Abstract
One of the most common differentials for the acute scrotum is an epididymo-orchitis (EO), which can mimic the presentation of testicular torsion. We present a case of a 37-year-old man presented to the Emergency department with a 3-day history of progressive left testicular pain. A Doppler ultrasound was done which revealed increased flow to the left testicle with no evidence of testicular torsion and he was discharged. He was re-admitted with worsening pain and a repeat scan showed that the penile arterial diastolic flow had reversed, indicating testicular infarction. This was confirmed at exploration and an orchidectomy was performed. EO causing severe complications is an uncommon manifestation of a common disorder. Features suggesting a lack of response to antibiotics include sepsis, pronounced scrotal oedema, severe testicular pain and scrotal wall inflammation. The presence of a positive urine culture has also been highlighted as a poor prognostic factor.
INTRODUCTION
The acute scrotum can provide many diagnostic challenges to the Emergency Room Physician, Radiologist and Urologist. To compound the diagnostic dilemma, pathologies such as testicular torsion are time sensitive with a delay in diagnosis being potentially catastrophic to the young male. One of the commonest differentials for the acute scrotum is an epididymo-orchitis (EO), which can mimic the presentation of testicular torsion. This infectious pathology is often managed as an outpatient with good results; rarely requiring surgical intervention.
Testicular infections are usually treated with enteral or parenteral antibiotics, with little to no morbidity, it must be borne in mind that the progression to further complications can occur leading to greater morbidity and testicular loss. Few case reports and case series have been written highlighting acute testicular infarcts progressing from routine epididymal and testicular infections. Fehily et al. presented a review of seven published cases and presented two case reports [1]. The series by Mittemeyer et al. of 610 cases suggested a rate of ~3–5% [2] and another paper by Fernández-Pérez quoted a figure of 3.5% [3]. There is little available evidence to guide the management in these complicated infections if they progress to testicular loss.
CASE REPORT
We present a case of a 37-year-old man presented to the Emergency department with a 3-day history of left testicular pain. He had no chronic illnesses and was not immunocompromised. The pain was associated with mild storage lower urinary tract symptoms. He was sexually active but had no previous sexually transmitted diseases and no urethral discharge. He had no history of trauma and had not had any similar episodes before. His examination revealed a swollen tender left testicle; equivocal for testicular torsion. A Doppler ultrasound was done which revealed increased flow to the left testicle with no evidence of testicular torsion (Fig. 1). The patient was subsequently discharged on oral ciprofloxacin, analgesia and instructed to perform scrotal elevation. The patient subsequently presented 6 h later with worsening of his pain and was reviewed and re-imaged with a color Doppler. At this time, imaging findings demonstrated reversal of diastolic flow a feature suggesting impending infarction, along with other features of acute inflammation (Fig. 2). The patient was taken to the operating room and a scrotal exploration was performed. No evidence of torsion was identified. A congested testicle was observed. No evidence of infarction or abscess formation was seen. Day 1 post-operatively the patient continued to have left sided testicular pain, now associated with lower abdominal pain. A KUB ultrasound and a repeat scrotal ultrasound were performed. These demonstrated absent flow in the left testicle (Fig. 3). On repeat exploration a dusky blue testicle was found and a left orchidectomy performed. Testicular histopathological analysis demonstrated features suggestive of acute necrotizing inflammation of the testes and epididymis as well as the spermatic cord and its vessels. Cultures of the urine subsequently showed significant growth of Escherichia coli.
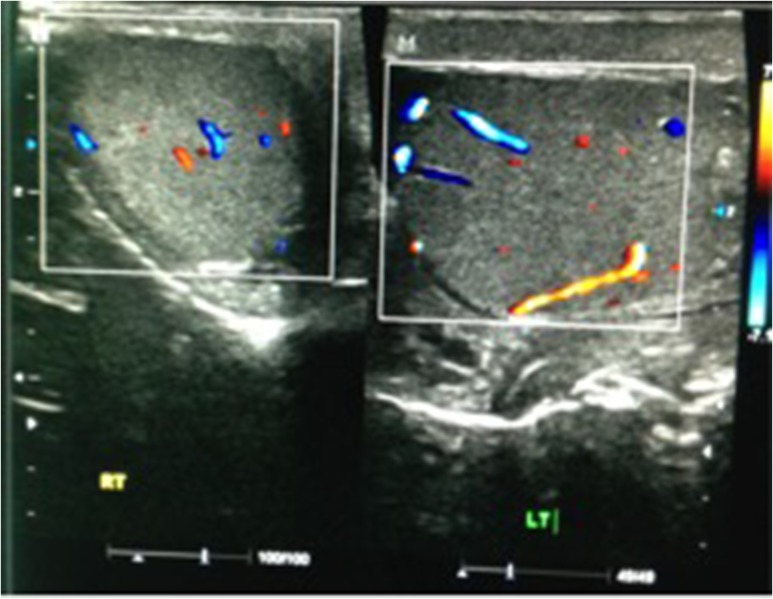
Figure 1:
Ultrasound scan showing both testicles at initial presentation, with increased flow on the left side, indicative of EO.
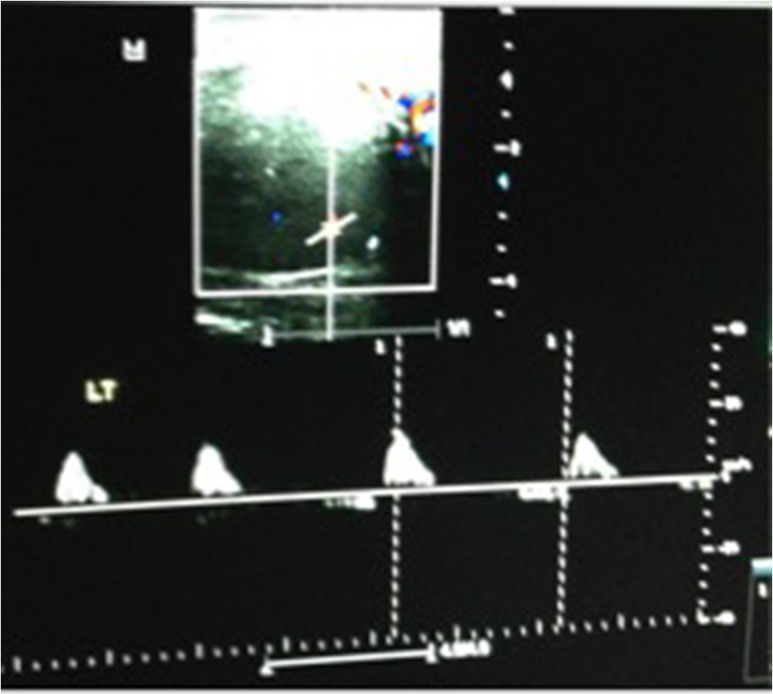
Figure 2:
Repeat ultrasound scan 6 h later showing reversal of diastolic flow.
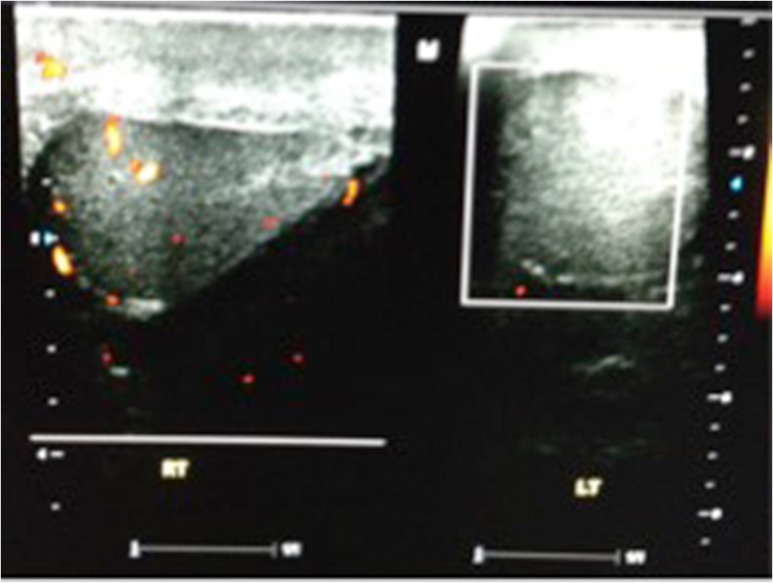
Figure 3:
Repeat ultrasound scan showing no flow within the left testicle.
DISCUSSION
Documented rates of EO are around 50 per 100 000 outpatient visits, with comparable rates in all ages [4]. Cases in men younger than 35 are commonly associated with a sexual transmitted infection, while the reverse is true over 35 years of age [5]. EO causing severe complications is uncommon with a study by Desai et al. looking at 33 men suffering with EO finding a complication rate of 39%, with complications including: suppurative necrosis, late atrophy as well as infarction [6]. Mittemeyer et al. quoted an incidence of scrotal abscess formation of 3–5% [2].
With such rich supply the likelihood for infarction of this organ should be very low. The pathogenesis of a testicular infarct due to EO is poorly understood. In the event when it occurs a number of factors are postulated to contribute: inflammatory infiltration causing compression of the spermatic cord, thrombosis secondary to venous congestion and bacterial exotoxins are all thought to play a role [1]. Radionuclide imaging of the scrotum has demonstrated compromised testicular blood flow in severe cases of epididymitis [7]. This is contrary to the hyperaemia and vascular congestion associated with an acute inflammatory process.
Antibiotic therapy in EO is usually with a combination of a third generation Cephalosporin and/or a Quinolone. Doxycycline may be added to cover Chlamydia Trachomatis. However, how can one differentiate between routine EO, which will resolve well with basic management, and the more sinister EO, which can cause more serious consequences. Strong evidence to support clinical features, which may predict a worse outcome, is limited. Features suggesting a lack of response to antibiotics include sepsis, pronounced scrotal oedema, severe testicular pain and scrotal wall inflammation [8]. The presence of a positive urine culture has been cited as being a factor leading to increased complications such as hydrocele, abscess formation, testicular infarction and infertility [9]. The confirmation of this is usually too delayed to guide preventative surgical intervention. In our case, refractory pain and a high index of suspicion prompted re-imaging and re-exploration.
Further theoretical management options include anticoagulantion, antiplatelet or thrombolytic drugs. Testicular and or spermatic cord fasciotomy in an attempt to salvage the testicle is also a consideration. If the tunica vaginalis is considered as a tough unyielding layer, then a compartment syndrome like picture may well occur and surgical decompression may offer a chance at testicular salvage. Animal studies in rats have shown a statistically significant increase in testicular size and volume using this technique in torted rodent testicles compared with a control group [10]. Other authors have decompressed the epididymis and the spermatic cord in isolated cases with varying successes [7]. Testicular fasciotomy may seem like an excessive option to an orchidectomy however; in a patient with a solitary testis or sub-fertility a decision to perform an orchidectomy may render reproduction significantly less successful.
Unfortunately strong evidence to answer these questions will be unlikely to be provided in the near future. The rarity of this phenomenon, the unlikelihood of making the diagnosis at the point of reversal of diastolic flow and lack of guidelines will limit standardized approaches to managing this phenomenon.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Fehily SR, Trubiano JA, McLean C, Teoh BW, Grummet JP, Cherry CL, et al. Testicular loss following bacterial epididymo-orchitis: case report and literature review. Can Urol Assoc J 2015;9:E148–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mittemeyer BT, Lennox KW, Borski AA. Epididymitis: a review of 610 cases. J Urol 1966;95:390–2. [DOI] [PubMed] [Google Scholar]
- 3. Fernández-Pérez GC, Tardáguila FM, Velasco M, Rivas C, Dos Santos J, Cambronero J, et al. Radiologic findings of segmental testicular infarction. Am J Roentgenol 2005;184:1587–93. [DOI] [PubMed] [Google Scholar]
- 4. Chorba T, Scholes D, Bluespruce J, Operskalski BH, Irwin K. Sexually transmitted diseases and managed care: an inquiry and review of issues affecting service delivery. Am J Med Qual 2004;19:145–56. [DOI] [PubMed] [Google Scholar]
- 5. Berger RE, Alexander ER, Harnisch JP, Paulsen CA, Monda GD, Ansell J, et al. Etiology, manifestations and therapy of acute epididymitis: prospective study of 50 cases. J Urol 1979;121:750–4. [DOI] [PubMed] [Google Scholar]
- 6. Desai KM, Gingell JC, Haworth JM. Fate of the testis following epididymitis: a clinical and ultrasound study. J R Soc Med 1986;79:515–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vordermark JS 2nd, Favila MQ. Testicular necrosis: a preventable complication of epididymitis. J Urol 1982;128:1322–4. [DOI] [PubMed] [Google Scholar]
- 8. Witherington R, Harper WM 4th. The surgical management of acute bacterial epididymitis with emphasis on epididymotomy. J Urol 1982;128:722–5. [DOI] [PubMed] [Google Scholar]
- 9. Luzzi GA, O’Brien TS. Acute epididymitis. BJU Int 2001;87:747–55. [DOI] [PubMed] [Google Scholar]
- 10. Quintaes IP, Tatsuo ES, Paulo DN, Musso C, Boasquevisque PC. Decompressive fasciotomy in testicular torsion of the spermatic cord in rats. Acta Cir Bras 2013;28:423–9. [DOI] [PubMed] [Google Scholar]