Abstract
Purpose:
Despite therapeutic effects of radioiodine in patients with differentiated thyroid cancer, there are some disadvantages due to harmful radiation to other tissues. According to the current guidelines, patients are recommended to drink lots of water and frequent voiding to reduce the amount of 131I in the body. This study was designed to assess the impact of the amount of liquid intake on reduction of the measured dose rate of radioiodine-treated patients.
Materials and Methods:
A total of 42 patients with differentiated thyroid cancer without metastasis who had undergone total thyroidectomy and had been treated with radioiodine were selected. The patients were divided into two groups according to the amount of their fluid intake which was measured during the first 48 h after 131I administration. In all patients, the dose rate was measured immediately and 48 h after iodine administration.
Results:
Each group included 21 patients. Dose rate ratio (the ratio of the second dose rate to the first dose rate) and dose rate difference ratio (the ratio of the difference between the two measured dose rates to the first dose rate) were calculated for each patient. Despite the significant difference in the amount of the liquid drunk, no statistically significant difference was seen between the different groups in parameters of dose-rate ratio and dose-rate difference ratio.
Conclusion:
Higher fluid intake (>60 ml/h in our study) alone would not effectively reduce the patient's radiation dose rate at least not more than a well-hydrated state. It seems that other interfering factors in the thyroidectomized patients may also have some impacts on this physiologic process.
Keywords: Differentiated thyroid cancer, dose rate, radioiodine, urinary iodine excretion
Introduction
Thyroid cancer is the most common cancer of the endocrine system with an increasing incidence during the past decades.[1] Differentiated thyroid cancer (DTC) is categorized into papillary and follicular thyroid carcinomas which comprise 80% and 10%–20% of all thyroid malignancies, respectively.[2]
The management of DCT is total thyroidectomy to remove the thyroid cancer cells followed by radioiodine (131I) ablation as an adjuvant therapy to destroy the remnant thyroid cancer cells.[3,4,5,6,7,8] Using radioactive iodine for thyroid remnant ablation and metastasis treatment in patients with DTC is still a well-accepted and effective method after more than six decades. Emitting 806 keV beta particles, 131I can destroy the remnant thyroid tissue and remaining cancer cells. For the same reason, 131I can be harmful for the other organs that uptake, metabolize or excrete the radioiodine as well.[9,10,11,12] Radioactive iodine is almost completely absorbed from the gastrointestinal tract when administered orally. Then, it would be absorbed in the remnant thyroid tissue, salivary glands, and stomach mucosa. The main excretion route of iodine is through the urinary system. To reduce the side effects of radioactive iodine and also reduce hospitalization of patients, attempts have been made to accelerate the excretion of iodine from the body and consequently lower the total radiation dose of patients.[11]
Since urinary excretion accounts for the main way of radioiodine excretion from the body, many guidelines and experts recommend drinking lots of water and voiding on a regular basis to reduce the total dose of 131I.[13,14,15] However, there is no relevant study in the literature to assess how much liquid is sufficient to effectively reduce total radiation dose rate. The objective of this study was to assess the impact of the amount of liquid intake on reduction of the measured dose rate of radioiodine treated patients at the distance of 1 m.
Materials and Methods
A total of 62 patients with DTC and without distant metastasis who had undergone total thyroidectomy and were candidates for radioiodine ablation at Nuclear Medicine Department of Shiraz Namazi hospital during 2014–2015 were selected to be included in this study. The patients who had vomiting after administration were excluded from the study. Finally, 42 patients participated in this study. All patients were asked to have a well-fluid intake, take shower 4 times, and have the same diet with frequent voiding during the course of admission. For all patients, the amount of fluid intake and frequency of voiding were measured during the first 48 h after 131I administration for all patients.
The dose of 100–200 mCi of radioiodine was administered orally to the patients. For all patients, the dose rate at 1 m which is the recommended criteria for the discharge of patients[16] was measured by a gamma ray dosimeter (Radiation alert, monitor 5) at two different times, immediately (first dose rate) and 48 h (second dose rate) after 131I administration. The patients were asked to void immediately before each dose rate measurement. To eliminate the interfering effect of the difference in administered radioiodine activity and amount of thyroid remnant, two factors were calculated to normalize the dose rate reduction for each patient: (1) Ratio of the second dose rate to the first dose rate as dose rate ratio, (2) ratio of the differences of two dose rates to the first dose rate as dose rate difference ratio. According to the amount of fluid intake, the patients were categorized into both groups with fluid intake <60 ml/h and ≥60 ml/h while each consisted of 21 patients.
All statistical analyses were performed using a commercially available software program (Statistical Package for the Social Sciences, version 21; SPSS, Chicago, Illinois, USA). The normality distribution of the differences was assessed separately in each group, using the Shapiro–Wilk test of normality in which the P > 0.05 represented the normal distribution. To determine whether there were any significant differences between the means of groups, we used the independent t-test, and to determine the correlation of the amount of liquid intake and each factor, we used Pearson's correlation test.
Results
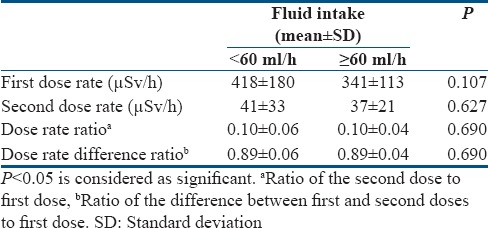
The baseline characteristics of each group's members are shown in Table 1. The mean age and fluid intake in all patients were 35 ± 11 and 61 ± 27, respectively. The averages of voiding frequency during the study and the administered radioiodine activity (mCi) were not statistically different between the two groups [Table 1]. Comparison of the two groups with ANOVA test revealed a significant difference neither for the dose rate ratio (0.10 ± 0.06 vs. 0.10 ± 0.04 in group with higher liquid intake vs. group with lower liquid intake, respectively) nor for the dose rate difference ratio (0.89 ± 0.06 vs. 0.89 ± 0.04 in group with higher liquid intake vs. group with lower liquid intake, respectively) between the groups [Table 2]. Pearson's correlation analysis also showed no statistically significant correlation between drinking more water and dose rate reduction as an decrease in the calculated dose rate ratio and dose rate difference ratio (r = −0.034, P = 0.831).
Table 1.
Baseline characteristics of patients in each group
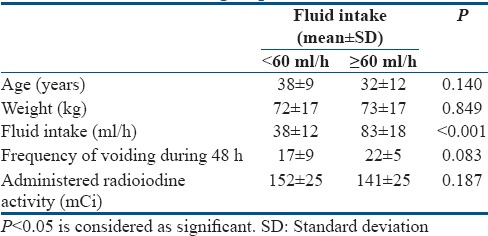
Table 2.
Comparison of the two groups for the radiation dose rate parameters
Discussions
Since the urinary secretion of iodine is known as the main root of iodine excretion from the body, current guidelines recommend excessive fluid intake after radioiodine administration to enhance the urinary flow and consequently radioiodine excretion to remove harmful radiation from the body more rapidly.[16] However, our study revealed that increasing the amount of fluid intake above the level of regular fluid intake by the patients did not simply result in the reduction of measured dose rate which is widely used as a criterion for safe discharge of patients from hospital.[16] There are many studies in the literature assessing the metabolism and excretion of iodine in the body, most of which showing that more than 80% of serum iodine is excreted through the urinary system;[17] however, few of them were focusing on the patients who had undergone thyroidectomy and were candidates for radioiodine ablation.[18] Regarding the altered metabolism of iodine, it would be of great importance not to directly extend these results to this group of patients. On the other hand, since the majority of these patients are in a hypothyroid state which can reduce the renal excretory function,[19,20] enhancing the urinary flow would not be as effective as in the normal euthyroid patients.
In addition, the patients are always recommended that they should be on a low-iodine diet for 2 weeks before radioiodine ablation to deplete the iodine sources of the body for better thyroid iodine absorption which itself can lead to reduction of urinary iodine loss.[21]
Besides the mentioned points, some researchers have also stated that water diuresis and increase in urinary flow do not result in more urinary iodine excretion,[22,23] whereas in an animal study, this has been found that dehydration can significantly reduce urinary iodine excretion in rabbits.[24] Another study conducted by Johner et al. revealed that higher urinary volume due to increasing the liquid intake in a physiologic range leads to additional urinary excretion.[25] Comparison of these results with those of our study showed that although inadequate fluid intake and dehydration can reduce the iodine excretion, increasing the fluid intake, and urinary flow above the physiologic range (over hydration) would not significantly increase urinary iodine excretion.
Some authors have recommended that overhydration not only can increase iodine excretion but also may promote the frequency of voiding and subsequent reduction in the duration of activity retention in the bladder.[16] Since we measured the dose rate just at two time points and immediately after voiding, the effect of retention of activity as an accumulated radiation dose rate to the patient could not be evaluated in this study though the frequency of voiding in both groups was not statistically different. It seems that voiding on a regular basis in all patients should be recommended regardless of the intake amount because the higher fluid intake in our study does not necessarily result in higher frequency of voiding.
Finally, this is suggested that although the dehydration should be avoided in the patients who receive radioiodine, higher volume intake just over the physiologic rate seems to be ineffective in these patients; this could be even intolerable in some patients, especially the elderly ones and those with cardiac, liver or renal problems.
Limitations
In this study, the patients were allowed to drink any kind of fluid they desired including tea, coffee, fruit juice, sweet and salty nonalcoholic beverages, and carbonated drinks which may have different diuretic effects[26] though the water was the most popular liquid. Although these differences may somehow interfere with our results, it could be more practical and realistic not to restrict the patients to some specific types of fluid. Furthermore, the relatively small sample size and the observational nature of our study limited us in precise analysis of the results. In addition, higher fluid intake group in our study was limited to the mean of 83 ± 18 ml/h, and the effect of more fluid intake above this level which may have different effect, could not be evaluated in this study. Further dedicated prospective biochemical studies on a larger population are still needed to confirm and explain these results.
Conclusion
This should be stated that higher fluid intake (>60 ml/h, mean 83 ml/h) alone would not effectively reduce the patient's radiation dose rate at least not more than a well-hydrated state. It seems that other factors such as baseline serum iodine level, amount of remnant functioning thyroid tissue, and the presence of hypothyroid state in the thyroidectomized patients may also have some impact on this physiologic process.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This work was supported by a grant from Nuclear Medicine and Molecular Imaging Research Center, Shiraz University of Medical Sciences, Shiraz, Iran (reference No.6122). The authors would like to thank the staff of nuclear medicine department of Namazi Teaching hospital for their cooperation.
References
- 1.Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: Update on epidemiology and risk factors. J Cancer Epidemiol. 2013;2013:965212. doi: 10.1155/2013/965212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26:1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simpson WJ, McKinney SE, Carruthers JS, Gospodarowicz MK, Sutcliffe SB, Panzarella T, et al. Papillary and follicular thyroid cancer. Prognostic factors in 1,578 patients. Am J Med. 1987;83:479–88. doi: 10.1016/0002-9343(87)90758-3. [DOI] [PubMed] [Google Scholar]
- 4.Ravishankar U, Pande S, Savita N. I-131 in the management of differentiated thyroid cancer - An update on current recommendations and practices. Apollo Med. 2009;6:347–54. [Google Scholar]
- 5.Fatourechi V, Hay ID. Treating the patient with differentiated thyroid cancer with thyroglobulin-positive iodine-131 diagnostic scan-negative metastases: Including comments on the role of serum thyroglobulin monitoring in tumor surveillance. Semin Nucl Med. 2000;30:107–14. doi: 10.1053/nm.2000.4600. [DOI] [PubMed] [Google Scholar]
- 6.Aktolun C, Goldsmith SJ. Nuclear medicine therapy: Principlesand clinical applications. New York, NY: Springer Science and Business Media; 2012. [Google Scholar]
- 7.Sherma SI. Thyroid carcinoma. The Lancet. 2003;361:501–11. doi: 10.1016/s0140-6736(03)12488-9. [DOI] [PubMed] [Google Scholar]
- 8.Haghighatafshar M, Khajehrahimi F. Hiatal hernia uptake of iodine-131 mimicking mediastinal metastasis of papillary thyroid carcinoma. Indian J Nucl Med. 2015;30:347–9. doi: 10.4103/0972-3919.164020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tuttle RM. Differentiated thyroid cancer: Radioiodine treatment. UpToDate. 2015 [Google Scholar]
- 10.Ravichandran R, Al Balushi N. Radioactive 131Iodine body burden and blood dose estimates in treatment for differentiated thyroid cancer by external probe counting. World Journal of Nuclear Medicine? 2016;15:153–160. doi: 10.4103/1450-1147.174701. doi:10.4103/1450-1147.174701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Nostrand D. The benefits and risks of I-131 therapy in patients with well-differentiated thyroid cancer. Thyroid. 2009;19:1381–91. doi: 10.1089/thy.2009.1611. [DOI] [PubMed] [Google Scholar]
- 12.Piruzan E, Haghighatafshar M, Faghihi R, Entezarmahdi SM. Calculation of blood dose in patients treated with 131I using MIRD, imaging, and blood sampling methods. Medicine (Baltimore) 2016;95:e3154. doi: 10.1097/MD.0000000000003154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bushberg JT, Boone JM. Philadelphia, PA, USA: Lippincott Williams & Wilkins; 2011. The Essential Physics of Medical Imaging. [Google Scholar]
- 14.Hamizah N, Juliana M, Waidi A, Ismalina S, Ahmad Z. Surface contamination in skin and room during hospitalization of thyroid cancer patient receiving radioiodine ablation. JDMS. 2012;2:27–33. [Google Scholar]
- 15.Hewamanna R, Loganathan N, Perera D. Releasing thyroid cancer patients from the hospital based on dose rate measurement after 131I activity administration. J Natl Sci Found Sri Lanka. 2014;42:137–141. [Google Scholar]
- 16.American Thyroid Association Taskforce On Radioiodine Safety. Sisson JC, Freitas J, McDougall IR, Dauer LT, Hurley JR, et al. Radiation safety in the treatment of patients with thyroid diseases by radioiodine 131I: Practice recommendations of the american thyroid association. Thyroid. 2011;21:335–46. doi: 10.1089/thy.2010.0403. [DOI] [PubMed] [Google Scholar]
- 17.Keating FR, Jr, Power MH. The urinary excretion of radioiodine in various thyroid states. J Clin Invest. 1947;26:1138–51. [PubMed] [Google Scholar]
- 18.Matović M. Preparation for radioiodine therapy: How to increase therapeutic efficacy and accelerate unbound radioiodine excretion. Vojnosanit Pregl. 2013;70:504–10. doi: 10.2298/vsp1305504m. [DOI] [PubMed] [Google Scholar]
- 19.Saini V, Yadav A, Arora MK, Arora S, Singh R, Bhattacharjee J, et al. Correlation of creatinine with TSH levels in overt hypothyroidism-A requirement for monitoring of renal function in hypothyroid patients? Clin Biochem. 2012;45:212–4. doi: 10.1016/j.clinbiochem.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 20.van Hoek I, Daminet S. Interactions between thyroid and kidney function in pathological conditions of these organ systems: A review. Gen Comp Endocrinol. 2009;160:205–15. doi: 10.1016/j.ygcen.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 21.Harrison MT. Iodine balance in man. Postgrad Med J. 1968;44:69–71. doi: 10.1136/pgmj.44.507.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Giebisch G, Macleod MB, Kavaler F. Renal excretion of radioiodide in the dog. Am J Physiol. 1956;187:529–35. doi: 10.1152/ajplegacy.1956.187.3.529. [DOI] [PubMed] [Google Scholar]
- 23.Bricker NS, Hlad CJ Jr. Observations on the mechanism of the renal clearance of I131. J Clin Invest. 1955;34:1057–72. doi: 10.1172/JCI103155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reichlin S, Koussa M.G. The effect of starvation and dehydration on radioiod1ne excretion following injections of I labeled thyroxine. Endocrinology. 1958;62:868–72. doi: 10.1210/endo-62-6-868. [DOI] [PubMed] [Google Scholar]
- 25.Johner SA, Shi L, Remer T. Higher urine volume results in additional renal iodine loss. Thyroid. 2010;20:1391–7. doi: 10.1089/thy.2010.0161. [DOI] [PubMed] [Google Scholar]
- 26.Wemple RD, Lamb DR, McKeever KH. Caffeine vs. caffeine-free sports drinks: Effects on urine production at rest and during prolonged exercise. Int J Sports Med. 1997;18:40–6. doi: 10.1055/s-2007-972593. [DOI] [PubMed] [Google Scholar]


