Abstract
Lipomas of gastrointestinal (GI) tract could occur at any anatomical level and represent 1–2% of all GI tumours. Amongst them, <2% are noted in jejunum and almost all in later decade of life with varied and non-specific symptoms. Their intussusception is even rarer and mostly present with full obstructive symptoms. Herein, we would like to report a successfully treated case of subtle jejunal lipomata with intussusception in an otherwise healthy a 21-year-old female.
INTRODUCTION
Gastrointestinal (GI) lipomas are benign and slow growing tumours of submucosal origin. Their peak incidence is at fifth to seventh decade of life with female predominance. Their presentation is varied, vast and non-specific [1]. In order of prevalence they commonly present with mild to severe GI bleed, abdominal pain, constipation, diarrhoea and intussusception. They can occur at any part of GI anatomy and are unusual entity representing 1–2% of all GI tumours. Amongst them, 64% are seen in the colon, 4% in the second part of the duodenum and <2% are noted in the jejunum [2]. Jejunal lipomas are usually solitary but in 5% of cases they could be multiple in nature. The jejunal lipomas are incidentally detected during investigation for other abdominal aetiologies and are mainly asymptomatic [1, 2]. Their invagination and subsequent intussusception in association with subtle symptoms in second decade of life, are significantly rare. In fact, the search of literature in English language revealed five cases of jejunal intussusception of which none occured in second decade. Herein, we would like to report a successfully treated case of subtle jejunal lipoma with intussusception in a 21-year-old female with 6-month follow-up.
CASE REPORT
A 21-year-old lady with past medical history of psoriasis, urolithiasis and allergic rhinitis presented with 4-week history of colicky and intermittent epigastric pain associated with single and isloated episode of vomiting and diarrhoea. On presentation, she was found to be afebrile with normal observations. Clinical examination revealed, soft, non-tender abdomen with normal haematological markers. Ultrasonography of the abdomen demonstrated a hyperechoic lesion within the lumen of jejunum measuring ~1.6 cm (transverse) × 3.6 cm (longitudinal) in size, raising the suspicion of polypoid tumour and intussusception. Magnetic resonance (MR) enterography exhibited 2 cm circumferential lipoma, with 7 cm intussusception of the small bowel in the left upper quadrant (Fig. 1).
Figure 1:
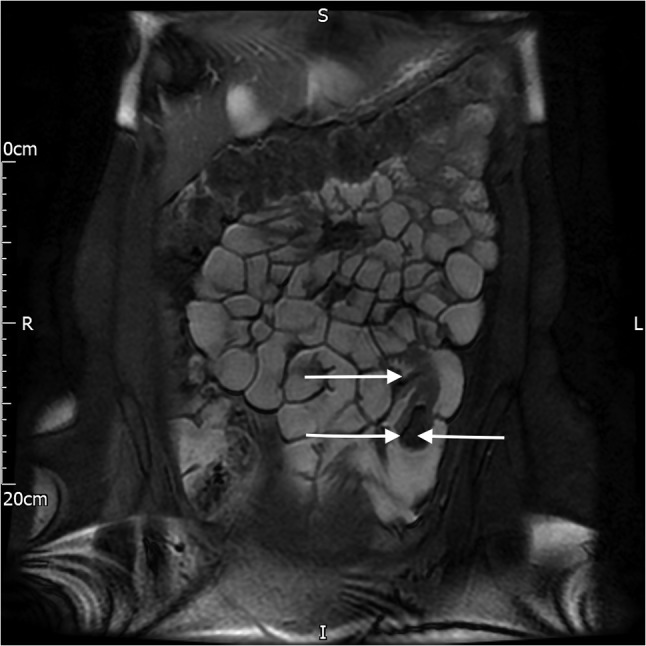
MR image of the lipoma (single arrow, left side) and the intussusception (double arrow, right side).
A laparoscopic approach for the resection of the tumour (lipoma/polyp) was adopted. This was achieved by Hassan technique and use of three laparoscopic ports (12, 10 and 5 mm). Small bowel resection inclusive of the intussusception and the lipoma was conducted with primary side-to-side anastomosis using stapler device. The specimen was removed through a 4 cm Pfannenstiel incision (Fig 2). Patient made an uneventful recovery and was discharged 3 days later and on 6-month follow-up reported no complications. Histopathological examination of the specimen confirmed a jejunal lipoma with intussusception and no sign of malignancy.
Figure 2:

Resected specimen demonstrating the lipomata (single arrow) of the jejunum and intussusception with its length.
DISCUSSION
GI intussusception in adults is not a common occurrence and majority are secondary to neoplastic entity with 80% in colon and 20% in small bowel. In addition, majority of benign aetiologies for small bowel intussusception are secondary to polyps (Peutz-Jeghers, hamartomas, adenomas, gut stromal tumours and fibro-inflammatory), diverticular disease (Meckel’s) and rarely lipomas [3]. According to Mouaqit et al. of the total 51 reported cases of GI lipomas in the literature, only 26 originated from the small bowel and only 5 were from submucosa of the Jejunum [4]. Amongst them majority had non-specific partial and intermittent obstructive symptoms with few bleeding episodes secondary to mucosal ulceration [3, 4].
Due to their vague and non-specific symptoms, majority are diagnosed late and as a part of full bowel obstruction and/or acute GI bleed in elderly population. Furthermore, in earlier decade of life such presentations might be labelled as non-specific abdominal pain. The best modality of investigation remains computed tomography specially in older population when possibility of malignancy could not be ruled out [5]. However, MR imaging is another modality with good sensitivity and specificity specially in younger population when malignancy is not suspected. Other useful modalities are, video capsule endoscopy, double balloon enteroscopy, barium studies and ultrasonography. However, they are not free from their own limitation due to body habitus, operator dependency and specificity [6].
Upon diagnosis of lipomata of the jejunum, despite intermittent symptom and lack of complete obstruction, a full resection of the lipoma and the invaginated segment of the small bowel remains the best modality of treatment [6]. In such circumstances, a reduction of the intussusception following limited excision of the lipomata should not be attempted, as the weakened mesentery, local inflammation and systemic changes can result in further herniation, ischaemia and intermittent intussusception. In rare scenarios, malignancy might also be a feature or an associated component. Furthermore, if lipoma and intussusception is not resected, a full obstruction and/or acute GI bleed might complicate patient care in the future. Overall, Jejunum lipomata are rare and have non-specific presentation but they should be considered as a part of differential diagnosis in any GI bleed and obstructive (partial and intermittent) presentations.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Michel LA, Ballet T, Collard JM, Bradpiece HA, Haot J. Severe bleeding from submucosal lipoma of the duodenum. J Clin Gastroenterol 1988;10:541–5. [DOI] [PubMed] [Google Scholar]
- 2. Zirpe D, Wani M, Tiwari P, Ramaswamy PK, Kumra RP. Duodenal lipomatosis as a curious cause of upper gastrointestinal bleed: a report with review of literature. J Clin Diagn Res 2016;10:PE01–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Seow-En I, Foo FJ, Tang CL. Jejunojejunal intussusception secondary to submucosal lipoma resulting in a 5-year history of intermittent abdominal pain. BMJ Case Rep 2014;29:bcr2014207297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mouaqit O, Hasnai H, Chbani L, Benjelloun B, El Bouhaddouti H, et al. Adult intussusceptions caused by a lipoma in the jejunum: report of a case and review of the literature. World J Emerg Surg 2012;7:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Goh BK, Quah HM, Chow PK, Tan KY, Tay KH, Eu KW, et al. Predictive factors of malignancy in adults with intussusception. World J Surg 2006;30:1300–4. [DOI] [PubMed] [Google Scholar]
- 6. Manouras A, Lagoudianakis EE, Dardamanis D, Tsekouras DK, Markogiannakis H, Genetzakis M, et al. Lipoma induced jejunojejunal intussusception. World J Gastroenterol 2007;13:3641–4. [DOI] [PMC free article] [PubMed] [Google Scholar]


