Abstract
Background
To determine whether a computerized clinical documentation system (CDS): 1) decreased time spent charting and increased time spent in patient care; 2) decreased medication errors; 3) improved clinical decision making; 4) improved quality of documentation; and/or 5) improved shift to shift nursing continuity.
Methods
Before and after implementation of CDS, a time study involving nursing care, medication delivery, and normalization of serum calcium and potassium values was performed. In addition, an evaluation of completeness of documentation and a clinician survey of shift to shift reporting were also completed. This was a modified one group, pretest-posttest design.
Results
With the CDS there was: improved legibility and completeness of documentation, data with better accessibility and accuracy, no change in time spent in direct patient care or charting by nursing staff. Incidental observations from the study included improved management functions of our nurse manager; improved JCAHO documentation compliance; timely access to clinical data (labs, vitals, etc); a decrease in time and resource use for audits; improved reimbursement because of the ability to reconstruct lost charts; limited human data entry by automatic data logging; eliminated costs of printing forms. CDS cost was reasonable.
Conclusions
When compared to a paper chart, the CDS provided a more legible, compete, and accessible patient record without affecting time spent in direct patient care. The availability of the CDS improved shift to shift reporting. Other observations showed that the CDS improved management capabilities; helped physicians deliver care; improved reimbursement; limited data entry errors; and reduced costs.
Background
Computerized clinical documentation systems (CDS) provide for the documentation of patient care using computers. For example, the CDS records the vital signs directly from the cardio-respiratory monitors, while other documentation, such as nursing assessments are entered by the clinician. Reported benefits of computerized clinical systems in the adult care setting include: 1) nursing time savings [1,2]; 2) improved decisions and productivity of physicians [3,4] ; 3) decreased medication errors [5]; 4) decreased turn-around time for results [4]; 5) easier quality assurance process [6]. These potential benefits have not been studied well in the pediatric setting [7].
As part of the implementation of a CDS in our Pediatric Intensive Care Unit (PICU), we evaluated some effects of this system. The objectives of the study were to determine whether the CDS affected time spent by nursing in patient care; decreased medication errors; increased the speed of clinical decision making; improved the quality of documentation; and improved shift to shift continuity when compared to paper charting.
Computer software/hardware
The Eclipsys Continuum 2000 CDS (Eclipsys Corporation, Delray Beach, Fl.) was chosen for implementation in the PICU at Children's Hospital, Columbus, OH. At the time of the study, the PICU had 16 beds with an average daily census of 11.3, an average length of stay of 3.4 days and 1205 admissions for the year. Recently, we opened a new PICU with 35 beds with the Eclipsys as the CDS, but we haven't studied it yet in the larger unit. At the time of this study, the system used Sun SPARCstations (Sun Microsystems, Mountain View, CA) with a peer to peer network. There was an Eclipsys workstation at each bedside and 2 at the nursing station. There was built in redundancy for reliability with mirrored copies of individual patient data stored in 2 different Sun SPARCstations on the network. Since this study was completed, the system was upgraded to a client server architecture using either pc's or x-terms as the client .
The system was connected to the Hewlett Packard Component Monitoring System (Hewlett Packard, Palo Alto, CA) using Hewlett Packard's proprietary Careport interface. In addition, the Eclipsys system is connected through the hospital's interface engine using an HL7 interface to the hospital laboratory system and the hospital information system. The connections permit the automatic logging of data from the cardiorespiratory monitor to the ECLIPSYS System, and the automatic transfer of laboratory data to the Eclipsys system as soon as the laboratory personnel verify them as being accurate. Nursing, laboratory, and respiratory care staff used a graphical user interface to document care on the ECLIPSYS System. The graphical interface allows for 'point and click' data entry, charting by exception, and text entry by keyboard. Each clinician has a unique electronic signature. All data entry is automatically included in an audit trail that maintains all versions of data as is changed or corrected. The clinical information is stored in a proprietary database designed by ECLIPSYS for fast individual patient access. After discharge the patient's information is archived. During the hospitalization of a patient all non-textual information is sent to a relational database, which allows ad hoc and prewritten queries about the information in the database which cannot be obtained using the clinical database. These queries use Structured Query Language (SQL) and were the basis of the computerized chart audits.
Methods
Five aspects of care were studied during two three month time periods before and one three-month time period after the installation of the CDS as suggested by the statistician since we underwent a paper charting change at the time of this study. This is a modified one group, pretest-posttest design. An independent observer performed a time/motion study to measure time spent charting and in direct patient care by the nursing staff. As a measure of medication error, we chose to evaluate delays in medication delivery since this system did not have order entry. A chart (paper or computer) audit was performed to determine the difference in time between scheduled and actual medication delivery. To assess the speed of clinical decision-making we audited charts (paper or computer) to determine the time it took for abnormal potassium and ionized calcium values to return to normal. The presumption was that if clinicians had better access to laboratory data, they would respond to abnormalities in a more timely fashion. This improved response would result in a more rapid return of abnormal values to normal.
We evaluated the completeness of nursing documentation by a review of nursing documentation. The specific questions addressed were: 1) did the nurses notes reflect the care plan; 2) were the care goals based on nursing diagnosis; 3) were the nursing care plans completed; 4) was a psychosocial assessment completed; 5) were safety precautions documented; 6) were the parent education sessions documented; 7) was the parent's response to the education reported; and 8) were nursing interventions evaluated
The last aspect of the study included an evaluation of shift to shift continuity. We wanted to compare the "paper" shift change with the "computer" shift change. The major difference was the replacement of multiple sources of paper info about the patient with a single computerized source of information about the patient available at the time of shift change. We accomplished this with a Likert scale questionnaire administered to nursing staff immediately following change of shift report. The questionnaire was designed to determine attitudes of the incoming nursing staff about shift report (a copy of the questionnaire is available upon request). Each question was rated on a scale of 1 to 5 with 5 expressing the most positive attitude towards the shift report experience. In addition, one question rated the time it took to complete the shift report.
All five assessments were completed for each time period. The data were analyzed using one way or two way ANOVA where appropriate.
Results
The nursing time study demonstrated no significant difference in nursing time devoted to direct patient care or charting between the pre-CDS and the CDS time periods (Table 1). The medication delivery audit showed an apparent significant increase in delayed medication deliveries during the CDS time period (Table 1). The laboratory normalization time data could not be analyzed because too many data concerning the time of reporting of results were missing from the paper chart audit. Data obtained from the CDS were 100% complete, however.
Table 1.
Nursing Time Study Data, Medication Error Study Data, and Shift Change Survey Data
| Significance when | |||
|---|---|---|---|
| Measure | n | Mean ± standard deviation | compared to Post-Test |
| Time Spent | |||
| Charting | Minutes/Hour | ||
| Pretest 1 | 12 | 21.26 ± 3.64 | not significant |
| Pretest 2 | 12 | 22.35 ± 3.92 | not significant |
| Post-Test | 12 | 21.87 ± 3.09 | |
| Significance when | |||
| Measure | n | Mean ± standard deviation | compared to Post-Test |
| Direct | |||
| CareTime | Minutes/Hour | ||
| Pretest 1 | 12 | 25.74 ± 4.83 | not significant |
| Pretest 2 | 12 | 30.14 ± 2.83 | not significant |
| Post-Test | 12 | 29.37 ± 4.23 | |
| Significance when | |||
| Measure | n | Mean ± standard deviation | compared to Post-Test |
| Medication | |||
| Delivery Delay | Minutes | ||
| Pretest 1 | 601 | 8.5 ± 27.9 | p < 0.01 |
| Pretest 2 | 513 | 12.8 ± 22.7 | p < 0.01 |
| Post-Test | 856 | 16.9 ± 34.9 | |
| Significance when | |||
| Measure | n | Mean ± standard deviation | compared to Post-Test |
| Nursing Shift | |||
| Survey Score | Scale 1–5/5 is best score | ||
| Pretest 1 | 17 | 3.57 ± 0.64 | p < 0.03 |
| Pretest 2 | 10 | 3.54 ± 0.57 | p < 0.01 |
| Post-Test | 28 | 4.05 ± 0.36 | |
| Significance when | |||
| Measure | n | Mean ± standard deviation | compared to Post-Test |
| Time for Shift | |||
| Change | Minutes | ||
| Pretest 1 | 17 | 13.97 ± 3.43 | not significant |
| Pretest 2 | 10 | 13.3 ± 7.0 | not significant |
| Post-Test | 28 | 15.0 ± 5.6 | |
In all areas, nursing documentation was superior during the CDS time period both in content and legibility (Figure 1). The survey of shift-to-shift reporting showed significantly more positive reporting experiences during the CDS time period, with no increase in time required (Table 1).
Figure 1.
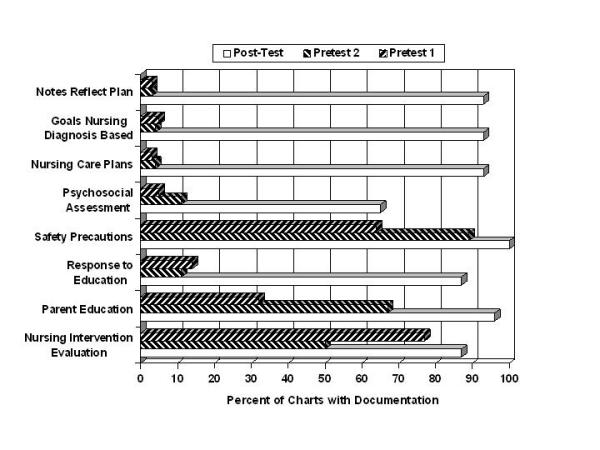
Improvement in quality of documentation: A barchart comparing the completeness of nursing documentation for each time period and for each area of documentation.
Throughout the study, we attempted to document important incidental findings related to the implementation of the CDS. To this end, we made several observations during the course of the study that we thought important to report. The complete and legible computerized clinical documentation helped our nurse manager to increase her span of managerial control by providing better incident documentation, and enhanced her ability to develop employees with easier access to legible charting by individual nurses. During the CDS portion of our study, we had a JCAHO audit and noted that our documentation was in compliance because the CDS forced legible and complete documentation. Our clinicians (physicians, nurses and respiratory therapists) appreciated the automated calculations done by the CDS (shift and daily I&O) and the ability to compare physiological data graphically. Accessibility to the patient's chart improved since an individual chart could be viewed on any of the 18 computer workstations in the unit. This improved accessibility gave the clinicians the ability to chart concurrently while viewing clinical data (lab and vital signs) during resuscitations. According to the hospital's internal auditor, the hospital increased hospital reimbursement by about $300,000 during the first year because of the CDS's ability to recreate lost charting from the computer files. Automatic logging of information reduced human data entry and the associated transcription errors. We eliminated the cost for standard nursing and respiratory forms. Finally, the cost of the system seemed reasonable. Using the figures at the time of the purchase, the cost of the hardware and the software, if expanded to all our critical care beds would be $24/patient day if amortized over 3 years.
Discussion
In the last five years, computerized clinical systems have become generally more available [8]. Evaluations of the usefulness and effectiveness of some these clinical systems have been reported, but most evaluations are in the adult care setting [7]. The evaluation of the implementation of the CDS in the PICU at Children's Hospital provides some insight into the use of computerized clinical systems in a pediatric critical care setting. Prior to the implementation of the CDS in our PICU, the only computer systems available was a stat lab report printer and access to the laboratory's departmental computer system using a very crude user interface.
A decrease in documentation time and consequently an increase in the time available to the nurse for direct patient care are described as a benefit of these computerized systems [9] In contrast, our experience demonstrated no increase in time devoted to direct patient care with the introduction of the CDS. One of the reasons for this lack of observed benefit might be our timing of the Posttest time period. We may still have been on the learning curve and this probably warrants further study. However, we did note that the documentation provided by the CDS was more complete and always legible; in addition, it took no longer to chart with the CDS as compared to the paper system. The content was more complete because the CDS, depending on the documentation, forced the clinician to document a certain way, guided the clinician, or made documentation easier for the clinician. Although we did not perform a measurement of accessibility, a single chart can be accessed simultaneously by all 18 workstations in the PICU. This is one of the major benefits of an effective clinical system [10]. The Eclipsys System handles record locking on a first com first served basis. A record cannot be updated by more than one person at a time. In addition, to access the system, one must logon using a unique ID and password. Each use of the system is provided and ID and password. Once logged on, the system presents a census list of patients from which the user can open any one chart at a time. Access time is almost instantaneous.
Another major benefit of computerized clinical documentation systems is a reduction of medication errors [5]. In our institution, we have 2 major sources of medication error – transcription errors and delivery time errors. We did not implement a physician order entry component (we are currently in the process of doing so), but chose to evaluate the effect of CDS on delays in delivery of medications. We noted a surprising increase in delayed delivery of medications during the CDS time period. However, after closer analysis and discussion with the nursing staff, it appeared the observed increase in delayed medications resulted from better data from the CDS. Times of delivery of medications are logged by the CDS automatically during the charting process. When using the paper system, nurses would commonly chart a medication that was delivered within 30 minutes of a scheduled time as being delivered on time. The more accurate CDS data led to the identification of a hitherto unrecognized problem of the paper system.
During analysis of chart audit of laboratory value normalization, we noted that the paper chart did not contain the information needed to complete the analysis in the majority of the cases. In contrast, every CDS chart contained all the necessary information. In addition, the audit of the paper chart required in excess of 40 hours to get a set of incomplete data, whereas the CDS audit required about 20 minutes, which included developing the SQL search statements required by the CDS. We learned that not only could we get more complete data from the CDS, but also we could do it in a fraction of the time when compared to the paper chart audit. Hence, both the medication and the laboratory audit were simpler using the CDS.
The evaluation of the end-of-shift reporting study suggests that use of the CDS resulted in more positive attitudes towards the change of shift reporting by the nurses. This is likely related in part to the more complete, readable and organized CDS chart. Having the chart available for the shift report may also have influenced the nurses. Moreover, shift change reporting did not take more time with the CDS.
The introduction of the CDS represented a major change in the way the clinicians cared for patients in the PICU at Children's Hospital. For most people change is hard and if not managed well may result in confrontation as occurred at the University of Virginia Medical Center when a computerized order entry system was implemented [11],[12]. While there were a number of institutional issues involved in the confrontation over the physician order system, the University of Virginia's system forced people to change the way they did their job [12]. Innovation may be easier if the individual perceives a 'personal' benefit that results from the change [13]. The 'personal' benefit must be of importance to the individual. In our situation, we found several "value added" benefits for the clinicians that included legibility, completeness, accessibility, and timeliness of information. Furthermore, there was no time cost of the change since the new CDS method of clinical documentation took no longer than the paper based system.
As the Post-test period progressed, unanticipated benefits became apparent. We found that the system allowed for improved management functions of the nurse manager, and 'forced' JCAHO documentation compliance. Our clinicians noted the automated calculations provided by the CDS and the graphic display of physiologic data to be helpful. Having the chart available in more than one location was noted to be helpful both in normal situations as well as during resuscitative efforts. The CDS reduced the time and resources need for audits while at the same time it increased hospital reimbursement. Automatic logging of information reduced human data entry and the associated transcription errors.
Conclusions
The computerized documentation system provided a more legible, complete patient record without increasing the time needed to document care. The CDS was more accessible and it improved shift to shift reporting. We speculate that the widespread use of computerized documentation systems giving better access to clinical data will improve clinician's ability to evaluate outcomes and improve care. This will take some degree of intentionality and an understanding of the data storage systems. Furthermore, the integration of clinical paths and automated variance analysis with the CDS will make the process of reducing variance in patient care much simpler. Finally, we believe the cost savings from having clinical data available in an organized fashion will more than pay for the CDS systems.
Abbreviations and glossary of computer terms
CDS – computerized clinical documentation system
Decision Support Database – a collection of information about the patients that the clinician's have decided to save in order to ask global questions about groups of patients.
Graphical User Interface – software on the computer that uses pictures/graphics and text to communicate with the user and allows the user to manipulate a pointing device (mouse) to move about the software and to enter information.
Interface Engine – A computer/software system that translates information between various computer networks.
JCAHO – Joint Commission on Accreditation of Healthcare Organizations
Network – a number of microcomputer workstations connected together using cables. The connections allow the computers to communicate with each other and a central computer running the network.
PICU – pediatric intensive care unit
Relational Database – a collection of information, which has been, structured such that it is relatively easy to ask questions about the data in the collection.
Structured Query Language (SQL) – a standard way of asking questions about information in a relational database.
Sun SPARCstation – a microcomputer based workstation that has strong graphic capabilities.
Competing interests
Deborah Y. Campbell, R.N. – at the time of this study Ms Campbell was an employee of Children's Hospital, subsequently she worked for Eclipsys
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
James A Menke, Email: menkej@pediatrics.ohio-state.edu.
Cynthia W Broner, Email: menkej@pediatrics.ohio-state.edu.
Deborah Y Campbell, Email: campbeid@musc.edu.
Michelle Y McKissick, Email: McKissiM@chi.osu.edu.
Joy A Edwards-Beckett, Email: jedwardsbeckett@yahoo.com.
References
- Minda S, Bundage DJ. Time Differences In Handwritten and Computer Documentation Of Nursing Assessment. Computers in Nursing. 1994;12(6):277–279. [PubMed] [Google Scholar]
- Hendrickson G, Kovner CT. Effects of computers on nursing resource use; Do computers save nurses time? Computers in Nursing. 1990;8(1):16–22. [PubMed] [Google Scholar]
- Austin SM, Balas A, Mitchell JA, Ewigman BG. Effect of Physician Reminders on Preventive Care: Meta-Analysis of Randomized Clinical Trials. In Proceedings of 18th Symposium on Computer Applications in Medical Care. JAMIA Symposium Supplement. 1994. pp. 121–124. [PMC free article] [PubMed]
- Kuperman GJ. Detecting Alerts, Notifying Physician, And Offering Action Items: A Comprehensive Alerting System. In Proceedings of 1996 American Medical Informatics Association Fall Symposium. JAMIA Symposium Supplement. 1996. pp. 704–708. [PMC free article] [PubMed]
- Sturek JK. Point-of-service computer system and drug-use evaluation: implications for pharmacy practice in ambulatory. American Journal of Hospital Pharmacy. 1989;46(7 Pt 2):S17–20. [PubMed] [Google Scholar]
- Henry SB. Essential Infrastructure For Quality Assessment And Improvement In Nursing. JAMIA. 1995;2(3):169–182. doi: 10.1136/jamia.1995.95338870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohane IS. Getting the Data In: Three Year Experience With A Pediatric Electronic Medical Record System. In Proceedings of 18th Symposium on Computer Applications in Medical Care. JAMIA Symposium Suppement, 1994. pp. 457–461. [PMC free article] [PubMed]
- Lorenzi NM. Antecedents of the People and Organizational Aspects of Medical Informatics: Review of the Literature. JAMIA. 1997;4(2):79–93. doi: 10.1136/jamia.1997.0040079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childs BW. Bedside Systems: Make their Contributions in Hospitals Across the Country. Healthcare Informatics. 1991;8(5):10–16. [PubMed] [Google Scholar]
- The Computer-Based Record: Meeting Health Care Needs. In, The Computer-Based Record: an Essential Technology for Health Care. eds. Dick, RS and Steen, EB. National Academy Press, Washington, D.C., 1991. [PubMed]
- Massaro TA. Introducing Physician Order Entry At A Major Academic Medical Center: I Impact On Organizational Culture And Behavior. Academic Medicine. 1993;68(1):20–5. doi: 10.1097/00001888-199301000-00003. [DOI] [PubMed] [Google Scholar]
- Massaro TA. Introducing Physician Order Entry At A Major Academic Medical Center: II Impact On Medical Education. Academic Medicine. 1993;68(1):25–30. doi: 10.1097/00001888-199301000-00004. [DOI] [PubMed] [Google Scholar]
- Leonard-Barton D, Kraus WA. Implementing New Technology. Harvard Business Review. 1985;85612:102–110. [Google Scholar]


