Abstract
Hispanics or Latinos constitute the largest racial/ethnic minority in the United States. They are also a very diverse population. Latino/Hispanic’s health varies significantly for subgroups defined by national origin, race, primary language, and migration-related factors (place of birth, immigration status, years of residence in the United States). Most Hispanics speak Spanish at home, and one-third have limited English proficiency (LEP). There is growing awareness on the importance for population health monitoring programs to collect those data elements (Hispanic subgroup, primary language, and migration-related factors) that better capture Hispanics’ diversity, and to provide language assistance (translation of data collection forms, interpreters) to ensure meaningful inclusion of all Latinos/Hispanics in national health monitoring. There are strong ethical and scientific reasons for such expansion of data collection by public health entities. First, expand data elements can help identify otherwise hidden Hispanic subpopulations’ health disparities. This may promote a more just and equitable distribution of health resources to underserved populations. Second, language access is needed to ensure fair and legal treatment of LEP individuals in federally supported data collection activities. Finally, these strategies are likely to improve the quality and representativeness of data needed to monitor and address the health of all Latino/Hispanic populations in the United States.
Keywords: Hispanic health, Latino health, health equity, health disparities, public health ethics, data collection, language access, limited English proficiency
Introduction
The 55.2 million Hispanics or Latinos (the terms “Hispanic,” “Latino,” and “Latino/Hispanic” are used interchangeably in this report) constitute the largest racial/ethnic minority group in the United States (Stepler & Baron, 2016). The U.S Office of Management and Budget (OMB) currently defines “Hispanic or Latino” as U.S. residents of Cuban, Mexican, Puerto Rican, South or Central America, or “other” Spanish culture or origin. Hispanic origin is based on self-identification, and can be viewed as the heritage, nationality group, lineage, or country of birth of the person or the person’s parents or ancestors before arrival in the United States. People who identify their origin as Hispanic or Latino may be any race (Office of Management and Budget [OMB], 1997).
Latinos/Hispanics are among the most culturally, linguistically, and racially diverse populations in the United States. They trace their roots to many ancestral origins, mostly from Latin American and Caribbean countries. The majority are of Mexican origin, followed by Puerto Ricans, Salvadorans, and Cubans. Many consider themselves to be “Afro-descendent” or of “indigenous background” (Krogstad & Lopez, 2016; Lopez & Gonzalez-Barrera, 2016). Nearly three out of four Hispanics speak Spanish at home, while others are monolingual English speakers or speak one of the many indigenous languages from Latin America (Stepler & Baron, 2016).
For decades, adverse economic conditions, political unrest, wars, insecurity, and environmental disasters in Latin American countries have propelled millions to seek a more secure and prosperous life for themselves and their families in the United States. The arrival of immigrants and their U.S.-born children has been a major driver behind Latino population growth and diversity (Pew Research Center, 2015).
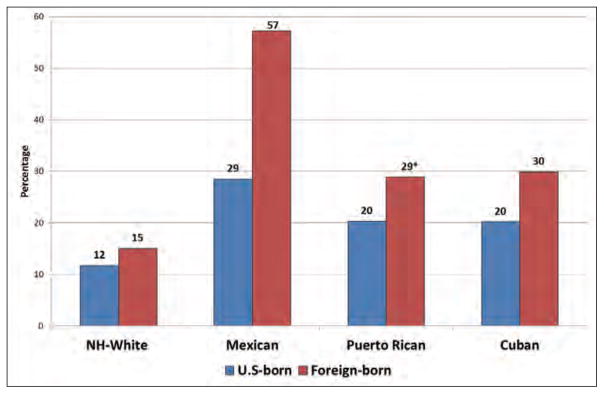
There is strong evidence that determinants of health and health outcomes of Latinos/Hispanics in the United States vary significantly for subgroups defined by national origin, race, primary language, place of birth, and migration-related factors such as years of residence in the United States and immigration status (DHHS, 2014; Dominguez et al., 2015; Singh, Rodríguez-Lainz, & Kogan, 2013; Singh & Lin, 2013). For example, the age-adjusted percentage of adult Hispanics in the United States with multiple chronic conditions (including hypertension, coronary heart disease, diabetes, cancer, or asthma) was lower than among non-Hispanics (20.8% vs. 24.6%); however, the percentage for Hispanics of Puerto Rican origin (27.3%) was higher than for non-Hispanics (Lucas, Freeman, & Adams, 2016). As illustrated in Figure 1, adult Hispanics have overall lower health insurance coverage compared to non-Hispanic Whites, while Mexican foreign-born individuals experience the greatest health insurance disparity (Singh & Lin, 2013). Language and migration-related characteristics of foreign-born parents affect the health and access to healthcare of their children born in the United States (Singh & Lin, 2013; Pastor, Reuben & Duran, 2015).
Figure 1.
Lack of health insurance coverage (%) for adult Non-Hispanic (NH) Whites and selected Hispanic-origin subgroups by place of birth (NHIS 2008–2010)
Reference: Gopal K. Singh and Sue C. Lin. Marked Ethnic, Nativity, and Socioeconomic Disparities in Disability and Health Insurance among US Children and Adults: The 2008–2010 American Community Survey. BioMed Research International Volume 2013, Article ID 627412, 17 pages
*Born in Puerto Rico
Note: Adjusted for age, gender, marital status, education, poverty, and employment
The following examples illustrate the importance of collecting expanded detailed (“granular”) racial and ethnic data, language, and migration-related data in order to identify health needs and disparities among Latino/Hispanic subpopulations. That conclusion is supported by multiple reports by federal agencies, advisory groups, non-governmental organizations, and health researchers that have recommended collecting those data elements in a way that properly represents the increasing racial, cultural and linguistic diversity of the U.S. population in general and Latinos in particular, and can assist with identifying underserved subpopulations.
Such information is considered important for monitoring and eliminating health disparities in the United States (Department of Health and Human Services [DHHS], 2005, 2014; Dominguez et al, 2015; Dorsey et al., 2014; Institute of Medicine [IOM], 2009; National Research Council [NRC], 2004; Richardson, 2016). Title VI of the Civil Rights Act of 1964 (Title VI), which prohibits intentional discrimination of the basis of race, color or national origin in the provision of any services supported by federal funds, provides the legal foundation for the collection of race, ethnicity and primary language (as a proxy for national origin) data (Perot & Youdelman, 2001). Thus the collection of these data elements is also important for monitoring nondiscrimination in the provision of health services (Dorsey et al., 2014; NRC, 2004).
In addition to gathering these expanded data elements, there is another data collection issue especially relevant to Hispanics: language access. Because the majority (73%) of Hispanics speak Spanish at home, and nearly one-third have LEP (Stepler & Baron, 2016), it is important to implement strategies that facilitate Latino participation in data collection activities (DHHS, 2013a). Important ethical and scientific questions include the following: If data collection methods are designed exclusively for English-fluent Hispanics, who is being excluded? Is it ethical to exclude those populations? How does this exclusion affect the representativeness and quality of data collected? In 2000, Presidential Executive Order 13166 directed each federal agency to develop a plan to ensure that the programs and activities they normally provide in English are accessible to LEP persons and thus avoid discrimination on the basis of national origin in violation of title VI of the Civil Rights Act of 1964” (U.S. Department of Justice, 2000). The National Standards for Culturally and Linguistic Appropriate Services (CLAS), which also apply to public health programs, recommend offering language services to individuals with LEP (DHHS, 2013a).
Gathering the needed expanded data elements in a linguistically and culturally appropriate way is critical to: a) ensure fair representation of Latinos/Hispanics’ subpopulations in federal data collection systems; b) monitor health status and identify priority community health problems, including health disparities; c) design and implement linguistically and culturally appropriate public health interventions; d) ensure fair and effective policies and distribution of public health resources and actions; and d) evaluate effectiveness, accessibility, and quality of health services (Dorsey et al., 2014; NRC, 2004; Public Health Functions Steering Committee, 1994).
In this paper the authors provide additional background on the growth and diversity of the Latino/Hispanic population in the United States. The authors then discuss gaps in the availability and quality of national Latino health data. Next the authors propose strategies for consideration by public health programs to expand and enhance Latino health data, based on guidance and recommendations from the U.S. Department of Health and Human Services (DHHS), other organizations and researchers. Both the suggested expanded data elements and provision of language access in data collection are discussed. Finally, the authors provide both scientific and ethical rationales for implementation of the proposed strategies. While this paper focuses on Latinos/Hispanics, this discussion is relevant to all population health data collection implemented or supported by federal agencies, including national population-based surveys, research, public health surveillance, disease registries, and other activities used to assess and monitor the health of the U.S. population.
Latinos/Hispanics in the United States: Growth and Diversity
To better illustrate why and how enhanced data elements and language access are important for Latino/Hispanic health, we provide a review of demographic growth and trends for this population in the United States. The percentage of Latino/Hispanics in the United States has surged over the past decades, from 3.5% to 17.3% of the total U.S. population between 1960 and 2014. In some states, including some non-traditional destinations for Hispanics (i.e., places to which Hispanics have not historically emigrated in large numbers, such as Georgia and Colorado), the Hispanic population growth has been even more accelerated (Turner, Wildsmith, Guzman & Alvira-Hammond, 2016).
Latinos/Hispanics are the youngest major racial or ethnic group in the United States, with a median age of 28 years (19 years for U.S.-born Hispanics), compared to 33 years of age for African-American, 36 years of age for Asians, and 43 years of age for Whites (Stepler & Baron, 2016). Mexicans are by far the largest Hispanic origin group (35.4 million or 64.0% of all Latinos/Hispanics), followed by Puerto Ricans (5.3 million or 9.6%) and Salvadorans (2.1 million or 3.8%). For Latinos/Hispanics, the concepts of race and ethnicity are complex and varied. According to surveys by the Pew Research Center, 26% of adult Latinos/Hispanics in the United States self-identify as Afro-Latino, Afro-Caribbean, or of African descent with roots in Latin America, while only 18% of those report their race as black or African-American. Similarly, 25% say they are of indigenous background, while only 0.9% report their race as American-Indian or Alaska Native, as defined by the U.S. Census Bureau (Krogstad & Lopez, 2016; Lopez G & Gonzalez-Barrera, 2016; Stepler & Baron, 2016).
Most Latinos/Hispanics living in the United States (65%) are U.S.-born. This includes 8.5 million Puerto Ricans, both on the island of Puerto Rico and in the U.S. Puerto Rican diaspora, who are U.S. citizens by birth. Among the 35% of Hispanics who are foreign-born, the majority are from Mexico (60.2%). The percentage of foreign-born varies widely across Hispanic origin groups. For example, 65% of Hondurans and Colombians and 32.9% of Mexicans living in the United States are foreign-born. In terms of immigration status, 76.8% of Hispanics are U.S. citizens (either U.S.-born or naturalized). More than three-quarters of foreign-born Latinos have been living in the United States for more than 10 years (Stepler & Baron, 2016).
Most (73.0%) Hispanics speak Spanish at home, and 25.8% speak only English (Stepler & Baron, 2016). English proficiency varies by Hispanic origin, nativity, education, gender, age, and years residing in the United States, among other factors. For example, 50% or more of Salvadorans, Guatemalans, and Hondurans, respectively, have LEP, compared to 32% of Mexicans and 17% of Puerto Ricans. By nativity, 65.6% of foreign-born Hispanics have LEP vs. 10.6% of U.S.-born Hispanics. A higher percentage of Hispanic adults have LEP compared to children 5 to 17 years old (38.2% vs. 12.4%, respectively). As would be expected, longer residence in the United States is associated with increasing English proficiency among the foreign-born (Stepler & Baron, 2016).
Latinos/Hispanics have the lowest healthcare insurance coverage of any racial/ethnic group in the United States (Smith and Medalla, 2015). The magnitude of this disparity varies by Latino/Hispanic origin, and is primarily driven by very low coverage among the foreign-born (Smith and Medalla, 2015). Latinos/Hispanics also have lower educational attainment and higher rates of living in poverty compared to other racial/ethnic groups (Stepler & Baron, 2016). A high proportion of Latinos report experiencing discrimination because of their race, ethnicity, or assumed immigration status (Ayón, 2015; Krogstad & Lopez, 2016).
Are Latino/Hispanic Health Data Needs Being Met?
This snapshot of Latino/Hispanic demographics demonstrates Latinos’ growing significance as a share of the total U.S.-population, as well as a major driver in the United States’ sociodemographic diversity. As a consequence, Latino/Hispanic health is highly relevant to the overall future health of the nation. Thus it is important to ensure that data collected and reported by national data systems is of quality and representative of diverse Hispanic subpopulations.
Limitations in the inclusiveness, specificity, availability, and quality of Latino/Hispanic health data, has been widely noted in various landmark reports and studies (DHHS 2005, 2014; Dominguez et al., 2015; Dorsey et al., 2014; IOM, 2009; NRC, 2004). Reported data gaps for Latino/Hispanic health include:
Lack of collection, analysis, and/or reporting of ethnicity, primary language, place of birth, length of time in the United States and immigration status in public health information systems (Beltran et al., 2011; DHHS, 2005; Dominguez et al., 2015; Dorsey et al., 2014; IOM, 2009; Johnson, Blewett, & Davern, 2010; NRC, 2004).
Lack of collection detailed Hispanic subgroup information. By grouping diverse Latino/Hispanic subpopulations together for statistical and programmatic purposes into a broad and single “Hispanic” ethnic category, important differences in risk factors and health disparities affecting those subpopulations are likely to be missed, and thus remain unaddressed (DHHS, 2005, 2014; Singh, Rodríguez-Lainz, & Kogan, 2013)
Even when data elements are included in data collection instruments, the elements may not actually be collected. This problem can be widespread, such as in the National Notifiable Disease Surveillance System, in which more than half of reported cases lack ethnicity information (Adekoya, Truman, & Ajani, 2015).
Questionable validity of information due to limited translation and lack of cultural validation of data collection instruments and/or availability of qualified Spanish-English interpreters to facilitate communication with people with LEP (Landrine & Corral, 2014; Li et al., 2001).
Lack of representation due to non-inclusion or small/inadequate sample sizes of Latino/Hispanic subpopulations. Many national Latino/Hispanic health statistics are likely driven by the health of Mexicans, given their overrepresentation among Hispanics (Logan & Turner, 2013).
Given these gaps, it is no surprise that for many health issues, the United States currently has an incomplete picture of the health of Latino/Hispanic subpopulations, their burden of disease, and their risk factors. The reasons for these limitations and gaps in Latino/Hispanic health data can be multiple. One challenge is the complexity of the concepts of race and ethnicity and the categories used to collect them, which may be confusing or even considered inappropriate by respondents (OMB, 2016). Federal initiatives are underway to improve the collection and acceptability of racial and ethnic information by federal programs, including the U.S. Census Bureau (OMB, 2016).
In addition, multiple regulation, statutes, policies and practices influence what data are collected; these vary across federal agencies and over time (Perot & Youdelman, 2016). For many federal programs there is no requirement to collect race, ethnicity, language or migration-related data (Perot & Youdelman, 2016). Missing information may be due to questions not being asked or responders refusing to provide personal information (Perot & Youdelman, 2001).
Uniformity and comparability of federal statistics depends on the existence of standards for collection and on those being properly implemented. The Office of Management and Budget (OMB) has developed standards for collecting and presenting data on race and ethnicity (OMB, 1997). Currently there are no federal standards for language or migration-related data (Perot & Youdelman, 2016). The current (1997) OMB data standards require federal agencies to use a minimum of two ethnic categories when collecting and reporting population information: “Hispanic or Latino” and “Not Hispanic or Latino” (OMB, 1997). The OMB directive permits, and encourages, the collection of more detailed racial and ethnic categories, provided they can be aggregated to the minimum standard categories (OMB, 1997). However, according to OMB, the minimum reporting categories have often been misinterpreted as the only permissible ones (OMB 2016). That might partly explain the limited availability of detailed racial and ethnic data in federal statistics. In 2011, DHHS published new data standards that included more detailed racial and ethnic categories (beyond OMB 1997 minimum standards) and also (for the first time), the requirement to collect primary language. However, DHHS data standards apply only to federally-supported population-based surveys and have not been fully implemented (DHHS, 2011).
Data Needed to Capture Hispanic or Latino Population’s Diversity
As indicated earlier, there has been growing awareness among federal agencies, advisory groups and health researchers, about the importance of collecting standardized data elements that would allow better assessment of health disparities within racial and ethnic minority subgroups and other underserved communities, and evaluate efforts addressing them (DHHS, 2005, 2014; Dominguez et al., 2015; Dorsey et al., 2014; IOM, 2009; NRC, 2004; Wildsmith, Ansari & Guzman, 2015; Richardson, 2016)
The two data elements for which there is greater consensus in terms of their priority for data collection are more “granular” (that is, detailed) racial and ethnic origin subcategories and primary language (Beltran et al., 2011; Blendon et al., 2007; Dean et al., 2016; DHHS, 2005, 2014; Dominguez et al., 2015; Dorsey & Graham, 2011; Islam et al., 2010; Institute of Medicine, 2009; National Committee on Vital and Health Statistics [NCVHS], 1968; NRC, 2004; Penman-Aguilar et al., 2016; Holland & Palaniappan, 2012).
These two data elements are also included in the DHHS’s 2011 Data Standards (DHHS, 2011). Although HHS data standards reportedly only apply to federally supported population-based surveys (DHHS, 2011), the Affordable Care Act (ACA) legislation on which the standards are based actually relates to “any federally conducted or supported healthcare or public health program, activity, or survey” “to the extent practicable” (Patient Protection and Affordable Care Act, 2010; Dorsey & Graham, 2011),). The rationale for including expanded data elements in population surveys has relevance for many other public health data sources used to monitor the health of the U.S. population, such as surveillance systems, disease registries, and vital statistics.
Detailed Hispanic subgroup information is important to document disparities in health determinants and outcomes between and among Latino/Hispanic subpopulations (Dominguez et al, 2015; Islam et al, 2010; Logan & Turne, 2013; Lucas et al 2016; Singh & Lin, 2013). Primary language data is needed, first and foremost, to prioritize languages for which translation and interpretation are needed for rigorous data collection and provision of public health services, activities that are highly dependent on effective communication (DHHS, 2005; IOM, 2009; NRC, 2004). Primary language also serves as a proxy for acculturation, which has been shown to affect health status and which many view as essential for identifying appropriate approaches to providing health services (NRC, 2004).
The importance of collecting migration-related data by public health data systems has been recognized for decades (NCVHS, 1968). In a globalized world, migration is a social determinant of health, which affects access to care and disease risk of migrants and their families (Gushulak, Weekers & MacPherson, 2009). In more recent years, the body of scientific evidence has grown about the diverse effects of migration-related factors (e.g., place of birth, years of U.S. residence, and citizenship) on the health of Latinos/Hispanics and other racial/ethnic minorities (Beltran et al., 2011; Blendon et al., 2007; DHHS, 2005, 2014; Dominguez et al., 2015; IOM, 2009; Islam et al., 2010; Koch-Weser et al., 2004; NRC, 2004; Singh, Rodríguez-Lainz, & Kogan, 2013). For example, compared to U.S.-born Hispanics, Hispanics born in Puerto Rico and Latin America experience greater inequities in access to care, and are at higher risk of some conditions and diseases, including neglected infections (Colson et al., 2014; Hotez, 2008; Kimbro, Gorman, & Schachter, 2012; Lu et al., 2014; Steege et al., 2014;), while at lower risk for other conditions, such as breast and lung cancer (Singh, Rodríguez-Lainz & Kogan, 2013).
For Hispanics, the above-noted expanded data element recommendations point to the importance for federally-supported programs of collecting the following information in a standardized manner (DHHS, 2005, 2014; Dominguez et al, 2015; IOM, 2009; NRC, 2004; Richardson, 2016; NCVHS, 1968; Wildsmith, Ansari & Guzman, 2015):
Detailed Hispanic origin subgroup. The HHS data standards include the following subgroups: Mexican, Puerto Rican, Cuban and Other Hispanic (DHHS, 2011). Collection of additional Latino subgroups has been recommended (Wildsmith, Ansari & Guzman, 2015). Noting self-identification as Afro-Latino (increasingly referred to as Afro-descendent) or indigenous is also important.
Primary language. The 2011 HHS data standards include questions on English-speaking proficiency and language spoken at home (DHHS, 2011).
-
Migration-related factors. This includes Place of birth (to include the U.S. Island Territories and the specific country of birth for those born outside the United States). Other important migration-related data elements are the length of time a person has been living in the United States and immigration status (e.g., citizenship). The U.S. Census Bureau has validated questions to collect that information (U.S. Census Bureau, 2016)
(Note: For child-related data collection, all the above variables should be collected about parents (Wildsmith, Ansari & Guzman, 2015).
In addition to the collection of expanded standard data elements and provision of language access, it is also important that culturally and scientifically appropriate data collection methodologies be used with Hispanic populations. Sampling and recruitment methods and modes of interviewing need to be appropriate to specific Latino/Hispanic subpopulations. For example, oversampling geographic areas of concentration for specific subpopulations and engaging community-based organizations or leaders to gain trust of community members (Brown, 2015). In addition, appropriate sample sizes in surveys would ensure statistical reliability of estimates for Latino/Hispanic subpopulations. Finally, targeted studies of smaller or harder-to-reach Latino/Hispanic sub-populations (e.g., farmworkers, recent immigrants, non-Spanish speaking indigenous population) could increase the likelihood of these groups being properly represented in national data sets (DHHS, 2005; NRC, 2004).
“No entiendo” (“I don’t understand”): Provision of Language Access for Data Collection
The question of language access in data collection also looms large among data challenges impacting Latino/Hispanics’ health. If data collection instruments (printed or electronic forms) are not available in Spanish and/or Spanish-speaking interpreters are not available during data collection, a high proportion of Hispanics could be essentially excluded from the data collection activity. This issue not only affects many Latinos, but also others among the 25.3 million (9%) of the U.S. population who are LEP. (Of note, this statistic reflects an 81% increase between 1990 and 2011 (Whatley & Batalova, 2013). Populations with LEP frequently include disproportionately high numbers of vulnerable individuals, such as those living in poverty, the less educated, and the elderly (Li et al., 2001).
Ongoing federal efforts have been carried out to improve the cultural and linguistic appropriateness of healthcare services and public health programs, including the publication of national standards and DHHS’s Language Access Plan (DHHS, 2013a, 2013b). According to DHHS’s 2011 Language Access Plan, language access is achieved when individuals with limited English proficiency (LEP) (i.e., speak English less than “very well”) can communicate effectively with HHS employees and contractors and participate in HHS programs and activities (DHHS, 2013b). The DHHS Plan includes two “essential elements” of language access: a) providing oral language assistance services, such as qualified interpreters; and b) translating and making accessible “vital documents” in languages other than English (DHHS, 2013b). DHHS’s Language Access Plan states DHHS agencies must provide oral and written language services needed to assist individuals with LEP to communicate effectively with DHHS staff and contractors and gain meaningful access and an equal opportunity to participate in the services, activities, programs, or other benefits administered by DHHS. (DHHS, 2013b). In addition, HHS has strongly recommended that, among other recommendations related to cultural and linguistic appropriate services, all members of the health and healthcare community, including public health personnel, use cultural and linguistically competent personnel to collect health information from individuals (DHHS, 2013a).
Information about provision of language access by public health data systems is incomplete. It has been reported that a number of national population health surveys translate their questionnaires into Spanish and provide access to bilingual English-Spanish interviewers (Waksberg, Levine & Marker, 2000). In spite of existing federal and state language access laws specific to healthcare settings, gaps in availability and quality of language services have been reported due to lack of comprehensive implementation and enforcement (Youdelman, 2008).
Provision of language access by federal data collection systems is particularly relevant in three instances: 1) for racial/ethnic minorities with a high proportion of individuals with LEP (for example, 50% or more of Salvadorans, Guatemalans, and Hondurans are LEP); 2) geographic areas where individuals with LEP are a high proportion of the population (e.g., 19% of California’s population are LEP); and 3) for health issues and conditions for which people with LEP experience disparities (e.g., occupational health, infectious and parasitic diseases, access to health services) and/or have different risk factors compared to English-speaking individuals (Holland & Palaniappan, 2012; Hunt & Bhopal, 2004; Koch-Weser et al., 2004; Lee, Nyguyen, Jawad & Kurata, 2008; Link, Mokdad, Stackhouse & Flowers, 2006).
A number of strategies have been recommended to enhance provision of language access for data collection. These include:
Translation of data collection instruments into the main languages spoken by individuals with LEP in the target population. Translation and back translation are the minimum recommended strategies; it is also important to ensure equivalence of meaning across languages by approaches such as cognitive testing, focus groups, and/or piloting with the target monolingual Spanish-speaking population (DHHS, 2005; Fukijshiro et al., 2010; Hunt & Bhopal, 2004; Landrine & Corral, 2014; Li et al., 2001).
Cross-cultural validation of data collection instruments. Questions included on data collection forms need to be conceptually and functionally equivalent for all participants, independent of their culture, preferred language, and English-speaking ability. Even when instruments are translated, measurement errors may still occur because of differences in the use and interpretation of specific terms, culturally based attitudes and beliefs about health issues (such as mental or physical well-being), inappropriate or unclear response categories, the order and context in which the items are presented, and/or differences in perceived social desirability of certain answers (DHHS 2013a; Hunt & Bhopal, 2004; Li et al., 2001; Westat 2007).
Use of trained interviewers and/or third-party (e.g., by phone) interpreters who are fluent in the most frequently used languages spoken by individuals with LEP in the target population. The use of community or agency staff that speak a variety of languages but are not trained interpreters should be considered with caution because of the difficulty in ensuring the quality of the interpretation. Although the use of English-speaking household members or community members as interpreters may improve participation by individuals with LEP; their use may also be a barrier to data collection because participants may be reluctant to share information about confidential or culturally sensitive topics with someone from their community (Hu, Link, & Mokdad, 2010; Hunt & Bhopal, 2004; Li et al., 2001; Link et al., 2006).
Although cost is frequently mentioned as the most significant barrier to including individuals with LEP in data collection activities, an increasing number of innovative approaches and technologies exist that can decrease such cost. For example, the rapidly expanding realm of machine translation technology can allow professional translators to focus on refining a translation, thus reducing the time required to complete a translation. Another approach worth exploring is the use or adaptation of relevant questionnaires validated by other organizations (Li et al., 2001).
Ethical and Scientific Implications of Public Health Data Collection Practices
Alongside poor language access practices, the potential negative results of current data element identification and collection practices have a number of ethical and scientific and technical implications.
A. Ethical implications: Doing “what is right”
Public health ethics is an emerging discipline that has expanded upon the related fields of clinical ethics, research ethics, and bioethics (Beauchamp & Childress, 2012; Coughlin, 2009; Ortmann et al., 2016). The discipline is also informed by public health professionals’ codes of conduct (e.g., American Public Health Association and American College of Epidemiology) and by public health core values and beliefs regarding the role of health, science, and community (American College of Epidemiology, 2000; Lee, Heilig, & White, 2012; Public Health Leadership Society, 2002).
Because of the population focus of public health, ethical considerations for public health practice include broader social and political considerations than those raised in traditional clinical or biomedical ethical questions. Thus, the field of public health ethics brings a fundamental consideration of social justice and a focus on achieving health equity. The “dream of social justice” requires that ethics be applied to all aspects of public health practice and services, including data collection. Consideration of the ethical aspects of public data collection have mainly focused on protecting privacy and confidentiality and on data use issues (Coughlin, 2006; Lee, Heilig, & White, 2012). Broader issues of data element identification and data collection have also become part of the current discourse on health equity (Beltran et al., 2011; Blendon et al., 2007; Braveman et al., 2006; Dean et al., 2016; Penman-Aguilar et al., 2016).
When exploring ethical considerations for the expansion of data elements to better meet Hispanic or Latino health needs, it is useful to consider the four basic bioethical principles (also referred to as the Belmont Principles) (Beauchamp & Childress, 2012): justice, beneficence, non-maleficence, and respect for persons, while also applying the lens of what is unique about public health ethics, (i.e., a focus on prevention and addressing the root causes of disease, achieving community or population benefit, the interdependence of people, and striving for social justice and solidarity (Ortmann et al., 2016).
-
Justice: this principle is about ensuring that social burdens and benefits are distributed fairly across populations (Heilig & Sweeney, 2010). In public health, it implies ensuring that conditions for health are available to all, especially those who are vulnerable and disenfranchised (Lee, Heilig, & White, 2012). It also means that public health actions and services should not discriminate against individuals on the basis of their race, ethnicity, nationality, religious beliefs, sex, sexual orientation, or disability (Heilig & Sweeney, 2010).
For public health data collection, first and foremost, the principle of justice supports and echoes the importance of making all Latinos/Hispanics — and subpopulations — count in all public health data collection efforts. This is related to the concept of “equity in data capture across populations” (Heilig & Sweeney, 2010). In other words, no population (Hispanic or other population group) should be systematically and unfairly excluded from participating in a federally supported data collection activity. If there is a valid exception in which populations are knowingly excluded, we suggest that, from ethical and scientific perspectives, the onus is on the data collector to provide a valid rationale for why their data collection effort is an exception. Ensuring equity in data capture would also help fulfill the requirement for federal agencies to ensure non-discrimination on the basis of race, color, or national origin (Dorsey et al., 2014). Given that primary language is a proxy for national origin, it implies that federal data systems need effective strategies to allow individuals with LEP opportunities equal to English speakers to participate and benefit from data collection activities. Li et al (2001) have argued that equal access to federally sponsored programs (which would include national public health monitoring data systems) is a “basic civil right regardless of whether or not an individual is a fluent English speaker”.
The application of the justice principle has led to the collection and analysis of information on social determinants of health (including structural factors) and calls to identify and eliminate health disparities by addressing those determinants (Heilig & Sweeney, 2010). In public health, it is also critical to collect data to support just and equitable distribution of care and prevention resources (Lee, Heilig, & White, 2012). Failure to properly reflect Latino/Hispanic subpopulations experiencing disparities in data collection efforts is counter to, and even fails, this principle.
An ethical and social justice based approach to data collection takes pains to create and maintain community trust, ensures informed and empowered community participation, and ensures that all information collected is used to benefit affected communities (Helig & Sweeney, 2010). Timely engagement of the target communities is important prior to acquiring or disseminating data, especially when the data are sensitive or populations are particularly vulnerable (Lee, Heilig, & White, 2012). This, in turn, might help to improve the actual data collection system and increase the likelihood of the community acting on the findings (Heilig & Sweeney, 2010).
-
Beneficence (doing good) and non-maleficence (doing no harm): These two complementary principles direct us to strive to maximize possible benefits and minimize possible harms of any action (Heilig & Sweeney, 2010; Beauchamp & Childress, 2012). Beneficence implies the duty to promote health by collecting, analyzing, and using data to inform and prioritize public health interventions (Heilig & Sweeney, 2010). There is also an obligation by those collecting public health information from a community to share their findings in a timely fashion, utilizing culturally and linguistically appropriate methods so that community will benefit from their participation (Heilig & Sweeney, 2010).
In particular, the collection and reporting of granular race, ethnicity, and primary language “on all public health data sets” is considered an essential component to achieving health equity (Richardson, 2016). If Latino/Hispanic subpopulations are not identified by the data system, their particular health issues are more likely to be unrecognized and, thus, ignored. Another aspect of beneficence in data collection is making language access a standard rather than an exception. Doing so will increase the inclusion of Hispanics and make it possible for health needs and perspectives to be reflected in programs, research, and surveillance. The opposite — exclusion — is a denial of the principle of non-maleficence, or doing no harm.
Both lack of collection of data elements needed to identify Latino/Hispanic subgroups experiencing disparities and language exclusion practices can produce biased information which may cause harm, including implementation of ineffective public health interventions and misallocation of funds to the most “visible” (not necessarily most underserved) subgroups, and, ultimately, failure to prevent/control disease and reduce health disparities (Lee, Heilig, & White, 2012). Even if the appropriate data collection procedures are implemented, if data are not analyzed and reported disaggregated by Latino/Hispanic subgroups, those populations essentially remain invisible. Latino/Hispanics in the United States include many vulnerable groups, with limited social capital, including individuals with LEP, victims of human trafficking, asylum seekers, indigenous persons, migrant workers, and unauthorized immigrants (Truman et al., 2009). Because of the ethical obligation to use (i.e., act on) information collected to benefit overburdened and underserved communities and to reduce health inequities (Lee, Heilig, & White, 2012), collecting data on Latino/Hispanic subgroups will contribute to public health efforts to protect and improve the health of the most vulnerable.
Some potential harms for participants in public health data collection activities include the time burden of completing interviews and, in some circumstances, the anxiety or grief caused by sharing painful or sensitive personal information (Coughlin, 2009). Another potential harm is the stigmatization of communities by disseminating health findings that may reinforce negative social and cultural stereotypes. As a consequence, community members may experience discrimination in employment or housing, may have their access to healthcare and other public benefits limited, or have their immigration status jeopardized. Similar harms can result from breaches in confidentiality (Coughlin, 2009). The risk of community stigmatization can be reduced by emphasizing relevant structural and social determinants for the identified health disparity and highlighting strategies to address the disparity and improve the health of the community and general population. The risk of stigmatization must always be weighed against the communities’ need for information, regardless of whether the findings are troubling, so that they can mobilize to protect their own health, as well as the potential benefit of additional targeted resources to address health disparities (Heilig & Sweeney, 2010; Lee, Heilig, & White, 2012). To mitigate potential harms, the affected community should be consulted about the best communication messages and ways to disseminate the information (vs. traditional mass media messages) (Lee, Heilig, & White, 2012). Other potential harms of data collection can also be reduced by collecting individual identifiers only when absolutely necessary for public health purposes, by acquiring the minimal amount of information needed, and by developing policies and procedures that ensure appropriate access to and use of the data and protection of participants from the risk of disclosure of information (Heilig and Sweeney, 2010).
Respect for persons is the obligation to treat individuals as autonomous agents who have the ability to make their own decisions and to act on these decisions free from interference or coercion (Beauchamp& Childress, 2012). The principle of respect for persons is the underlying concept for obtaining informed consent, and it accords special protections for persons with diminished autonomy (Beauchamp& Childress, 2012; Heilig & Sweeney, 2010). In public health practice, this principle often must be weighed against the need to protect the common good (e.g., use of interventions which may limit personal autonomy, such as quarantine and isolation, when needed to control the spread of infectious diseases). For data collection, a core application of this ethical principle is the requirement to seek free and informed consent by prospective subjects for public health research (Heilig & Sweeney, 2010). Other public health data collection activities (e.g., public health surveillance) by necessity sometimes involve the collection of individual-level, identifiable data without explicit patient consent; this is justified by the obligation of public health to protect population health and prevent harm (Heilig & Sweeney, 2010; Lee, Heilig, & White, 2012). Still, those data elements must represent the minimal necessary information needed to achieve effective public health actions, and the data must be maintained securely and confidentially (Lee, Heilig, & White, 2012).
B. Scientific and technical implications: collecting valid and representative data
Besides these ethical considerations, failure to collect the data elements needed to properly monitor and investigate Latino/Hispanic subpopulations’ health, and to provide language access have a range of scientific and technical implications that may negatively impact the quality and usefulness of the data collected. As described earlier, lack of collection of granular ethnic and language data may hide emerging health issues and health disparities affecting Latino/Hispanic subpopulations. This may result in less-effective public health interventions and use of resources.
Failure to provide language access can potentially exclude a high percentage of the target population for a data system. Such practices can effectively make whole populations invisible and distort evidence. For example, English-only data systems could exclude the more than 32% of Hispanics that have LEP and half of all Salvadorans, Guatemalans, and Hondurans. The percentage excluded could be even larger if the target populations are adults and include a high proportion of foreign-born individuals (Landrine & Corral, 2014). Participants in English-only systems are also more likely to be U.S.-born, more acculturated, better educated, with a higher income, and better access to healthcare. This can potentially result in the introduction of additional biases in the findings (Hunt & Bhopal, 2004; Koch-Weser et al., 2004; Landrine & Corral, 2014; Lee et al., 2008; Li et al., 2001). Unbiased data collection that is complete enough to answer the public health questions of the day is a hallmark of good stewardship of public health resources.
If language access is not provided, the data system and related public health program may be less acceptable for a community with a high number of individuals with LEP if they feel excluded from participating (CDC, 2001). That may result in lower response rates, which, in turn, can cast great doubt on the representativeness of the data (Koch-Weser et al., 2004; Ladrine & Corral, 2014; Li et al., 2001).
Quality of the data can also be influenced by lack of translation of data collection forms and unavailability of qualified interpreters. If a respondent with LEP does not understand the questions being asked, and/or the person collecting the data misinterprets the participants’ responses, the validity and completeness of the information are likely to suffer (Li et al., 2001; Pastor, Reuben, & Duran, 2015; Pearson, Garvin, Ford, & Balluz, 2010). Thus, language access in data systems and programs will likely result in better data down the road.
Conclusion - Moving Forward
Data collection practices that have not adapted to the increased ethnic, cultural, and linguistic diversity of the United States, and objectively exclude language minorities from data collection activities, currently contribute to the near invisibility of tens of millions of persons residing in the United States, particularly many Hispanic or Latino persons. This invisibility, and the concomitant potential exclusion from public health priorities, amounts to injustice that highlights the importance of ensuring equity in data collection. The above-described challenges to the quality and representativeness of data collected by national public health monitoring systems can be expected to increase in the future as the size and share of Hispanic origin subgroups and language minority populations increase in the United States (Li et al., 2001).
A consensus on the need for collection of additional standardized data elements on Hispanic or Latino health needs, as well as improved practices to ensure language access in data collection is growing. A number of valuable tools exist to promote sound and inclusive Latino/Hispanic health-related data practices. Some of these include established national guidelines and recommendations discussed earlier. These recommendations are often feasible and achievable, as demonstrated by the data systems that have implemented most or some of those practices. For example, the National Notifiable Disease Surveillance System (NNDSS) in 2014 and Arbonet in 2016 (for Zika case reporting) added country of birth to their report forms (CDC, 2016a). In 2016, the CDC Listeria Initiative added detailed race and ethnicity, country of birth, and language, and their questionnaire is available in Spanish (CDC, 2016b). The National Immunization Survey (Child)’s questionnaire is available in Spanish and the program provides bilingual staff interviewers and use of Language Line Services for interpretation in multiple languages (U.S. National Center for Health Statistics, 2007). The 2016 questionnaire collects granular race and ethnicity information for the child and parent and the child’s country of birth (U.S. National Center for Health Statistics, 2016).
In the authors’ view, and based on the literature discussed in this paper, expansion of data element selection and collection could improve the quality and representativeness of data needed to monitor and address the health of all Latino/Hispanic subpopulations. Expanding and strengthening data collection for Latino/Hispanic health is firmly based on ethical and social justice principles. This paper has provided both ethical and scientific arguments to support those contentions. Data collection improvements are a prerequisite for identifying and addressing racial/ethnic health disparities, promoting health equity, and improving the health of an increasingly diverse nation. In this article, the authors have focused on Latino/Hispanic health, but the same arguments apply to other racial and ethnic populations which have to date been typically characterized as monolithic, such as Asian Americans.
Although implementation of these recommendations may imply the need for additional personnel and/or financial resources, the authors believe that cost alone never justifies inaction. Implementing, as resources allow, the appropriate expanded data collection practices required by the reality of 21st century U.S. population diversity is sound public health practice. The authors hope this paper will contribute to the dialogue regarding how to confront data collection challenges and address health inequities and inspire action, bringing closer the time when no Hispanic or Latino community in the United States will be “invisible” and instead all will be routinely and robustly counted and included in the nation’s public health data and intervention initiatives.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Adekoya N, Truman BI, Ajani UA. Completeness of reporting of race and ethnicity data in the nationally notifiable diseases surveillance system, United States, 2006–2010. J Public Health Manag Pract. 2015;21(2):E16–22. doi: 10.1097/PHH.0000000000000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of Epidemiology. American College of Epidemiology Ethics Guidelines. 2000 doi: 10.1016/s1047-2797(00)90000-0. Retrieved August 9, 2016, from http://acepidemiology.org/sites/default/files/EthicsGuide.pdf. [DOI] [PubMed]
- Ayón C. Economic, Social and Health Effects of Discrimination on Latino Immigrant Families. Washington, DC: Migration Policy Institute; 2015. Retrieved August 9, 2016, from http://www.migrationpolicy.org/research/economic-social-and-health-effects-discrimination-latino-immigrant-families. [Google Scholar]
- Beauchamp BE, Childress JF. Principles of Biomedical Ethics. 7. New York: Oxford University Press; 2012. [Google Scholar]
- Beltran VM, Harrison KM, Hall HI, Dean HD. Collection of social determinant of health measures in U.S. national surveillance systems for HIV, viral hepatitis, STDs, and TB. Public Health Rep. 2011;126(Suppl 3):41–53. doi: 10.1177/00333549111260S309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blendon RJ, Buhr T, Cassidy EF, Pérez DJ, Hunt KA, Fleischfresser C, … Herrmann MJ. Disparities In Health: Perspectives Of A Multi-Ethnic, Multi-Racial America. Health Aff. 2007;5(26):1437–1447. doi: 10.1377/hlthaff.26.5.1437. [DOI] [PubMed] [Google Scholar]
- Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–194. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- Brown A. The Unique Challenges of Surveying U.S. Latinos. Washington, D.C: Pew Research Center, November; 2015. Retrieved August 9, 2016, from http://www.pewresearch.org/2015/11/12/the-unique-challenges-of-surveying-u-s-latinos/ [Google Scholar]
- Colson PW, Couzens GL, Royce RA, Kline T, Chavez-Lindell T, Welbel S Tuberculosis Epidemiologic Studies Consortium. Examining the impact of patient characteristics and symptomatology on knowledge, attitudes, and beliefs among foreign-born tuberculosis cases in the US and Canada. J Immigr Minor Health. 2014;16(1):125–135. doi: 10.1007/s10903-013-9787-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coughlin SS. Ethical issues in epidemiologic research and public health practice. Emerg Themes Epidemiol. 2006;3:3–16. doi: 10.1186/1742-7622-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coughlin SS. Am J Public Health. 2. Washington, DC: American Public Health Association; 2009. Ethics in epidemiology and public health practice: Collected works. [Google Scholar]
- Dean HD, Roberts GW, Bouye KE, Green Y, McDonald M. Sustaining a Focus on Health Equity at the Centers for Disease Control and Prevention Through Organizational Structures and Functions. J Public Health Manag Pract. 2016;22(Suppl 1):S60–7. doi: 10.1097/PHH.0000000000000305. [DOI] [PubMed] [Google Scholar]
- Dominguez K, Penman-Aguilar A, Chang MH, Moonesinghe R, Castellanos T, Rodríguez-Lainz A, Schieber R. Vital Signs: Leading Causes of Death, Prevalence of Diseases and Risk Factors, and Use of Health Services Among Hispanics in the United States-2009–2013. MMWR Morb Mortal Wkly Rep. 2015;64:469–478. [PMC free article] [PubMed] [Google Scholar]
- Dorsey R, Graham G. New HHS Data Standards for Race, Ethnicity, Sex, Primary Language, and Disability Status. JAMA. 2011;306(21):2378–2379. doi: 10.1001/jama.2011.1789. [DOI] [PubMed] [Google Scholar]
- Dorsey R, Graham G, Glied S, Meyers D, Clancy C, Koh H. Implementing health reform: improved data collection and the monitoring of health disparities. Annu Rev Public Health. 2014;35:123–138. doi: 10.1146/annurev-publhealth-032013-182423. [DOI] [PubMed] [Google Scholar]
- Fujishiro K, Gong F, Baron S, Jacobson CJ, Jr, DeLaney S, Flynn M, Eggerth DE. Translating questionnaire items for a multi-lingual worker population: the iterative process of translation and cognitive interviews with English-, Spanish-, and Chinese-speaking workers. 2010:194–203. doi: 10.1002/ajim.20733. Retrieved August 10, 2016, from http://onlinelibrary.wiley.com/doi/10.1002/ajim.20733/abstract;jsessionid=667C70462FAD41B655F5FCAE6DD7FE2E.f01t04. [DOI] [PubMed]
- Gushulak BD, Weekers J, MacPherson DW. Migrants and emerging public health issues in a globalized world: threats, risks and challenges, an evidence-based framework. Emerg Health Threats J. 2009;2:e10. doi: 10.3134/ehtj.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heilig CM, Sweeney P. Ethics in Public Health Surveillance. In: Lee LM, Teutsch SM, Thacker SB, St Louis ME, editors. Principles and Practice of Public Health Surveillance. 3. New York: Oxford University Press; 2010. pp. 198–216. [Google Scholar]
- Holland AT, Palaniappan LP. Problems with the collection and interpretation of Asian-American health data: omission, aggregation, and extrapolation. Ann Epidemiol. 2012;22(6):397–405. doi: 10.1016/j.annepidem.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotetz PJ. Neglected Infections of Poverty in the United States of America. PLOS Neglected Tropical Diseases. 2008 doi: 10.1371/journal.pntd.0000256. http://dx.doi.org/10.1371/journal.pntd.0000256. [DOI] [PMC free article] [PubMed]
- Hu SS, Link MW, Mokdad AH. Reaching Linguistically Isolated People: Findings from a Telephone Survey Using Real-time Interpreters. Field Methods. 2010;22(1):39–56. [Google Scholar]
- Hunt SM, Bhopal R. Self-report in clinical and epidemiological studies with non-English speakers: the challenge of language and culture. J Epidemiol Community Health. 2004;58(7):618–622. doi: 10.1136/jech.2003.010074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC: The National Academies Press; 2009. Retrieved August 10, 2016, from https://www.nap.edu/read/12696/chapter/1. [PubMed] [Google Scholar]
- Islam NS, Khan S, Kwon S, Jang D, Ro M, Trinh-Shevrin C. Methodological issues in the collection, analysis, and reporting of granular data in Asian American populations: historical challenges and potential solutions. J Health Care Poor Underserved. 2010;21:1354–1381. doi: 10.1353/hpu.2010.0939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson PJ, Blewett LA, Davern M. Disparities in public use data availability for race, ethnic, and immigrant groups: national surveys for healthcare disparities research. Med Care. 2010;48(12):122–1127. doi: 10.1097/MLR.0b013e3181ef984e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbro RT, Gorman BK, Schachter A. Acculturation and Self-Rated Health among Latino and Asian Immigrants to the United States. Social Problems. 2012;59(3):341–363. [Google Scholar]
- Koch-Weser S, Grigg-Saito D, Liang S, Toof R, Kreth NN, Pot M, … Giles W. Health Status of Cambodians and Vietnamese - Selected Communities, United States, 2001–2002. MMWR Morb Mortal Wkly Rep. 2004;53(33):760–765. [PMC free article] [PubMed] [Google Scholar]
- Krogstad JM, Lopez J. Roughly half of Hispanics have experienced discrimination. Pew Research Center; Jun 26, 2016. Retrieved August 10, 2016, from http://www.pewresearch.org/fact-tank/2016/06/29/roughly-half-of-hispanics-have-experienced-discrimination/ [Google Scholar]
- Landrine H, Corral I. Advancing research on racial–ethnic health disparities: improving measurement equivalence in studies with diverse samples. Front Public Health. 2014;2:82. doi: 10.3389/fpubh.2014.00282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee LM, Heilig CM, White A. Ethical justification for conducting public health surveillance without patient consent. Am J Public Health. 2012;102(1):38–44. doi: 10.2105/AJPH.2011.300297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Nguyen HA, Jawad M, Kurata J. Linguistic Minorities and Nonresponse Error. Public Opin Q. 2008;72(3):470–486. [Google Scholar]
- Li RM, McCardle P, Clark RL, Kinsella K, Berch D, editors. Diverse Voices—Inclusion of Language-Minority Populations in National Studies: Challenges and Opportunities. National Institute on Aging and National Institute of Child Health and Human Development; Bethesda, MD: 2001. Retrieved August 10, 2016, from https://www.nichd.nih.gov/publications/pubs/documents/Diverse_Voices.pdf. [Google Scholar]
- Link MW, Mokdad AH, Stackhouse HF, Flowers NT. Race, ethnicity, and linguistic isolation as determinants of participation in public health surveillance surveys. Prev Chronic Dis. 2006 Retrieved August 10, 2016, from http://www.cdc.gov/pcd/issues/2006/jan/05_0055.htm. [PMC free article] [PubMed]
- Logan JR, Turner RN. Hispanics in the United States: Not Only Mexicans. Brown University; 2013. [Google Scholar]
- Lopez G, Gonzalez-Barrera A. Afro-Latino: A deeply rooted identity among U.S. Hispanics. Pew Research Center; 2016. Retrieved August 10, 2016, from http://www.pewresearch.org/fact-tank/2016/03/01/afro-latino-a-deeply-rooted-identity-among-u-s-hispanics/ [Google Scholar]
- Lu PJ, Rodríguez-Lainz A, O’Halloran A, Greby S, Williams WW. Adult vaccination disparities among foreign-born populations in the U.S., 2012. Am J Prev Med. 2014;47(6):722–733. doi: 10.1016/j.amepre.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas JW, Freeman G, Adams PF. Health of Hispanic Adults: United States, 2010–2014. 2016 (NCHS Data Brief No. 251). Retrieved August 12, 2016, from http://www.cdc.gov/nchs/data/databriefs/db251.pdf. [PubMed]
- National Committee on Vital and Health Statistics (NCVHS) (US) Migration, Vital, and Health Statistics. U.S. Department of health, Education, and Welfare. Public Health Service Health Services and Mental Health Administration; Washington, D: 1968. Retrieved August 12, 2016, from http://www.cdc.gov/nchs/data/series/sr_04/sr04_009.pdf. [Google Scholar]
- National Research Council (US) Eliminating Health Disparities: Measurement and Data Needs. In: Ver Ploeg M, Perrin E, editors. Panel on DHHS Collection of Race and Ethnicity Data. Committee on National Statistics, Division of Behavioral and Social Sciences and Education; Washington, DC: The National Academies Press; 2004. Retrieved August 12, 2016, from https://www.nap.edu/read/10979/chapter/3#15. [PubMed] [Google Scholar]
- Office of Management and Budget (OMB) Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity. Washington, D.C: Government Printing Office; 1997. Retrieved August 12, 2016, from www.whitehouse.gov/omb/fedreg/1997standards.html. [Google Scholar]
- Office of Management and Budget (OMB) Standards for Maintaining, Collecting, and Presenting Federal Data on Race and Ethnicity. 190. Vol. 81. Washington, D.C.: Government Printing Office; 2016. pp. 67398–67401. Retrieved October 23, 2016, https://www.gpo.gov/fdsys/pkg/FR-2016-09-30/pdf/2016-23672.pdf. [Google Scholar]
- Ortmann LW, Barret D, Saenz C, Bernheim R, Dawson A, Valentine J, Reis A. Public Health Ethics: Global Cases, Practice, and Context. In: Barrett DH, Ortmann LH, Dawson A, Saenz C, Reis A, Bolan G, editors. Public Health Ethics: Cases Spanning the Globe. Springer International; 2016. pp. 3–35. [PubMed] [Google Scholar]
- Pastor PN, Reuben CA, Duran CR. Reported Child Health Status, Hispanic Ethnicity, and Language of Interview: United States, 2011–2012. 2015 (National Health Statistics Reports No. 82). Retrieved August 12, 2016, from http://www.cdc.gov/nchs/data/nhsr/nhsr082.pdf. [PubMed]
- Patient Protection and Affordable Care Act. Public Law No. 111-148, Section 4302, 124 Stat. 119. 2010 Retrieved August 12, 2016, from https://www.gpo.gov/fdsys/pkg/PLAW-111publ148/pdf/PLAW-111publ148.pdf.
- Pearson WS, Garvin WS, Ford ES, Balluz LS. Analysis of five-year trends in self-reported language preference and issues of item non-response among Hispanic persons in a large cross-sectional health survey: implications for the measurement of an ethnic minority population. Popul Health Metr. 2010;8(7) doi: 10.1186/1478-7954-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penman-Aguilar A, Talih M, Huang D, Moonesinghe R, Bouye K, Beckles G. Measurement of Health Disparities, Health Inequities, and Social Determinants of Health to Support the Advancement of Health Equity. J Public Health Manag Pract. 2016;22(1 Suppl):S33–S42. doi: 10.1097/PHH.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perot RT, Youdelman M. Racial, Ethnic, and Primary Language Data Collection in the Health Care System: An Assessment of Federal Policies and Practices. The Commonwealth Fund; 2001. Sep, Retrieved August 12, 2016, from http://www.commonwealthfund.org/~/media/files/publications/fund-report/2001/sep/racial--ethnic--and-primary-language-data-collection-in-the-health-care-system--an-assessment-of-fed/perot_racialethnic_492-pdf.pdf. [Google Scholar]
- Pew Research Center. Modern Immigration Wave Brings 59 Million to U.S., Driving Population Growth and Change Through 2065: Views of Immigration’s Impact on U.S. Society Mixed. 2015 Retrieved August 12, 2016, from http://www.pewhispanic.org/files/2015/09/2015-09-28_modern-immigration-wave_REPORT.pdf.
- Public Health Leadership Society. Principles of the Ethical Practice of Public Health. 2002 Retrieved August 12, 2016, from http://ethics.iit.edu/ecodes/node/4734.
- Public Health Functions Steering Committee. Essential Public Health Services. 1994 Retrieved August 12, 2016, from http://www.cdc.gov/nphpsp/essentialServices.html.
- Richardson LD. Integrating Health Equity Into Practice and Policy. J Public Health Manag Pract. 2016;22(1 Supplement):S107–109. doi: 10.1097/PHH.0000000000000372. [DOI] [PubMed] [Google Scholar]
- Singh GK, Lin SC. Marked Ethnic, Nativity, and Socioeconomic Disparities in Disability and Health Insurance among US Children and Adults: The 2008–2010 American Community Survey. Biomed Res Int. 2013;2013:17. doi: 10.1155/2013/627412. (Article ID 627412) Retrieved August 29, 2016 from http://dx.doi.org/10.1155/2013/627412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Rodríguez-Lainz A, Kogan MD. Immigrant Health Inequalities in the United States: Use of Eight Major National Data Systems. ScientificWorldJournal. 2013;2013:21. doi: 10.1155/2013/512313. (Article ID 512313) Retrieved August 29, 2016 from http://dx.doi.org/10.1155/2013/512313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JC, Medalia C. U.S. Census Bureau. Current Population Reports, P60–253, Health Insurance Coverage in the United States: 2014. Vol. 2015 U.S. Government Printing Office; Washington, DC: 2015. [Google Scholar]
- Steege AL, Baron SL, Marsh SM, Menéndez CC, Myers JR. Examining Occupational Health and Safety Disparities Using National Data: A Cause for Continuing Concern. Am J Ind Med. 2014;57(5):527–538. doi: 10.1002/ajim.22297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepler R, Brown A. Statistical Portrait of Hispanics in the United States. Washington, D.C: Pew Research Center; 2016. Apr, Retrieved August 29, 2016 from http://www.pewhispanic.org/2016/04/19/statistical-portrait-of-hispanics-in-the-united-states/ [Google Scholar]
- Turner K, Wildsmith E, Guzman L, Alvira-Hammond M. The changing geography of Hispanic children and family. National Research Center on Hispanic Children & Families; 2016. Jan, [Google Scholar]
- Truman BI, Tinker T, Vaughan E, Kapella BK, Brenden M, Woznica CV, … Lichtveld M. Pandemic Influenza Preparedness and Response Among Immigrants and Refugees. Am J Public Health. 2009 Oct;99(S2):S278–S286. doi: 10.2105/AJPH.2008.154054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. American Community Survey. Questionnaire Archive. 2016 Retrieved August 29, 2016 from http://www.census.gov/programs-surveys/acs/methodology/questionnaire-archive.html.
- U.S. Centers for Disease Control and Prevention (CDC) Updated guidelines for evaluating public health surveillance systems: recommendations from the guidelines working group. MMWR 2001. 2001;50(RR-13) [PubMed] [Google Scholar]
- U.S. Centers for Disease Control and Prevention (CDC) National Notifiable Diseases Surveillance System (NNDSS) 2016a Retrieved August 12, 2016, from https://wwwn.cdc.gov/nndss/data-collection.html.
- U.S. Centers for Disease Control and Prevention (CDC) CDC Listeria Initiative Case Report Form, Version 2.0. 2016b Retrieved August 12, 2016, from https://www.cdc.gov/listeria/pdf/listeria-case-report-form-omb-0920-0004.pdf.
- U.S. Department of Health and Human Services (DHHS), National Committee on Vital and Health Statistics. Eliminating Health Disparities: Strengthening Data on Race, Ethnicity, and Primary Language in the United States. 2005 Retrieved August 12, 2016, from http://www.cdc.gov/nchs/data/misc/elihealthdisp.pdf.
- U.S. Department of Health and Human Services (DHHS), Office of the Assistant Secretary for Planning and Evaluation. HHS Implementation Guidance on Data Collection Standards for Race, Ethnicity, Sex, Primary Language, and Disability Status. 2011 Retrieved August 12, 2016, from https://aspe.hhs.gov/basic-report/hhs-implementation-guidance-data-collection-standards-race-ethnicity-sex-primary-language-and-disability-status.
- U.S. Department of Health and Human Services (DHHS)/Office of Minority Health. National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care: A Blueprint for Advancing and Sustaining CLAS Policy and Practice. 2013a Apr; Retrieved August 12, 2016, from https://www.pcpcc.org/sites/default/files/resources/A%20Blueprint%20for%20Advancing%20and%20Sustaining%20CLAS%20Policy%20and%20Practice.pdf.
- U.S. Department of Health and Human Services (DHHS) Language Access Plan 2013. 2013b Retrieved August 12, 2016, from https://www.hhs.gov/sites/default/files/open/pres-actions/2013-hhs-language-access-plan.pdf.
- U.S. Department of Health and Human Services (DHHS) Survey Data Elements to Unpack Diversity of Hispanic Populations, OPRE Report #2014-30. Washington, DC: Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; 2014. Prepared by Akilah Swinton and Ann Rivera, Office of Planning, Research and Evaluation. Retrieved August 12, 2016, from http://www.acf.hhs.gov/sites/default/files/opre/brief_survey_data_to_unpack_hispanic_final_03_27_2014.pdf. [Google Scholar]
- U.S. Department of Justice. The President Executive Order 13166 - Improving Access to Services for Persons With Limited English Proficiency. Federal Register. 2000 Aug;65(159) Retrieved August 12, 2016, from https://www.gpo.gov/fdsys/pkg/FR-2000-08-16/pdf/00-20938.pdf. [Google Scholar]
- U.S. National Center for Health Statistics. Program Review National Immunization Survey (NIS) and State and Local Area Integrated Telephone Survey (SLAITS) November 27–28, 2007. 2007 Retrieved August 12, 2016, from https://www.cdc.gov/nchs/data/bsc/program_review_reports/bsc_nis_progmatl.pdf.
- U.S. National Center for Health Statistics. National Immunization Survey Child (NIS-Child) NIS-Child Hard Copy Questionnaire Q3/2016. 2016 Retrieved August 12, 2016, from http://www.cdc.gov/vaccines/imz-managers/nis/downloads/nis-childquestionnaire-2016.pdf.
- Waksberg J, Levine D, Marker D. Assessment of Major Federal Data Sets for Analyses of Hispanic and Asian or Pacific Islander Subgroups and Native American: Task 2 Report: Extending the Utility of Federal Databases. 2000 Prepared for DHHS/ASPE: Westat, Rockville, MD. Retrieved August 12, 2016, from https://ia800908.us.archive.org/30/items/assessmentofmajo00west/assessmentofmajo00west.pdf.
- Westat. Gaps and Strategies for Improving AI/AN/NA Data, Final Report. 2007 Jan; Prepared for DHHS/ASPE: Westat, Rockville, MD. Retrieved August 12, 2016, from https://aspe.hhs.gov/sites/default/files/pdf/74926/report.pdf.
- Whatley M, Batalova J. Limited English Proficient Population of the United States. 2013 Jul; Retrieved August 12, 2016, from http://www.migrationpolicy.org/article/limited-english-proficient-population-united-states-1.
- Wildsmith E, Ansari A, Guzman L. Improving Data Infrastructure to Recognize Hispanic Diversity in the United States. 2015. (Publication No. 2015-23) [Google Scholar]
- Youdelman MK. The Medical Tongue: U.S. Laws And Policies On Language Access. Health Aff. 2008;27(2):424–433. doi: 10.1377/hlthaff.27.2.424. [DOI] [PubMed] [Google Scholar]