Abstract
Objective
The aim of this study was to compare anesthetic and surgical outcomes of external dacryocystorhinostomy (DCR) under loco-regional anesthesia (LA) versus general anesthesia (GA).
Methods
Retrospective chart review of all patients that underwent DCR by one surgeon (IH) over the course of a ten-year period (April 1994 to March 2003).
Results
A total of 221 DCR were performed on 209 patients during the study period: 71 were done under LA (72.0 ± 13.3 years) and 150 under GA (64.2 ± 13.0 years; P<0.001). LA patients had a shorter length of surgery (56.2 ± 15.3 vs. 64.0 ± 18.1 minutes; P=0.001) and required less antiemetic drugs during the first four hours after surgery (P=0.03). Pain was well controlled and patients were comfortable per- and post-operatively. Excluding ecchymosis (38.0% LA vs. 21.6% GA; P=0.01), the rate of minor complications did not differ between the two groups: infection, inflammation or edema (14.1 vs. 18.2%; P=0.13), hematoma (1.4 vs. 2.7%; P=0.52) and epistaxis (22.5 vs. 14.2%; P=0.44). Rates of recurrent symptoms and/or re-intervention (11.3 vs. 13.1%; P=0.91) were comparable for LA and GA.
Conclusion
This study suggests that external DCR performed under LA and monitored anesthesia care may be advantageous. The length of surgery is reduced, post-operative side effects are diminished, and excluding ecchymosis, the rate of minor complications is not increased. These benefits are desirable in a predominantly elderly population where avoidance of GA risks is at times necessary.
Introduction
Epiphora from acquired nasolacrimal duct obstruction is a common ophthalmic problem and accounts for up to 3% of ophthalmology clinic visits.1 A dacryocystorhinostomy (DCR) is a procedure designed to relieve chronic epiphora by bypassing the site of nasolacrimal duct obstruction, or dacryostenosis. A fistula is created between the lacrimal sac and the nasal cavity at the level of the anterior middle turbinate.
DCR can be performed under general anesthesia (GA) or attended loco-regional anesthesia (LA). Historically, GA has been chosen to eliminate the pain that was often incompletely controlled with LA and to alleviate the anxiety associated with passage through bone and proximity to the eye. Since acquired dacryostenosis is most frequently encountered in elderly patients who suffer from co-morbid conditions, avoidance of GA is desirable.
This paper describes a technique of LA combined with the use of sedatives. The purpose of this study is to evaluate the anesthetic and surgical outcomes of DCR by comparing results following LA versus GA.
Materials and Methods
A retrospective review of patient charts, including hospital and office charts, anesthetic records and surgical protocols, was performed. This study received approval from the Institutional Review Board and adhered to the tenets of the Declaration of Helsinki. All patients who had undergone DCR by the same surgeon (IH) from April 1994 to March 2003 were included in this study. Information such as age, gender, side and duration of surgery was collected for every patient. The type of anesthesia used was noted.
For patients who received LA, peri-operative comfort level was determined by the opioid analgesics used. To be more specific, narcotics were divided into low, moderate, and high doses. By definition, moderate doses of fentanyl ranged from 50 to 150 mcg, moderate doses of sufentanil ranged from 5 to 15 mcg and moderate doses of alfentanil ranged from 500 to 1500 mcg.
Four indicators of pain were used to determine the patient’s comfort level: 1) use of high doses of narcotics, 2) repetitive administration of narcotics when the initial dose was moderate or high, 3) use of more than one type of opioid analgesic, and 4) supplementary injection of local anesthetic.
Sedatives, such as midazolam, and hypnotics, such as propofol and ketamine, were noted but were not used to infer peri-operative pain, as these may have been administered for anxiety and do not reliably reflect pain.
For both LA and GA groups, pain was inferred, during the first four post-operative hours, by the use of analgesics in the post-anesthesia care unit (PACU) and by the length of time to analgesic request. Similarly, antiemetic drugs administered during the first four hours in the PACU or on the ward were also noted.
Finally, rates of complications, unplanned admission, recurrence of symptoms, and/or need for re-intervention were compared between study groups. In order to identify these events, all follow-up visits were reviewed.
Statistical analysis
Data were analyzed with the JMP 5.01 software (SAS Institute Inc, Cary NC USA, 2002) and a P value of less than 0.05 was considered significant. Sex distribution and side of surgery were compared with Chi-square tests. Age, time to request the first analgesic drug, and length of surgery were compared across the study groups with ANOVA. In the LA group, narcotic dose and pain indicators were tested against three variables: gender, sedatives (used in any amount vs. none used) and age (<70 vs. > or = 70 years old) in an attempt to insure the independence of these variables. A chi-square test with 2 degrees of freedom was used for this purpose. Likelihood ratio tests were used to compare rates of complications (ecchymosis, hematoma, epistaxis, infection, unplanned admission, need for analgesics, doses of antiemetics used) between study groups. Rate of symptom recurrence and/or need for re-intervention was compared with survival curve analysis.
Loco-regional anesthesia technique
In the operating room, the patient first receives a topical instillation of proparacaine HCl 0.5% in the conjunctival cul-de-sac of each eye. This prevents any burning sensation associated with the facial prep. Oxygen is delivered through a tube suspended close to the patient’s mouth that will later be covered with the drapes. The patient’s nasal cavity on the involved side is sprayed with less than 1ml of 2% lidocaine and 1:100 000 epinephrine solution. This vasoconstricts the mucosa and minimizes discomfort during nasal packing.
After 3 or 4 minutes, and after IV narcotics have administered by the anesthesiologist, the nasal cavity is packed with cotonoid strips soaked in 5 to 10% cocaine solution. A fiberoptic headlight and a nasal speculum are useful for this procedure. Bayonet forceps should be used to insert the strip between the head of the middle turbinate and the inferior turbinate, adjacent to the lacrimal fossa. The forceps should be directed to the medial canthus in order to place the pack properly. Controlling the force of the upward packing can prevent an inadvertent fracture of the cribriform plate. The cotton gauze will be left in place until the nasal mucosa is incised during the surgery.
Local and regional anesthesia is performed with the same solution. A mixture of 2 parts lidocaine 2% with epinephrine 1:100 000 combined with 1 part of bupivicaine 0.5% is prepared in a 10cc syringe with a 26-gauge needle. Two milliliters of solution are injected subcutaneously over the incision site, below the medial canthal tendon. Injection into the muscle is avoided to prevent hematoma formation. Tissues deeper to the skin will eventually be anesthetized by diffusion.2 The skin of the medial lower and upper eyelids should also be infiltrated approximately 5 mm away from the lid margin in order to avoid the marginal vessels that run 2–4 mm from the margin.3
The most important regional anesthesia is the infra-trochlear and anterior ethmoidal nerve block. Both are branches of the nasociliary nerve, a branch of the ophthalmic division of the trigeminal nerve. They supply the inner canthus, the medial end of the upper eyelid, the medial conjunctiva and caruncle, the lacrimal sac, and the skin and mucosa of the nose.3,4 A 25-gauge, 1 1/2” needle should be inserted lateral to the caruncle and directed 10 degrees towards the medial orbital wall. It should be advanced and redirected posteriorly every time bone is met, until the needle reaches a distance of about 2.5 cm from the anterior lacrimal crest. One to two milliliters are injected. A temporary dilated pupil or medial rectus paralysis is not unusual.3 A block of the posterior ethmoidal nerve, located 12 mm posteriorly, is not necessary.
Injections should be completed 10–15 minutes prior to surgery to ensure adequate vasoconstriction and anesthesia. During the surgery, a piece of gelfoam (absorbable gelatin sponge, Pharmacia & Upjohn) soaked in lidocaine 2% with epinephrine 1:100 000 is placed directly against the outer nasal mucosa through the site of osteotomy for approximately 3 minutes for added vasoconstriction.
Local techniques used during GA
In order to ensure vasoconstriction during GA, patients received local infiltration over the incision site, nasal packing soaked in decongestant nasal spray solution, and a piece of gelfoam soaked in anesthetic solution against the nasal mucosa, as described above.
Results
A total of 221 DCR procedures were performed in 209 patients during the study period. A bilateral DCR was considered as a single procedure if both sides were operated at the same time. When the second side or a revision was done at a later date, these were considered separate procedures. Out of 221 DCR, 71 (32%) were performed under LA and sedation. The remainder was done under GA.
Patients operated under GA were younger than those operated under LA (64.2 vs. 72.0 years; P<0.001). In the LA group, they were equally separated as to the side of the surgery with 48% done on the right and 48% done on the left. In the GA group, 50% were done on the right and 43% done on the left. The rest were bilateral surgeries. The length of the surgery was on average shorter when done under LA rather than GA (56.2 vs. 64.0; P=0.001) (Table 1).
Table 1.
General Information
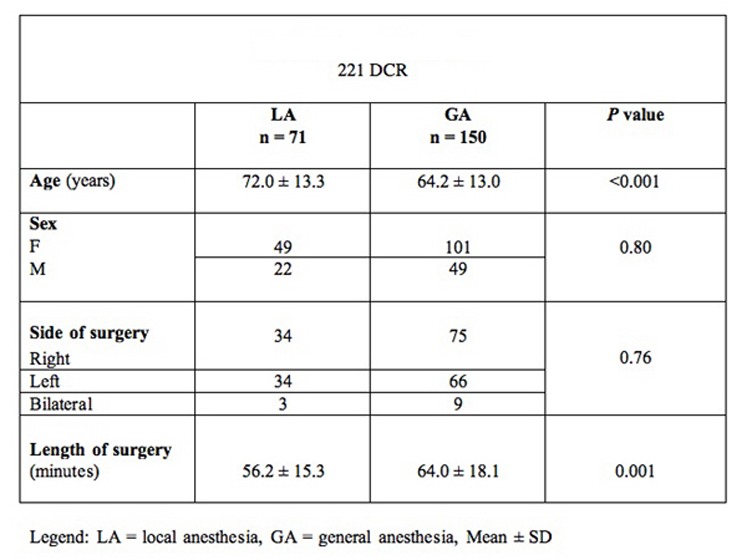
|
In most of LA cases (65%), a moderate dose of peri-operative opioid analgesic was administered. The characteristics previously described to indicate pain were rarely present. No patient required high doses of narcotics and 17% patients did not receive any narcotics for the surgery. A repeat administration of narcotics was required in 23% of cases. More than one type of opioid analgesic was used only 4.2% of the time. Supplementary local anesthetics were never required.
At most, two out of four peri-operative pain indicators were noted in only 4% of LA cases. 18% had one indicator, but in most LA surgeries (78%), none of the studied pain indicators were found.
There was a statistically significant inverse correlation between age and the dose of opioids administered during the LA surgery (Chi-squared = 8.070, p = 0.018). When lower doses were used, patients tended to be older. In fact, when no narcotics were utilized, all patients were older than 70 years of age. No correlation was found with respect to gender or sedative use.
The type of anesthesia did not influence the number of patients who needed a postoperative analgesic drug during the first four hours after the surgery and the time when it was first required. The number of doses of antiemetic drug administered in the first four hours after the surgery was however significantly less when LA was used (P=0.03) (Table 2).
Table 2.
Drugs Administered Post-operatively
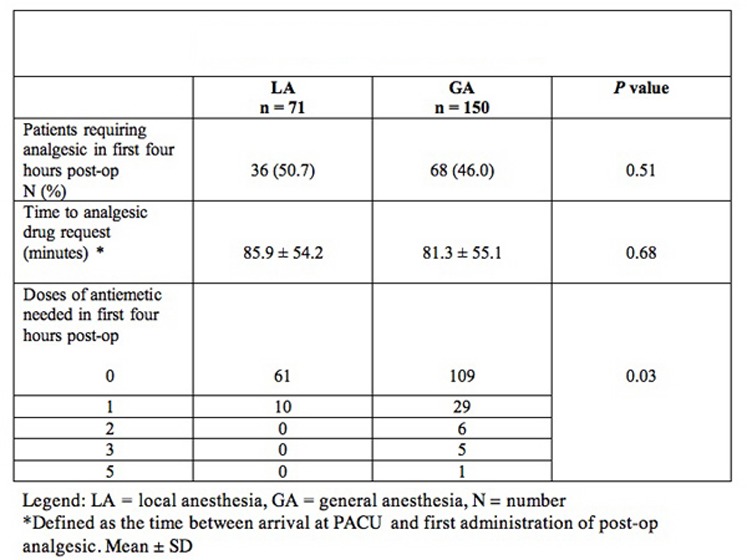
|
For minor complications, the two groups differed only in the incidence of ecchymosis, which occurred significantly more often when LA was used (38.0 vs. 21.6%; P=0.01). More significant LA events include one patient who was reanimated after respiratory arrest due to very high doses of narcotics and sedatives and another patient who required administration of naloxone for narcotic reversal. Reversion to GA was not required for any of the LA patients.
Statistically, the type of anesthesia provided did not influence the incidence of unplanned admission. All but 10 patients were observed post-operatively for the same amount of time. These 10 patients were kept extra 1–3 days for epistaxis, cardiac monitoring, or suspicion of infection. Patients were followed for an average of 10.7 months (0.25 to 89 months). Over this period of time, the overall incidence of recurrent symptoms or the need for a re-intervention was 12.5% and was not related to the type of anesthesia provided as indicated by the survival analysis curves (P=0.91). (Table 3)
Table 3.
Complication Rate
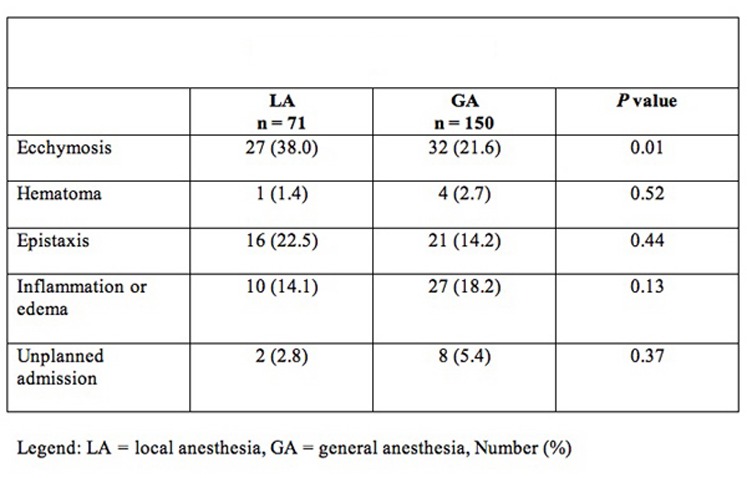
|
Discussion
The purpose of this paper was to evaluate the anesthetic and surgical outcomes of LA used concurrently with IV sedatives during DCR surgery compared to surgery performed under GA.
Because pain had to be evaluated peri-operatively and retrospectively, subjective data was unavailable. Verbal or visual analogical pain scale scores were neither systematically noted intra-operatively nor in PACU, and could not be retained for analysis. Pain had to be inferred by the amount of narcotics received and by various pain indicators. Generally, patients were comfortable with the technique used. When surgery was performed under LA, narcotics never exceeded moderate, “standard”, doses. In approximately one fifth of surgeries, patients actually did not require any narcotics at all.
Of all four LA pain indicators, only two were positive. The most frequent one was a repeat administration of narcotics, which was noted in 23% of patients. In almost four out of five surgeries, no pain indicator was found.
Pain in the recovery room is a weak reflection of the effectiveness of local anesthetic, even if longer-lasting bupivicaine was mixed in to the solution. In fact, pain during the first four hours after the surgery, as measured by the number of patients who required an analgesic drug and the time when it was first required was not significantly lower in patients operated under LA. On the other hand, the incidence of nausea and vomiting as inferred by the number of doses of antiemetic drugs administered was significantly lower in these patients. Since nausea and vomiting is a significant factor contributing to delayed discharge in patients operated on an ambulatory basis this is an appreciable benefit.5
This method of evaluation of pain has certain limitations. As was demonstrated, opioid dose and pain indicators were tested against some patient variables. It was found that the dose of narcotics used is dependent upon the patient’s age. Anesthetists, in general, administered lower or doses to older patients, possibly to prevent adverse effects such as respiratory depression. Because the average age in this study was 72 years and because older patients were administered lower doses or no medication at all, this could partly explain lower pain indicator numbers. Another limitation is the fact that different anesthesiologists contributed to the cases presented in this study. As a result, several narcotic “recipes” were used. Some patients received higher doses of opioid analgesics at the beginning of a case therefore, may have been less likely to require a repeat administration or supplementation with another type of narcotic. The length of surgery could theoretically influence the need for added analgesia but most procedures took approximately 60 minutes, which is well within the duration of action of lidocaine. The three longer bilateral cases required only moderate doses of narcotics and no pain indicators were noted.
One third of the external DCR performed by this surgeon (IH) were done under LA. Most of the surgeries were performed under GA prior to 1998. Today, this modality is chosen according to patient’s preference after explanation of the surgical procedure and in the absence of systemic contra-indications. McNab and Simmie reported the use of LA in 76.5% of their DCR performed after 1997.6 Hurwitz et al. also used it in 82% of their elderly patients (70–90 years).7 These patients often have cardio-vascular contra-indications to GA. In both of these studies, no formal comparison between LA and GA was done. In the population presented here, younger, often more anxious patients tended to choose GA more often.
Ecchymoses were more frequent in the LA group (38.0 vs. 21.6%; P=0.01) even though both groups received subcutaneous injections of anesthetic/vasoconstrictive solution. This may be due to the added regional block in LA patients or because this group may be more subject to labile blood pressure. Apart from ecchymosis, the rate of minor complications was not increased in patients operated under LA, despite the fact that patients who accepted this technique were significantly older (72.0 ± 13.3 vs. 64.2 ± 13 years; P<0.0001). Moreover, it is possible that major complications, secondary to general anesthesia, were prevented by its avoidance in an aged population; our oldest patient was 95 years old.
Local anesthetics can lead to complications such as retrobulbar hemorrhage, injury to the globe or the optic nerve.6 Sedatives and local anesthetics can cause respiratory or cardio-vascular compromise. Inadequate protection of the patient’s airway can become complicated by obstruction by blood originating from the nasal cavity. 6 In this study, two patients (2.8% LA) suffered complications from opioid/sedative overdose. Since these complications happened when patients were under monitored anesthesia care, there were no long-term deleterious consequences.
Although sedation/analgesia has been recommended to improve a patient’s acceptance of major regional anesthesia procedures, its use in ophthalmic surgeries is, however, a more controversial issue.6–8 The use of intravenous sedatives in cataract surgery, has been associated with a significant increase in adverse events for topical or injection anesthesia, relative to topical or injection anesthesia without intravenous sedation.8 The use of short-acting hypnotic agents with injection anesthesia has also been associated with an incremental increase in adverse events when used alone, in combination with opioids, with sedatives or, with opioids and sedatives. Although the incidence of respiratory depression requiring intervention is probably lower with infusions of sub-hypnotic doses of propofol, its administration in conjunction with peribulbar anesthesia has also been associated with respiratory adverse events.9 Of course, this literature may not be relevant to DCR that generally require more sedation than cataract patients.
An important lesson is that intravenous sedation and analgesia should not be used as a substitute for insufficient local anesthesia; instead supplementing local anesthesia or reverting to general anesthesia is preferable. A patient’s noncompliance is another factor that may prompt the physician to revert to GA.7
Ultimately, whether patients were operated on under local anesthesia or general anesthesia, long-term results were comparable. For the patients presented in this series, survival analysis curves showed absolutely no difference in the rate of symptom recurrence or re-intervention (11.3 vs. 13.1%; P=0.91).
Since results were comparable, a thorough discussion with the patient should be undertaken preoperatively to determine patient preference for the type of anesthesia. Also, future evaluation of patient satisfaction with each technique may be an important indicator as well for the type of anesthesia that is chosen. Finally, the level of experience of the surgeon may also dictate which anesthesia is used. While the senior authors have extensive experience and may perform DCR at ease under LA or GA, certain starting surgeons may prefer to develop a comfort level under GA before proceeding with surgery under LA. In addition, in university-based hospitals where residents and fellows are in training, it may be preferable for teaching purposes to use GA to facilitate teaching.
Conclusion
This study suggests that external DCR performed under LA and monitored anesthesia care may be advantageous. Compared to GA, the length of surgery was diminished and, excluding ecchymosis, the rate of minor complications was not increased. Pain was well controlled and patients were comfortable during the surgery. With the advantage of diminished post-operative side effects, attended LA using this technique is very beneficial, especially in the predominantly elderly population seeking this operation, where avoidance of GA risks is at times essential.
References
- 1.Linberg JV, Mc Cormick SA. Primary acquired nasolacrimal duct obstruction: a clinicopathologic report and biopsy technique. Ophthalmology. 1986;93:1055–63. doi: 10.1016/s0161-6420(86)33620-0. [DOI] [PubMed] [Google Scholar]
- 2.Tse DT. In: Colour Atlas of Ophthalmic Surgery: Oculoplastic Surgery. Wright KW, editor. Philadelphia: J.B. Lippincott Company; 1992. pp. 75–79. [Google Scholar]
- 3.Levine MR. Manual of Oculoplastic Surgery. New York: Churchill Livingstone Inc; 1988. pp. 1–16.pp. 245–255. [Google Scholar]
- 4.Tyers AG, Collin JRO. Colour Atlas of Ophthalmic Plastic Surgery. 2nd ed. Woburn, MA: Butterworth-Heinemann; 2001. p. 64. [Google Scholar]
- 5.Shaikh S, Chung F, Imarengiaye C, Yung D, Bernstein M. Pain, nausea, vomiting and ocular complications delay discharge following ambulatory microdiskectomy. Can J Anaesth. 2003;50:514–8. doi: 10.1007/BF03021067. [DOI] [PubMed] [Google Scholar]
- 6.McNab AA, Simmie RJ. Effectiveness of local anesthesia for external dacryocystorhinostomy. Clinical and Experimental Ophthalmology. 2002;30:270–2. doi: 10.1046/j.1442-9071.2002.00535.x. [DOI] [PubMed] [Google Scholar]
- 7.Hurwitz JJ, Merkur S, DeAngelis D. Outcome of lacrimal surgery in older patients. Can J. Ophthalmol. 2000;35:18–22. doi: 10.1016/s0008-4182(00)80104-0. [DOI] [PubMed] [Google Scholar]
- 8.Katz J, Feldman MA, Bass EB, et al. Study of Medical Testing for Cataract Surgery Study Team Adverse intraoperative medical events and their association with anesthesia management strategies in cataract surgery. Ophthalmology. 2001;108:1721–6. doi: 10.1016/s0161-6420(01)00704-7. [DOI] [PubMed] [Google Scholar]
- 9.Habib NE, Balmer HG, Hocking G. Efficacy and safety of sedation with propofol in peribulbar anaesthesia. Eye. 2002;16:60–2. doi: 10.1038/sj.eye.6700062. [DOI] [PubMed] [Google Scholar]


