Abstract
Background:
Comprehensive management of diabetes should include management of its comorbid conditions, especially cardiovascular complications, which are the leading cause of morbidity and mortality among patients with diabetes. Dyslipidemia is a comorbid condition of diabetes and a risk factor for cardiovascular complications. Therefore, lipid level management is a key of managing patients with diabetes successfully. However, it is not clear that how well dyslipidemia is managed in patients with diabetes in local Chinese health-care communities. This study aimed to assess how well low-density lipoprotein cholesterol (LDL-C) was managed in Nanjing community hospitals, China.
Methods:
We reviewed clinical records of 7364 diabetic patients who were treated in eleven community hospitals in Nanjing from October 2005 to October 2014. Information regarding LDL-C level, cardiovascular risk factors, and use of lipid-lowering agents were collected.
Results:
In patients without history of cardiovascular disease (CVD), 92.1% had one or more CVD risk factors, and the most common CVD risk factor was dyslipidemia. The overall average LDL-C level was 2.80 ± 0.88 mmol/L, which was 2.62 ± 0.90 mmol/L and 2.82 ± 0.87 mmol/L in patients with and without CVD history respectively. Only 38% of all patients met the target goal and 37.3% of patients who took lipid-lowering agents met target goal. Overall, 24.5% of all patients were on lipid-lowering medication, and 36.3% of patients with a CVD history and 20.9% of patients without CVD history took statins for LDL-C management. The mean statin dosage was 13.9 ± 8.9 mg.
Conclusions:
Only a small portion of patients achieved target LDL-C level, and the rate of using statins to control LDL-C was low. Managing LDL-C with statins in patients with diabetes should be promoted, especially in patients without a CVD history and with one or more CVD risk factors.
Keywords: Community Hospitals, Diabetes, Dyslipidemia, Low-density Lipoprotein Cholesterol, Statin
INTRODUCTION
Diabetes mellitus (DM) is a prevalent health problem worldwide. The World Health Organization reported that the global prevalence of diabetes among adults (over 18 years of age) was 8.5% in 2014.[1] In recent years, diabetes has become one of the most prevalent noncommunicable chronic diseases in China. The estimated overall diabetes prevalence rate in the Chinese adult population is 11.6%, and the prevalence of prediabetes is estimated to be 50.1%, which could represent up to 113.9 million adult Chinese individuals with diabetes and 493.4 million who are prediabetic.[2]
Comprehensive management of DM should include treatments of comorbid conditions, including dyslipidemia, hypertension, and cardiovascular complications.[3] Among these comorbid conditions, cardiovascular complications are the leading causes of mortality and morbidity.[4,5] Although other risk factors such as hormone levels and race could also play a role,[6,7,8] dyslipidemia has been identified as one of the major risk factors for cardiovascular disease (CVD) in DM patients.[8] Effective management of lipid levels contributes to the early-prevention of CVD[9] and is recommended for managing DM. Particularly, low-density lipoprotein cholesterol (LDL-C) is a main target for lipid therapy.[10,11] Statin therapy is an effective and safe cholesterol-lowering agent[12,13] that is recommended for all patients with diabetes at risk for vascular events.[14,15]
A recent study found that in the middle-aged and elderly Chinese populations, overweight/obesity, dyslipidemia, and diabetes are the leading risk factors for CVD.[16] Thus, controlling CVD risk factors, especially the LDL-C level, is essential in managing CVD in DM patients. The Chinese diabetes management guidelines recommend lipid-lowering therapy for all DM patients regardless of their baseline LDL-C level.[17] The recommendation is to lower the plasma LDL-C level with lifestyle optimization and with the adjunctive use of statin therapy as the lipid-lowering agent of choice.[17,18] However, despite a high prevalence of dyslipidemia in Chinese patients with diabetes,[3,19] it is unclear that how well local Chinese health-care communities are implementing treatment guidelines, managing dyslipidemia, and utilizing statin therapy in patients with diabetes.
In the Chinese health-care system, the community hospitals are tasked with delivering the majority of care for noncommunicable chronic diseases including diabetes. However, few studies have evaluated the efficacy of current practices regarding the management of lipid levels, particularly, LDL-C levels, in DM patients at the community hospital level. This study aimed to assess the current status of LDL-C control by assessing the rate of LDL-C target goal achievement in DM patients. In addition, the use of statin therapy was also evaluated in accordance with recommended treatment guidelines.
METHODS
Ethical approval
The study was conducted in accordance with the ethical standards of participating institutions and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was waived due to the nature of the retrospective study.
Study design
The present study was an observational, cross-sectional, retrospective study. This study included 7364 diabetic patients who were treated in eleven Nanjing community hospitals from October 2005 to October 2014.
Cardiovascular disease risk factor data collection and lipid measurements
Relevant patient data were collected from the clinical examination records and medical charts from eleven community hospitals in the Nanjing and vicinity area. CVD risk factors that were assessed include smoking, weight status (i.e., overweight or obese), hypertension, albuminuria, and dyslipidemia.
Smoking habits were self-reported. A DM patient with a body mass index of ≥24 kg/m2 was considered as risk for CVD.[20] Patients who had a history of hypertension, or were currently on medication to treat hypertension, or whose systolic pressure measured ≥140 mmHg (1 mmHg = 0.133 kPa), and/or whose diastolic blood pressure measured ≥90 mmHg were considered to have hypertension. Albuminuria was assessed by calculating the urinary albumin-to-creatinine ratio, with a ratio of <30 mg/g as normal. Documented CVD history included stable or unstable angina pectoris, myocardial infarction, and cerebral ischemic stroke. Patients who underwent coronary revascularization or coronary bypass were also considered to have a history of CVD. Each patient's lipid profile was collected from his/her clinical record; total cholesterol (TC), LDL-C, high-density lipoprotein cholesterol (HDL-C), and triglycerides (TG) were assessed. A patient was diagnosed with dyslipidemia if any of the following criteria was met:[17] (1) a TC level of ≥4.5 mmol/L, (2) a LDL-C level of ≥1.8 mmol/L for patients with CVD and 2.6 mmol/L for patients without a CVD history, (3) a HDL-C level of ≤1.0 mmol/L for males and 1.3 mmol/L for females, and (4) a TG level ≥1.7 mmol/L.
Statin use and treatment goals
Statins used for LDL-C management included atorvastatin, simvastatin, lovastatin, pravastatin, rosuvastatin, fluvastatin, and xuezhikang (a medicine that is developed from traditional Chinese medicinal herbs and contains statins). The dosage of each above statin was converted to comparable atorvastatin dosages for the purposes of this study [Table 1].
Table 1.
Commonly used statin dosages compared to comparable atorvastatin dosages (mg)
| Atorvastatin | Simvastatin | Lovastatin | Pravastatin | Fluvastatin | Rosuvastatin | Xuezhikang |
|---|---|---|---|---|---|---|
| – | 10 | 20 | 20 | 40 | – | 600 |
| 10 | 20 | 40 | 40 | 80 | 5 | – |
| 20 | 40 | 80 | – | – | 10 | – |
| 40 | 80 | – | – | – | – | – |
| 80 | – | – | – | – | – | – |
–: Not applicable.
Statin use adherence and dosages were self-reported. The target goal of LDL-C was <1.8 mmol/L for patients with CVD and <2.6 mmol/L for patients without a CVD history. These targets were recommended as the target goals in the Chinese guidelines for patients with diabetes.[18]
Statistical analysis
Categorical variables are presented as frequencies and percentages, and continuous variables as means ± standard deviation (SD) unless otherwise noted. Statistical analyses were performed using SPSS statistics software (version 22.0, IBM, Armonk, USA). Between-group differences were determined using t-tests for continuous variables and Chi-square tests for percentage values. A P < 0.05 was considered statistically significant.
RESULTS
Patients demographic and disease characteristics
This study included a total of 7364 diabetic patients who were treated in eleven Nanjing community hospitals from October 2005 to October 2014. The demographic information and baseline characteristics are summarized in Table 2. The age of the patients ranged from 33.0 to 93.0 years, with the average age being 64.1 ± 11.2 years. Most of the patients (5358/7364, 72.8%) had a history of diabetes of more than 10 years.
Table 2.
Patients’ demographic information and baseline characteristics
| Characteristics | Total | Without CVD history | With CVD history | t or χ2 | P (with vs. without CVD history) |
|---|---|---|---|---|---|
| Patients number, n (%) | 7364 (100) | 6406 (87) | 958 (13) | ||
| Age (years) | 64.08 ± 11.15 | 63.21 ± 11.21 | 69.86 ± 8.85 | 17.56 | <0.01 |
| <40, n (%) | 159 (2.2) | 158 (2.5) | 1 (0.1) | 145.11* | <0.01 |
| 40–75, n (%) | 5993 (81.5) | 5315 (83.0) | 678 (70.8) | ||
| >75, n (%) | 1200 (16.3) | 921 (14.4) | 279 (29.1) | ||
| Gender (male), n (%) | 4169 (56.6) | 3653 (57.0) | 516 (53.9) | 3.59* | 0.06 |
| Highest education level, n (%) | |||||
| High school and below | 4625 (62.9) | 3968 (62.1) | 657 (68.6) | 15.13* | <0.01 |
| Associate and above | 2725 (37.1) | 2424 (37.9) | 301 (31.4) | ||
| Diabetes history (years), n (%) | |||||
| <1 | 978 (13.3) | 904 (14.1) | 74 (7.7) | 41.93* | <0.01 |
| ≥1 and <5 | 748 (10.2) | 666 (10.4) | 82 (8.6) | ||
| ≥5 and <10 | 280 (3.8) | 255 (4.0) | 25 (2.6) | ||
| ≥10 | 5358 (72.8) | 4581 (71.5) | 777 (81.1) | ||
| Smoking | 1464 (20.1) | 1298 (20.5) | 166 (17.6) | 4.36* | <0.05 |
| BMI ≥24 (kg/m2) | 4429 (61.3) | 3806 (60.5) | 623 (66.7) | 13.31* | <0.01 |
| Blood lipids (mmol/L) | |||||
| TC | 4.84 ± 1.10 | 4.87 ± 1.09 | 4.62 ± 1.15 | 6.17 | <0.01 |
| LDL-C | 2.80 ± 0.88 | 2.82 ± 0.87 | 2.62 ± 0.90 | 6.43 | <0.01 |
| HDL-C | 1.24 ± 0.40 | 1.25 ± 0.41 | 1.21 ± 0.33 | 2.64 | <0.01 |
| TG | 1.77 ± 1.47 | 1.79 ± 1.49 | 1.67 ± 1.39 | 2.22 | <0.05 |
| Non-HDL-C | 3.59 ± 1.07 | 3.62 ± 1.06 | 3.41 ± 1.10 | 5.49 | <0.01 |
| Blood pressure | |||||
| Hypertension, n (%) | 4859 (66.3) | 4078 (64.0) | 781 (81.5) | 19.83* | <0.01 |
| Systolic pressure (mmHg) | 129.59 ± 14.93 | 129.31 ± 14.91 | 131.39 ± 14.90 | 4.01 | <0.01 |
| Diastolic pressure (mmHg) | 77.33 ± 9.19 | 77.51 ± 9.20 | 76.12 ± 9.04 | 4.38 | <0.01 |
| Chronic kidney disease, n (%)† | 1854 (28.7) | 1510 (26.9) | 344 (40.3) | 64.94* | <0.01 |
*χ2 value; †Criteria of chronic kidney disease: Previous history of chronic kidney disease, or either of the following present for >3 months, ACR ≥30 mg/g and eGFR <60 ml·min−1 ·1.73 m−2. BMI: Body mass index; TC: Total cholesterol; LDL-C: Low-density lipoprotein cholesterol; HDL-C: High-density lipoprotein cholesterol; TG: Triglycerides; CVD: Cardiovascular disease; ACR: Albumin-to-creatinine ratio; eGFR: Estimated glomerular filtration rate.
The majority of patients (6406/7364, 87.0%) had no history of CVD; however, 92.1% (5899/6406) of these patients had one or more CVD risk factors. Among the CVD risk factors, dyslipidemia was the most common, with a total of 87.5% of patients having the condition [Figure 1].
Figure 1.
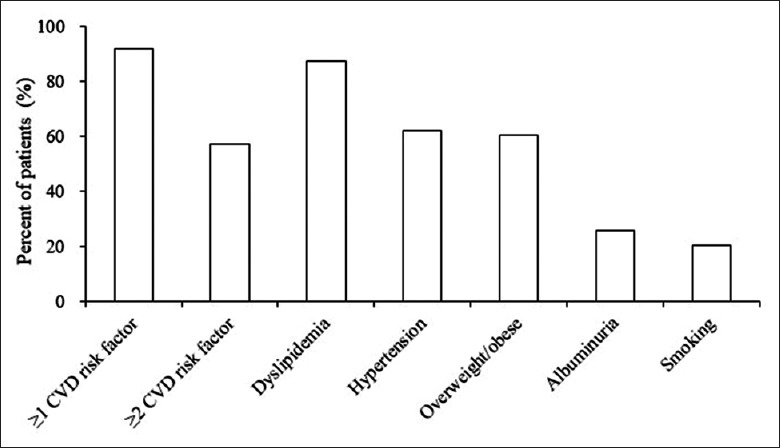
Risk factors in patients without cardiovascular disease history. The majority of patients without cardiovascular disease history had at least one risk factor. Dyslipidemia was the most common risk factor, affecting 87.5% of the patients in this group.
Low-density lipoprotein cholesterol level
As the study was conducted based on real-world experience, some patients did not have clinical record of lipid profile. The LDL-C level was obtained in 6328 (85.9%) patients of the total 7364 patients. The LDL-C level measured on average was 2.80 ± 0.88 mmol/L in all patients, 2.82 ± 0.87 mmol/L in patients without CVD history, and 2.62 ± 0.90 mmol/L in patients with a CVD history (t = 6.43, P < 0.01). Overall, the LDL-C level in the patients enrolled in the study was higher than the target goals, which were lower than 2.6 mmol/L for patients without CVD history and lower than 1.8 mmol/L for patients with a CVD history.
Rate of statin use in patients with diabetes
Overall, 24.5% (1803/7355) of all patients were on any lipid-lowering medication, and 22.9% (1683/7355) of all patients used statin therapy for lipid management. Furthermore, 36.3% (347/956) of patients with a CVD history and 20.9% (1336/6399) of patients without CVD history used statin therapy as their lipid-lowering medication [Figure 2]. It is worth noting that in patients who were using lipid-lowering agents, 96.7% (347/359) of patients with and 92.5% (1336/1444) of patients without CVD history used statin therapy for management of their lipid levels. The mean dose of statins used in all patients was 13.9 ± 8.9 mg/d. Further analyses found that the average dose of statins used was 15.0 ± 11.5 mg in patients with a CVD history and 13.5 ± 8.0 mg in patients without a CVD history.
Figure 2.
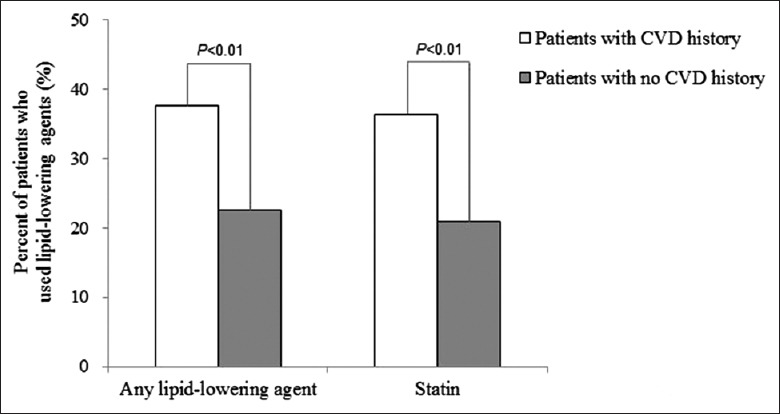
Rates of lipid-lowering agents and statin use. Lipid-lowering agents include atorvastatin, simvastatin, lovastatin, pravastatin, rosuvastatin, fluvastatin, and xuezhikang.
Rate of patients who achieved their low-density lipoprotein cholesterol target goal
At the time of the study, 38.0% of all the patients had met their target goal (<1.8 mmol/L for patients with a CVD history and 2.6 mmol/L for patients without a CVD history). In patients who had a history of CVD, 17.1% had met the target goal, whereas 41.3% of patients who had no CVD history had met the goal.
In patients who had used lipid-lowering agents, 37.3% had achieved their target LDL-C goal, with 23.9% of patients who had CVD history and 40.6% of patients who had no CVD history reaching their target LDL-C level [Figure 3].
Figure 3.
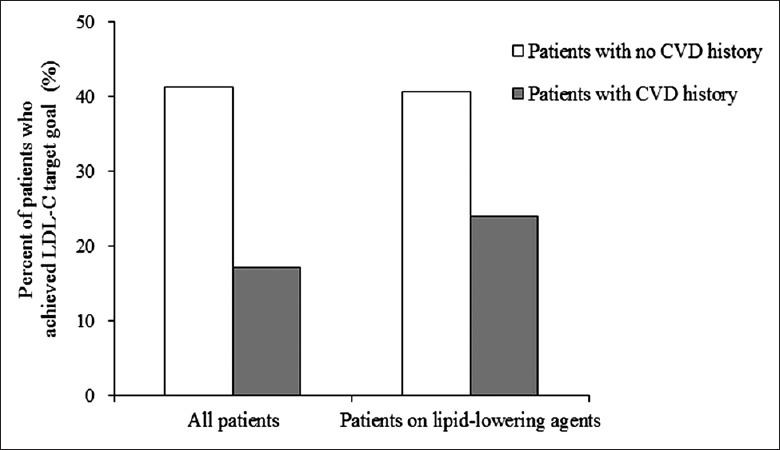
Rates of achieving low-density lipoprotein cholesterol target goal.
DISCUSSION
CVD is the leading cause of mortality in patients with diabetes, and thus effective management of CVD risk factors, especially LDL-C, is essential for managing patients with diabetes. Because of the unique structure of the Chinese health-care system, the community hospitals are often the most accessible health-care resource to patients and thus are tasked with managing DM patients. Therefore, understanding how effective community hospitals are managing their DM patients and providing these hospitals with adequate support and education are essential for delivering optimal care by implementing the recommended treatment guidelines. However, studies in this field are sparse.
In this cross-sectional study of patients with diabetes who were treated in Nanjing community hospitals, we found that more than 60% of patients did not achieve the target LDL-C goal. Furthermore, we observed that a higher proportion (41.3%) of patients without CVD history achieved their target goal compared with patients with a CVD history (17.1%). As the target LDL-C levels for patients with diabetes are lower than for the healthy population, it is more challenging for them to achieve their goals. Nevertheless, more than half of the patients who were treated with lipid-lowering agents did not achieve their target LDL-C level, indicating that lipid abnormalities were not managed effectively in these patients. A similar study of patients with diabetes with hypertension conducted in Beijing community hospitals showed that the mean LDL-C was 3.2 mmol/L, and that the rate of LDL-C target goal achievement (the target goal was <2.6 mmol/L) was 25.6% at baseline. Both the Nanjing community hospitals and Beijing hospitals were well situated to provide optimal care for those patients. However, although the Nanjing community hospitals managed the DM patients more effectively than the Beijing community hospitals, the gap between the clinical results and the target goals recommended by the guidelines was wide.
The rate of following the treatment guideline recommendations of statin therapy for the management of LDL-C was low, which could contribute to the low rate of achieving target LDL-C levels in the present study. Although in the study the vast majority of patients who were on lipid-lowering agents used statins, we found that the overall use of statins as a lipid-lowering agent in patients with diabetes was low. Despite the finding that statin use might be associated with a higher rate of diabetes incidence,[21,22] the current consensus is that the benefits of managing LDL-C with statins outweighs the adverse effects. A recent study conducted in Beijing community hospitals found that an increase in statin use was associated with an increase in the rate of T2DM patients who achieved LDL-C target goals in patients who participated in a 3-year intervention program.[23] Thus, statin use as recommended by the guidelines should be promoted in DM patients in China, especially given the prevalence of dyslipidemia in this population.[3,19] The present study of a Chinese diabetes patient population in the Nanjing area found that the overall rate of statin use was as low as 22.9%. Our finding is consistent with previous studies that found that the overall use of statins for management of dyslipidemia in the Chinese population is relatively low.[1,19,24,25] Particularly, Lyu et al.[23] reported that only 18.3% patients with diabetes with hypertension used statins for lipid management. This discrepancy between clinical practice and guideline recommendations should be addressed to improve management of DM patients.
For the patients who were over forty without CVD history, but with one or more CVD risk factors for life-threatening cardiovascular complications, the primary prevention of CVD is particularly essential. However, the rate of statin use was significantly lower (20.9%) in this subpopulation of DM patients, and the LDL-C level (2.82 ± 0.87 mmol/L) was significantly higher compared with DM patients with a CVD history (2.62 ± 0.90 mmol/L). According to the Chinese diabetes treatment and management guidelines, the LDL-C target goal is below 2.6 mmol/L when DM patients have one or more CVD risk factors. In our study, more than 90% of the patients without a CVD history had one or more CVD risk factors, and the most common CVD risk factor was dyslipidemia (87.5%), indicating that the majority of these patients should be treated with statins to achieve the LDL-C management goal. Therefore, this subpopulation that was especially vulnerable to risks of CVD should be monitored more closely and managed more effectively.
In addition to the low rate of statin use, another possible cause for the low rate of achieving LDL-C target goals in DM patients is that statins are not being prescribed at effective dosages, especially for DM patients with a CVD history. For DM patients with atherosclerotic CVD, although Chinese guidelines recommend moderate intensity (10–20 mg atorvastatin) statin therapy, the latest American Diabetes Association guidelines (2017) recommend high-intensity (40–80 mg atorvastatin) statin therapy.[26] Thus, it is likely that high-intensity statin is required to effectively manage the LDL-C level in DM patients. We found in this study that the mean statin dose prescribed for these patients was 15 ± 11.5 mg, which might not be sufficient for reducing LDL-C.
The low statin use rate and the inadequate statin dosages may be due to the following factors: lack of awareness about statin therapy, adverse effects of statins, and costs of statin.[25] To control CVD in patients with diabetes, blood glucose, blood pressure, and blood lipids should all be managed.[3] Statin therapy is the recommended first-line LDL-C-lowering agent for the management of high LDL-C in patients with diabetes.[11,18,27,28] However, the physicians who treat patients with diabetes often solely focus on lowering blood glucose and do not provide adequate lipid-lowering therapy.[3] It is also possible that some physicians do not follow treatment guidelines. Therefore, educating health-care providers and patients about the benefits of statin therapy and encouraging the use of statins should be promoted to better manage lipid abnormalities in patients with diabetes. Particularly, raising awareness of the importance of treating dyslipidemia among physicians is crucial to controlling CVD in patients with diabetes.
Moreover, patients' adherence to treatment regimens may not have been ideal, which could have also contributed to the low rate of achieving target LDL-C levels in the present study. Previous studies have described that the benefits of statin therapy that have been observed in clinical trials can only be replicated in real life in patients who completely adhere to treatment regimens.[29,30] Finally, the present study is a cross-sectional study, and the history of statin use is not taken into consideration; therefore, the statin therapy might have not reached its full potency in all patients at the time of study.
One limitation of the study is that there was no follow-up for patients included in the study; therefore, the study does not provide information regarding long-term management of DM. As DM is a chronic condition, more study efforts should be directed at investigating long-term management. In addition, community hospitals in Nanjing area are known to be well managed and represent the high-quality health-care facilities in China. As a result, this cross-sectional study was not representative of the care provided by the average community hospital in China. Therefore, it is alarming that even in the top community hospital, LDL-C was poorly managed in DM patients, indicating a high risk of CVD for these patients nationwide.
In conclusion, overall, in this cross-sectional study, we found that LDL-C was not managed effectively in DM patients treated in Nanjing community hospitals. Furthermore, the use of statins for lipid management is low. The real-world clinical results of LDL-C management in DM patients are far from the target goal set by the guidelines. Furthermore, a particularly vulnerable patient subpopulation consisted of those patients without a CVD history; more than 90% of them had one or more other CVD risk factors but the rate of statin use was only 20.9%, and it is imperative to start primary prevention of CVD in these patients as soon as possible. DM-associated CVD poses substantial burden on the health-care system, and effective control of risk factors such as LDL-C is a pivotal step in managing public health. The results of this cross-sectional study indicate that the delivery of care is challenging in the setting of everyday practice, and implementation of the guideline recommendations should be promoted and encouraged.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Li-Shao Guo
REFERENCES
- 1.WHO; 2016. [Last accessed on 2016 Jun 27, 11:26:39]. World Health Organization. Global Report on Diabetes. Available from: http://www.who.int/diabetes/global-report/en/ [Google Scholar]
- 2.Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310:948–59. doi: 10.1001/jama.2013.168118. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 3.Ji L, Hu D, Pan C, Weng J, Huo Y, Ma C, et al. Primacy of the 3B approach to control risk factors for cardiovascular disease in type 2 diabetes patients. Am J Med. 2013;126:925.e11–22. doi: 10.1016/j.amjmed.2013.02.035. doi: 10.1016/j.amjmed.2013.02.035. [DOI] [PubMed] [Google Scholar]
- 4.Diabetes mellitus: A major risk factor for cardiovascular disease. A joint editorial statement by the American Diabetes Association; the National Heart, Lung, and Blood Institute; the Juvenile Diabetes Foundation International; the National Institute of Diabetes and Digestive and Kidney Diseases; and the American Heart Association. Circulation. 1999;100:1132–3. doi: 10.1161/01.cir.100.10.1132. doi: 10.1161/01.cir.100.10.1132. [DOI] [PubMed] [Google Scholar]
- 5.Chen YY, Lin YJ, Chong E, Chen PC, Chao TF, Chen SA, et al. The impact of diabetes mellitus and corresponding HbA1c levels on the future risks of cardiovascular disease and mortality: A representative cohort study in Taiwan. PLoS One. 2015;10:e0123116. doi: 10.1371/journal.pone.0123116. doi: 10.1371/journal.pone.0123116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheung KK, Lau ES, So WY, Ma RC, Ozaki R, Kong AP, et al. Low testosterone and clinical outcomes in Chinese men with type 2 diabetes mellitus – Hong Kong diabetes Registry. Diabetes Res Clin Pract. 2017;123:97–105. doi: 10.1016/j.diabres.2016.11.012. doi: 10.1016/j.diabres.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 7.Wright AK, Kontopantelis E, Emsley R, Buchan I, Sattar N, Rutter MK, et al. Life expectancy and cause-specific mortality in type 2 diabetes: A Population-based cohort study quantifying relationships in ethnic subgroups. Diabetes Care. 2017;40:338–45. doi: 10.2337/dc16-1616. doi: 10.2337/dc16-1616. [DOI] [PubMed] [Google Scholar]
- 8.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. doi: 10.1016/s0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 9.Miller M. Dyslipidemia and cardiovascular risk: The importance of early prevention. QJM. 2009;102:657–67. doi: 10.1093/qjmed/hcp065. doi: 10.1093/qjmed/hcp065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–S45. doi: 10.1161/01.cir.0000437738.63853.7a. doi:10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 11.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult treatment panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 12.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, et al. Implications of recent clinical trials for the national cholesterol education program adult treatment panel III guidelines. Circulation. 2004;110:227–39. doi: 10.1161/01.CIR.0000133317.49796.0E. doi: 10.1161/01.cir.0000133317.49796.0e. [DOI] [PubMed] [Google Scholar]
- 13.Ramkumar S, Raghunath A, Raghunath S. Statin therapy: Review of safety and potential side effects. Acta Cardiol Sin. 2016;32:631–9. doi: 10.6515/ACS20160611A. doi: 10.6515/ACS20160611A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.US Preventive Services Task Force. Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW, Jr, et al. Statin use for the primary prevention of cardiovascular disease in adults: US preventive services task force recommendation statement. JAMA. 2016;316:1997–2007. doi: 10.1001/jama.2016.15450. doi: 10.1001/jama.2016.15450. [DOI] [PubMed] [Google Scholar]
- 15.Cholesterol Treatment Trialists' (CTT) Collaborators. Kearney PM, Blackwell L, Collins R, Keech A, Simes J, et al. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: A meta-analysis. Lancet. 2008;371:117–25. doi: 10.1016/S0140-6736(08)60104-X. doi: 10.1016/S0140-6736(08)60104-X. [DOI] [PubMed] [Google Scholar]
- 16.Lin H, Li Q, Hu Y, Zhu C, Ma H, Gao J, et al. The prevalence of multiple non-communicable diseases among middle-aged and elderly people: The shanghai changfeng study. Eur J Epidemiol. 2017;32:159–63. doi: 10.1007/s10654-016-0219-6. doi: 10.1007/s10654-016-0219-6. [DOI] [PubMed] [Google Scholar]
- 17.Dyslipidemia tCAoPaTo. Guidelines of the prevention and treatment of dyslipidemia in the adult Chinese population (in Chinese) Chin Circulaiton J. 2016;31:937–53. doi: 10.3969/j.issn.1000-3614.2016.10.001. [Google Scholar]
- 18.Society Chinese Diabetes. Guidelines for prevention and treatment of type 2 diabetes in Chinese (2013 edition) (in Chinese) Chin J Endocrinol Metab. 2014;30:893–42. doi: 10.3760/cma.j.issn.1000-6699.2014.10.020. [Google Scholar]
- 19.Yan L, Xu MT, Yuan L, Chen B, Xu ZR, Guo QH, et al. Prevalence of dyslipidemia and its control in type 2 diabetes: A multicenter study in endocrinology clinics of China. J Clin Lipidol. 2016;10:150–60. doi: 10.1016/j.jacl.2015.10.009. doi: 10.1016/j.jacl.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 20.Physicians CCoC, Committee CEBM, GSC CoC-C-VDo, Hu D. Chinese experts consensus of the omprehensive management of multiple cardiovascular risk factors in diabetic patients (in Chinese) Chin J Hypertens. 2010;18:1177–83. [Google Scholar]
- 21.Agouridis AP, Kostapanos MS, Elisaf MS. Statins and their increased risk of inducing diabetes. Expert Opin Drug Saf. 2015;14:1835–44. doi: 10.1517/14740338.2015.1096343. doi: 10.1517/14740338.2015.1096343. [DOI] [PubMed] [Google Scholar]
- 22.Lee J, Noh Y, Shin S, Lim HS, Park RW, Bae SK, et al. Impact of statins on risk of new onset diabetes mellitus: A population-based cohort study using the Korean National Health Insurance claims database. Ther Clin Risk Manag. 2016;12:1533–43. doi: 10.2147/TCRM.S117150. doi: 10.2147/tcrm.s117150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lyu Y, Niu W, Han Z, Qi Y, Sun F, Fu H, et al. Effect of community management of diabetic patients with hypertension (in Chinese) Chin J Gen Pract. 2016;15:108–13. doi: 10.3760/cma.j.issn.1671-7368.2016.02.009. [Google Scholar]
- 24.Bai H. Investiagion on the use of statin drugs in patients with dyslipidemia in the community (in Chinese) Hebei Med. 2014;9:1577–1580. doi: 10.3969/j.issn.1006-6233.2014.09.067. [Google Scholar]
- 25.Jia Y, Li L. Use of statin in type 2 diabetes patients in community hospitals (in Chinese) Med Innov China. 2012;9:91–2. doi: 10.3969/j.issn.1674-4985.2012.19.056. [Google Scholar]
- 26.Marathe PH, Gao HX, Close KL. American Diabetes Association Standards of Medical Care in Diabetes 2017. J Diabetes. 2017;9:320–324. doi: 10.1111/1753-0407.12524. doi: 10.1111/1753-0407.12524. [DOI] [PubMed] [Google Scholar]
- 27.Raymond C, Cho L, Rocco M, Hazen SL. New cholesterol guidelines: Worth the wait? Cleve Clin J Med. 2014;81:11–9. doi: 10.3949/ccjm.81a.13161. doi: 10.3949/ccjm.81a.13161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the american college of cardiology/American heart association task force on practice guidelines. J Am Coll Cardiol. 2014;63:2889–934. doi: 10.1016/j.jacc.2013.11.002. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 29.De Vera MA, Bhole V, Burns LC, Lacaille D. Impact of statin adherence on cardiovascular disease and mortality outcomes: A systematic review. Br J Clin Pharmacol. 2014;78:684–98. doi: 10.1111/bcp.12339. doi: 10.1111/bcp.12339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maningat P, Gordon BR, Breslow JL. How do we improve patient compliance and adherence to long-term statin therapy? Curr Atheroscler Rep. 2013;15:291. doi: 10.1007/s11883-012-0291-7. doi: 10.1007/s11883-012-0291-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


