with steroid is recommended as <6 months.[13] Future research should focus on the pathogenesis of bronchial inflammatory reaction and the resulting fibrosis to prevent bronchial stenosis at an early stage.
Herein, the efficacy of interventional bronchoscopy treatment for scarring airway stenosis in China was evaluated. The treatment efficacies vary in different centers, which may be influenced by equipment, proficiency of interventional physician, anesthesia methods (local or general anesthesia), and other factors. The present study showed that the average clinical success rate of interventional bronchoscopy treatment for scarring airway stenosis in China is 60.5%, indicating that more than half of the scarring airway stenosis patients could benefit from this technique, and surgical resection could be avoided.
The usage of the stent for scarring airway stenosis treatment in China was also observed in this study. The stent is a foreign body that can induce new strictures or complications, but patients with benign tracheobronchial strictures have a long life expectancy, which requires lifelong adjunctive procedures to maintain stent patency.[14] Therefore, placement of conventional, nonremovable, expandable bare metallic stents is rarely indicated for benign tracheobronchial strictures because long-term patency is poor.[15] In developed countries, silicone stent was the most commonly used airway stent for benign airway stenosis; however, in China, due to economic and technique reasons, silicone stent insertion (including T tube) was used much less (19/392, 4.8% in this study) and usually was the last choice after other interventional bronchoscopy treatment (such as balloon dilation) failed, or used only for those with obvious dynamic stenosis or airway fistula.[16,17] Covered retrievable expandable nitinol stent was cheaper in China and easier to be implanted; therefore, it sometimes was used for benign tracheobronchial strictures to instead silicone stent. However, studies examining the use of such stents for benign tracheobronchial strictures have involved only small numbers of patients and short follow-up times.[18,19]
It is speculated that benign airway stenosis should be exclusively treated using temporary rather than permanent stents in order to avoid severe stent-related complications, presuming that the stent will not be required after healing of the stenosis or that a sufficient duration of stent support will prevent the restructure after removal.[14] Nevertheless, among the 34 scarring airway stenosis patients who received stent insertion, 11 (32.4%) had to retain the stents in the airway, suggesting that not all benign stenosis could be healed even after sufficient duration of stent support.
In the current study, 11 stents (40.7%) had to be removed because of severe complications. Granulation tissue formation is the most common complication (23.5%), which is similar to other studies;[20,21] the second complication is stent migration (14.7%). Predictably, the technical improvements in stent design, including retrievability and absorbability, would result in airway stent placement expanding in its indications in benign diseases.
In summary, the scarring airway stenosis exhibits specific characteristics in China. EBTB was the most common cause of scarring airway stenosis in Chinese adults. Interventional bronchoscopy is a valuable treatment method for the disease.
Financial support and sponsorship
This study was supported by the grants from Capital Health Development Research Project (No. 2016-2-2048) and Youth Fund of Beijing Tian Tan Hospital (2017-YQN-17).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank those doctors from the seventeen hospitals for the help in the data collection.
Yu Fu, Wei-Min Ding, Department of Endoscopy, Beijing Chest Hospital, Capital Medical University
Cheng-Ping Hu, Hua-Ping Yang, Department of Respiratory, Xiangya Hospital, Central South University
Li-Ping Lyu, Department of Interventional Pulmonology, Anhui Chest Hospital
Xiao-Ping Wang, Li Xu, Department of Endoscopy, Shandong Chest Hospital
Ji-Wang Wang, Department of Respiratory, Jiangsu Provincial Hospital
Bo Wu, Department of Lung Transplantation, Wuxi People Hospital, Nanjing Medical University
Hong-Mei Zhou, Department of Respiratory, Second People's Hospital of Gansu
Xiao-Qi Xiong, Department of Respiratory, People's Hospital of Yichang City
Ming-Yao Ke, Rui Huang, Department of Respiratory, Second Affiliated Hospital of Xiamen Medical College
Zhuang Ma, Department of Respiratory, The General Hospital of Shenyang Military
Hang Li, Department of Respiratory, Yantai YuHuangDing Hospital
Zhen Wang, Department of Respiratory, Beijing Chao-Yang Hospital, Capital Medical University
Dong-Hui Huang, Department of Respiratory, Guangdong Provincial Hospital of Traditional Chinese Medicine
Peng Li, Department of Respiratory, Shengjing Hospital of China Medical University
Yan Duan, Department of Endoscopy, Xi'an Chest Hospital
Zhi-Gang Cai, Department of Respiratory, the Second Hospital of Hebei Medical University
Zhi-Gang Yao, Department of Respiratory, Beijing Friendship Hospital, Capital Medical University.
Footnotes
Edited by: Li-Min Chen
REFERENCES
- 1.Freitag L, Ernst A, Unger M, Kovitz K, Marquette CH. A proposed classification system of central airway stenosis. Eur Respir J. 2007;30:7–12. doi: 10.1183/09031936.00132804. doi: 10.1183/09031936.00132804. [DOI] [PubMed] [Google Scholar]
- 2.Krajc T, Janik M, Benej R, Lucenic M, Majer I, Demian J, et al. Urgent segmental resection as the primary strategy in management of benign tracheal stenosis. A single center experience in 164 consecutive cases. Interact Cardiovasc Thorac Surg. 2009;9:983–9. doi: 10.1510/icvts.2009.213215. doi: 10.1510/icvts.2009.213215. [DOI] [PubMed] [Google Scholar]
- 3.Rahman NA, Fruchter O, Shitrit D, Fox BD, Kramer MR. Flexible bronchoscopic management of benign tracheal stenosis: Long term follow-up of 115 patients. J Cardiothorac Surg. 2010;5:2. doi: 10.1186/1749-8090-5-2. doi: 10.1186/1749-8090-5- [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dalar L, Karasulu L, Abul Y, Özdemir C, Sökücü SN, Tarhan M, et al. Bronchoscopic treatment in the management of benign tracheal stenosis: Choices for simple and complex tracheal stenosis. Ann Thorac Surg. 2016;101:1310–7. doi: 10.1016/j.athoracsur.2015.10.005. doi: 10.1016/j.athoracsur.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Cotton RT. Pediatric laryngotracheal stenosis. J Pediatr Surg. 1984;19:699–704. doi: 10.1016/s0022-3468(84)80355-3. [DOI] [PubMed] [Google Scholar]
- 6.Myer CM, 3rd, O'Connor DM, Cotton RT. Proposed grading system for subglottic stenosis based on endotracheal tube sizes. Ann Otol Rhinol Laryngol. 1994;103(4 Pt 1):319–23. doi: 10.1177/000348949410300410. doi: 10.1177/000348949410300410. [DOI] [PubMed] [Google Scholar]
- 7.Okiror L, Jiang L, Oswald N, Bille A, Rajesh P, Bishay E, et al. Bronchoscopic management of patients with symptomatic airway stenosis and prognostic factors for survival. Ann Thorac Surg. 2015;99:1725–30. doi: 10.1016/j.athoracsur.2015.01.061. doi: 10.1016/j.athoracsur.2015.01.061. [DOI] [PubMed] [Google Scholar]
- 8.Li YQ, Li Q, Bai C, Huang Y, Zhao LJ, Yao XP, et al. Causes of benign central airway stenoses and the efficacy of interventional treatments through flexible bronchoscopy. Zhonghua Jie He He Hu Xi Za Zhi. 2008;31:364–8. doi: 10.3321/j.issn:1001-0939.2008.05.011. [PubMed] [Google Scholar]
- 9.Stoelben E, Koryllos A, Beckers F, Ludwig C. Benign stenosis of the trachea. Thorac Surg Clin. 2014;24:59–65. doi: 10.1016/j.thorsurg.2013.09.001. doi: 10.1016/j.thorsurg.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Lei Y, Tian-Hui Z, Ming H, Xiu-Jun C, Yong D, Fu-Gen L, et al. Analysis of the surgical treatment of endobronchial tuberculosis (EBTB) Surg Today. 2014;44:1434–7. doi: 10.1007/s00595-014-0865-9. doi: 10.1007/s00595-014-0865-9. [DOI] [PubMed] [Google Scholar]
- 11.Lee JH, Chung HS. Bronchoscopic, radiologic and pulmonary function evaluation of endobronchial tuberculosis. Respirology. 2000;5:411–7. doi: 10.1111/j.1440-1843.2000.00285.x. [PubMed] [Google Scholar]
- 12.Shim YS. Endobronchial tuberculosis. Respirology. 1996;1:95–106. doi: 10.1111/j.1440-1843.1996.tb00017.x. doi: 10.1111/j.1440-1843.1996.tb00017.x. [DOI] [PubMed] [Google Scholar]
- 13.Shim YS. New classification of endobronchial tuberculosis and balloon dilatation of bronchial stenosis. Kekkaku. 1992;67:353–7. [PubMed] [Google Scholar]
- 14.Kim JH, Shin JH, Song HY, Shim TS, Yoon CJ, Ko GY, et al. Benign tracheobronchial strictures: Long-term results and factors affecting airway patency after temporary stent placement. AJR Am J Roentgenol. 2007;188:1033–8. doi: 10.2214/AJR.06.0888. doi: 10.2214/AJR.06.0888. [DOI] [PubMed] [Google Scholar]
- 15.Walser EM. Stent placement for tracheobronchial disease. Eur J Radiol. 2005;55:321–30. doi: 10.1016/j.ejrad.2005.03.005. doi: 10.1016/j.ejrad.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Qiu XJ, Zhang J, Wang T, Pei YH, Xu M. Nonstent combination interventional therapy for treatment of benign cicatricial airway stenosis. Chin Med J (Engl) 2015;128:2154–61. doi: 10.4103/0366-6999.162496. doi: 10.4103/0366-6999.162496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ke MY, Huang R, Lin LC, Zeng JL, Wu XM. Efficacy of the dumon™ stent in the treatment of airway gastric fistula: A Case series involving 16 patients. Chin Med J (Engl) 2017;130:2119–20. doi: 10.4103/0366-6999.213420. doi: 10.4103/0366-6999.213420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choi EK, Song HY, Shin JH, Lim JO, Park H, Kim CS, et al. Management of recurrent urethral strictures with covered retrievable expandable nitinol stents: Long-term results. AJR Am J Roentgenol. 2007;189:1517–22. doi: 10.2214/AJR.07.2149. doi: 10.2214/AJR.07.2149. [DOI] [PubMed] [Google Scholar]
- 19.Kim JH, Shin JH, Shim TS, Hong SJ, Ko GY, Lim JO, et al. Results of temporary placement of covered retrievable expandable nitinol stents for tuberculous bronchial strictures. J Vasc Interv Radiol. 2004;15:1003–8. doi: 10.1097/01.RVI.0000133857.09327.1A. doi: 10.1097/01.RVI.0000133857.09327.1A. [DOI] [PubMed] [Google Scholar]
- 20.Ost DE, Shah AM, Lei X, Godoy MCB, Jimenez CA, Eapen GA, et al. Respiratory infections increase the risk of granulation tissue formation following airway stenting in patients with malignant airway obstruction. Chest. 2012;141:1473–81. doi: 10.1378/chest.11-2005. doi: 10.1378/chest.11-2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu HC, Liu YH, Wu YC, Hsieh MJ, Chao YK, Wu CY, et al. Granulation tissue formation following Dumon airway stenting: The influence of stent diameter. Thorac Cardiovasc Surg. 2011;59:163–8. doi: 10.1055/s-0030-1250667. doi: 10.1055/s-0030-1250667. [DOI] [PubMed] [Google Scholar]