Abstract
Incarceration history can affect sexual health behaviors. A randomized controlled trial of a prevention intervention tailored for post-incarcerated men was administered in a reentry setting. Men ≤45 days post release were recruited into a five-session intervention study. Participants (N = 255) were assessed and tested for three sexually transmitted diseases (STDs) and HIV at baseline and 3 months post-intervention and followed up for 3 more months. The intervention group’s STD risks knowledge (p < .001), partner communication about condoms (p < .001), and condom application skills (p < .001) improved. Although fewer men tested positive for an STD at 3 months post-intervention (10% vs. 8%) and no new HIV cases were found, the finding was not significant. A tailored risk reduction intervention for men with incarceration histories can affect sexual risk behaviors.
Keywords: post release, African American men, STDs, risk reduction, cognitive behavioral
Introduction
Incarceration can affect the health of inmates and their partners, families, and residential communities (Broad et al., 2009; Gaiter, Potter, & O’Leary, 2006; Fullilove, 2006; Flanigan et al., 2010; Iguchi, Bell, Ramchand, & Fain, 2005; James & Glaze, 2006; Jarrett, Adeyemi, & Huggins, 2006; Mallik-Kane & Visher, 2008; Maruschak, 2012; National Center on Addiction and Substance Abuse, 1998, 2010; National Commission on Correctional Health Care, 2002a, 2002b; National Institute on Drug Abuse, 2011). Arrests, detainment, and incarceration disproportionately affect minorities, men, and those who live in low-income and underserved communities, thus perpetuating health disparities (e.g., Crutchfield, 2010; Glaze, 2010; State University of New York, 2003). Risk factors such as low educational attainment, poverty, unemployment, inadequate housing, homelessness, substance use or abuse, intimate partner or family violence, and maltreatment contribute to the likelihood of incarceration and poor health outcomes on an individual and community level (e.g., Crutchfield, 2010; Gaiter et al., 2006; Fullilove, 2006; National Center on Addiction and Substance Abuse, 2010).
Procedures for community reentry from long-term facilities (i.e., prisons) often involve opportunities for detecting, treating, and preventing infectious and chronic diseases (e.g., tuberculosis or HIV) as well as for the continuity of care. Short-term facilities (i.e., jails) might have opt-in (voluntary) or opt-out (refusal based) screening for sexually transmitted diseases (STDs). However, testing without rapid results might increase the possibility of inmates being released without adequate treatment. Given previous findings of sexual risk behaviors immediately post release (e.g., Broad et al., 2009; Flanigan et al., 2010), detection and treatment of STDs before the person’s return to the community has health benefits to the inmate, their sexual networks, and the broader community. Disease detection and treatment before release warrants expedited testing and treatment when possible, but in the absence of such protocols, sexual risk prevention programs and resources that target jail detainees might decrease the STD burden among certain vulnerable populations.
A behavioral and sexual risk reduction intervention was developed and tailored specifically for minority men who were being released from jail. This study aimed to determine the efficacy of the cognitive-behavioral intervention in improving the sexual health of minority men after jail release. The study was led by a local community-based organization (CBO) that provided comprehensive services for men’s reentry, substance use recovery, and HIV testing. Planning and coordination of the study was a collaborative effort among the CBO, the local health department, and the local jail administration. The protocol and instruments were approved by the Centers for Disease Control and Prevention (CDC) institutional review board.
The study was a two-arm, randomized controlled trial of a five-session small group intervention with a baseline assessment (Time 1) and follow-up at immediately post intervention (Time 2), at 3 months (Time 3), and at 6 months (Time 4). This analysis examined four hypotheses: the intervention having an effect on STD knowledge; condom use during sexual episodes; condom communication, negotiation, and application skills; and STD acquisition.
Method
Participants
Men released from jail within 45 days and between 18 and 60 years were recruited in 2003 and 2004 to participate. Recruitment initially focused on one county jail in a large southeastern city and later expanded to another county jail, community centers, probation offices, drug courts, and drug treatment programs. The study opportunity and reentry services were offered by the CBO that managed all on-site study activities. Eligibility criteria included English proficiency, self-reported HIV-negative, sexually active (i.e., penetrative sex with men or women in 30 days before arrest), and use of alcohol or drugs in the month prior to arrest. Participation requirements included attending five 2-hour sessions over 3 consecutive weeks.
After eligibility was determined, men were enrolled immediately, signed consent and release-of-information forms, provided jail release date confirmation and comprehensive contact information, and were given a return date with a description of what to expect. All information was kept confidential, and identifying information was kept separate from participant information. Enrollment continued until 15 cohorts of approximately 22 men were reached.
Randomization and Incentives
Average time between study enrollment and randomization was 21 days. At baseline (Time 1), randomization was conducted using a colored ball method in which participants selected a colored ball that had been designated as either the control or intervention group. After randomization, the control group participants received appointments for their Time 2 assessment and community resources, while the intervention participants started their first session that day. All participants were compensated for public transportation, $20 for baseline assessment, $25 for Time 2, $30 for Time 3, and $40 for Time 4. Intervention group compensation also included public transportation, a T-shirt, and $20 per session. Other incentives (e.g., grocery store/restaurant gift cards) were offered to encourage retention. Refreshments were provided during screening, assessments, and intervention sessions.
Intervention
The intervention, Men Involved in STD Training and Empowerment Research Study (MISTERS), was developed using a cognitive-behavioral, skill-building approach by the CBO executive director, a staff member, and a CDC behavioral scientist. The MISTERS curriculum was based on the information–motivation–behavior model, which posits that changes in HIV risk behavior are a function of having accurate information about prevention, being motivated to change risk behaviors, and having risk-lowering skills (J. D. Fisher & Fisher, 1992; W. A. Fisher & Fisher, 1993; W. A. Fisher, Fisher, & Harman, 2003). Prior to this study, the intervention sessions were pilot-tested with clients who previously used the CBO’s reentry services. Recommendations from the pilot were used to modify the session activities and protocol.
The implemented intervention consisted of five 2-hour group sessions that were completed within a 3-week period. Four Black male facilitators were trained to deliver the curriculum, which incorporated videos, role-playing, group activities, and skill-building practice. Session 1 started with STD and HIV prevention information that included visual media and group activities. Session 2 was a condom use, negotiation, and communication skill-building and practice session. Sessions 3 and 4 included information on avoiding drug use triggers and emotions management (not included in this analysis). At the final intervention session and/or assessment (for controls), all participants received information on supportive community resources, which included job-seeking skills and how to access these resources.
Assessment Procedures and Measures
The assessment included a self-completed questionnaire with sections on the participants’ demographics, incarceration history, knowledge of STDs, substance abuse and sexual behavior history, anger management triggers, and spirituality. The questionnaire was administered in a group setting. Participants also completed two skill assessments: a condom skill assessment and a communication skill assessment, which were both administered to participants individually by a trained interviewer. Each assessment session was completed in approximately 2 hours. The data for the 6-month assessment were excluded from this analysis due to attrition and inadequate power. The selected measures used for this analysis are as described.
STD knowledge was measured by a 15-item tool assessing information about contraceptives, STDs, and condom use (15 points possible). Actual condom use and nonuse during oral, vaginal, and anal sex with main and/or nonmain partners were measured, as well as participants’ present attempts at practicing safer sex. The condom skill assessment was measured by observation of the participants’ ability to correctly place a condom on a penis model and scored by the trained interviewer (9 points possible). Condom use negotiation was measured by a 5-point Likert-type scale assessing agreement with statements related to the participant’s ability to negotiate condom use in certain scenarios. The communication skills assessment recorded the participant’s response to scripted communication and negotiation scenarios. Condom communication skills were observed and scored by a trained interviewer (12 points possible). Perceived STD risk was assessed by asking participants’ perception of risk of STD or HIV if their sex behavior stayed the same as it was before their most recent arrest (10-point Likert-type scale). Participants were also asked about their number of sex partners during the month before their arrest (Time 1), since participating in the intervention (Time 2), and since their last interview (Times 3 and 4). Lastly, STD outcomes were measured through self-reported history of STD, and STD/HIV tests that were administered at Times 1 and 3. Men who tested positive for STDs were referred for treatment.
Analyses
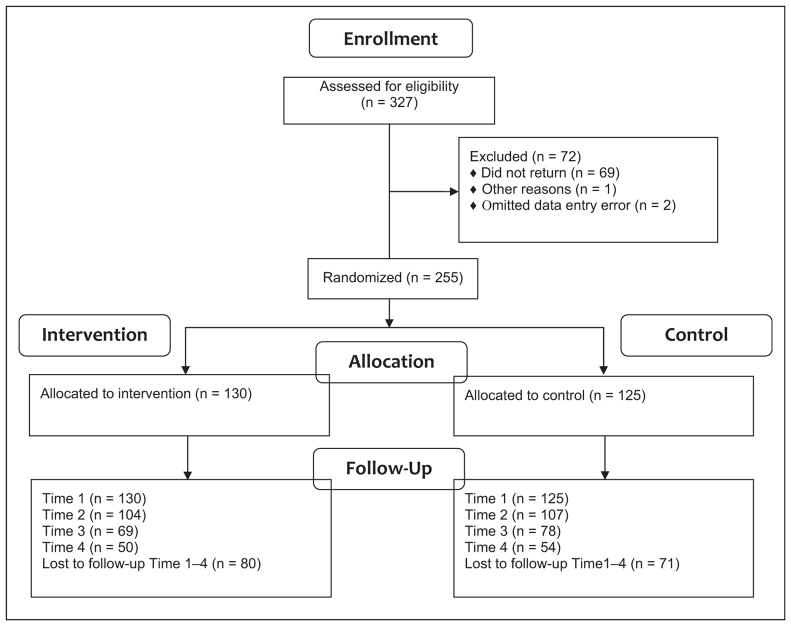
A sample size of 126 per group with a Type I error rate at 0.05 for a two-tailed test yields 84% power to detect a 15% difference in condom use between the intervention and control groups, assuming values of 0.80 and 0.65, respectively. Using an expected recidivism rate of ~30% (Pew Center on the States, 2011), recruitment of 300 men was attempted to maintain power. Analyses were performed on the specified hypotheses and included assessment data for intervention members who may not have completed all sessions. Due to high attrition at the 6-month follow-up (Figure 1), analyses tested the hypotheses at Time 1, Time 2, and Time 3 only.
Figure 1.
Recruitment to follow-up.
A repeated measure design using analysis of variance methods was used to assess mean differences on selected measures (i.e., condom negotiation skills, the ability to communicate about condom use in specific scenarios, and the ability to use condoms correctly) between the intervention and control groups across the three periods as well as within-group differences between the intervention and individual control groups. For STD acquisition, frequencies and proportions were calculated to assess the number of STD infections for each group by assessment time (limited cell size prohibited statistical significance testing for differences).
For condom use outcomes, logistic regression was used to compute relative risk (RR) and 95% confidence intervals (CIs) for the dichotomous outcome (condom use or no condom use). Longitudinal analyses were used to assess condom use over the entire 3-month period (from Time 1 to Time 3 assessment). Multivariate and bivariate tests were used for other variables where appropriate, that is, partner status (main partner or not) and group (intervention or control).
Results
Participants
A total of 327 men were enrolled during April 2003 to February 2004; of these, 69 (21%) discontinued participation after completing the Time 1 questionnaire and 1 person died. After randomization, two cases were omitted due to data entry error. The resulting sample (N = 255) included 130 in the intervention group and 125 in the control group (Figure 1). Most participants were Black, mid-30s, never married, and had completed high school. More than two thirds were unemployed and looking for work before arrest. On average, participants spent 69 nights in jail before enrollment. The control group’s average number of nights in jail at last arrest was 14 nights fewer than that of the intervention group (Table 1). The participants who discontinued the study were similar to those who continued in that the majority were Black (94%), of similar age (median 34 years), never married (67%), and unemployed (70%).
Table 1.
Baseline (Time 1) Demographics.
| Sample Characteristics | Control Group (n = 125) | Intervention Group (n = 130) | ||
|---|---|---|---|---|
|
|
|
|||
| No. | % | No. | % | |
| Mean age (years) | 36.0 | 34.5 | ||
| Race/ethnicity | ||||
| Black, non-Hispanic | 118 | 94.4 | 116 | 89.2 |
| Hispanic | 1 | 0.8 | 1 | 0.8 |
| White, non-Hispanic | 6 | 4.8 | 12 | 9.2 |
| Other | — | — | 1 | 0.8 |
| Marital status | ||||
| Never married | 78 | 62.4 | 82 | 63.1 |
| Married | 15 | 12.0 | 21 | 16.2 |
| Divorced | 26 | 20.8 | 22 | 16.9 |
| Other | 6 | 4.8 | 5 | 3.8 |
| Education | ||||
| ≤12 years | 25 | 20.0 | 38 | 29.2 |
| GED/high school diploma | 75 | 60.0 | 72 | 55.4 |
| Technical school/associate’s degree | 19 | 15.2 | 13 | 10.0 |
| Bachelor’s degree or higher | 3 | 2.4 | 4 | 4.9 |
| Other | 2 | 1.6 | 1 | 1.2 |
| Employment | ||||
| Employed | 20 | 16.0 | 23 | 17.7 |
| Unemployed, seeking work | 85 | 68.0 | 90 | 69.2 |
| Unemployed, not seeking work | 10 | 8.0 | 9 | 6.9 |
| Disabled (and unemployed) | 5 | 4.0 | 4 | 3.1 |
| Other | 4 | 3.2 | 3 | 2.3 |
| Arrest history | ||||
| On parole | 31 | 24.8 | 30 | 23.1 |
| On probation | 59 | 47.2 | 58 | 44.6 |
| Ever convicted of a felony | 76 | 60.8 | 87 | 66.9 |
| Average nights in jails this arrest (mean) | 61.94 | 76.09 | ||
STD Knowledge
Significant differences between the control and intervention groups, F(1.854, 250.294) = 55.494; p < .001, were found at Time 1 and Time 2, but not for Time 3 (Table 2). There was a main effect for STD knowledge across assessment periods, F(1.854, 250.294) = 102.971; p < .0001, with the mean STD knowledge scores increasing from 8.99 at Time 1 to 11.15 at Time 2 and a slight decline (11.03) at Time 3 (Table 3).
Table 2.
Interaction Effects of Intervention Across Assessment Periods.
| Factor | Interaction Effect Across Time 1–3 (n = 255) | I Versus C | Difference Between Means I Versus C | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| T1 M ± SD |
T2 M ± SD |
T3 M ± SD |
Time 1 | Time 2 | Time 3 | ||
| STD knowledge | F(1.854, 250.294) = 55.494*** versus 9.35 ± 2.30 | 8.58 ± 2.51 versus 9.83 ± 2.43 | 12.62 ± 2.08 versus 10.10 ± 2.09 | 12.06 ± 2.08 | p < .001 | p < .001 | — |
| Condom use negotiation | F(2, 266) = 1.092 versus 11.94 ± 2.66 | 11.25 ± 3.09 versus 12.72 ± 2.40 | 12.52 ± 3.12 versus 12.21 ± 2.74 | 12.36 ± 3.01 | — | — | — |
| Condom communication skills | F(1.799, 235.704) = 13.395*** versus 2.30 ± 1.59 | 2.08 ± 1.77 versus 4.24 ± 2.47 | 2.56 ± 1.71 versus 3.35 ± 1.59 | 2.40 ± 1.42 | p < .001 | p < .016 | p < .001 |
| Condom skill assessment | F(1.756,235.341) = 15.753*** versus 6.48 ± 1.70 | 6.66 ± 1.54 versus 6.63 ± 1.55 | 8.46 ± 0.99 versus 6.87 ± 1.29 | 8.12 ± 1.01 | p < .001 | p < .001 | — |
| Perceived STD/HIV risk | F(2, 266) = 1.450 versus 4.69 ± 3.02 | 5.33 ± 3.31 versus 2.60 ± 2.25 | 2.62 ± 2.92 versus 2.51 ± 2.20 | 2.21 ± 2.33 | — | — | — |
| Number of sex partners during the month before arrest | F(1.523,205.630) = 1.005 versus 2.75 ± 2.92 | 3.35 ± 3.43 versus 0.92 ± 0.96 | 0.91 ± 1.67 versus 1.28 ± 1.13 | 1.48 ± 2.43 | — | — | — |
Note. One-way repeated measures analyses of variance (ANOVAs) and 3 × 2 ANOVAs conducted to evaluate main effects of Men in STD Training and Empowerment Research Study at T1, T2, and T3. Post hoc tests using Bonferroni correction conducted to compare across periods. T1 = Time 1; T2 = Time 2; T3 = Time 3; C = control group; I = intervention group; M = mean; SD = standard deviation; STD = sexually transmitted disease.
p < .05.
p < .01.
p < .001.
Table 3.
Main Effects: Intervention Group Versus Control Group.
| Factor | Main Effect Across Time (n = 255) |
T1 | T2 | T3 | Intervention Within-Group Effect (n = 130) |
T1 Versus T2 | T2 Versus T3 | T1 Versus T3 | Control Within- Group Effect (n = 125) |
T1 Versus T2 | T2 Versus T3 | T1 Versus T3 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | ||||
| STD knowledge | F(1.854, 250.294) = 102.971*** | 8.99 ± 2.42 | 11.15 ± 2.66 | 11.03 ± 2.24 | F(1.695, 108.472) = 119.607*** | 8.58 ± 2.51 versus 12.62 ± 2.08*** | 12.62 ± 2.08 versus 12.06 ± 2.08* | 8.58 ± 2.51 versus 12.06 ± 2.08*** | F(2, 142) = 6.153** | 9.35 ± 2.30 versus 9.83 ± 2.43 | 9.83 ± 2.43 versus 10.10 ± 2.09 | 9.35 ± 2.30 versus 110.10 ± 2.09** |
| Condom use negotiation | F(2, 266) = 6.616** | 11.61 ± 2.88 | 12.62 ± 2.76 | 12.28 ± 2.86 | F(1.812, 114.134) = 5.530** | 11.25 ± 3.09 versus 12.52 ± 3.12* | 12.52 ± 3.12 versus 12.36 ± 3.01 | 11.25 ± 3.09 versus 12.36 ± 3.01** | F(2, 140) = 1.995 | — | — | — |
| Condom communication skills | F(1.799, 235.704) = 21.372*** | 2.20 ± 1.67 | 3.35 ± 2.26 | 2.85 ± 1.57 | F(1.666, 103.311) = 24.391*** | 2.30 ± 1.59 versus 4.24 ± 2.47*** | 4.24 ± 2.47 versus 3.35 ± 1.59* | 2.30 ± 1.59 versus 3.35 ± 1.59*** | F(2, 138) = 0.739 | — | — | — |
| Condom skill assessment | F(1.756, 235.341) = 27.427*** | 6.57 ± 1.62 | 7.51 ± 1.60 | 7.47 ± 1.32 | F(1.587, 101.580) = 41.597*** | 6.66 ± 1.54 versus 8.46 ± 0.99*** | 8.46 ± 0.99 versus 8.12 ± 1.01 | 6.66 ± 1.54 versus 8.12 ± 1.01*** | F(2, 140) = 1.791 | — | — | — |
| Perceived STD/HIV risk | F(2, 266) = 53.973*** | 4.99 ± 3.16 | 2.61 ± 2.57 | 2.37 ± 2.26 | F(2, 124) = 29.521*** | 5.33 ± 3.31 versus 2.62 ± 2.92*** | 2.62 ± 2.92 versus 2.21 ± 2.33 | 5.33 ± 3.31 versus 2.21 ± 2.33*** | F(2, 142) = 23.668*** | 4.69 ± 3.02 versus 2.60± 2.25*** | 2.60 ± 2.25 versus 2.51 ± 2.20 | 4.69± 3.02 versus 2.51 ± 2.20*** |
| Number of sex partners during the month before arrest | F(1.523, 205.630) = 52.431*** | 3.04 ± 3.18 | 0.91 ± 1.34 | 1.37 ± 1.86 | F(1.691, 108.237) = 27.953*** | 3.35 ± 3.43 versus 0.91± 1.67*** | 0.91 ± 1.67 versus 1.48± 2.43 | 3.35 ± 3.43 versus 1.48 ± 2.43*** | F(1.284, 91.185) = 23.897*** | 2.75 ± 2.92 versus 0.92 ± 0.96*** | 0.92 ± 0.96 versus 1.28 ± 1.13* | 2.75± 2.92 versus 1.28± 1.13*** |
Note. One-way repeated measures analyses of variance (ANOVAs) and 3 × 2 ANOVAs conducted to evaluate main effects of Men in STD Training and Empowerment Research Study at T1, T2, and T3. Post hoc tests using Bonferroni correction conducted to compare across periods. T1 = Time 1; T2 = Time 2; T3 = Time 3; M = mean; SD = standard deviation; STD = sexually transmitted disease.
p < .05.
p < .01.
p < .001.
Condom Use and Safer Sex Practice Attempt
Logistic regression was used to calculate the RR of using a condom at last time of sex with a main partner and nonmain partner. No differences occurred in reported condom use with a main partner between the intervention and control groups (p = .086). Results were similar for condom use with a nonmain partner with no significant differences observed in condom use when the intervention and control groups were compared (p = .684).
Condom Negotiation, Communication, and Application Skills
Condom use negotiation
No significant differences were found between the control and intervention groups across the 3 periods, F(2, 266) = 1.092 and p = .337, for condom use negotiation (Table 2). The main effect results show difference in the condom use negotiation scores across time periods, F(2, 266) = 6.616 and p ≤ .01. Specifically, the mean scores for the entire sample improved from Time 1 (11.61) to Time 2 (12.62) and declined slightly at Time 3 (12.28), and within-group differences were significant only for the intervention group (see Table 3).
Condom communication skills
As shown in Table 2, significant differences were found between the control and intervention groups across time, F(1.799, 235.704) = 13.395; p < .001. Although the control group started with a higher mean condom communication score at Time 1, the intervention group mean improved significantly at Time 2 and remained higher than the control group at Time 3. The main effect results are shown in Table 3.
Condom application skills
The interaction effect by group and time (Table 2) was statistically significant, F(1.756, 235.341) = 15.753; p < .001. The intervention and control groups differed significantly at Time 1 (p < .001) and Time 2 (p < .001), but not at Time 3. Main effect results indicated a difference in condom skill scores across time, F(1.756, 235.341) = 27.427; p < .001. Within-group differences were significant for the intervention group from Time 1 to Time 2 (p < .001) and Time 1 to Time 3 (p < .001).
Perceived STD Risk and Sex Partners
As shown in Table 2, no significant differences were found between the control and intervention groups with regard to the participants’ perceived STD risk, F(2, 266) = 1.450 and p = .237, or reported number of sex partners, F(1.523, 205.630) = 1.005 and p = .367.
Similar to other measures, main effect differences for perceived STD risk were observed across the periods, F(2, 266) = 53.973; p < .001. Specifically, the perceived risk scores changed across time for both intervention group, F(2, 124) = 29.521; p < .001, and control group, F(2, 142) = 23.668; p < .001 (Table 3).
Reduction in sex partners is identified as a main effect across periods, F(1.523, 205.630) = 52.431; p < .001. As shown in Table 3, the mean number of sex partner for the intervention and control groups was similar in their pattern of change across time. On average, participants reported three sex partners on the Time 1 assessment (3.04 ± 3.18), one partner at Time 2 (0.91 ± 1.34), and one or two partners at Time 3 (1.37 ± 1.86).
STD History and STD Testing Outcomes
As shown in Table 4, 31 (12%) participants self-reported an STD history. However, no significant differences were found between the control and intervention groups (p = .747). In the model with assessment time, group, and assessment by group interaction, no significant assessment by group interaction (p = .975) occurred. As shown in Table 5, 26 (10%) men tested positive for an STD (i.e., gonorrhea, chlamydia, syphilis, and HIV). At Time 3, 12 (8%) men tested positive for an STD. The RR ratio indicated the control group was less likely than the intervention group to say that they had an STD (RR = 0.901, standard error = 0.291, and CI = [0.479, 1.697]), but the difference was not statistically significant.
Table 4.
Sexually Transmitted Disease (STD) History.
| STD | Time 1 (n = 255) | Time 2 (n = 211) | Time 3 (n = 147) | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Intervention n = 130 No. (%) |
Control n = 125 No. (%) |
Intervention n = 104 No. (%) |
Control n = 107 No. (%) |
Intervention n = 69 No. (%) |
Control n = 78 No. (%) |
|
| Gonorrhea | 9 (6.9%) | 5 (4.0%) | 1 (0.9%) | 1 (0.9%) | — | — |
| Chlamydia | 3 (2.3%) | 1 (0.8%) | 1 (0.9%) | 1 (0.9%) | 1 (1.4%) | 1 (1.3%) |
| Syphilis | 4 (3.1%) | 2 (1.6%) | — | — | — | — |
| Genital warts | 1 (0.8%) | — | — | — | — | — |
| Herpes | 2 (1.5%) | 1 (0.8%) | — | — | — | — |
| Pubic lice | — | 1 (0.8%) | — | — | — | — |
| Scabies | 1 (0.8%) | 1 (0.8%) | — | — | — | — |
| Sub-Total by groups | 20 (15.4%) | 11 (8.8%) | 2 (1.9%) | 2 (1.9%) | 1 (1.4%) | 1 (1.3%) |
| Totals by time | 31 (12.2%) | 4 (1.9%) | 2 (1.4%) | |||
Table 5.
Sexually Transmitted Disease (STD) Testing Outcomes.
| STD | Time 1 (N = 255) | Time 3 (N = 147) | ||
|---|---|---|---|---|
|
|
|
|||
| Intervention n = 130 |
Control n = 125 |
Intervention n = 69 |
Control n = 78 |
|
| Gonorrhea | 2 (1.3%) | 3 (2.4%) | 3 (4.3%) | 1 (1.3%) |
| Chlamydia | 6 (4.6%) | 3 (2.4%) | 5 (7.2%) | 1 (1.3%) |
| Syphilis | 4 (3.1%) | 2 (1.6%) | 1 (1.4%) | 1 (1.3%) |
| HIV | 3 (2.3%) | 3 (2.4%) | — | — |
| Cases Group × Time | 15 (11.5%) | 11 (8.8%) | 9 (13%) | 3 (3.8%) |
| Total cases | 26 (10.1%) | 12 (8.1%) | ||
Discussion
This study demonstrated that an intervention tailored for formerly jailed men and implemented post release can enhance certain prevention behaviors. Significant results were identified in STD prevention knowledge, partner communication about condoms, and condom application skills on a model. At baseline, 31 (12%) men self-reported an STD history, and 26 (10%) tested positive for an STD; six of the cases were presumably new HIV cases. At Time 3, 2 (1.4%) men self-reported an STD, yet 12 (8%) participants tested positive for a bacterial STD, and no new HIV cases were found.
The intervention was able to improve STD knowledge, which can be a precursor to changes in behavior (W. A. Fisher et al., 2003), but it seemed to have a limited effect on other sexual risk indicators. The intervention examined in this study did not result in statistically significant decreases in STD acquisition, yet it highlighted the value of providing risk reduction information to men exiting jail. Also, our analysis did not find differences regarding condom use at last sex with a partner, unlike previous intervention studies that reported improvements in protective sex with a main partner among men released from prison (Wolitski, 2006).
Much of the literature regarding negotiation and condom use targets women (Crepaz et al., 2009), but recent work illustrates the benefit of enhancing men’s condom use negotiation (Raiford, Seth, Braxton, & DiClemente, 2013). Communication is considered a crucial component of negotiation (Noar, Carlyle, & Cole, 2009). The main and interaction effects revealed for condom communication skills demonstrate that, within a short time frame, sexual communication skills can be improved (Table 2).
Areas of further research include clarifying what might be missing between the ability to talk about engaging in safer sex and its practice. Sex partners were measured by number and type (main or non-main). Whether the sex partners reported at Time 2 and Time 3 were the same-sex partners before incarceration is unknown. Given the duration of the jail stay that men typically reported (average 69 days), the sex partners reported in Time 2 assessment might have been previous partners with whom condoms were not used. If this is the context, a change in condom use, given the timing of the intervention in relation to detainment time and post release, might have been an unrealistic expectation.
A chief limitation of this study was the retention rate. Efforts to follow up with participants included collecting detailed contact information at screening and confirming that information during the Time 1 assessment. Despite using study staff with demonstrated experience in locating hard-to-reach clients, the retention decreased at each time point. Of the 255 participants, 211 (83%) completed Time 2 assessments, but only 147 (58%) completed the third assessment at Time 3, and only 104 (41%) were located for the 6-month follow-up, which was not included in this analysis. The 42% lost to follow-up at the 3-month post intervention follow-up was substantially greater than the estimated 20%. Follow-up with the population was considerable and often due to circumstances related to participants’ challenges with returning to their lives from detainment. Approaches such as shorter sessions across fewer days may address challenges to retention for this population.
One possible explanation for the lack of an intervention effect might also have been unanticipated memberships in overlapping social networks and neighborhood contexts. More than 70% of the participants were recruited from two jails in two counties. However, the counties were neighboring with few physical boundaries and adequate public transportation. Also, CBOs would offer diverse reentry services to inmates in both jails. We did not require participants to not accept, or to discontinue, any needed reentry or social support services during their participation in the study. With this in mind, it was possible for the men within the cohorts to have met or known each other prior to participating in the study or to have interacted in other contexts during the course of the study, thus creating the opportunity for possible exchange of intervention information (i.e., information from the intervention group is unintentionally shared with members of the control group during casual conversations or encounters). In addition, participants within cohorts had an opportunity to interact during randomization night, which might have contributed to possible intervention information exchange. Intervention information exchange speculation can be supported by the statistically significant main effects identified across periods for all variables included in this analysis (Table 3). Although the possible intervention information exchange speculation compromises the study findings, the reasons for sharing information and peer connection are consistent with evidence-based community reentry programs, which include elements of social capital building (Domurad & Carey, 2010; Wang et al., 2012). Examining geospatial variables, in addition to the behavioral- and skills-related variables, might aid in better understanding the intervention effects.
Despite these limitations, the study also has strengths. At the time the data were collected, collaborative efforts between correctional facilities, reentry organizations, and health departments in facilitating sexual health and STD prevention behaviors among post jail-release adults were limited. The collaboration raised awareness of the sexual health needs of formerly incarcerated men. Incorporating community feedback into the intervention’s curriculum increased acceptability among the community stakeholders.
The study also was an example of how criminogenic factors could be included in the conceptualization and operationalization of an STD prevention intervention. The findings from this study, along with the findings from the study that included a modified version of the MISTERS intervention (Potter, Akers, & Bowman, 2013), provide dual examples of how sexual risk prevention can be applied to reentry preparation, and potentially prevention of recidivism.
The data and intervention have contemporary relevance, though the data are not recent. To date, there has not been an intervention study that has examined the efficacy of an STD risk reduction program tailored for minority men exiting jails, beyond the replication study mentioned prior (Potter et al., 2013). For this reason, the results from this analysis contribute to both the contemporary corrections and STD literature regarding risk reduction and prevention education, partner communication, and the condom use efficacy of formerly incarcerated minority men. Also, the main effect findings indicating improvement across the entire sample points to the public health opportunity after jail detainment when STD screening and risk reduction prevention are initiated upon release, which could be an enhancement if initiated at jail entry. Continued examination of the individual, social, criminogenic, and contextual factors that influence the sexual health outcomes of persons with histories of incarceration and shorter term detainment would mutually inform correctional and public health efforts.
Acknowledgments
The authors gratefully acknowledge the contributions of the MISTER Project Research Group, which was led by Charles Sperling, MS.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by cooperative agreement U52/CCU422491 titled “MISTERS Project: A Community-Based STD/HIV Intervention for Men Newly Released from Jail” and funded by the Centers for Disease Control and Prevention.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. For information about JCHC’s disclosure policy, please see the Self-Study Program.
References
- Broad J, Cox T, Rodriguez S, Mansour M, Murphy-Swallow D, … Wong W. The impact of discontinuation of male STD screening services at a large urban county jail: Chicago, 2002–2004. Journal of Sexually Transmitted Diseases. 2009;36:S49–S52. doi: 10.1097/OLQ.0b013e318156159a. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Marshall LW, Aupont ED, Jacobs ED, Mizuno Y, Kay LS, … O’Leary A. The efficacy of HIV/STI behavioral interventions for African American females in the United States: A meta-analysis. American Journal of Public Health. 2009;99:2069–2078. doi: 10.2105/AJPH.2008.139519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crutchfield RD. Racial and ethnic disparity and criminal justice: How much is too much? Journal of Criminal Law and Criminology. 2010;100:903–932. [Google Scholar]
- Domurad F, Carey M. Implementing evidence-based practices—Coaching packet. Silver Spring, MD: Center for Effective Public Policy; 2010. Retrieved from http://www.reentrycoalition.ohio.gov/docs/initiative/coaching/Implementing%20Evidence%20Based%20Practices.pdf. [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher WA, Fisher JD. A general social psychological model for changing AIDS risk behavior. In: Pryor JB, Reeder GD, editors. The social psychology of HIV infection. Hillsdale, NJ: Lawrence Erlbaum; 1993. pp. 127–153. [Google Scholar]
- Fisher WA, Fisher JD, Harman JJ. The information–motivation–behavioral skills model: A general social psychological approach to understanding and promoting health behavior. In: Suls J, Wallston KA, editors. Social psychological foundations of health. London, England: Blackwell; 2003. pp. 82–106. [Google Scholar]
- Flanigan TP, Zaller N, Beckwith CG, Bazerman LB, Rana A, Gardner A, … Altice FL. Testing for HIV, sexually transmitted infections, and viral hepatitis in jails: Still a missed opportunity for public health and HIV prevention. Journal of Acquired Immune Deficiency Syndromes. 2010;55:S78–S83. doi: 10.1097/QAI.0b013e3181fbc94f. [DOI] [PubMed] [Google Scholar]
- Fullilove R. African Americans, health disparities and HIV/AIDS: Recommendations for confronting the epidemic in Black America. Washington, DC: National Minority AIDS Council; 2006. Retrieved from http://img.thebody.com/nmac/blacks_aids.pdf. [Google Scholar]
- Gaiter JL, Potter RH, O’Leary A. Disproportionate rates of incarceration contribute to health disparities. American Journal of Public Health. 2006;96:1148–1149. doi: 10.2105/AJPH.2006.086561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaze LE. Correctional populations in the United States, 2009 (NCJ 231681) Washington, DC: Bureau of Justice Statistics; 2010. Retrieved from http://www.bjs.gov/content/pub/pdf/cpus09.pdf. [Google Scholar]
- Iguchi MY, Bell J, Ramchand RN, Fain T. How criminal system racial disparities may translate into health disparities. Journal of Health Care for the Poor and Underserved. 2005;16:48–56. doi: 10.1353/hpu.2005.0114. [DOI] [PubMed] [Google Scholar]
- James DJ, Glaze LE. Mental health problems of prison and jail inmates (NCJ 213600) Washington, DC: Bureau of Justice Statistics; 2006. Retrieved from http://bjs.ojp.usdoj.gov/content/pub/pdf/mhppji.pdf. [Google Scholar]
- Jarrett NC, Adeyemi SA, Huggins T. Bridging the gap: Providing health care to newly released men. Journal of Health Care for the Poor and Underserved. 2006;17:70–80. doi: 10.1353/hpu.2006.0008. [DOI] [PubMed] [Google Scholar]
- Mallik-Kane K, Visher C. Health and prisoner reentry: How physical, mental, and substance abuse conditions shape the process of reintegration. Washington, DC: The Urban Institute; 2008. Retrieved from http://www.urban.org/sites/default/files/alfresco/publication-pdfs/411617-Health-and-Prisoner-Reentry.PDF. [Google Scholar]
- Maruschak LM. HIV in prisons (NCJ 238877) Washington, DC: Bureau of Justice Statistics; 2012. Retrieved from http://www.bjs.gov/content/pub/pdf/hivp10.pdf. [Google Scholar]
- National Center on Addiction and Substance Abuse at Columbia University. Behind bars: Substance abuse and America’s prison population. 1998 Retrieved from https://www.centeronaddiction.org/addiction-research/reports/behind-bars-substance-abuse-and-america%E2%80%99s-prison-population.
- National Center on Addiction and Substance Abuse at Columbia University. Behind bars II: Substance abuse and America’s prison population. 2010 Retrieved from https://www.centeronaddiction.org/addiction-research/reports/behind-bars-ii-substance-abuse-and-america%E2%80%99s-prison-population.
- National Commission on Correctional Health Care. The health of soon-to-be-released inmates: A report to Congress. 2002a;1 Retrieved from http://www.ncchc.org/filebin/Health_Status_vol_1.pdf. [Google Scholar]
- National Commission on Correctional Health Care. The health of soon-to-be-released inmates: A report to Congress. 2002b;2 Retrieved from http://www.ncchc.org/filebin/Health_Status_vol_2.pdf. [Google Scholar]
- National Institute on Drug Abuse. Comorbidity: Addiction and other mental disorders. 2011 Retrieved from https://www.drugabuse.gov/publications/drugfacts/comorbidity-addiction-other-mental-disorders.
- Noar SM, Carlyle K, Cole C. Why communication is crucial: Meta-analysis of the relationship between safer sexual communication and condom use. Journal of Health Communication. 2009;11:365–390. doi: 10.1080/10810730600671862. [DOI] [PubMed] [Google Scholar]
- Pew Center on the States. State of recidivism: The revolving door of America’s prisons. Washington, DC: Author; 2011. Retrieved from http://www.pewtrusts.org/~/media/legacy/uploadedfiles/pcs_assets/2011/pewstateofrecidivismpdf.pdf. [Google Scholar]
- Potter RH, Akers TA, Bowman D. Replicating MISTERS: An epidemiological criminology framework analysis of a program for criminal justice-involved minority males in the community. Journal of Correctional Health Care. 2013;19:4–14. doi: 10.1177/1078345812458085. [DOI] [PubMed] [Google Scholar]
- Raiford JL, Seth P, Braxton ND, DiClemente RJ. Masculinity, condom use self-efficacy and abusive responses to condom negotiation: The case for HIV prevention for heterosexual African-American men. Sexual Health. 2013;10:467–469. doi: 10.1071/SH13011. [DOI] [PubMed] [Google Scholar]
- State University of New York at Albany. Sourcebook of criminal justice statistics, Characteristics of Federal prisoners. 2003 Retrieved from http://www.albany.edu/sourcebook/pdf/t653.pdf.
- Wang EA, Hong CS, Shavit S, Sanders R, Kessell E, Kushel MB. Engaging individuals recently released from prison into primary care: A randomized trial. American Journal of Public Health. 2012;102:e22–e29. doi: 10.2105/AJPH.2012.300894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitski RJ. Relative efficacy of a multisession sexual risk-reduction intervention for young men released from prisons in 4 states. American Journal of Public Health. 2006;96:1854–1861. doi: 10.2105/AJPH.2004.056044. [DOI] [PMC free article] [PubMed] [Google Scholar]