Abstract
Background
Lower ethnic-specific body mass index (BMI) cutpoints have been proposed for Asians and adapted in some countries. However, to our knowledge, no study has directly compared Asians to other ethnic groups to test differences in associations between BMI and all-cause mortality using common methods.
Objectives
We estimated the association between BMI and all-cause mortality in Chinese Asians and Caucasian Americans to determine if lower Asian-specific BMI cutpoints are warranted.
Methods
Extant data of the People’s Republic of China Study (1983-1997) including 5546 Chinese and the Atherosclerosis Risk in Communities Study (1987-2002) including 9932 Caucasians aged 45-64 years at baseline were used. All analyses were performed using Cox proportional regression models.
Results
Standardized mortality rates were 6.88 (95% confidence interval (CI): 5.75-8.24) and 5.50 (95% CI: 4.74-6.39) per 1000 person-years for Chinese and Caucasians, respectively. Standardized mortality probabilities by age 70 were similar across all BMI categories among Chinese. Furthermore, the probabilities were similar to those among Caucasians with BMI of 27.5-<32.5 kg/m2. The BMI associated with lowest mortality risk was almost identical between Chinese (25.1 kg/m2) and Caucasians (25.2 kg/m2). The analysis of categorical BMI did not reveal an increased mortality risk at any BMI category among Chinese. In contrast, compared to those with a BMI of 23.0-<25.0 kg/m2, risk was elevated by 35% among Caucasians with a BMI of 30.0-<32.5 kg/m2.
Conclusions
These findings do not support different BMI cutpoints for Chinese than Caucasians on the basis of mortality rates.
Keywords: body mass index, all-cause mortality, Chinese, Caucasians, BMI cutpoint
INTRODUCTION
It is has been proposed that Asian populations experience more morbidity and mortality at a lower body mass index (BMI) compared to Caucasian populations in the United States and Europe possibly due to a higher percentage of body fat and abdominal obesity among some Asian populations.1 This notion has led to recommendations for lower ethnic-specific cutpoints of 23.0 kg/m2 for overweight (instead of 25.0 kg/m2) and 25.0 kg/m2 for obesity (instead of 30.0 kg/m2). Those advocating lower BMI cut-points for Asian populations have based their arguments mainly on studies of the relationship between BMI and cardiometabolic risk factors, with little data on mortality.
With the notable exception of diabetes, cardiometabolic risk factors do not themselves affect length of life, but are important causes of more serious outcomes (e.g., heart disease, cancer) that can lead to premature death. Since the associations between risk factors, disease and mortality can vary by ethnic group, risk factors alone might not be logical outcomes on which to base BMI standards.2 For well over 50 years mortality has been an important outcome in the formulation of recommendations for desirable weight for height. Mortality studies formed the basis of Metropolitan Life Insurance Studies tables of desirable weight for height,3 and studies of BMI-mortality were included in the determination of the now widely used World Health Organization (WHO) BMI cutpoints for normal weight (18.5-<25.0 kg/m2), overweight (≥25.0 kg/m2) and obesity (≥30.0 kg/m2).4–7
Stevens et al have extensively discussed the logic of BMI cutpoint determination with specific reference to whether different BMI cutpoints for obesity are needed in Asians.2,6,8,9 They advocated basing the decision on the examination of BMI associations with quality of life measures and specific “hard” health outcomes (e.g., myocardial infarction, cancer). Additionally, studies of mortality were advised with careful comparisons made among ethnic groups to determine the BMI levels associated with increased risk. These kinds of comparisons are stronger when derived from a pooled analysis of original data that directly contrast associations in different ethnic groups estimated using similar methodologies.
A recent pooled analysis of 19 cohorts10 estimated the effect of BMI on all-cause mortality in more than 1 million Chinese, Japanese and Koreans and showed that risk was U-shaped with elevated risk at a BMI lower or higher than the reference category of 22.6-25.0 kg/m2. This study provided important information on the shape of the BMI-mortality association in Asians in multiple countries, but since other ethnic groups were not included, ethnic comparisons could not be made directly. To our knowledge no previous study has directly compared the BMI-mortality associations in Asians to those among other ethnic groups in a pooled study using the same analytical methods. Therefore, the goal of this study was to directly compare the associations between BMI and all-cause mortality among Chinese Asians and Caucasian Americans using individual-level data from the People’s Republic of China (PRC) and the Atherosclerosis Risk in Communities (ARIC) Studies.
METHODS
Study population
The PRC study included urban and rural populations from Beijing (northern China) and Guangzhou (southern China).11 In this analysis 6588 Chinese men and women aged 45-64 years at baseline (1983-1984) were included to match the age range of the ARIC data. The ARIC cohort recruited 11 478 Caucasian men and women aged 45-64 years at baseline (1987-1989) from three US communities (Forsyth County, NC; the northwestern suburbs of Minneapolis, MN; and Washington County, MD).12 In both cohorts individuals with missing information on baseline BMI, mortality, smoking, alcohol consumption and education (in ARIC only) were excluded (59 Chinese and 53 Caucasians). A separate category for missing education among Chinese was created since 2.5% of Chinese had missing information and we wanted to avoid losing this large proportion of data. Furthermore, individuals with a BMI <18.5 kg/m2 (945 Chinese and 97 Caucasians) and ≥32.5 kg/m2 (38 Chinese and 1396 Caucasians) were excluded to improve comparability between the ethnic groups since the numbers of Caucasian Americans with a BMI <18.5 kg/m2 and Chinese with a BMI ≥32.5 kg/m2 were extremely low. The final dataset included 5546 Chinese and 9932 Caucasians. These studies were approved by the Institutional Review Boards (IRB) at each field center and this secondary analysis was approved by the University of North Carolina at Chapel Hill (UNC) Non-Biomedical IRB on research involving human subjects.
Baseline and follow-up assessment
The Collaborative Studies Coordinating Center at UNC developed the protocols and training manuals for all measurements and handled the review, processing and analyses of all data from PRC and ARIC. In both cohorts body weight was measured to the nearest pound using a beam balance scale with participants wearing light clothing in PRC and a scrub suit in ARIC.11,12 Height was measured to the nearest centimeter using a metal ruler attached to a wall and a standard triangular headboard with participants wearing no shoes. Height and weight were used to calculate BMI, which was categorized using the WHO categories: 18.5-<23.0 kg/m2, 23.0-<25.0 kg/m2, 25.0-<27.5 kg/m2, 27.5-<30.0 kg/m2, and 30.0-<32.5 kg/m2.
Interviewer-administered questionnaires assessed education, smoking and alcohol consumption at baseline.12 Education was categorized as low, medium and high to improve comparability between education in the US and in China. Current smoking status and alcohol consumption were dichotomized.
Outcome ascertainment
In PRC, vital status was ascertained in 1997 during a follow-up examination or through contacting the participants’ homes or workplaces. For all descendents death certificates were obtained. To ascertain vital status in ARIC in 2002, cohort and community surveillance including discharge lists from local hospitals, local obituaries and annual vital statistics reviews tapes were used.12,13 Vital status and date of death are known in approximately 99% of the PRC and ARIC cohorts.
Statistical analysis
Poisson regression was used to calculate crude incidence rates and incidence rates standardized to a BMI of 21 kg/m2, which is consistent with a previous study,14 nonsmoker, non-drinker at age 53.2 years (mean age) using the overall gender distribution (53.7% female) and ethnic-specific distributions for education and field center. This standardization was also used to estimate mortality probabilities by age 70 by BMI category. Estimates by age 70 were chosen since we considered death at that age premature, yet not uncommon. We used Cox regression models15 to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between all-cause mortality and BMI using the five WHO BMI categories and continuous BMI. The proportional hazards assumption, tested by examining Kaplan-Meier survival curves and Schoenfeld residuals, was not violated. Likelihood Ratio Tests were used to determine a parsimonious model that described the relationship between the exposure variables and mortality. We first examined quadratic spline regression models16 with 9-knots using years in study as the time scale. By testing successively simplified models we found that a quadratic model was sufficient for analysis of both ethnic groups. These models were adjusted for field center, centered age, centered age squared, gender, education, smoking status and alcohol consumption. The gender-BMI interaction was not significant and, thus results stratified by gender are not presented. All statistical analyses were performed using SAS, version 9.2 (SAS Institute, Inc, Cary, NC, USA).
RESULTS
Baseline characteristics are presented in Table 1. Chinese were on average slightly younger and had a lower mean BMI at baseline than Caucasians. The crude mortality rate, per 1000 person-years, was 7.93 (95% CI: 7.27-8.58) for Chinese and 9.14 (95% CI: 8.63-9.65) for Caucasians. After standardization, mortality rates decreased to 6.88 (95% CI: 5.75-8.24) and 5.50 (95% CI: 4.74-6.39), respectively.
Table 1.
Baseline characteristics of the Chinese Asians and Caucasian Americans in the People’s Republic of China and the Atherosclerosis Risk in Communities Studies
| Characteristics | Chinese (n=5546) | Caucasians (n=9932) |
|---|---|---|
| Age at baseline (years) [mean (SD†)] | 51.0 (4.2) | 54.4 (5.7) |
| BMI [N (%)]‡ | ||
| 18.5 to <23.0 kg/m2 | 3121 (56.3%) | 2180 (22.0%) |
| 23.0 to <25.0 kg/m2 | 1089 (19.6%) | 1966 (19.8%) |
| 25.0 to <27.5 kg/m2 | 819 (14.8%) | 2658 (26.8%) |
| 27.5 to <30.0 kg/m2 | 403 (7.3%) | 1923 (19.4%) |
| 30.0 to <32.5 kg/m2 | 114 (2.1%) | 1205 (12.1%) |
| BMI (kg/m2) [mean (SD†)] | 22.9 (3.0) | 25.8 (3.2) |
| Female gender | 2744 (49.5%) | 5072 (51.1%) |
| Education | ||
| Low | 1669 (30.1%) | 1625 (16.4%) |
| Medium | 2528 (45.6%) | 3570 (35.9%) |
| High | 891 (16.1%) | 4737 (47.7%) |
| Missing§ | 458 (8.3%) | – |
| Current smokers | 2669 (48.1%) | 2836 (28.6%) |
| Current consumers of alcoholic beverages | 1543 (27.8%) | 6552 (66.0%) |
SD: standard deviation.
Individuals with a BMI <18.5 and ≥32.5 were excluded to improve comparability between ethnic groups.
Chinese with missing information on education were included as a separate category to avoid too extensive missing data.
Figure 1 shows the standardized mortality probabilities by age 70 by BMI categories. The mortality probability (pr) at a BMI of 18.5-<23.0 kg/m2 was similar between Chinese (pr=0.14) and Caucasians (pr=0.10). In contrast, across the span of 23.0-<30.0 kg/m2 the probability of dying was lower among Caucasians (pr=0.09-0.10) than Chinese (pr=0.15). Finally, the mortality probabilities were similar between the two ethnic groups in the highest BMI category (pr=0.12). Within ethnic groups, the mortality probabilities did not fluctuate much among Chinese and Caucasians across BMI categories.
Figure 1.
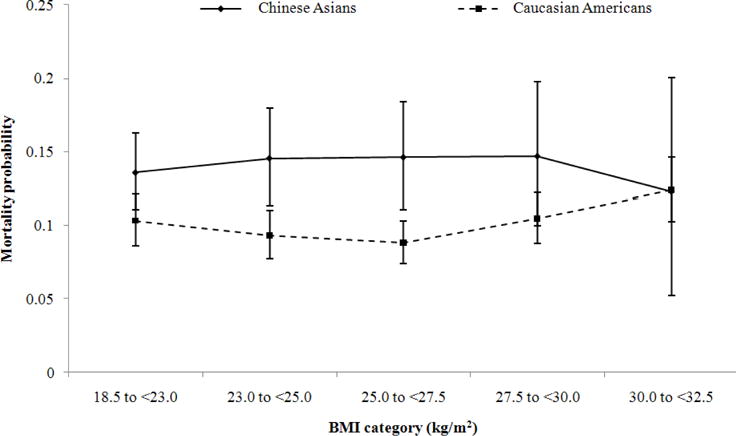
Mortality probability by age 70 years among Chinese Asians and Caucasian Americans standardized to a BMI of 21 kg/m2, nonsmoker, nondrinker at age 53.5 years (mean age) using the overall gender distribution of 53.7% female and ethnic-specific distributions for education and field center.
No association between any BMI category and mortality was observed in Chinese (Table 2). Compared to a BMI of 23.0-<25.0 kg/m2, a BMI of 30.0-<32.5 kg/m2 significantly elevated mortality risk by 35% (95% CI: 1.11-1.64) among Caucasians. The association between continuous BMI and all-cause mortality was a U-shaped among Caucasians and to a lesser degree also among Chinese (Figure 2). The BMI associated with the lowest mortality risk was almost identical between Chinese (25.1 kg/m2) and Caucasians (25.2 kg/m2).
Table 2.
Association between BMI and all-cause mortality among Chinese Asians and Caucasian Americans†
| BMI categories | Chinese
|
Caucasians
|
||||
|---|---|---|---|---|---|---|
| Events | HR‡ | 95% CI‡ | Events | HR‡ | 95% CI‡ | |
| 18.5 to <23.0 kg/m2 | 314 | 0.93 | 0.74, 1.16 | 246 | 1.11 | 0.93, 1.34 |
| 23.0 to <25.0 kg/m2 | 112 | 1.00 | 225 | 1.00 | ||
| 25.0 to <27.5 kg/m2 | 84 | 1.01 | 0.76, 1.34 | 306 | 0.94 | 0.79, 1.12 |
| 27.5 to <30.0 kg/m2 | 37 | 1.01 | 0.70, 1.47 | 270 | 1.13 | 0.95, 1.35 |
| 30.0 to <32.5 kg/m2 | 10 | 0.84 | 0.44, 1.60 | 193 | 1.35 | 1.11, 1.64 |
Adjusted for gender, centered age, centered age squared, field center, education, smoking status and alcohol consumption.
HR: hazard ratio; CI: confidence interval.
Figure 2.
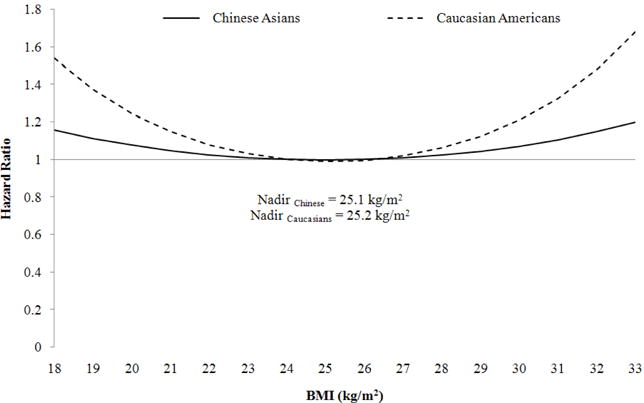
Continuous, quadratic BMI and all-cause mortality among Chinese Asians and Caucasian Americans adjusted for field center, centered age, centered age squared, gender, education, smoking status and alcohol consumption.
DISCUSSION
This study contrasted the BMI-mortality association in Chinese and Caucasians using several different approaches. We found that across a BMI of 18.5 to <30.0 kg/m2 the probability of dying by age 70 tended to be higher among Chinese than Caucasians, but similar probabilities were observed at the highest BMI category (30.0 to <32.5 kg/m2). Our analyses of death rates in BMI categories showed no increase associated with overweight or obesity in Chinese, whereas rates were significantly increased in obese Caucasians. Perhaps, most importantly the BMI associated with the lowest mortality risk was ~25 kg/m2 among Chinese and Caucasians. Thus, these results gave no support to the hypothesis that Chinese suffer increased risk of death due to excess weight at a lower BMI than Caucasians or that the risk of death is elevated at a BMI of 23 in the Chinese population.
Researchers17–19 and policy-making organizations7,20 have used different approaches to advocate for lower BMI cutpoints. A common argument is that Asians have a higher percent body fat at a lower BMI compared to Caucasians. For example, a study among 242 Asians (93% Chinese) and 445 Caucasians living in New York showed that Asians of the same age and sex had on average a lower BMI but a higher percentage of body fat than Caucasians, as measured by dual photon absorptiometry.21 A literature review22 concluded that at the same BMI, Asian populations (Indonesians, Singaporean Chinese, Malays, Indians and Hong Kong Chinese) had a higher mean percent body fat than Caucasians as assessed by deuterium oxide dilution or dual-energy X-ray absorptiometry. Another study23 found no differences in percent body fat between Caucasians in the Netherlands and Chinese in Beijing using underwater weighing. However, the groups were not matched on BMI (the average BMI was 23.3±2.9 in Caucasians and 22.3±3.1 kg/m2 in Chinese). Finally, the WHO expert consultation reported that Hong Kong Chinese, Indonesians, Singaporeans, urban Thai and young Japanese had lower BMI levels than Europeans at the same body fat, while Beijing Chinese and rural Thai had similar values to those of Europeans.1 This study indicated potentially important differences among different Asian groups. More studies are needed to better understand these ethnic and national variations.
Despite evidence supporting differences in body composition, a review by Stevens and Nowicki6 did not indicate increased risk of all-cause mortality in Asian populations at a BMI lower than 30. To our knowledge, studies in Chinese published since this review further support this conclusion and estimated that the BMI associated with the lowest mortality risk was within the normal WHO BMI range and sometimes even extended into overweight.4,5,24
Wen et al4 studied the BMI-mortality association in 36 386 civil servants and school teachers in Taiwan aged 40 years and older. They found that a BMI of 15.0-24.9 kg/m2 was associated with the lowest mortality risk. Compared to non-smokers in the reference category of 18.5-22.9 kg/m2, risk was not significantly different among non-smokers with a BMI of 15.0-18.4 kg/m2 (RR=0.88, 95% CI: 0.51-1.51) or 23.0-24.9 kg/m2 (RR=1.00, 95% CI: 0.82-1.22). However, mortality risk increased by ~25% for BMI ≥25.0 kg/m2, by 64% for BMI ≥30.0 kg/m2 and by 130% for BMI ≥35.0 kg/m2 indicating that the standard WHO BMI cutpoints are consistent with the patterns of increased mortality risk in this Chinese sample.
Although Wen et al did not observe increased mortality risk below a BMI of 25, they concluded that the WHO cutpoints are too high for use in Chinese. The authors suggested that BMI cutpoints for overweight should be lowered for Chinese such that there would be no increase in mortality in the group called “overweight” (25.0-29.9 kg/m2), as was seen in the study by Flegal et al in American Caucasians in the combined National Health and Nutrition Examination Surveys I, II and III.25 In that study, compared to Caucasians with a BMI of 18.5-24.9 kg/m2, the relative risk among overweight Caucasians was not increased. Wen et al contended that a BMI of 23.0-24.9 kg/m2 should be called overweight since Chinese in that BMI range were not at increased risk compared to Chinese with a BMI of 18.5-22.9 kg/m2. Similarly, since the relative mortality risk in the obesity I category (30.0-34.9 kg/m2) in Caucasians was elevated and comparable in magnitude to the relative risk among overweight Chinese, they suggested 25.0 kg/m2 as a cutpoint for obesity in Chinese. This logic could be debated, and other issues need to be considered. These two studies are not directly comparable because they used different reference categories for some comparisons, with Wen et al using 18.5-22.9 kg/m2 and Flegal et al using 18.5-24.9 kg/m2. Furthermore, the samples differed considerably in the ranges of ages included and the adjustment factors used. Last, the use of relative rather than absolute risk should be considered.
Another large cohort study5 among a nationally representative sample of 154 736 Chinese aged 40+ years used ten BMI categories and found a U-shaped relationship between BMI and mortality with the lowest risk being associated with a BMI of 24.0-26.9 kg/m2. Similarly, a cohort study that examined 71 243 women (40-70 years) from the Shanghai Women’s Health Study found an inverse J-shaped association between BMI and mortality with an elevated risk associated with underweight and a lower risk associated with BMI 18.5-29.9 kg/m2 compared to the obese category according to the standard WHO BMI categories.24 Other studies investigating the association between BMI and mortality among Chinese focused on samples of elderly adults.26–28 The findings of these studies may not be representative of BMI associations over all adults since BMI at older ages could be a marker of factors other than adiposity (e.g., muscle mass, fitness and health status).27
It was unexpected that overweight and obesity were not associated with mortality rates in Chinese in our analysis and that only obesity was associated with mortality in Caucasians. A reason for these mostly null findings could be that all-cause mortality is a too crude measure to capture health risks of BMI. Additionally, the main causes of death differ between ethnic groups. The top three leading causes of death among Caucasians in the US are diseases of the heart, malignant neoplasms and cerebrovascular disease,29 compared to cerebrovascular disease, chronic obstructive pulmonary disease and ischemic heart disease in China,30 Unfortunately, ICD-9 codes were not available for the PRC to determine cause-specific mortality. However, studies like ours that determine the differential effects of BMI on definite outcomes, such as all-cause mortality, by ethnic groups are needed as an evidence base for clinical recommendations.
Our study had several strengths including the use of the same coordinating center for the Chinese and Caucasians samples and use of measured weight and height. Further, all-cause mortality is an easily standardized outcome on which recommendations for BMI have been based previously. It is a strength that we provided mortality probabilities as a measure of absolute risk, and that we used flexible modelling to determine the BMI associated with the lowest risk in each ethnic group. Our sample of Chinese was from China, making our comparisons relevant to the different BMI cutpoints that are applied there.
A limitation was that confounders, such as education level, might not be directly comparable across ARIC and PRC as they are country-specific; however, we did standardize these values by ranking individuals rather than assigning them specific grade levels. Additionally, given the higher smoking rates in Chinese men, smoking could have reduced the association between BMI and mortality in Chinese more than in Caucasians. However, we performed a sensitivity analysis among never smokers and the HRs in the analyses of continuous and categorical BMI remained null. Additionally, weight loss due to illness could have distorted the relationship between leanness and health. We performed a second sensitivity analysis excluding cases within the first 3 years of follow-up and the HRs associated with overweight and obesity remained similar as those presented in Table 2. However, after these exclusions the association between BMI 18.5-<23.0 kg/m2 and mortality among Caucasians was more pronounced (HR=1.26, 95% CI: 1.04-1.53, data not shown).
Our study did not indicate that Chinese are at greater relative mortality risk due to overweight or obesity than are Caucasians and, therefore, does not support Asian-specific BMI cutpoints to define the disease of obesity. Thus, we recommend the continued use of the international WHO standard BMI categories across different countries and ethnic groups to facilitate comparisons. Nevertheless, the very different BMI distributions in Chinese compared to Western populations can be used as an argument for the use of ethnic-specific BMI action points for triggering use of resources targeting prevention and treatment of excess weight to lower the population burden of co-morbidities (e.g. diabetes) that tend to increase with increasing BMI without a specific threshold.9
Acknowledgments
The authors thank the staff and participants of the ARIC and the PRC Study for their important contributions.
The Atherosclerosis Risk in Communities (ARIC) Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts [grant numbers HHSN268 201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201 100010C, HHSN268201100011C, and HHSN268201100012C]. The People’s Republic of China (PRC) Study was carried out by the National Heart, Lung, and Blood Institute [grant numbers N01-HV-12243, N01-HV-08112, and N01-HV-59224] with the University of North Carolina, Chapel Hill, North Carolina, and the People’s Republic of China Ministry of Public Health, the Cardiovascular Institute and Fu Wai Hospital, Chinese Academy of Medical Sciences, Beijing, and the Guangdong Provincial Cardiovascular Institute, Guangzhou. This research was also supported in part by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases [grant number R01 DK069678] and this secondary data analysis was supported by a grant from the National Heart, Lung, and Blood Institute [grant number 1 RC1 HL099429Z].
Footnotes
AUTHOR DISCLOSURES
The authors have no conflict of interest to report.
References
- 1.WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 2.Stevens J. Debate: ethnic-specific revisions of body mass index cutoffs to define overweight and obesity in Asians are not warranted. Int J Obes. 2003;27:1297–9. doi: 10.1038/sj.ijo.0802417. [DOI] [PubMed] [Google Scholar]
- 3.Kuczmarski R, Flegal K. Criteria for definition of overweight in transition: background and recommendations for the United States. Am J Clin Nutr. 2000;72:1074–81. doi: 10.1093/ajcn/72.5.1074. [DOI] [PubMed] [Google Scholar]
- 4.Wen CP, Cheng TYD, Tsai SP, Chan HT, Hsu HL, Hsu CC, Eriksen MP. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. 2009;12:497–506. doi: 10.1017/S1368980008002802. [DOI] [PubMed] [Google Scholar]
- 5.Gu D, He J, Duan X, Reynolds K, Wu X, Chen J, Huang G, Chen CS, Whelton PK. Body weight and mortality among men and women in China. JAMA. 2006;295:776–83. doi: 10.1001/jama.295.7.776. [DOI] [PubMed] [Google Scholar]
- 6.Stevens J, Nowicki E. Body mass index and mortality in Asian populations: Implications for obesity cut-points. Nutr Rev. 2003;61:104–7. doi: 10.1301/nr.2003.marr.104-107. [DOI] [PubMed] [Google Scholar]
- 7.International Diabetes Institute. The Asia-Pacific perspective: redefining obesity and its treatment. Geneva: World Health Organization; 2000. pp. 1–55. [Google Scholar]
- 8.Stevens J. BMI cutoffs for obesity should not vary by ethnic group. BMI cutoffs for obesity should not vary by ethnic group. In: Medeiros-Neto G, Halpern A, Bouchard C, editors. Progress in Obesity Research: 9. Montrouge, France: John Libbey Eurotext Ltd; 2003. pp. 554–7. Chap 116. [Google Scholar]
- 9.Stevens J. Commentary: ethnic-specific cutpoints for obesity vs country-specific guidelines for action. Int J Obes. 2003;27:287–8. doi: 10.1038/sj.ijo.0802255. [DOI] [PubMed] [Google Scholar]
- 10.Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364:719–29. doi: 10.1056/NEJMoa1010679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.People’s Republic of China-United States Cardiovascular and Cardiopulmonary Epidemiology Research Group. An epidemiological study of cardiovascular and cardiopulmonary disease risk factors in four populations in the People’s Republic of China. Baseline report from the PRC-USA Collaborative Study. Circulation. 1992;85:1083–96. doi: 10.1161/01.CIR.85.3.1083. [DOI] [PubMed] [Google Scholar]
- 12.Investigators A. The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 13.White A, Folsom A, Chambless L, Sharrett A, Yang K, Conwill D, Higgins M, Williams O, Tyroler H. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study. J Clin Epidemiol. 1996;49:223–33. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 14.Stevens J, Truesdale KP, Wang C, Cai J, Erber E. Body mass index at age 25 and all-cause mortality in whites and african americans: the atherosclerosis risk in communities study. J Adolesc Health. 2012;50:221–7. doi: 10.1016/j.jadohealth.2011.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cox D. Regression models and life tables. J Roy Statist Soc. 1972;34:457–81. [Google Scholar]
- 16.Witte J, Greenland S. A nested approach to evaluating dose-response and trend. Ann Epidemiol. 1997;7:188–93. doi: 10.1016/S1047-2797(96)00159-7. [DOI] [PubMed] [Google Scholar]
- 17.Moon O, Kim N, Jang S, Yoon T, Kim S. The relationship between body mass index and the prevalence of obesity-related diseases based on the 1995 National Health Interview Survey in Korea. Obes Rev. 2002;3:191–6. doi: 10.1046/j.1467-789X.2002.00073.x. [DOI] [PubMed] [Google Scholar]
- 18.Ko G, Tang J, Chan J, Sung R, Wu M, Wai H, Chen R. Lower BMI cut-off value to define obesity in Hong Kong Chinese: an analysis based on body fat assessment by bioelectrical impedance. Br J Nutr. 2001;85:239–42. doi: 10.1079/BJN2000251. [DOI] [PubMed] [Google Scholar]
- 19.Deurenberg P, Yap M, van Staveren W. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes. 1998;22:1164–71. doi: 10.1038/sj.ijo.0800741. [DOI] [PubMed] [Google Scholar]
- 20.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 21.Wang J, Thornton J, Russell M, Burastero S, Heymsfield S, Pierson R. Asians have lower body mass index (BMI) but higher percent body fat that do whites: comparisons of anthropometric measurements. Am J Clin Nutr. 1994;60:23–8. doi: 10.1093/ajcn/60.1.23. [DOI] [PubMed] [Google Scholar]
- 22.Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3:141–6. doi: 10.1046/j.1467-789X.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- 23.Deurenberg P, Ge K, Hautvast JG, Jingzhong W. Body mass index as predictor for body fat: comparison between Chinese and Dutch adult subjects. Asia Pac J Clin Nutr. 1997;6:102–5. [PubMed] [Google Scholar]
- 24.Nechuta SJ, Shu XO, Li HL, Yang G, Xiang YB, Cai H, et al. Combined impact of lifestyle-related factors on total and cause-specific mortality among Chinese women: prospective cohort study. PLoS Med. 2010;7:e1000339. doi: 10.1371/journal.pmed.1000339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 26.Auyeung TW, Lee JS, Leung J, Kwok T, Leung PC, Woo J. Survival in older men may benefit from being slightly overweight and centrally obese - a 5-year follow-up study in 4,000 older adults using DXA. J Gerontol. 2010;65A:99–104. doi: 10.1093/gerona/glp099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schooling CM, Lam TH, Li ZB, Ho SY, Chan WM, Ho KS, Tham MK, Cowling BJ, Leung GM. Obesity, physical activity, and mortality in a prospective Chinese elderly cohort. Arch Intern Med. 2006;166:1498–504. doi: 10.1001/archinte.166.14.1498. [DOI] [PubMed] [Google Scholar]
- 28.Woo J, Ho SC, Sham A. Longitudinal changes in body mass index and body composition over 3 years and relationship to health outcomes in Hong Kong Chinese age 70 and older. J Am Geriatr Soc. 2001;49:737–46. doi: 10.1046/j.1532-5415.2001.49150.x. [DOI] [PubMed] [Google Scholar]
- 29.National Center for Health Statistics. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD: 2012. pp. 1–583. [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. global Health - China. 2013 [cited 2013/06/19]; Available from: http://www.cdc.gov/globalhealth/countries/china/


