Sir,
Pseudocirrhosis is an unusual complication that develops postchemotherapy, typically in patients of breast cancer with multiple liver metastases. We present a recent such case from our institute.
A 35-year-old female patient with carcinoma of the right breast had undergone right modified radical mastectomy and adjuvant chemotherapy and radiotherapy. She had hormone receptor-positive and Her2-negative disease. She subsequently presented with increasing bone pain 4 years later. An 18F-fludeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) done at that point of time showed extensive liver metastases with multiple skeletal lesions [Figure 1a and b]. The patient was treated with palliative radiotherapy for painful sternal and vertebral bone metastases. Palliative chemotherapy was started with gemcitabine and carboplatin for two cycles, after which chemotherapy was stopped due to poor hematologic tolerance. Evaluation revealed bone marrow involvement with disease. She was put on hormonal therapy with letrozole. Subsequent 18F-FDG PET/CT was done 7 months later as the patient presented with distention of the abdomen and ascites. The CT showed significant loss of volume of the liver with nodular contour and capsular retraction over multiple places. Evidence of portal hypertension was also noticed in the form of collateral vessels and ascites along with the development of splenomegaly. Multiple new lytic bone lesions were also noticed in the PET scan [Figure 1c and d]. Subsequent attempts at chemotherapy with cisplatin and capecitabine commensurate with the liver dysfunction and the bone marrow compromise that the patient had was also ill-tolerated. She had progressive liver failure and succumbed to the disease 10 months after the diagnosis of the metastatic disease.
Figure 1.
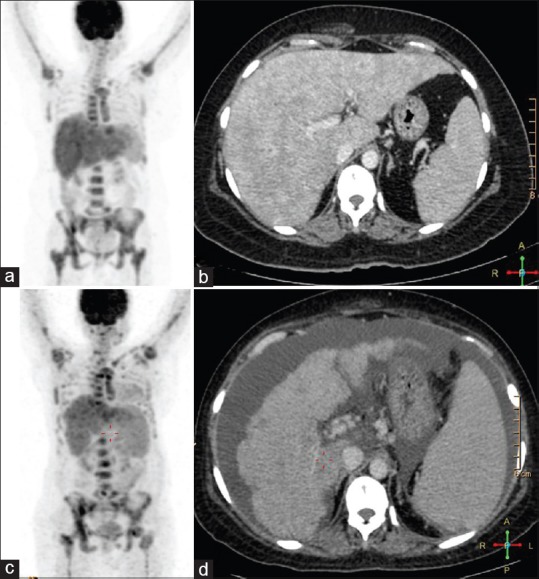
(a) Whole-body PET image of the patient with extensive liver and skeletal hypermetabolism. (b) Contrast-enhanced computed tomography image done as a part of the positron emission tomography computed tomography demonstrating the multiple enhancing liver metastases. (c) Positron emission tomography done at a later point of time showing shrunken liver with multiple new foci of metabolic activity within the skeleton. (d) contrast-enhanced computed tomography done as part of the positron emission tomography computed tomography done at a later point of time in the course showing significant volume loss of liver with nodular surface and ascites, collateral vessels at the porta, and splenomegaly – all features of hepatic dysfunction and portal hypertension
Development of nodular contour of the surface of the liver is termed pseudocirrhosis. However, this term is an apparent misnomer as the patients develop all the signs of liver cirrhosis with hepatic dysfunction, portal hypertension with lobular contour, shrinking of the liver capsular retraction, and splenomegaly. Young et al.[1] showed that nodular regeneration of the liver with compression and atrophy of intervening parenchyma without fibrosis could be a possible factor for this appearance. However, few studies have also demonstrated desmoplastic reaction surrounding the tumor as a possible cause.[2] In another case report, Christina et al.[3] gave histological evidence of intrasinusoidal infiltration of the tumors resulting in features of cirrhosis in a patient with metastatic breast cancer. Direct toxic effect of the chemotherapeutic drugs is also a possible mechanism. Qayyum et al.[4] have shown that morphological changes in the liver can be appreciated in approximately 75% of the patients of breast cancer with liver metastases following chemotherapy. However, development of portal hypertension is infrequent. In their extensive research, Adike et al.[5] have enlisted only eighteen publications in addition to theirs that describe this phenomenon. The cases described in the literature show increased mortality and morbidity for this subset of the patients, as exemplified by our case, and demonstration of this phenomenon in imaging should alert the treating clinician.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Young ST, Paulson EK, Washington K, Gulliver DJ, Vredenburgh JJ, Baker ME, et al. CT of the liver in patients with metastatic breast carcinoma treated by chemotherapy: Findings simulating cirrhosis. AJR Am J Roentgenol. 1994;163:1385–8. doi: 10.2214/ajr.163.6.7992734. [DOI] [PubMed] [Google Scholar]
- 2.Nascimento AB, Mitchell DG, Rubin R, Weaver E. Diffuse desmoplastic breast carcinoma metastases to the liver simulating cirrhosis at MR imaging: Report of two cases. Radiology. 2001;221:117–21. doi: 10.1148/radiol.2211001754. [DOI] [PubMed] [Google Scholar]
- 3.Fournier C, Tisman G, Kleinman R, Park Y, Macdonald WD. Clinical evidence for overcoming capecitabine resistance in a woman with breast cancer terminating in radiologically occult micronodular pseudo-cirrhosis with portal hypertension: A case report. J Med Case Rep. 2010;4:112. doi: 10.1186/1752-1947-4-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qayyum A, Lee GK, Yeh BM, Allen JN, Venook AP, Coakley FV, et al. Frequency of hepatic contour abnormalities and signs of portal hypertension at CT in patients receiving chemotherapy for breast cancer metastatic to the liver. Clin Imaging. 2007;31:6–10. doi: 10.1016/j.clinimag.2006.09.028. [DOI] [PubMed] [Google Scholar]
- 5.Adike A, Karlin N, Menias C, Carey EJ. Pseudocirrhosis: A Case series and literature review. Case Rep Gastroenterol. 2016;10:381–91. doi: 10.1159/000448066. [DOI] [PMC free article] [PubMed] [Google Scholar]


