Abstract
Lifelong learning is essential for the practicing cardiologist. Present lifelong learning mechanisms are stagnant and at risk for not meeting the needs of currently practicing cardiologists. With the increasing burden of cardiovascular disease, growing complexity of patient care, and ongoing pressures of non-clinical responsibilities, educational programming must evolve to meet the demands of the contemporary cardiovascular professional. A paradigm shift, replete with modern and practical educational tools, is needed in the lifelong learning armamentarium. Emerging evidence of novel educational strategies in graduate medical education supports the promise of broader application of these tools to different stages of professional life. In this commentary from the Fellows-In-Training (FIT) Section Leadership Council, we propose three novel educational tools—personalized learning, adaptive learning, and the flipped classroom—to improve lifelong learning to meet the educational needs of FITs to practicing cardiologists alike.
Keywords: graduate medical education, personalized learning, adaptive learning, flipped classroom, fellows in training
Introduction
The development and maintenance of professional competence through lifelong learning is indispensable to all physicians (1). As trainees progress from medical students to established practitioners, learning becomes increasingly self-directed and time-limited. Modalities used in the canonical paradigm to educate medical students, traditionally based on textbooks and lectures, are less well-suited to fellows-in-training (FIT) or practicing cardiologists. In addition, the learning preferences of FITs may not reflect those of more established clinicians. Finally, technological developments, expanding patient volume and complexity, escalating financial pressures, increasing non-clinical responsibilities, and a rapidly evolving healthcare landscape demand that physicians adopt new methods to engage in lifelong learning and maintain competency in clinical practice (1–6).
Lifelong learning has been defined “as a continuation of medical education with an ongoing process of professional development along with self-assessment, which enables physicians to maintain the requisite knowledge, skills, and professional standards.” (7) Using the framework employed by the Accreditation Council for Graduate Medical Education (ACGME) for its six core competencies, the American College of Cardiology (ACC) has recently developed lifelong learning competencies for all areas of cardiovascular medicine to address evolving learner needs (1). Thus, a methodical and critical examination of how the variety of available education platforms can best be incorporated at all stages of training and across the arc of a professional career is needed. As evidence continues to emerge on lifelong learning tools and strategies within graduate medical education (1), a notable gap as it pertains to lifelong learning for medical subspecialists currently exists.
This commentary from the Fellows-in-Training Section Leadership Council examines transformations in the approach to graduate medical education (GME) for FITs and lifelong learning for cardiologists from training to retirement. We identify challenges and explore currently available methods of learning in their respective context. Finally, we propose strategies that modern-day trainees and practicing cardiologists can adopt to improve learning skills, including several innovative learning concepts, such as personalized learning, adaptive learning, and the “flipped classroom”.
Importance of Lifelong Learning
As cardiovascular medicine has evolved over the past several decades (8,9), diagnostic and therapeutic complexity has markedly increased. In addition to the challenges facing general cardiologists to master a rapidly accumulating body of knowledge (1,10,11), those with a more specialized career focus face similarly formidable challenges. As more FITs pursue advanced training in sub-subspecialties such as advanced heart failure, multimodality imaging, or catheter-based interventions, practicing cardiologists will need to keep abreast of developments in their own field of special expertise while remaining current in the broader aspects of the field. To meet the demands for lifelong learning, cardiologists need timely access to evidence-based educational materials that address both the narrow and wider spheres of knowledge (1,12).
Current Graduate Medical Education and Lifelong Learning Strategies
Traditionally, the education of physicians takes place in the classroom, lecture hall, at the bedside, in laboratories, at scientific sessions or through continuing medical education (CME) programs (13). The challenges of the modern day healthcare environment call for critical examination of learning methods by the profession (14). The curriculum and expectations for general cardiology fellowship have been standardized in the ACC 2015 Core Cardiovascular Training Statement (COCATS-4) and the policies of the Accreditation Council for Graduate Medical Education (ACGME) (10,15). Requirements for training in emerging sub-disciplines, such as multimodality imaging, cardio-oncology, or sports cardiology, are less well-defined by specified curricula. Fellows entering the workforce are expected to maintain expertise in these fields, but opportunities for personalized education to ensure continued competency beyond the formal fellowship training years are relatively limited. While resources for lifelong learning should be personalized with respect to individual physicians, present programs typically offer limited customization. The problem is particularly acute for those physicians seeking to gain competencies in new areas for which they were not trained during fellowship. While there is skepticism of the often industry-sponsored ‘weekend course’ at which new techniques are taught, alternative opportunities for those seeking genuine competency are scarce.
Emerging concepts of adult learning theory create opportunities for lifelong learning. Early career learners depend on teachers to provide foundational knowledge. As trainees progress through residency and fellowship, individual learning paths evolve in different directions. Independent learning utilizes an education cycle (16) that recognizes the needs of the physician, sets clear objectives for learning, and includes assessments of how well the objectives are met. Lifelong learning programs should incorporate the following key elements (Table 1):
Table 1.
Key components necessary for the ideal lifelong learning program. Based on concepts from adult learning theory and the educational cycle, the key characteristics listed below are fundamental for development of any lifelong learning educational program.
| Key Component | Description |
|---|---|
| Learning Objectives |
|
| Evidenced-Based Medicine |
|
| Translatable to Clinical Practice |
|
| Smart Use of Technology |
|
| Efficiency |
|
| Critical Assessment of Programs |
|
Generate discrete learning objectives for educational programs.
Incorporate evidence-based medicine to guide development of learning programs.
Provide high-yield and practical educational programming that is readily applicable to clinical practice.
Effectively utilize technology and innovative educational platforms.
Ensure educational programs efficiently utilize time.
Critically examine lifelong learning programs by both educators and learners with the goal to continually optimize and refine programs.
In the following section, we explore several strategies for lifelong learning that can be initiated during fellowship and pursued throughout practice. These strategies address some of the challenges inherent in current models of learning by adult learning theories as they apply to continuing medical education in cardiology.
Strategies to Improve Graduate Medical Education and Lifelong Learning
Three strategies in particular - personalized learning, adaptive learning and the ‘Flipped Classroom’ - can be deployed to help meet the educational needs of cardiologists across the different stages of their careers (Table 2).
Table 2.
Novel educational tools for lifelong learning in cardiology. Three proposed educational strategies (personalized learning, adaptive learning, and the flipped classroom) to improve lifelong learning for cardiologists are detailed.
| Educational Strategy | Description | Advantages | Applications |
|---|---|---|---|
| Personalized Learning |
|
|
|
| Adaptive Learning |
|
|
|
| Flipped Classroom |
|
|
|
Personalized Learning
Personalized learning is an attractive alternative to the traditional ‘one-size-fits-all’ educational model (17). In this system, knowledge acquisition is facilitated by identifying specific learner needs, as identified in COCATS 4 (10) for FITs and in the ACC’s lifelong learning competencies for general cardiologists (1). Both of these documents define competencies within specific practice foci within cardiology, helping clinicians identify their potential learner needs and customizing educational content to meet them. A curriculum is generated based on strengths and weaknesses identified from an individual’s survey or standardized pre-test assessment. Training needs could also be identified from clinical practice and patient care through various assessment tools, including surveys and needs-based evaluations. Thus, these ACC core competency documents will need to be updated frequently in concert with the practice of cardiovascular medicine (18). Applications of personalized learning include simulation training, educational portfolios, and digital platforms that could be customized for both trainees and practicing cardiologists.
Simulation Training
While simulation-based training is not new, its synergy with personalized learning makes for an effective learning tool to achieve and maintain competency in both procedural and nonprocedural domains of cardiology (19,20). It can be employed to enhance existing skills or acquire new skills in a collaborative, low-stress environment. Several studies support the benefit of simulation training in graduate medical education. A quantitative meta-analysis of 14 studies spanning 20 years (1990–2010) demonstrated significant effectiveness of simulation-based medical education with deliberate practice as compared with traditional clinical medical education (21). Although the number of reports analyzed was small, the results suggest a promising and favorable effect of simulation training (21). Similarly, another systematic review examining patient outcomes, such as procedural success or complication rates, in simulation-based medical education demonstrated small to moderate benefits in comparison to no intervention; however, no significant difference was noted when comparing simulation-based training to non-simulation instruction, such as the classical apprenticeship training model (22).
The evidence base supporting the use of simulation-based training in cardiology is slowly mounting (23). One survey found that 84% of respondents learned from some form of simulation training, 64% had participated in mannequin-based simulation, 59% preferred online simulation, and 70% believed simulation training was effective (24). Interventional cardiology fellows scored better on diagnostic coronary angiography skills, with less cine-fluoroscopy exposure, after training with an endovascular simulator (25–27). Similarly, simulation training in transesophageal and transthoracic echocardiography was associated with improved image acquisition skills and efficiency (28,29). The technology also shows promise in other fields, such as resuscitation (30,31) and electrophysiology (32–34). While the strength of the available evidence in these studies is sometimes limited by small sample size, cohort bias, or absence of blinding of assessors to the intervention, the evidence supporting improved performance in real patients following simulation-based training in various cardiovascular procedures is slowly growing (23).
While most simulation training in cardiology has been based on specific curricula, personalization of simulated scenarios is a potentially valuable pathway for lifelong learning. Based on the simulated performance of the learner as evaluated by both the simulator and instructors, layers of complexity can be added. For interventional cardiology simulations, these might include potential complications, such as coronary perforation or air embolism, or advancing to the next steps in patient management, such as percutaneous coronary intervention or valvuloplasty. Based on the physician’s level of training, modules could be personalized as the learner progresses in knowledge and expertise, incorporating more complex and challenging simulation scenarios at more advanced stages of training. In this manner, simulation-based training could prove useful for practicing cardiologists aspiring to avoid skill decay or to demonstrate achievement of minimum competencies for low-volume centers for certain procedures (23).
Coaching has emerged as an important model for medical education (35). Extending simulation training to video-based coaching has been utilized successfully in training surgeons (36). Guided by expert ‘coaches’ and top performers, learners view video recordings of procedures (such as percutaneous coronary intervention or pacemaker insertion) and critique performance. Learners are encouraged to recognize mistakes with the goals of both avoidance and management of complications. While video-based coaching has been used mainly to improve procedural skills, wider use of this technology could expand its scope across an array of practice settings and specialties. Incorporating video-based coaching into competency-based assessments could make it a practical valuable alternative to traditional testing models for practicing cardiologists.
While organized simulation sessions often take place at national conferences, they are typically housed in exhibit halls and are centered around a particular technology or device. Consideration should be given to shifting simulation toward mastery learning. Mastery learning is an emerging paradigm for medical education which espouses two fundamental tenets: 1) educational excellence is not only expected, but can also be achieved by all learners and 2) results should be uniform with little or no variation in outcomes (37). Thus, as learners progress toward their goals at different rates, educational time may vary considerably among learners in a mastery environment (37). In pursuit of mastery learning, simulation sessions could be integrated into the program of the scientific session. Moreover, personalized learning simulation curricula could be developed and shared across societies, providing users with opportunities to advance skills at simulation sessions in meetings more than once a year, track their progress over time, and amalgamate experiences to address gaps in knowledge and skills.
Simulation curricula can be applied to multiple disciplines of cardiology, including but not limited to interventional cardiology and electrophysiology, as a complement to clinical training for FITs and to enhance skill sets for practicing cardiologists (23,25–27,38–40). This would provide opportunities to hone clinical skills and enhance knowledge of the management of a variety of clinical scenarios such as cardiogenic shock, unstable arrhythmias and other frequently encountered conditions. As simulation is still an emerging educational tool in cardiovascular education, further research and validation is needed to confirm its impact on retention of knowledge and clinical outcomes and affirm its value as sufficient to justify the cost and effort involved in creating and promulgating this technology (20). Additionally, further investigation into the optimal amount of simulation experience to learn a new skill set or achieve competence is needed.
Educational Portfolios
While online portfolios are an established method of collecting and documenting formal professional education, they have been underutilized for lifelong learning (41). A personalized educational portfolio created during fellowship and automatically updated throughout one’s career could be helpful to physicians in practice. Content should be specific to the individual’s career focus or clinical interest and might include clinical practice guidelines, best practices, review articles, and pertinent research data. Ideally these resources would be compiled across the breadth of cardiology – from specialty societies to journals to conference proceedings. Quizzes and other self-assessment tools could be generated that could be used to earn credit for continuing medical education. Professional organizations, including the American College of Cardiology, are developing such personalized educational portfolios (42), but the various stakeholders (including professional societies and accrediting bodies) must work together to optimize implementation and dissemination.
Digital Platforms
Digital educational platforms can also be leveraged to create a personalized foundation for lifelong learning. The physician-authored reference site, UpToDate, which provides comprehensive reviews of topics in cardiology and medicine, is viewed more than 32 million times each month by nearly 1.3 million users (43). Trainees and practicing cardiologists also turn to podcasts and webcasts to learn about developments in the field. Weekly audio summaries of Journal of American College of Cardiology (JACC) articles by the Editor-In-Chief have been downloaded more than 3 million times since their inception in 2014 (24) while the College’s ACCEL platform has enjoyed success for over 50 years. Similar podcasts from Circulation (20), “Quick-Take” videos from The New England Journal of Medicine, and online extensions of other journals are also popular. Social media platforms have also been widely adopted. Society-specific Twitter feeds and Facebook pages facilitate information sharing and knowledge dissemination (especially during annual meetings). While these digital tools are presently popular in cardiology graduate medical education, expanding their scope into lifelong learning endeavors is an unfulfilled opportunity.
Virtual journal clubs have emerged as a medium for discussing landmark papers (44). Twitter hashtags and lists allow users to filter content and identify others with common interests. Several professional journals and societies utilize Twitter to conduct journal clubs. Virtual journal clubs bring together participants with diverse backgrounds and perspectives, bridge geographic divides, and promote timely dissemination of research developments and innovations. Twitter journal clubs typically introduce a targeted hashtag, announcing the topic through channels familiar to the intended audience, and invite broad discussion and sharing of clinical experience (45). This avenue of communication and interaction allow researchers to connect with other investigators, clinical experts and patients. Metrics reflecting the number of times posts are shared, retweeted, or marked as favorites, or the popularity of topics or hashtags can be tracked using tools like Altmetric® to assess impact (46).
Personalized online streaming media portals (similar to the Khan Academy model) can enhance professional education. Consolidating podcasts, webcasts, and information from other digital resources (point-of-care references) along thematic categories make these lifelong learning tools readily accessible via the Internet. These commercial resources could be combined or housed by professional societies as an online educational library of member-submitted content and may include de-identified case material, journal clubs, and expert analyses. While proprietary issues may potentially pose a problem, cooperative efforts to ensure appropriate authorship and revenue equity would encourage sharing to promote lifelong learning.
While efforts to consolidate content from various digital resources are necessary, organizing the content so it is readily accessible and searchable is equally important. One solution is to ‘tag’ content. Beyond identifying content across disciplines (i.e. hypertension, acute coronary syndrome, echocardiography, etc), categorizing educational content according to competencies delineated in competency statements would allow cardiologists to identify knowledge gaps and areas that require further study. While such efforts are underway by the College, the ultimate goal would be to create a standardized taxonomy for tagging.
Adaptive Learning
Clinicians learn best when they confront clinical problems that mirror real-world situations, receive feedback on the choices they make, and come to understand their mistakes (47). Adaptive learning employs computational algorithms to continuously adapt questions and outcomes to identify knowledge gaps and enhance performance. This approach provides an opportunity for learning in a practical format that optimizes “teachable moments” and refines clinical acumen.
Eleven medical schools participating in the American Medical Association’s Accelerating Change in Medical Education initiative are developing adaptive learning curricula (48). In this program, faculty seek to identify educational milestones and promote the development of master adaptive learners, emphasizing transitions from pre-medical to undergraduate and graduate medical education (49). At the New York University School of Medicine, clinical choices made by panels of students based on real-time patient data are compared to the decision made by experienced practitioners. At Vanderbilt University, data generated from students in response to online video lectures, demonstrations, discussions, assignments and testing are collected and individual curricula are adapted to focus on areas of weakness (48). Similar data-driven strategies could be adapted to promote lifelong leaning in cardiology. Data compiled from simulations and digital learning tools can form the foundation of high-yield learning modules for fellows and practicing cardiologists.
The New England Journal of Medicine Knowledge+ program is an example of an online adaptive learning platform that could be adapted to cardiologists. Designed for internal medicine physicians as well as subspecialists, this platform uses more than 1500 clinical vignettes developed by expert authors and serial assessments tailored to the specific learning needs of each user. A key feature is the emphasis upon active testing rather than passive reading. The question-delivery engine uses algorithms to assess how an individual learns and delivers questions targeted to knowledge gaps (47). Subject areas in which the examinee scores well are deemphasized in favor of areas in which the user scores poorly to identify knowledge gaps and facilitate acquisition of competency. A similar program is now underway for the educational technology startup, Knowledge to Practice®, which offers CME opportunities to busy cardiovascular professionals through its online, adaptive learning platform and has been featured in the Mayo Cardiovascular Medicine Board Review for initial certification and recertification.
Adaptive learning using small-group, case-based sessions complement conventional medical conferences and can potentially replace didactic, lecture-based sessions (50). In this context, participants critically examine clinical management scenarios under the guidance of expert moderators. Each set of choices (i.e., selection of medical therapies, fluid management, inpatient versus outpatient monitoring, use of invasive procedures or devices) is accompanied by clinical data. Various iterations result in different outcomes. The sessions are followed by debriefing sessions in which mistakes are addressed and corrective actions are explained.
Adaptive methods can also be useful for gaining competency in procedural skills. In a study of trainees learning transesophageal echocardiography in which one group employed an adaptive learning module while the control group did not, the adaptive learning group achieved greater accuracy in diagnosis of cardiac pathology (51). This example may be transferable to other areas of cardiology.
Finally, adaptive learning might be particularly useful to gain mastery of challenging topics such as congenital heart disease or hemodynamics. Adaptive learning programs are well suited to delivery on mobile devices, in keeping with the spirit of lifelong learning, and in the future, could be used not only for self-assessment but also for maintenance of board certification. While the majority of adaptive learning research has focused on trainees, its impact on lifelong learning for practicing cardiologists could be immense but at present requires further exploration.
The Flipped Classroom
In the ‘flipped classroom’ model, the traditional approach by which an instructor provides didactic information to the learner is reversed, and the learner views instructional material (typically via multiple modalities, such as videos, articles, online discussions) in advance and participants work collaboratively on an assignment based on this material. This model is readily applicable to lifelong learning, but having the right type of ‘advance’ work assigned is crucial to success. The content must be engaging, compliant with adult learning theory, and leverage multiple study strategies (visual, auditory, reading/writing, kinesthetic) to accommodate various types of learners.
The flipped classroom has been successfully implemented in other disciplines (52–56), but adoption has been slower in cardiology. Junior trainees randomly assigned to a flipped classroom scored higher on ECG interpretation than a control group taught in a lecture-based classroom (57). The Council on Functional Genomics and Translational Biology evaluated a flipped classroom model at the 2015 American Heart Association Scientific Sessions, and found that learners viewing online videos followed by small-group discussions preferred this method (76%) over didactic lectures (5%) (58). The flipped classroom has been associated with improved problem solving skills, better collaboration with colleagues, and increased satisfaction compared to the traditional classroom model (54,59). This modality has the additional advantages of translating theoretical knowledge into clinical applications and efficiency, which are appealing given time constraints upon physicians at all stages of their careers (60). As with personalized and adaptive learning, technological advances have made flipped classroom learning feasible, scalable, and customizable (61). Content can be customized to accommodate clinical schedules, multiple modalities can be made available in one location or simultaneously in several locations, and the best teachers can reach a larger number of students than is achievable under conventional educational models.
Conclusions and Future Directions
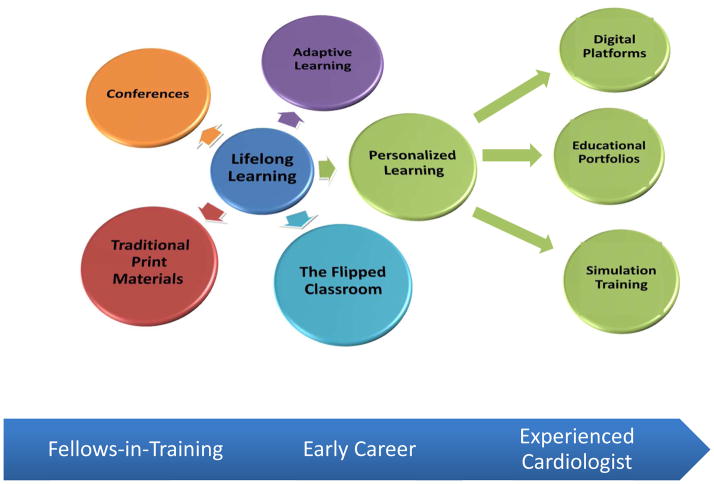
Graduate medical education and lifelong learning are a multifaceted mandate for fellows-in-training and cardiologists in practice to ensure optimal and efficient continuous professional education (Central Illustration). There is a notable lack of published literature on improving lifelong learning in the field of cardiovascular medicine. While learning strategies in graduate medical education have been explored in more depth, this, too, represents a fertile area where further research is warranted. In addition, the cost of implementing novel learning strategies is largely unknown but likely to be significant and the metrics of success for these novel tools (learner satisfaction, knowledge retention, and patient-centered outcomes) compared to standard educational practices needs clarification. Moreover, the growing clinical and non-clinical demands on the time and energy of cardiologists, an accelerating growth of knowledge and technology, increasing sub-specialization, fixed duration of formal training and the importance of achieving and maintaining competency while maintaining a healthy balance between personal pursuits and professional responsibilities remain challenging. Solutions to create an optimal lifelong learning environment depend upon continuously adopting appropriate learning methods and adapting to new techniques. In a technology-driven era, leveraging models such as the educational portfolio, personalized and adaptive learning and the flipped classroom can help balance educational and clinical responsibilities and practice more seamlessly than ever before. In this manner, the unrealized potential of lifelong learning may be achieved.
Central Illustration. Lifelong Learning Tools for Cardiovascular Medicine.
While traditional lifelong learning platforms have centered around conferences and print materials, novel educational platforms (adaptive learning, personalized learning, and the flipped classroom) are emerging as practical solutions to meet the lifelong learning needs of fellows-in-training and practicing cardiologists.
Acknowledgments
Funding: Dr. Sinha acknowledges grant funding from the National Institutes of Health (T32-HL007853).
The FIT Section Leadership Council would like to extend our deepest gratitude to Dr. Jonathan Halperin for his unparalleled guidance and mentorship and for his critical review of this manuscript. Additionally, we are deeply indebted to Mrs. Kristin West for her unwavering support of the FIT Section. Lastly, we are extremely grateful to Mrs. Justine Turco and Dr. Valentin Fuster for providing the FIT Section with the opportunity to write this manuscript.
Abbreviations
- ACGME
Accreditation Council for Graduate Medical Education
- COCATS
Core Cardiovascular Training Statement
- CME
Continuing Medical Education
- FIT
Fellow-in-Training
- GME
Graduate Medical Education
Footnotes
DISCLOSURE: The views expressed in this paper by the American College of Cardiology’s (ACC’s) Fellows-in-Training Section Leadership Council does not necessarily reflect the views of the Journal of the American College of Cardiology or the ACC.
Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Williams ES, Halperin JL, Arrighi JA, et al. 2016 ACC Lifelong Learning Competencies for General Cardiologists: A Report of the ACC Competency Management Committee. J Am Coll Cardiol. 2016;67:2656–95. doi: 10.1016/j.jacc.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 2.Narang A, Sinha SS, Rajagopalan B, et al. The Supply and Demand of the Cardiovascular Workforce: Striking the Right Balance. J Am Coll Cardiol. 2016;68:1680–1689. doi: 10.1016/j.jacc.2016.06.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017;135:e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Combes JR, Arespacochaga E. Physician competencies for a 21st century health care system. J Grad Med Educ. 2012;4:401–5. doi: 10.4300/JGME-04-03-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Virani SS, Maddox TM, Chan PS, et al. Provider Type and Quality of Outpatient Cardiovascular Disease Care: Insights From the NCDR PINNACLE Registry. J Am Coll Cardiol. 2015;66:1803–12. doi: 10.1016/j.jacc.2015.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sinsky C, Colligan L, Li L, et al. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Ann Intern Med. 2016;165:753–760. doi: 10.7326/M16-0961. [DOI] [PubMed] [Google Scholar]
- 7.Madewell JE. Lifelong learning and the maintenance of certification. J Am Coll Radiol. 2004;1:199–203. doi: 10.1016/j.jacr.2003.12.010. discussion 204–7. [DOI] [PubMed] [Google Scholar]
- 8.Chazal RA. Reading the Tea Leaves: Where Will Cardiology Be in 2050? J Am Coll Cardiol. 2016;68:227–30. doi: 10.1016/j.jacc.2016.05.035. [DOI] [PubMed] [Google Scholar]
- 9.Chazal RA. Recognizing Inevitable Change and Responding Responsibly. J Am Coll Cardiol. 2017;69:1637–1639. doi: 10.1016/j.jacc.2017.02.019. [DOI] [PubMed] [Google Scholar]
- 10.Halperin JL, Williams ES, Fuster V. COCATS 4 Introduction. J Am Coll Cardiol. 2015;65:1724–33. doi: 10.1016/j.jacc.2015.03.020. [DOI] [PubMed] [Google Scholar]
- 11.Sinha SS, Julien HM, Krim SR, et al. COCATS 4: Securing the Future of Cardiovascular Medicine. J Am Coll Cardiol. 2015;65:1907–14. doi: 10.1016/j.jacc.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 12.Beliveau ME, Nishimura RA, O’Gara P. Physician competence: a perspective from the practicing cardiologist. Methodist Debakey Cardiovasc J. 2014;10:50–2. doi: 10.14797/mdcj-10-1-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gourevitch D. The history of medical teaching. Lancet. 1999;354(Suppl):SIV33. doi: 10.1016/s0140-6736(99)90376-8. [DOI] [PubMed] [Google Scholar]
- 14.Nishimura RA, Warnes CA. Educating Cardiovascular Fellows in the Contemporary Era: Developing Competent Cardiologists. JAMA Cardiol. 2017;2:119–120. doi: 10.1001/jamacardio.2016.4084. [DOI] [PubMed] [Google Scholar]
- 15.ACGME Program Requirements for Graduate Medical Education in Cardiovascular Disease (Internal Medicine). Accreditation Council for Graduate Medical Education, 2016 (Revision).
- 16.eaching Made Easy - A manual for health professionals. Oxford: Radcliffe Medical Press Ltd; 2000. [Google Scholar]
- 17.Desy JR, Reed DA, Wolanskyj AP. Milestones and Millennials: A Perfect Pairing-Competency-Based Medical Education and the Learning Preferences of Generation Y. Mayo Clin Proc. 2017;92:243–250. doi: 10.1016/j.mayocp.2016.10.026. [DOI] [PubMed] [Google Scholar]
- 18.Kuvin JT, Williams ES. Defining, Achieving, and Maintaining Competence in Cardiovascular Training and Practice. J Am Coll Cardiol. 2016;68:1342–7. doi: 10.1016/j.jacc.2016.05.097. [DOI] [PubMed] [Google Scholar]
- 19.Westerdahl DE. The Necessity of High-Fidelity Simulation in Cardiology Training Programs. J Am Coll Cardiol. 2016;67:1375–8. doi: 10.1016/j.jacc.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 20.Gosai J, Purva M, Gunn J. Simulation in cardiology: state of the art. Eur Heart J. 2015;36:777–83. doi: 10.1093/eurheartj/ehu527. [DOI] [PubMed] [Google Scholar]
- 21.McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86:706–11. doi: 10.1097/ACM.0b013e318217e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zendejas B, Brydges R, Wang AT, Cook DA. Patient outcomes in simulation-based medical education: a systematic review. J Gen Intern Med. 2013;28:1078–89. doi: 10.1007/s11606-012-2264-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harrison CM, Gosai JN. Simulation-based training for cardiology procedures: Are we any further forward in evidencing real-world benefits? Trends Cardiovasc Med. 2017;27:163–170. doi: 10.1016/j.tcm.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 24.ACC. [Accessed: October 8, 2017];Simulation-Based Education: A Popular Tactile Learning Technique. 2016 http://www.acc.org/latest-in-cardiology/articles/2016/11/29/16/31/simulation-based-education.
- 25.Schimmel DR, Sweis R, Cohen ER, Davidson C, Wayne DB. Targeting clinical outcomes: Endovascular simulation improves diagnostic coronary angiography skills. Catheter Cardiovasc Interv. 2016;87:383–8. doi: 10.1002/ccd.26089. [DOI] [PubMed] [Google Scholar]
- 26.Casey DB, Stewart D, Vidovich MI. Diagnostic coronary angiography: initial results of a simulation program. Cardiovasc Revasc Med. 2016;17:102–5. doi: 10.1016/j.carrev.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 27.Voelker W, Petri N, Tönissen C, et al. Does Simulation-Based Training Improve Procedural Skills of Beginners in Interventional Cardiology? --A Stratified Randomized Study. J Interv Cardiol. 2016;29:75–82. doi: 10.1111/joic.12257. [DOI] [PubMed] [Google Scholar]
- 28.Damp J, Anthony R, Davidson MA, Mendes L. Effects of transesophageal echocardiography simulator training on learning and performance in cardiovascular medicine fellows. J Am Soc Echocardiogr. 2013;26:1450–1456. e2. doi: 10.1016/j.echo.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 29.Biswas M, Patel R, German C, et al. Simulation-based training in echocardiography. Echocardiography. 2016;33:1581–1588. doi: 10.1111/echo.13352. [DOI] [PubMed] [Google Scholar]
- 30.Wayne DB, Butter J, Siddall VJ, et al. Simulation-based training of internal medicine residents in advanced cardiac life support protocols: a randomized trial. Teach Learn Med. 2005;17:210–6. doi: 10.1207/s15328015tlm1703_3. [DOI] [PubMed] [Google Scholar]
- 31.Williams H, Yang L, Gale J, et al. Simulation of cardiac emergencies with real patients. Clin Teach. 2015;12:341–5. doi: 10.1111/tct.12322. [DOI] [PubMed] [Google Scholar]
- 32.Maytin M, Daily TP, Carillo RG. Virtual reality lead extraction as a method for training new physicians: a pilot study. Pacing Clin Electrophysiol. 2015;38:319–25. doi: 10.1111/pace.12546. [DOI] [PubMed] [Google Scholar]
- 33.De Ponti R, Marazzi R, Ghiringhelli S, Salerno-Uriarte JA, Calkins H, Cheng A. Superiority of simulator-based training compared with conventional training methodologies in the performance of transseptal catheterization. J Am Coll Cardiol. 2011;58:359–63. doi: 10.1016/j.jacc.2011.02.063. [DOI] [PubMed] [Google Scholar]
- 34.Kalman JM, Joseph SA. Simulation and clinical training: the future and the indispensable past. Heart Rhythm. 2012;9:1286–7. doi: 10.1016/j.hrthm.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 35.Deiorio NM, Carney PA, Kahl LE, Bonura EM, Juve AM. Coaching: a new model for academic and career achievement. Med Educ Online. 2016;21:33480. doi: 10.3402/meo.v21.33480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hu YY, Mazer LM, Yule SJ, et al. Complementing Operating Room Teaching With Video-Based Coaching. JAMA Surg. 2017;152:318–325. doi: 10.1001/jamasurg.2016.4619. [DOI] [PubMed] [Google Scholar]
- 37.McGaghie WC. Mastery learning: it is time for medical education to join the 21st century. Acad Med. 2015;90:1438–41. doi: 10.1097/ACM.0000000000000911. [DOI] [PubMed] [Google Scholar]
- 38.Gurm HS, Sanz-Guerrero J, Johnson DD, et al. Using simulation for teaching femoral arterial access: A multicentric collaboration. Catheter Cardiovasc Interv. 2016;87:376–80. doi: 10.1002/ccd.26256. [DOI] [PubMed] [Google Scholar]
- 39.Bagai A, O’Brien S, Al Lawati H, et al. Mentored simulation training improves procedural skills in cardiac catheterization: a randomized, controlled pilot study. Circ Cardiovasc Interv. 2012;5:672–9. doi: 10.1161/CIRCINTERVENTIONS.112.970772. [DOI] [PubMed] [Google Scholar]
- 40.Jensen UJ, Jensen J, Olivecrona G, Ahlberg G, Lagerquist B, Tornvall P. The role of a simulator-based course in coronary angiography on performance in real life cath lab. BMC Med Educ. 2014;14:49. doi: 10.1186/1472-6920-14-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tochel C, Haig A, Hesketh A, et al. The effectiveness of portfolios for post-graduate assessment and education: BEME Guide No 12. Med Teach. 2009;31:299–318. doi: 10.1080/01421590902883056. [DOI] [PubMed] [Google Scholar]
- 42.Zoghbi WA, Beliveau ME. President’s page: Lifelong learning in the digital age. J Am Coll Cardiol. 2012;60:944–6. doi: 10.1016/j.jacc.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 43.UpToDate. [Accessed: October 8, 2017]; http://www.uptodate.com/home/about-us.
- 44.Mehta N, Flickinger T. The times they are a-changin’: academia, social media and the JGIM Twitter Journal Club. J Gen Intern Med. 2014;29:1317–8. doi: 10.1007/s11606-014-2976-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Topf JM, Sparks MA, Phelan PJ, et al. The Evolution of the Journal Club: From Osler to Twitter. Am J Kidney Dis. 2017 doi: 10.1053/j.ajkd.2016.12.012. [DOI] [PubMed] [Google Scholar]
- 46.Melero R. Altmetrics - a complement to conventional metrics. Biochem Med (Zagreb) 2015;25:152–60. doi: 10.11613/BM.2015.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McMahon GT, Drazen JM. Introducing NEJM Knowledge+ and Its Adaptive Personalized Learning. N Engl J Med. 2014;370:1648–1649. [Google Scholar]
- 48.Creating the Medical School of the Future. American Medical Association; [Google Scholar]
- 49.Why training adaptive learners will be essential to med ed. American Medical Association; [Accessed: October 8, 2017]. https://wire.ama-assn.org/education/why-training-adaptive-learners-will-be-essential-med-ed. [Google Scholar]
- 50.Cooper AZ, Richards JB. Lectures for Adult Learners: Breaking Old Habits in Graduate Medical Education. Am J Med. 2017;130:376–381. doi: 10.1016/j.amjmed.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 51.Romito BT, Krasne S, Kellman PJ, Dhillon A. The impact of a perceptual and adaptive learning module on transoesophageal echocardiography interpretation by anaesthesiology residents. Br J Anaesth. 2016;117:477–481. doi: 10.1093/bja/aew295. [DOI] [PubMed] [Google Scholar]
- 52.Bonnes SL, Ratelle JT, Halvorsen AJ, et al. Flipping the Quality Improvement Classroom in Residency Education. Acad Med. 2017;92:101–107. doi: 10.1097/ACM.0000000000001412. [DOI] [PubMed] [Google Scholar]
- 53.Lew EK. Creating a contemporary clerkship curriculum: the flipped classroom model in emergency medicine. Int J Emerg Med. 2016;9:25. doi: 10.1186/s12245-016-0123-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lin Y, Zhu Y, Chen C, et al. Facing the challenges in ophthalmology clerkship teaching: Is flipped classroom the answer? PLoS One. 2017;12:e0174829. doi: 10.1371/journal.pone.0174829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liebert CA, Lin DT, Mazer LM, Bereknyei S, Lau JN. Effectiveness of the Surgery Core Clerkship Flipped Classroom: a prospective cohort trial. Am J Surg. 2016;211:451–457. e1. doi: 10.1016/j.amjsurg.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 56.Tainter CR, Wong NL, Cudemus-Deseda GA, Bittner EA. The “Flipped Classroom” Model for Teaching in the Intensive Care Unit. J Intensive Care Med. 2017;32:187–196. doi: 10.1177/0885066616632156. [DOI] [PubMed] [Google Scholar]
- 57.Rui Z, Lian-Rui X, Rong-Zheng Y, Jing Z, Xue-Hong W, Chuan Z. Friend or Foe? Flipped Classroom for Undergraduate Electrocardiogram Learning: a Randomized Controlled Study. BMC Med Educ. 2017;17:53. doi: 10.1186/s12909-017-0881-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Musunuru K, Haspel RL Genomics IAtEWGotI-SCCfPEi. Improving Genomic Literacy Among Cardiovascular Practitioners via a Flipped-Classroom Workshop at a National Meeting. Circ Cardiovasc Genet. 2016;9:287–90. doi: 10.1161/CIRCGENETICS.116.001415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ramnanan CJ, Pound LD. Advances in medical education and practice: student perceptions of the flipped classroom. Adv Med Educ Pract. 2017;8:63–73. doi: 10.2147/AMEP.S109037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chokshi BD, Schumacher HK, Reese K, et al. A “Resident-as-Teacher” Curriculum Using a Flipped Classroom Approach: Can a Model Designed for Efficiency Also Be Effective? Acad Med. 2017;92:511–514. doi: 10.1097/ACM.0000000000001534. [DOI] [PubMed] [Google Scholar]
- 61.Williams DE. The Future of Medical Education: Flipping the Classroom and Education Technology. Ochsner J. 2016;16:14–5. [PMC free article] [PubMed] [Google Scholar]