ABSTRACT
The primary aim was to identify muscle-tendon-related pain in 100 patients with hip dysplasia. The secondary aim was to test whether muscle-tendon-related pain is associated with self-reported hip disability and muscle strength in patient with hip dysplasia. One hundred patients (17 men) with a mean age of 29 years (SD 9) were included. Clinical entity approach was carried out to identify muscle-tendon-related pain. Associations between muscle-tendon-related pain and self-reported hip disability and muscle strength were tested with multiple regression analysis, including adjustments for age and gender. Self-reported hip disability was recorded with the Copenhagen Hip and Groin Outcome Score (HAGOS), and muscle strength was assessed with a handheld dynamometer. Iliopsoas- and abductor-related pain were most prevalent with prevalences of 56% (CI 46; 66) and 42% (CI 32; 52), respectively. Adductor-, hamstrings- and rectus abdominis-related pain were less common. There was a significant inverse linear association between muscle-tendon-related pain and self-reported hip disability ranging from −3.35 to − 7.51 HAGOS points in the adjusted analysis (P < 0.05). Besides the association between muscle-tendon-related pain and hip extension a significant inverse linear association between muscle-tendon-related pain and muscle strength was found ranging from −0.11 to − 0.12 Nm/kg in the adjusted analysis (P < 0.05). Muscle-tendon-related pain exists in about half of patients with hip dysplasia with a high prevalence of muscle-tendon-related pain in the iliopsoas and the hip abductors and affects patients' self-reported hip disability and muscle strength negatively.
INTRODUCTION
Symptomatic hip dysplasia normally presents in early life [1] and left untreated, hip dysplasia may lead to development of early osteoarthritis [2, 3]. The aetiology of hip osteoarthritis in hip dysplasia is unknown and often described as multifactorial [2]. However, the lack of acetabular support to the femoral head [4] and the compromised passive stability of the hip joint lead to an increased mechanical pressure on the acetabular labrum and cartilage [2], and intra-articular injury has been reported as one important predisposing factor to development of osteoarthritis [2]. Labrum injury or degeneration is present in 49–83% of patients with hip dysplasia [2, 5], and causes pain at the groin and/or lateral to the hip [5, 6]. Moreover, the shallow acetabulum and the reduced weight bearing are associated with increased load on the muscles acting close to the hip joint [7, 8], and muscle-tendon-related pain may potentially coexist with intra-articular pathology.
The acetabular labrum functions as an important anterior stabilizer to the dysplastic hip [9], and the location of the iliopsoas muscle close to the capsule–labral complex enables the muscle to work as an anterior stabilizer to the hip joint [10]. The gluteus medius and minimus muscles work together with the iliopsoas muscle as important lateral stabilizers to maintain a level led pelvis during ambulation [11]. The stabilizing role of the iliopsoas and gluteus medius and minimus muscles may be increased in hip dysplasia due to the morphology of the hip joint [7, 10], and potentially higher load on the muscles may lead to overuse-related pain in the muscles and tendons.
Muscle-tendon-related pain is present in hip dysplasia [6, 12], and abnormality of the iliopsoas muscle identified as internal snapping hip has been verified in 18% using hip arthroscopy [12]. In patients with femoroacetabular impingement muscle-tendon-related pain frequently coexist with the morphology of the hip joint [13], and in sports-active subjects with long-standing groin pain, muscle-tendon-related pain has been identified with the clinical entity approach [14, 15]. In patients with hip dysplasia, however, no previous studies have systematically examined the presence of muscle-tendon-related pain in a consecutive cohort scheduled for periacetabular osteotomy.
The primary aim was to identify muscle-tendon-related pain in 100 patients with hip dysplasia in the following clinical entities: (i) iliopsoas, (ii) abductors, (iii) adductors, (iv) hamstrings, and (v) rectus abdominis. The secondary aim was to test if muscle-tendon-related pain is associated with self-reported hip disability and muscle strength in patient with hip dysplasia.
MATERIALS AND METHODS
This study complies with the Helsinki Declaration and was notified to the Danish Committee on Biomedical and Research Ethics at 14 January 2014 (5/2014). The Danish Data Protection Agency gave permission for the handling of personal data (1-16-02-47-14), and the study was registered at ClinicalTrials.gov (20140401PAO).
Subjects
In a consecutive sample, patients with bilateral or unilateral hip dysplasia were invited to participate from May 2014 to August 2015 from the Department of Orthopedics at Aarhus University Hospital in Denmark. Inclusion criteria were Wiberg’s center-edge (CE) angle <25° [16], groin pain for at least 3 months and scheduled periacetabular osteotomy (PAO) [17]. Patients were excluded based on the following criteria: (i) Calvé Perthes and epiphysiolysis, (ii) Surgery due to herniated disc and spondylodesis, (iii) Previous joint preservation procedure or arthroplasty of the hip, knee or ankle, (iv) Neurological, rheumatological or medical conditions affecting the function of the hip joint, (v) Tenotomy of the iliopsoas tendon or z-plastic of the iliotibial band and (vi) Steroid-injection in the iliopsoas tendon and/or bursa trochanterica within the last 6 weeks.
Study design
All outcomes measures were collected prior to PAO during a clinical examination. The clinical examination was completed by two experienced physical therapists (CMS and JSJ) with 5 and 7 years of experience assessing patients with hip dysplasia, respectively. The patients were randomly assessed by the two physical therapists with approximately equal distribution between the two (60:40). The examination included recording of self-reported hip disability, examination of muscle-tendon-related pain in clinical entities and hip muscle strength tests.
Self-reported hip disability
The Copenhagen Hip and Groin Outcome Score (HAGOS) questionnaire was completed by all patients prior to the clinical examinations [18]. HAGOS has shown to be a valid, reliable and responsive measure of hip disability and associated problems in young to middle-aged physically active patients with longstanding hip and/or groin pain including patients undergoing hip arthroscopy [18, 19]. HAGOS consists of six separate subscales rating hip disability from 0 to 100 points, where zero points indicates the lowest outcome [18]. The six subscales measure pain, symptoms, physical function in daily living (ADL), physical function in sports and recreation, participation in physical activity and quality of life [18].
Muscle-tendon-related pain
A standardized clinical entity approach was carried out to identify muscle-tendon-related pain in clinical entities assessed in the limb scheduled for PAO [14, 15, 20]. The standardized entity approach includes a number of pain provocation tests covered by anatomic palpation, resistance testing and passive muscle stretch (Table I). The approach includes five entities, and the entities were tested in the following order: adduction-related pain, iliopsoas-related pain, rectus abdominis-related pain, abductor-related pain and hamstring-related pain. Rectus abdominis-related pain is in the Doha consensus covered by the term inguinal-related pain [20]. Inguinal-related pain is less relevant among patients with hip dysplasia as many of these patients are women in which the inguinal canal anatomy is somewhat different from males, and therefore rectus-abdominis-related pain was the focus in the present study.
Table I.
Diagnostic criteria for each individual entity
| Clinical entities | Diagnostic criteria |
|---|---|
| Iliopsoas-related pain | Palpatory pain of the muscle through the lower lateral part of the abdomen and/or just distal of the inguinal ligament and pain with passive stretching during modified Thomas’ test [14, 20, 21] |
| Abductor-related pain | Palpatory pain at the insertion point at the greater trochanter and pain with side-lying abduction against resistance |
| Adductor-related pain | Palpatory pain at the muscle origin at the pubic bone and pain with adduction against resistance [14, 20] |
| Hamstring-related pain | Palpatory pain at the muscle origin at the tuber ischii and pain with extension against resistance |
| Rectus abdominis-related pain | Palpatory pain of the distal tendon and/or the insertion at the pubic bone, and pain at contraction against resistance [14, 20] |
Muscle strength
Isometric muscle strength tests were performed using a reliable dynamometer technique [22]. Muscle strength was tested with a handheld dynamometer (powertrack II comandor, JTECH Medical, Salt Lake City, Utah). Isometric hip adduction, abduction, flexion and extension strength were measured in the limb scheduled for PAO, and the order of the individual tests was randomized before each session to avoid systematic bias. The examiner applied resistance 5 cm proximal to the proximal edge of the lateral malleolus for hip abduction, adduction and extension. Resistance in hip flexion was performed 5 cm proximal to the proximal border of patella. In all the isometric tests, the patients exerted 5-s Maximal Voluntary Isometric Contraction (MVIC) against the dynamometer. The highest value of four repeated measurements for each test was used in the analysis. To avoid fatigue, patients rested for 30 s between each measurement. All strength values were weight-adjusted and reported as Newton meters per kilogram of the bodyweight.
Baseline characteristics
Baseline characteristics were registered using standardized questions. Pain was measured on a numeric rating scale (NRS) in rest while sitting and lying. The center-edge (CE) angle [16], Tönnis’ acetabular index (AI) angle [23] and Tönnis’ osteoarthritis grade [23] were measured by a single rater (SSJ) using anteroposterior radiographs, whereas hospital charts was used to record unilateral or bilateral hip involvement and other pathologies.
Inter-rater reliability of the test battery
Two different testers assessed muscle-tendon-related pain and muscle strength and the inter-rater reliability of these measures was investigated. Twenty-five patients were tested 6 weeks after PAO by two physiotherapists, rater A and B (CMS and JSJ), with a 2-day period between a first and second test. Each patient was randomized to whether rater A or B performed the initial testing.
Sample size
Since it was not possible to calculate the sample size based on the prevalence of muscle-tendon-related pain, we chose to calculate it based on the secondary outcome of the study. The sample size calculation was based on the HAGOS ADL subscore with an estimated difference of 11.8 points and an estimated standard deviation of 18.5 points between patients with and without muscle-tendon-related pain. The estimated difference was based on the Minimal Important Change of 11.8 points reported in a cohort study on patients with femoroacetabular impingement scheduled for hip arthroscopy [19], and the standard deviation was based on the standard deviation of the HAGOS ADL subscore of 18.5 points reported in a cohort study on patients with intra-articular hip lesions undergoing hip arthroscopy [24]. Based on a significance level of 5% and a power of 80%, 80 patients were needed, and considering the risk of dropouts, we included 100 patients.
Statistics
Normal distribution was checked with histograms and probability plots. Multiple linear regression analyses were performed with muscle-tendon-related pain as the independent variable (i.e. the sum of positive clinical entities for each patient) and each HAGOS subscale as the dependent variable (pain, symptoms, ADL, physical function in sports and recreation, participation in physical activity and quality of life). Crude and adjusted β-coefficients were estimated, and adjustments were made for age and gender. Likewise, multiple linear regression analyses were performed with muscle-tendon-related pain as the independent variable (i.e. the sum of positive clinical entities for each patient) and strength of each muscle group as the dependent variable (i.e. flexion, abduction, adduction and extension). Crude and adjusted β-coefficients were estimated, and adjustments were made for age and gender. The assumptions (independent observations, linear association, constant variance of residuals, normally distribution of residuals) for the multiple and linear regression analyses were met. The significance level was 0.05 and STATA 14 (StataCorp, College Station, TX) software package was used for data analysis.
RESULTS
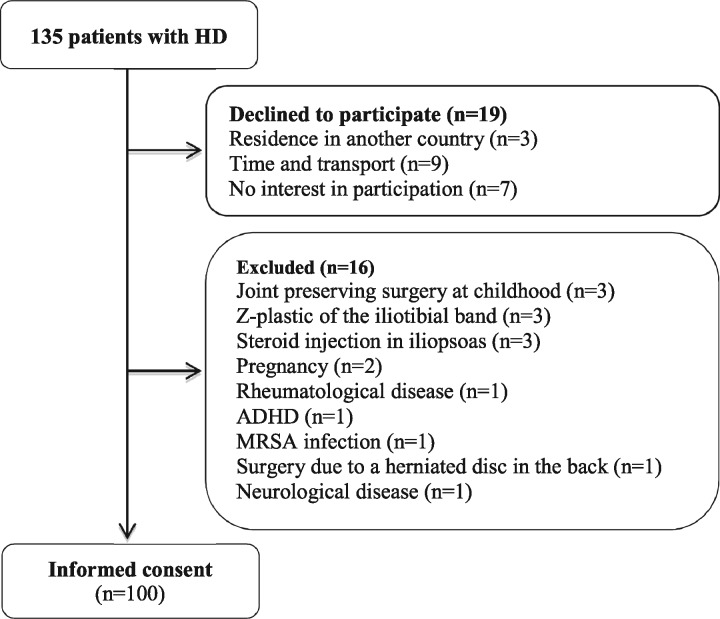
A consecutive sample of 135 patients was assessed for eligibility and out of those, 100 patients were included in this study (Fig. 1). Baseline characteristics of the included patients are reported in Table II.
Fig. 1.
Flowchart of the study process. One hundred consecutive patients with unilateral and bilateral symptoms were included from the Division of Hip Surgery, Department of Orthopedics, Aarhus University Hospital in Denmark from May 2014 to August 2015. Abbreviations: HD, hip dysplasia; ADHD, attention deficit/hyperactivity disorder; MRSA, methicillin-resistant Staphylococcus aureus.
Table II.
Baseline characteristics in 100 consecutive patients with hip dysplasia
| Outcomes | Patients (SD) |
|---|---|
| Men | 17 |
| Bilateral symptoms | 89 |
| Osteoarthritis grade 0/1 | 97/3 |
| Congenital hip dislocation | 6 |
| Age, years | 29.9 (9.2) |
| BMI, kg/m2 | 23.2 (3.0) |
| Duration of pain, years | 4.9 (5.6) |
| NRS pain lying, 0–10 | 3.1 (2.4) |
| NRS pain sitting, 0–10 | 3.8 (2.7) |
| CE angle preoperatively, degrees | 17.4 (4.7) |
| AI angle preoperatively, degrees | 13.8 (4.9) |
| HAGOS pain, 0–100 | 50.3 (18.0) |
| HAGOS symptoms, 0–100 | 49.2 (17.4) |
| HAGOS ADL, 0–100 | 55.5 (22.4) |
| HAGOS sport/recreation, 0–100 | 39.3 (20.7) |
| HAGOS participation, 0–100 | 23.0 (24.7) |
| HAGOS quality of life, 0–100 | 29.4 (14.3) |
| Hip flexion, Nm/kg | 1.2 (0.5) |
| Hip abduction, Nm/kg | 1.2 (0.4) |
| Hip adduction, Nm/kg | 1.1 (0.4) |
| Hip extension, Nm/kg | 1.8 (0.7) |
Baseline characteristics are presented as mean (SD) values and as numbers.
BMI, body mass index; CE, center-edge; AI, Tönnis’ acetabular index; HAGOS, Copenhagen hip and groin outcome score; ADL, activities of daily living; NRS, Numeric Rating Scale.
The inter-rater reliability of the standardized clinical entity approach is reported in Supplementary Appendix Table S1 and the inter-rater reliability of the muscle strength test is reported in Supplementary Appendix Table S2. Agreement between rater A and rater B ranged from 64% to 100% with kappa-coefficients ranging from 0.17 to 0.60. The ICC was >0.70 for all muscle strength measurements (0.72–0.92) and the standard error of measurement ranged between 9.45% and 14.44%.
The prevalence of muscle-tendon-related pain according to specific entities was: iliopsoas-related pain 56% (CI 46; 66), abductor-related pain 42% (CI 32; 52), adductor-related pain 14% (CI 8; 22), Hamstring-related pain 6% (CI 2; 13) and rectus abdominis-related pain 4% (CI 1; 10). Twenty-six percent of the patients reported no muscle-related pain, as defined by non-existence of pain in any of the predefined clinical entities, and the maximum number of pain-full clinical entities in individual patients was four. The distribution of muscle-tendon-related pain in clinical entities was as follows: pain in one entity (38%), pain in two entities (27%), pain in three entities (6%) and pain in four entities (3%).
Both the crude and adjusted linear regression proved an inverse linear association between muscle-tendon-related pain and the self-reported HAGOS score (Table III). Besides the adjusted association between muscle-tendon related pain and hip extension an inverse linear association between muscle-tendon-related pain and isometric hip muscle strength was found in both crude and adjusted analyses (Table IV).
Table III.
Associations between muscle-tendon-related pain and self-reported disability (n = 100)
| Crude |
Adjusted |
|||
|---|---|---|---|---|
| HAGOS points (0-100) | β Coefficient (95% CI) | P value | β Coefficient (95% CI) | P value |
| HAGOS Pain | −6.79 (−10.12; −3.46) | <0.001 | −6.90 (−10.18; −3.61) | <0.001 |
| HAGOS Symptoms | −6.26 (−9.52; −3.01) | <0.001 | −6.34 (−9.61; −3.07) | <0.001 |
| HAGOS ADL | −7.17 (−11.41; −2.93) | 0.001 | −7.51 (−11.53; −3.49) | <0.001 |
| HAGOS Sport/rec | −7.12 (−11.01; −3.23) | <0.001 | −7.39 (−11.22; −3.56) | <0.001 |
| HAGOS Participation | −5.73 (−10.55; −0.92) | 0.020 | −6.08 (−10.89; −1.27) | 0.014 |
| HAGOS Quality of life | −3.19 (−5.98; −0.41) | 0.025 | −3.35 (−6.12; −0.58) | 0.018 |
Linear regression of muscle-tendon-related pain on the self-reported HAGOS score reported as crude and adjusted β coefficients (95% confidence interval). Adjustments were made for age and gender.
ADL, activities of daily living; sport/rec, sport/recreation.
Table IV.
Associations between muscle-tendon-related pain and muscle strength (n = 100)
| Crude |
Adjusted |
|||
|---|---|---|---|---|
| Hip muscle strength (Nm/kg) | β Coefficient (95% CI) | P value | β Coefficient (95% CI) | P value |
| Flexion | −0.12 (−0.23; −0.02) | 0.021 | −0.11 (−0.21; −0.01) | 0.038 |
| Abduction | −0.10 (−0.19; −0.01) | 0.023 | −0.11 (−0.19; −0.03) | 0.011 |
| Adduction | −0.12 (−0.21; −0.03) | 0.009 | −0.12 (−0.20; −0.03) | 0.010 |
| Extension | −0.14 (−0.28; −0.01) | 0.037 | −0.12 (−0.25; 0.01) | 0.077 |
Linear regression of muscle-tendon-related pain on the muscle strength values reported as crude and adjusted β coefficients (95% confidence interval). Adjustments were made for age and gender.
DISCUSSION
Patients with symptomatic hip dysplasia are characterized by a high prevalence of muscle-tendon-related pain assessed with the clinical entity approach, and muscle-tendon-related pain evidently affects patients’ self-reported hip disability and muscle strength. Moreover, the findings suggest that muscle strength and hip disability may potentially be improved through exercise therapy focusing on reducing muscle-tendon-related lower extremity pain.
To our knowledge, no previous studies have systematically assessed presence of muscle-tendon-related pain in a large cohort of hip dysplasia patients scheduled for PAO. One cross-sectional study on 16 patients with symptomatic hip dysplasia documented pathology of the psoas tendon in three hips [12], and another cross-sectional study on hip dysplasia patients treated with PAO 24 months earlier reported non-specific soft-tissue injury in 17% [6]. In a sample of sports-active persons with long-standing groin pain muscle-tendon-related pain in clinical entities was systematically assessed [15], and adductor- and iliopsoas-related pain were reported as the most prevalent entities (58% and 36%, respectively). The higher prevalence of adductor-related pain in that study probably reflects that the population is dominated by males and soccer players opposed to our female and non-specific sports-active study population [15, 20, 25]. What was notable in our cohort was the large proportion of patients (42%) with abductor-related pain. This fits well with the results of a previous study reporting increased hip abduction and external rotation torques in patients with hip dysplasia [7]. Possibly, the higher torques reported among patients with hip dysplasia exist due to the shallow acetabulum and reduced weightbearing of the hip, where the muscles acting close to the hip may present with overuse-related pain in order to maintain a levelled pelvis during ambulation.
Abductor- and iliopsoas-related pain may potentially be improved by introducing heavy slow strength training using the side-lying hip abduction exercise and the standing hip flexion exercise [26, 27], both performed in full active range of motion [26, 27]. The heavy slow strength training including an eccentric emphasis could be an effective way of reducing muscle-tendon-related pain and improve hip disability as has been shown in patients with achilles and patellar tendinopathy [28–30]. In a randomized trial, improvement in adductor-related pain was documented in sports-active persons with longstanding groin pain [31], and in a cohort study, reduction of pain and successful return to sport were reported in runners with iliotibial band syndrome [32]. Similar exercise approaches seem feasible in patients with symptomatic hip dysplasia.
Our results showed significant associations between muscle-tendon-related pain and all six subscales of HAGOS, and the associations proved a linear relationship between the number of clinical entities with muscle-tendon-related pain and the reported HAGOS scores. This means that per added painful entity a patient experiences, the lower that patient will score in HAGOS. Patients with muscle-tendon-related pain in more than one entity is normally presented in our cohort (represent 36%). The HAGOS ADL score among these patients is minimum 15 points lower than in patients with no pain [i.e. a patient with pain in one entity reports a 7.5 points lower score than a patients with no pain, and a patient with pain in two entities reports a 15 points (2×7.5) lower score than a patient with no pain, Table III (adjusted analysis)]. A HAGOS ADL score of 15 points is higher than the Minimal Important Change of 11.8 points [19]. This means, that the impact of muscle-tendon-related pain on hip disability is of clinical relevance among patients with muscle-tendon-related pain, presenting with more than one entity. Based on this, the clinical entity approach may be used as a fast and in-expensive screening approach to select hip dysplasia patients with substantial disability in activities of daily living that is associated with the presence of muscle-tendon-related pain.
The isometric muscle strength tests likewise showed a linear and significant association between the number of clinical entities with muscle-tendon-related pain and muscle strength. This means that per added clinical entity with muscle-tendon-related pain the lower strength will that patient have. The relative lower strength values in a patient with muscle-tendon related pain in one clinical entity is approximately 10% and in two clinical entities is approximately 20%. The latter is the same as the recommended meaningful difference of 20% reported by the Cochrane Musculoskeletal Group [33] and higher than the SEM% values reported in this study, and the lower strength values indicate the relevance of muscle strength training.
Our study has a number of limitations. The analysis of inter-rater reliability showed slight to moderate agreement of the clinical entity approach. Compared with the reported inter-rater values of a previous study on sports-active people with long-standing groin pain our values are systematically lower [14]. This discrepancy may exist because the second test was performed 3 days after the first test and not on the same day, and because the kappa coefficient depends on the prevalence [34]. The prevalence of pain is low in the iliopsoas palpation lower abdomen (LA) test, the hamstrings palpation test and the hamstrings against resistance test, and the k values of these three tests should be interpreted with caution. The assessment of isometric hip muscle strength are also exposed to measurement error because of the assessor-dependent approach. Our values of the SEM% are similar but higher than the results reported in a previous study on inter-tester reliability of isometric hip muscle strength test using belt fixation [35]. However, the SEM% is lower than the 20% border reported by the Cochrane Musculoskeletal Group [33], and we included a large cohort where the measurement error has lesser impact. Based on the latter two arguments, we find the variability of our muscle strength tests acceptable. Another limitation is that we did not include a control group, and therefore we have no knowledge of the presence of muscle-tendon-related pain in healthy subjects. Presence of muscle-tendon-related pain in our study was however based on provocation of earlier experienced pain, which are probably unusual in subjects categorizing themselves as healthy. A third limitation is, that we included patients with both uni- and bilateral symptoms, which is similar to previous studies in this area [6, 36–38]. It cannot be ruled out that presence of hip dysplasia in one side of the body could have had influence on muscle-tendon-related pain of the other side.
The results of this study provide evidence that there is a high prevalence of muscle-tendon-related pain in patients with symptomatic hip dysplasia. Previously, labral tears and acetabular cartilage lesions have been described as the primary cause of pain at the groin and/or lateral to the hip [5, 6]. In the present study, we also found, a high prevalence of muscle-tendon-related pain in clinical entities dominated by a high prevalence of iliopsoas- and abductor-related pain. The implications of our results are that clinicians and scientists have to re-evaluate the cause of pain from hip dysplasia as solely being derived from the hip joint, and consider the impact of muscle-tendon-related pain on hip disability and muscle strength when assessing and planning conservative or surgical treatment in patients with hip dysplasia.
SUPPLEMENTARY DATA
Supplementary data are available at Journal of Hip Preservation Surgery online.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank physiotherapist Charlotte Møller Sørensen (CMS) for her invaluable assistance carrying out the clinical examinations.
FUNDING
Danish Rheumatism association (A3280) and Aase and Ejnar Danielsen Fund (10-000761/LPJ).
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Hartofilakidis G, Karachalios T, Stamos KG.. Epidemiology, demographics, and natural history of congenital hip disease in adults. Orthopedics 2000; 23: 823–7. [DOI] [PubMed] [Google Scholar]
- 2. McCarthy JC, Noble PC, Schuck MR. et al. Aufranc Award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res 2001; 393: 25–37. [DOI] [PubMed] [Google Scholar]
- 3. Guevara CJ, Pietrobon R, Carothers JT. et al. Comprehensive morphologic evaluation of the hip in patients with symptomatic labral tear. Clin Orthop Relat Res 2006; 453: 277–85. [DOI] [PubMed] [Google Scholar]
- 4. Mechlenburg I. Evaluation of Bernese periacetabular osteotomy: prospective studies examining projected load-bearing area, bone density, cartilage thickness and migration. Acta Orthop Suppl 2008; 79: 4–43. [DOI] [PubMed] [Google Scholar]
- 5. Ross JR, Zaltz I, Nepple JJ. et al. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med 2011; 39(Suppl): 72S–8S. [DOI] [PubMed] [Google Scholar]
- 6. Nunley RM, Prather H, Hunt D. et al. Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. J Bone Joint Surg Am 2011; 93(Suppl 2): 17–21. [DOI] [PubMed] [Google Scholar]
- 7. Skalshøi OO. Walking patterns and hip contact forces in patients with hip dysplasia. Gait Posture 2015; 42: 529; 529–33; 533. [DOI] [PubMed] [Google Scholar]
- 8. Kuroda D, Maeyama A, Naito M. et al. Dynamic hip stability, strength and pain before and after hip abductor strengthening exercises for patients with dysplastic hips. Isokinetics Exerc Sci 2013; 21: 95–100. [Google Scholar]
- 9. Henak CR, Ellis BJ, Harris MD. et al. Role of the acetabular labrum in load support across the hip joint. J Biomech 2011; 44: 2201–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fabricant PD, Bedi A, De La Torre K, Kelly BT.. Clinical outcomes after arthroscopic psoas lengthening: the effect of femoral version. Arthroscopy 2012; 28: 965–71. [DOI] [PubMed] [Google Scholar]
- 11. Grimaldi A. Assessing lateral stability of the hip and pelvis. Man Ther 2011; 16: 26–32. [DOI] [PubMed] [Google Scholar]
- 12. Domb BG, Lareau JM, Baydoun H. et al. Is intraarticular pathology common in patients with hip dysplasia undergoing periacetabular osteotomy? Clin Orthop Relat Res 2013; 472: 674–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Naal FD, Dalla Riva F, Wuerz TH. et al. Sonographic prevalence of groin hernias and adductor tendinopathy in patients with femoroacetabular impingement. Am J Sports Med 2015; 43: 2146–51. [DOI] [PubMed] [Google Scholar]
- 14. Holmich P, Holmich LR, Bjerg AM.. Clinical examination of athletes with groin pain: an intraobserver and interobserver reliability study. Br J Sports Med 2004; 38: 446–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Holmich P. Long-standing groin pain in sportspeople falls into three primary patterns, a “clinical entity” approach: a prospective study of 207 patients. Br J Sports Med 2007; 41: 247–52; discussion 252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Orthop Scand Suppl 1939; 58: 1–132. [Google Scholar]
- 17. Troelsen A, Elmengaard B, Soballe K.. A new minimally invasive transsartorial approach for periacetabular osteotomy. J Bone Joint Surg Am 2008; 90: 493–8. [DOI] [PubMed] [Google Scholar]
- 18. Thorborg K, Holmich P, Christensen R. et al. The Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist. Br J Sports Med 2011; 45: 478–91. [DOI] [PubMed] [Google Scholar]
- 19. Thomee R, Jonasson P, Thorborg K. et al. Cross-cultural adaptation to Swedish and validation of the Copenhagen Hip and Groin Outcome Score (HAGOS) for pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement. Knee Surg Sports Traumatol Arthrosc 2014; 22: 835–42. [DOI] [PubMed] [Google Scholar]
- 20. Weir A, Brukner P, Delahunt E. et al. Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med 2015; 49: 768–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Peeler J, Leiter J.. Using digital photography to document rectus femoris flexibility: a reliability study of the modified Thomas test. Physiother Theory Pract 2013; 29: 319–27. [DOI] [PubMed] [Google Scholar]
- 22. Thorborg K, Petersen J, Magnusson SP, Holmich P.. Clinical assessment of hip strength using a hand-held dynamometer is reliable. Scand J Med Sci Sports 2010; 20: 493–501. [DOI] [PubMed] [Google Scholar]
- 23. Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin Heidelberg, New York: Springer, 1987. [Google Scholar]
- 24. Kemp JL, Collins NJ, Roos EM, Crossley KM.. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med 2013; 41: 2065–73. [DOI] [PubMed] [Google Scholar]
- 25. Karlsson MK, Dahan R, Magnusson H. et al. Groin pain and soccer players: male versus female occurrence. J Sports Med Phys Fitness 2014; 54: 487–93. [PubMed] [Google Scholar]
- 26. Thorborg K, Bandholm T, Petersen J. et al. Hip abduction strength training in the clinical setting: with or without external loading? Scand J Med Sci Sports 2010; 20(Suppl 2): 70–7. [DOI] [PubMed] [Google Scholar]
- 27. Thorborg K, Bandholm T, Zebis M. et al. Large strengthening effect of a hip-flexor training programme: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 2016; 24: 2346–52. [DOI] [PubMed] [Google Scholar]
- 28. Roos EM, Engstrom M, Lagerquist A, Soderberg B.. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy – a randomized trial with 1-year follow-up. Scand J Med Sci Sports 2004; 14: 286–95. [DOI] [PubMed] [Google Scholar]
- 29. Langberg H, Ellingsgaard H, Madsen T. et al. Eccentric rehabilitation exercise increases peritendinous type I collagen synthesis in humans with Achilles tendinosis. Scand J Med Sci Sports 2007; 17: 61–6. [DOI] [PubMed] [Google Scholar]
- 30. Kongsgaard M, Kovanen V, Aagaard P. et al. Corticosteroid injections, eccentric decline squat training and heavy slow resistance training in patellar tendinopathy. Scand J Med Sci Sports 2009; 19: 790–802. [DOI] [PubMed] [Google Scholar]
- 31. Holmich P, Uhrskou P, Ulnits L. et al. Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: randomised trial. Lancet 1999; 353: 439–43. [DOI] [PubMed] [Google Scholar]
- 32. Fredericson M, Cookingham CL, Chaudhari AM. et al. Hip abductor weakness in distance runners with iliotibial band syndrome. Clin J Sport Med 2000; 10: 169–75. [DOI] [PubMed] [Google Scholar]
- 33. Maxwell L, Santesso N, Tugwell PS. et al. Method guidelines for Cochrane Musculoskeletal Group systematic reviews. J Rheumatol 2006; 33: 2304–11. [PubMed] [Google Scholar]
- 34. Sim J, Wright CC.. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther 2005; 85: 257–68. [PubMed] [Google Scholar]
- 35. Thorborg K, Bandholm T, Holmich P.. Hip- and knee-strength assessments using a hand-held dynamometer with external belt-fixation are inter-tester reliable. Knee Surg Sports Traumatol Arthrosc 2013; 21: 550–5. [DOI] [PubMed] [Google Scholar]
- 36. Pedersen EN, Simonsen EB, Alkjaer T, Soballe K.. Walking pattern in adults with congenital hip dysplasia: 14 women examined by inverse dynamics. Acta Orthop Scand 2004; 75: 2–9. [DOI] [PubMed] [Google Scholar]
- 37. Sucato DJ, Tulchin K, Shrader MW. et al. Gait, hip strength and functional outcomes after a Ganz periacetabular osteotomy for adolescent hip dysplasia. J Pediatr Orthop 2010; 30: 344–50. [DOI] [PubMed] [Google Scholar]
- 38. Jacobsen JS, Nielsen DB, Sorensen H. et al. Changes in walking and running in patients with hip dysplasia. Acta Orthop 2013; 84: 265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.