Abstract
The current study explores racial/ethnic disparities in the quality of patient-provider communication during treatment, among breast cancer patients. A unique data set, Medical Expenditure Panel Survey and Experiences With Cancer Supplement 2011, is used to examine this topic. Using measures of the quality of patient-provider communication that patients are best qualified to evaluate, we explore the relationship between race/ethnicity and patients’ perspectives on whether (1) patient-provider interactions are respectful, (2) providers are listening to patients, (3) providers provide adequate explanations of outcomes and treatment, and (4) providers spend adequate time in interacting with the patients. We also examine the relationship between race/ethnicity and patients’ perspectives on whether their (1) doctor ever discussed need for regular follow-up care and monitoring after completing treatment, (2) doctor ever discussed long-term side effects of cancer treatment, (3) doctor ever discussed emotional or social needs related to cancer, and (4) doctor ever discussed lifestyle or health recommendations. Multivariate ordinary least squares and ordered logistic regression models indicate that after controlling for factors such as income and health insurance coverage, the quality of patient-provider communication with breast cancer patients varies by race/ethnicity. Non-Hispanic blacks experience the greatest communication deficit. Our findings can inform the content of future strategies to reduce disparities.
Keywords: patient-doctor communication, breast cancer, racial/ethnic disparities, Medical Expenditure Panel Survey, experiences with cancer supplement, cultural competency, patient activation, ordered logistic regression
Introduction
Race and ethnicity pose critical roles as predisposing factors for breast cancer diagnosis and survival. While non-Hispanic white women are more likely to be diagnosed with breast cancer, non-Hispanic black women are more likely to die from breast cancer.1 Indeed, the black/white breast cancer mortality rate ratio in the largest United States cities has increased over the last 20 years, with morality rates for non-Hispanic white women improving substantially over the time period and disproportionately smaller improvements experienced by non-Hispanic black women.2 In 2013, non-Hispanic black women had a 39% higher mortality rate from breast cancer than non-Hispanic white women.3 In contrast, Hispanic women had significantly lower breast cancer incidence rates than non-Hispanic white women and non-Hispanic black women. Hispanic women also had significantly lower mortality rates,4 with mortality rates averaging 22.7, 30.8, and 14.8 for non-Hispanic white, non-Hispanic black, and Hispanic women, respectively, over the 2006-2010 period. There exists, therefore, a critical need to understand why race/ethnicity matters in breast cancer mortality outcomes and what needs to be done in order for non-Hispanic black women to experience similar reductions in breast cancer mortality as that experienced by non-Hispanic white and Hispanic women.
A number of factors have been identified as causal influences on disparities in breast cancer outcomes in the United States. Biological differences between black and white women, specifically the greater likelihood that black women experience more aggressive tumors at earlier ages, have been noted to be a key factor.5 Social and behavioral factors also play a role. Underuse of screening mammography and lack of diagnostic follow-up among black women have been associated with their relatively lower incomes, educational attainment, and health insurance coverage.6 Cultural preferences and fear have been documented to contribute to disparities. Health system factors may also play a role in breast health disparities. Structural and organizational differences in health facilities and provider communication of treatment options available for patients may affect patient outcomes.7
The current study explores racial/ethnic disparities in the quality of patient-provider communication during treatment, among breast cancer patients. Due to the correlation between race/ethnicity and socioeconomic factors (health insurance and income) and the potential for omitted variable bias, we distinguish between the unique roles of these 2 types of factors by including measures of both in our analysis. The central hypothesis of this article is that there are racial/ethnic differences in high-quality patient-provider communication, and these differences correspond with racial/ethnic differences in breast cancer survival rates. Thus, we predict that as survival rates are highest for Hispanic women compared with non-Hispanic whites and non-Hispanic blacks, higher quality patient-provider communication occurs with Hispanic women.
The main motivation guiding our research is to inform interventions focused on alleviating disparities by considering health system change strategies (ie, changes in health care delivery patterns, health policy, or environmental and community supports that improve health outcomes and health care). We seek to provide viable, yet underutilized solutions for reducing disparities in breast cancer outcomes. Many data sources used to explore breast health outcomes do not include detailed information on provider characteristics or patient-provider communication. We have identified a unique data set that allows such exploration and a first look at racial/ethnic disparities in patient-provider communication (a health care system characteristic) for a national sample of breast cancer survivors.
Study Design and Methodology
Databases
This study is a cross-sectional data analysis using the 2011 wave of the Medical Expenditure Panel Survey (MEPS) and its supplemental 2011 study on Experiences With Cancer Survivorship. The Agency for Healthcare Research and Quality (AHRQ) developed the first wave of the MEPS in 1996. The intent of this effort was to provide a national data source on health care utilization and expenditures, health status, and health insurance coverage and reimbursement, with patients, medical providers, health insurers, and employers as the sources of data.
To obtain a nationally representative sample, the MEPS sample of families and individuals is drawn from a subsample of households who participated in the annual National Health Interview Survey (NHIS). The NHIS is a continuing survey that is conducted annually by the National Center on Health Statistics to monitor trends in illness and disability, as well as whether national health objectives are achieved. While the NHIS includes an approximate survey sample of 35 000 to 40 000 households, MEPS is composed of a sample of 15 000 households.8,9
In addition to the data elements described above, MEPS also includes questions adapted from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey. CAHPS asks respondents to report on their experiences with health care and focuses on components of the quality of care that patients are best qualified to evaluate, that is, whether provider communication skills are effective and patient’s perceptions of their quality of access to care.
In addition, the 2011 MEPS included a supplement that specifically focused on patient experiences with cancer care, that is, Experiences With Cancer Survivorship Supplement. Participants in the 2011 MEPS study who had cancer were asked to complete a self-administered questionnaire. The Experiences With Cancer Survivorship questionnaire asks cancer survivors about financial costs of cancer, access to health care, conflicts of cancer survivorship with work and normal daily activities, and use of health care and prescription drugs.
MEPS and the Experiences With Cancer Supplement provide unique data for understanding quality of patient-provider communication during breast cancer treatment. MEPS includes 4 patient-physician communication questions from the CAHPS, based on the patient’s perception. The questions explore whether patient-provider interactions were respectful, providers listen to patients, providers provide adequate explanations of outcomes and treatment, and providers spend adequate time in interacting with the patients. The Experiences With Cancer supplement includes detailed questions about the types of information shared by providers with their patients, for example, whether the provider explained late or long-term effects of cancer treatments.
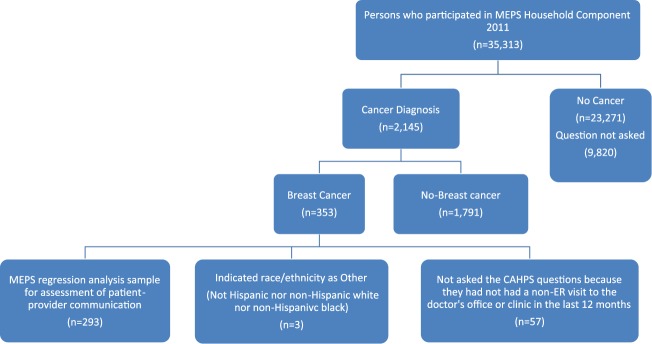
For our analysis, we use data for all women who reported having breast cancer in the 2011 MEPS. A diagnosis of breast cancer was based on an affirmative response to the survey question, “(Have/Has) (PERSON) ever been told by a doctor or other health professional that (PERSON) had a cancer or malignancy of any kind?” Then if the respondents indicated that the cancer was breast, they were included in our analysis sample. There were 353 women who participated in the 2011 MEPS and met the sample inclusion criteria. Among these women, we excluded those whose race/ethnicity was other (n = 3). In addition, 53 women did not answer the CAHPS questions because they did not meet the MEPS requirement that all respondents to these questions have at least 1 nonemergency room visit to the doctor’s office or clinic within 12 months of the survey date. Thus, our regression analysis sample included 293 respondents (see Figure 1).
Figure 1.
Analysis sample from MEPS using CAHPS patient-provider communication measures.
Note. MEPS = Medical Expenditure Panel Survey; CAHPS = Consumer Assessment of Healthcare Providers and Systems.
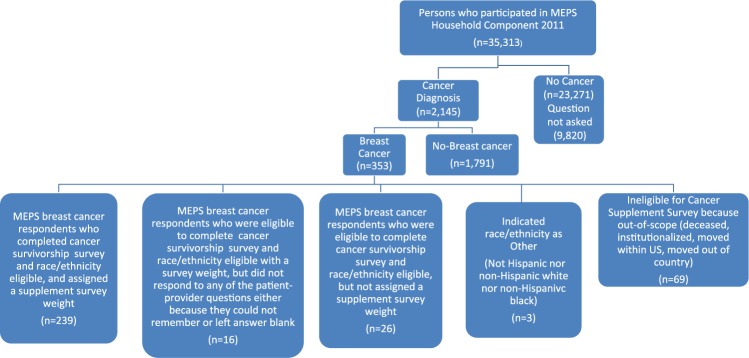
The Cancer Survivorship Supplement included a subset of respondents to the main MEPS survey. If cancer survivors who were interviewed by MEPS experienced a change in status due to death, institutionalization, moving to a different residence within the United States, or moving out of country, they were not interviewed for the subsequent Cancer Survivorship Supplement Survey. Among the 353 women with breast cancer who participated in the main MEPS survey, 69 experienced a change in status. We excluded an additional 3 women because they indicated that there race/ethnicity was other. Of the remaining 281 participants in the cancer survivorship survey, 26 were excluded from our analysis sample because MEPS did not assign them a positive sample weight. An additional 16 respondents were excluded from our analysis sample because for every dependent variable measure of patient-provider communication, they responded that they did not remember or they did not provide an answer to the question. Our final analysis sample included 239 respondents (see Figure 2). Regression analysis sample sizes using the survivor supplement varied from 216 to 239 depending on the number of respondents who provided information on a particular patient-provider communication question.
Figure 2.
Analysis sample from MEPS using cancer survivorship patient-provider communication measures.
Note. MEPS = Medical Expenditure Panel Survey.
For the ordinary least squares (OLS) model using the composite score, 34 observations were “missing.” This was because the composite measure of patient-provider communication requires that respondents answer all 4 of the patient-provider communication questions and that only occurred for 205 of the 239 respondents in our analysis sample. As these 34 observations consisted of 14% of our study sample, we imputed values of the composite variable to avoid losing observations, as well as to increase the statistical power of the model. However, before imputation, we examined why the data were missing and found that they were missing completely at random (MCAR). To test this, we created a binary variable that was equal to 1 if the value of composite score was missing and zero otherwise. Then, we ran a logit model to see whether any of any of the other variables in our model predicted whether the composite score was missing. Based on the result of the logit model, we identified that other variables did not predict whether the composite score was missing. We concluded that imputation would thus generate unbiased estimates. Therefore, multiple imputations by chain equation are implemented using Stata version 14.2, and a sample size of 239 was used for the OLS regression.
Regression Modeling and Descriptive Statistics
All analyses were conducted using Stata version 14.2, and all results take into account the complex sampling design of MEPS. Descriptive tables and regression analyses utilize the MEPS person-level weights or the person-level weight designed for those who participated in the self-administered Experiences With Cancer Supplement Survey. The cancer supplement weight adjusts for survey nonresponse and is an estimate of the adult population reporting diagnosis or treatment for cancer.
We estimated OLS models for our composite measures of patient-provider communication and ordered logistic regression models for categorical dependent variable models. In the latter case, a survivor’s answer was presented as an ordinal ranking such as (always, usually, sometimes/never) or (discussed in detail, briefly discussed, didn’t discuss). For this type of data, the ordered probability model is a suitable tool of analysis (see Greene10(pp469-481)). The ordered logit model specification is shown as follows:
where is vector of explanatory variables and is the error term. In this model, is unobserved. What we do observe is:
This is a form of censoring. The ’s are unknown parameters that are estimated with δ. The respondents have their own intensity of feelings, which depends on certain measurable factors, , and certain unobservable factors, . One could respond to the questionnaire with their own if asked to do so, but they are not. Given only 3 possible answers, they choose the category that most closely represents their own feelings. In the ordered logit model, has a standard logistic distribution. The reference category in each of our logistic regressions is the category where the most information is communicated, that is, always or discussed in detail.
Prior to performing the OLS regressions and ordered logistic regressions, data were examined to assure assumptions for all planned statistical tests were met, that is, tests of normality, examination of potential outliers, and formal tests for multicollinearity. Scatter plots of relationships between the dependent and independent variables were linear. No outliers were detected. No heteroscedasticity of errors was present. Collinearity diagnostics with variance inflation factor tests indicated that multicollinearity was not present in the regression models. In addition, we performed brant tests of the proportional odds assumption and the results indicate this assumption was not violated.
Dependent Variables
The 10 dependent variables in this study are measures from the CAHPS and the Experiences With Cancer Survivorship Supplement. The first 5 dependent variables are the patient-physician communication variables from CAHPS. The following 4 questions that the 2011 MEPS adapted from the CAHPS survey are the core elements of these dependent variables: (1) “How often have providers shown respect for what you had to say?” (2) “How often have health care providers listened carefully to you?” (3) “How often have health care providers explained things so you understood?” and (4) “How often have health providers spent enough time with you?” The response categories for each of these questions were never, sometimes, usually, and always. As recommended by CAHPS, we combined the first 2 responses never and sometimes into a single response category whose value was 1, with the last 2 response categories having coded values of 2 (usually) and 3 (always).11 Our first dependent variable measure, the patient-physician communication composite score, was composed by summing the coded values of each participant’s responses from the 4 CAHPS communication measures. Values for the composite score ranged from 4 (worst) to 12 (best). This composite score has been found to have high internal consistency reliability.12 We subsequently created 4 specific communication variables to examine the relationship between race/ethnicity and each of the components of the composite score. We coded each of the 4 questions mentioned above as 1 if the respondent reported (never/sometimes), 2 (usually), and 3 (always). Prior to creating the composite scores, the variables were all normalized. We tested the variance equality hypothesis and confirmed that we could not reject the null hypothesis that the variances of each question were equal.
The last 5 dependent variables are based on MEPS Experiences With Cancer Survivorship Supplement. They were developed from the following 4 questions: (1) “Doctor ever discussed need for regular follow-up care and monitoring after completing treatment,” (2) “doctor ever discussed long-term side effects of cancer treatment,” (3) “doctor ever discussed emotional or social needs related to cancer,” and (4) “doctor ever discussed lifestyle or health recommendations.” A quality of patient-provider information sharing composite score was derived by summing the values of the responses to the 4 questions, with the composite score ranging from 4 to 12. The response for each of the 4 quality of patient-provider information sharing variables was coded as 1 (didn’t discuss), 2 (briefly discussed), and 3 (discussed in detail).
Independent Variables
Several patient characteristics are consistently identified in the literature as factors associated with patient-provider communication.11,13-15 We include measures of the factors as independent variables in our regression models. These variables are age, race/ethnicity, marital status, education, insurance status, region of residence, and income status. We also used a continuous measure of the number of comorbid conditions.
We created 3 categorical variables for race/ethnicity: non-Hispanic white, non-Hispanic black, and Hispanic. The sample of respondents from other race/ethnicity groups was so small (n = 3) that we did not include them in this analysis. Our regression models include 4 levels of educational training: some education, General Education Development (GED) or high school, baccalaureate education, and postbaccalaureate education. The insurance measures are private insurance, public insurance, and uninsured. The marital status measures include married, widowed, divorced/separated, and never married. We also controlled for 3 levels of income/poverty status: low income (125% to less than 200% of poverty), middle income (200% to less than 400% of poverty), and high income (greater than or equal to 400% of poverty). There are 4 region measures, namely, Northeast, Midwest, South, and West. We include continuous variable measures of age and number of comorbidities. The comorbid conditions include hypertension, coronary heart disease, angina, myocardial infarction, stroke, emphysema, diabetes, arthritis, and asthma.
Statistical Analysis
As mentioned earlier, the outcomes of interest are 4 patient-physician communication variables and their composite score, and 4 variables on quality of patient-provider information sharing and their composite score. We estimated composite score patient-physician communication and composite score quality of patient-provider information sharing models using OLS. Thereafter, ordered logistic regression was used to estimate coefficients for the 8 communication and patient-provider information sharing variables.
Results
Descriptive Statistics
For the MEPS 2011 sample of persons who reported having breast cancer, Table 1 reports descriptive statistics for the composite patient-provider communication score, the 4 patient-provider communication variables, and all the regression independent variables according to race/ethnicity. The mean composite score on patient-provider communication is highest for non-Hispanic whites (10.27). The mean for non-Hispanic blacks is 9.40 and for Hispanics is 9.04. There is a statistically significant difference (P = .02) in the composite patient-provider communication score of non-Hispanic whites versus non-Hispanic blacks. Also, there is a statistically significant difference (P = .006) in the composite patient-provider communication score of non-Hispanic whites versus Hispanics.
Table 1.
Bivariate Analysis of CAHPS Patient-Provider Communication Variables and Patient Characteristics by Race/Ethnicity—MEPS 2011.
| Means and t tests by race/ethnicity | |||||||
|---|---|---|---|---|---|---|---|
| Variables | Race/ethnicity | Mean | Linearized SE | 95% CI | P value | ||
| Composite communication score | Non-Hispanic white | 10.2 | 0.15 | 10.1-10.7 | |||
| Non-Hispanic black | 9.3*** | 0.34 | 8.8-10.2 | .021 | |||
| Hispanics | 9.0*** | 0.48 | 8.05-9.99 | .006 | |||
| No. of comorbidities | Non-Hispanic white | 1.7 | 0.09 | 1.59-1.97 | |||
| Non-Hispanic black | 2.06 | 0.16 | 1.69-2.35 | .193 | |||
| Hispanics | 1.5*** | 0.20 | 0.79-1.62 | .020 | |||
| Age, y | Non-Hispanic white | 67.8 | 0.92 | 65.97-69.66 | |||
| Non-Hispanic black | 61.6*** | 1.34 | 59.08-64.42 | .001 | |||
| Hispanics | 56.3*** | 2.8 | 50.77-62.30 | .000 | |||
| Percentages and chi-square tests by race/ethnicity | |||||||
| Non-Hispanic white (n = 185) | Non-Hispanic black (n = 72) | Hispanics (n = 36) | Total | ||||
| Row % | 95% CI | Row % | 95% CI | Row % | 95% CI | Row % | |
| Respect | |||||||
| Sometimes/never (n = 32) | 54.6 | 35.9-72.1 | 37.7 | 21.4-57.3 | 7.7 | 2.3-23.3 | 100.0 |
| Usually (n = 63) | 79.8 | 67.3-88.4 | 11.6 | 5.2-24.2 | 8.5 | 4.1-16.8 | 100.0 |
| Always (n = 198) | 84.3 | 79.7-88.1 | 12.4 | 9.2-16.6 | 3.2 | 1.7-6.2 | 100.0 |
| Total (n = 293) | 81.1 | 76.7-84.8 | 14.2 | 11.0-18.2 | 4.7 | 3.0-7.2 | 100.0 |
| Pearson: Uncorrected χ2(4) = 15.0636 | |||||||
| Design-based F(3.81, 224.69) = 4.3919 Pr = 0.002 | |||||||
| Listen | |||||||
| Sometimes/never (n = 32) | 68.8 | 48.4-83.9 | 22.9 | 11.1-41.4 | 8.3 | 2.0-28.9 | 100.0 |
| Usually (n = 68) | 78.6 | 66.2-87.3 | 14.5 | 7.3-26.7 | 6.9 | 3.2-14.3 | 100.0 |
| Always (n = 193) | 83.6 | 78.5-87.7 | 12.9 | 9.3-17.6 | 3.5 | 2.0-6.0 | 100.0 |
| Total (n = 293) | 81.1 | 76.7-84.8 | 14.2 | 11.0-18.2 | 4.7 | 3.0-7.2 | 100.0 |
| Pearson: Uncorrected χ2(4) = 4.4890 | |||||||
| Design-based F(3.74, 220.92) = 1.1639 Pr = 0.327 | |||||||
| Explain | |||||||
| Sometimes/never (n = 23) | 62.0 | 39.2-80.4 | 31.1 | 14.7-54.1 | 6.9 | 1.6-25.6 | 100.0 |
| Usually (n = 84) | 80.6 | 70.6-87.7 | 12.3 | 6.8-21.3 | 7.2 | 3.5-14.1 | 100.0 |
| Always (n = 186) | 83.1 | 77.7-87.4 | 13.6 | 9.9-18.3 | 3.3 | 1.8-6.1 | 100.0 |
| Total (n = 293) | 81.1 | 76.7-84.8 | 14.2 | 11.0-18.2 | 4.7 | 3.0-7.2 | 100.0 |
| Pearson: Uncorrected χ2(4) = 6.6503 | |||||||
| Design-based F(3.84, 226.85) = 2.0566 Pr = 0.090 | |||||||
| Spend time | |||||||
| Sometimes/never (n = 47) | 56.9 | 39.9-72.5 | 29.9 | 17.5-46.2 | 13.1 | 5.5-28.0 | 100.0 |
| Usually (n = 81) | 81.3 | 74.1-86.9 | 12.7 | 8.3-18.9 | 6.0 | 3.1-11.2 | 100.0 |
| Always (n = 165) | 86.0 | 80.1-90.3 | 11.6 | 7.6-17.3 | 2.4 | 1.2-4.8 | 100.0 |
| Total (n = 293) | 81.1 | 76.7-84.8 | 14.2 | 11.0-18.2 | 4.7 | 3.0-7.2 | 100.0 |
| Pearson: Uncorrected χ2 (4) = 18.3509 | |||||||
| Design-based F(3.73, 220.07) = 6.1497 Pr = 0.000 | |||||||
| Health insurance | |||||||
| Private insurance (n = 189) | 82.7 | 77.3-87.0 | 12.6 | 9.1-17.1 | 4.7 | 2.7-8.0 | 100.0 |
| Public insurance (n = 92) | 75.7 | 66.6-82.9 | 16.7 | 11.1-24.4 | 7.6 | 3.9-14.1 | 100.0 |
| Uninsured (n = 12) | 72.9 | 38.6-92.0 | 20.6 | 5.1-55.3 | 6.5 | 1.5-24.1 | 100.0 |
| Total (n = 293) | 80.3 | 75.9-84.1 | 14.1 | 10.9-17.9 | 5.6 | 3.7-8.4 | 100.0 |
| Percentages and chi-square tests by race/ethnicity | |||||||
| Non-Hispanic white (n = 185) | Non-Hispanic black (n = 72) | Hispanics (n = 36) | Total | ||||
| Row % | 95% CI | Row % | 95% CI | Row % | 95% CI | Row % | |
| Pearson: Uncorrected χ2(4) = 2.8359 | |||||||
| Design-based F(3.41, 248.69) = 0.8569 Pr = 0.476 | |||||||
| Education levels | |||||||
| Some education (n = 22) | 67.2 | 50.8-80.2 | 27.9 | 16.2-43.6 | 4.9 | 1.8-13.1 | 100.0 |
| GED and HS (n = 173) | 83.3 | 77.7-87.7 | 11.9 | 8.4-16.7 | 4.8 | 2.6-8.5 | 100.0 |
| Baccalaureate (n = 50) | 80.7 | 67.4-89.4 | 12.4 | 5.5-25.5 | 6.9 | 2.6-17.5 | 100.0 |
| Postbaccalaureate (n = 48) | 79.2 | 68.0-87.2 | 13.8 | 7.5-24.0 | 7.0 | 3.0-15.3 | 100.0 |
| Total (n = 293) | 80.3 | 75.9-84.1 | 14.1 | 10.9-17.9 | 5.6 | 3.7-8.4 | 100.0 |
| Pearson: Uncorrected χ2(6) = 7.4488 | |||||||
| Design-based F(5.43, 396.23) = 1.3656 Pr = 0.232 | |||||||
| Marital status | |||||||
| Married (n = 138) | 82.6 | 76.3-87.5 | 11.5 | 7.6-16.9 | 5.9 | 3.3-10.2 | 100.0 |
| Widowed (n = 81) | 85.3 | 76.4-91.2 | 13.0 | 7.7-21.1 | 1.8 | 0.5-6.2 | 100.0 |
| Divorced (n = 41) | 68.5 | 56.5-78.4 | 21.4 | 13.1-33.1 | 10.1 | 5.1-19.2 | 100.0 |
| Never married (n = 33) | 69.4 | 47.4-85.1 | 22.2 | 10.3-41.5 | 8.4 | 1.8-31.0 | 100.0 |
| Total (n = 293) | 80.3 | 75.9-84.1 | 14.1 | 10.9-17.9 | 5.6 | 3.7-8.4 | 100.0 |
| Pearson: Uncorrected χ2(6) = 10.2464 | |||||||
| Design-based F(5.41, 394.71) = 1.8672 Pr = 0.093 | |||||||
| Family income as % of poverty line | |||||||
| Low income (n = 111) | 76.1 | 67.9-82.7 | 17.3 | 12.0-24.3 | 6.6 | 3.4-12.6 | 100.0 |
| Middle income (n = 90) | 79.6 | 71.3-86.0 | 14.6 | 9.4-22.0 | 5.8 | 2.8-11.4 | 100.0 |
| High income (n = 92) | 84.1 | 76.1-89.7 | 11.3 | 6.6-18.6 | 4.7 | 2.2-9.5 | 100.0 |
| Total (n = 293) | 80.3 | 75.9-84.1 | 14.1 | 10.9-17.9 | 5.6 | 3.7-8.4 | 100.0 |
| Pearson: Uncorrected χ2(4) = 3.1475 | |||||||
| Design-based F(3.80, 277.57) = 0.7212 Pr = 0.571 | |||||||
| Census regions | |||||||
| Northeast (n = 42) | 72.6 | 55.5-84.9 | 18.8 | 9.7-33.2 | 8.6 | 3.9-18.1 | 100.0 |
| Midwest (n = 84) | 88.5 | 79.0-94.0 | 11.2 | 5.7-20.7 | 0.3 | 0.0-2.4 | 100.0 |
| South (n = 120) | 77.3 | 69.5-83.6 | 15.5 | 10.8-21.7 | 7.2 | 3.8-13.2 | 100.0 |
| West (n = 55) | 83.6 | 73.7-90.3 | 9.8 | 4.7-19.1 | 6.6 | 2.8-14.8 | 100.0 |
| Total (n = 293) | 80.3 | 75.9-84.1 | 14.1 | 10.9-17.9 | 5.6 | 3.7-8.4 | 100.0 |
| Pearson: Uncorrected χ2(6) = 9.9688 | |||||||
| Design-based F(4.85, 353.82) = 1.8793 Pr = 0.100 | |||||||
| Number of population | 3 039 468 | 532 348 | 211 681 | 3 783 497 | |||
Note. Family income as % of poverty line is constructed by MEPS by dividing CPS family income by applicable poverty line. We treat survivors without family as 1-person families when constructing their poverty percentage and category. For CAHPS variables, we combined sometimes and never categories as one single category as “sometimes/never.” CAHPS = Consumer Assessment of Healthcare Providers and Systems; MEPS = Medical Expenditure Panel Survey; CPS = Current Population Survey; GED = General Education Development; HS = high school; CI = confidence interval.
P < .1. **P < .05. ***P < .01, indicates t-test P-value significance for mean differences of the continuous variables across race/ethnicity with non-Hispanic white as the base comparison group.
We can glean more insights about these racial/ethnic differences by looking at the responses to the 4 specific patient-provider communication questions. Using chi-square tests of association, the data suggest that there are statistically significant differences by race/ethnicity (at the .05 level or better) in patients’ perceptions of whether patient-provider interactions are respectful and providers spend adequate time in interacting with the patients. Looking at the distribution across race/ethnicity in the responses always, usually, and sometimes/never, non-Hispanic whites are most likely to perceive that patient-provider interactions are always respectful. Hispanic breast cancer patients are most likely to perceive that patient-provider interactions are usually respectful. Similarly, non-Hispanic blacks are most likely to perceive patient-provider interactions are sometimes/never respectful. Looking at the responses for whether patients perceive that providers spend adequate time in interacting with them, non-Hispanic whites are most likely to say always, while non-Hispanic blacks and Hispanics are most likely to say sometimes/never.
Accounting for racial/ethnic differences in education, region of residence, marital status, age, and comorbidities is also important because there are statistically significant differences in these variables by race/ethnicity. Non-Hispanic black breast cancer patients are more likely to have less than high school education than are non-Hispanic white and Hispanic patients. Non-Hispanic blacks and Hispanics are significantly younger than non-Hispanic whites. Hispanics also average significantly lower comorbidities than non-Hispanic blacks or non-Hispanic whites (1.51 vs 2.06 and 1.78). Although only marginally significant at the .093 level, note that non-Hispanic blacks are more likely to be never married, Hispanic breast cancer patients are more likely to be divorced, and non-Hispanic whites are more likely to be widowed. Non-Hispanic whites are more likely to live in the Midwest, while non-Hispanic blacks and Hispanics are more likely to live in the Northeast (P = .10).
Table 2 reports descriptive statistics for the final 5 dependent and all the regression independent variables according to race/ethnicity, for participants in the Experiences in Breast Cancer Survivorship Survey. There are sample size differences and differences in descriptive statistics in Tables 1 and 2 because respondents to the Experiences in Breast Cancer Survivorship Survey are a subset of the breast cancer survivors who participated in the MEPS.
Table 2.
Bivariate Analysis of Experiences With Cancer Supplement Patient-Provider Communication Variables and Patient Characteristics by Race/Ethnicity—MEPS 2011.
| Means and t tests by race/ethnicity | |||||||
|---|---|---|---|---|---|---|---|
| Variables | Race/ethnicity | Mean | Linearized SE | 95% CI | P value | ||
| Non-Hispanic white | 9.48 | 0.23 | 9.0-9.9 | ||||
| Non-Hispanic black | 10.11 | 0.40 | 9.10-10.9 | .255 | |||
| Hispanics | 11.05*** | 0.35 | 10.3-11.8 | .001 | |||
| No. of comorbidities | |||||||
| Non-Hispanic white | 1.85 | 0.11 | 1.6-2.9 | ||||
| Non-Hispanic black | 2.19 | 0.199 | 1.8-2.6 | .186 | |||
| Hispanics | 1.24*** | 0.239 | 0.74-1.7 | .026 | |||
| Age, y | |||||||
| Non-Hispanic white | 68.33 | 1.05 | 66.2-70.4 | ||||
| Non-Hispanic black | 61.35*** | 1.329 | 58.69-64.0 | .000 | |||
| Hispanics | 57.85*** | 3.19 | 51.5-64.2 | .003 | |||
| Percentages and chi-square tests by race/ethnicity | |||||||
| Non-Hispanic whites (n = 185) | Non-Hispanic black (n = 72) | Hispanics (n = 36) | Total | ||||
| Row % | 95% CI | Row % | 95% CI | Row % | 95% CI | Row % | |
| Follow-up | |||||||
| Didn’t discuss (n = 11) | 52.7 | 23.1-80.5 | 41.2 | 15.7-72.4 | 6.1 | 0.8-35.3 | 100.0 |
| Discussed briefly (n = 44) | 91.4 | 81.9-96.1 | 7.5 | 2.8-18.3 | 1.2 | 0.1-9.0 | 100.0 |
| Discussed in details (n = 178) | 79.5 | 73.7-84.3 | 14.2 | 10.3-19.3 | 6.3 | 3.7-10.4 | 100.0 |
| Total (n = 233) | 81.1 | 76.3-85.1 | 13.6 | 10.3-17.9 | 5.2 | 3.2-8.5 | 100.0 |
| Pearson: Uncorrected χ2(4) = 8.5460 | |||||||
| Design-based F(3.67, 172.37) = 3.1323 Pr = 0.019 | |||||||
| Side effects | |||||||
| Didn’t discuss (n = 42) | 84.7 | 72.3-92.1 | 14.3 | 7.1-26.5 | 1.1 | 0.1-7.7 | 100.0 |
| Discussed briefly (n = 55) | 90.0 | 80.8-95.0 | 7.1 | 3.0-15.9 | 2.9 | 0.9-9.4 | 100.0 |
| Discussed in details (n = 128) | 74.1 | 66.2-80.8 | 17.6 | 12.3-24.7 | 8.2 | 4.7-14.1 | 100.0 |
| Total (n = 225) | 80.4 | 75.4-84.6 | 14.2 | 10.7-18.6 | 5.5 | 3.3-8.8 | 100.0 |
| Pearson: Uncorrected χ2(4) = 8.4680 | |||||||
| Design-based F(3.81, 171.46) = 3.0498 Pr = 0.020 | |||||||
| Social effects | |||||||
| Didn’t discuss (n = 62) | 88.2 | 79.4-93.6 | 11.1 | 5.9-19.8 | 0.7 | 0.1-4.8 | 100.0 |
| Discussed briefly (n = 54) | 79.2 | 67.4-87.6 | 12.6 | 6.9-22.0 | 8.2 | 3.7-17.1 | 100.0 |
| Discussed in details (n = 101) | 76.0 | 67.5-82.9 | 16.4 | 10.5-24.6 | 7.6 | 3.9-14.2 | 100.0 |
| Total (n = 217) | 80.5 | 75.5-84.7 | 13.8 | 10.4-18.2 | 5.6 | 3.4-9.1 | 100.0 |
| Pearson: Uncorrected χ2(4) = 5.8211 | |||||||
| Design-based F(3.79, 166.55) = 2.0626 Pr = 0.092 | |||||||
| Lifestyle change | |||||||
| Didn’t discuss (n = 43) | 85.7 | 73.9-92.7 | 13.4 | 6.6-25.1 | 1.0 | 0.1-7.0 | 100.0 |
| Discussed in brief (n = 70) | 89.5 | 81.7-94.2 | 7.7 | 3.8-15.0 | 2.8 | 1.0-8.0 | 100.0 |
| Discussed in details (n = 113) | 71.7 | 62.0-79.6 | 18.6 | 12.6-26.7 | 9.7 | 5.5-16.6 | 100.0 |
| Total (n = 226) | 80.5 | 75.6-84.6 | 13.9 | 10.5-18.3 | 5.6 | 3.5-9.0 | 100.0 |
| Pearson: Uncorrected χ2(4) = 11.6661 | |||||||
| Design-based F(3.72, 159.92) = 4.0980 Pr = 0.004 | |||||||
| Percentages and chi-square tests by race/ethnicity | |||||||
| Non-Hispanic whites (n = 185) | Non-Hispanic black (n = 72) | Hispanics (n = 36) | Total | ||||
| Row % | 95% CI | Row % | 95% CI | Row % | 95% CI | Row % | |
| Health insurance | |||||||
| Private insurance (n = 155) | 81.9 | 75.9-86.7 | 13.3 | 9.4-18.5 | 4.7 | 2.6-8.5 | 100.0 |
| Public insurance (n = 75) | 76.0 | 65.6-84.1 | 15.3 | 9.5-23.7 | 8.7 | 4.4-16.6 | 100.0 |
| Uninsured (n = 9) | 87.9 | 58.8-97.4 | 5.5 | 0.6-35.8 | 6.5 | 1.2-28.9 | 100.0 |
| Total (n = 239) | 80.4 | 75.9-84.3 | 13.6 | 10.5-17.5 | 6.0 | 3.8-9.1 | 100.0 |
| Pearson: Uncorrected χ2(4) = 2.4882 | |||||||
| Design-based F(3.53, 204.59) = 0.8487 Pr = 0.484 | |||||||
| Education level | |||||||
| Some education (n = 29) | 69.2 | 51.4-82.7 | 27.0 | 14.8-44.0 | 3.8 | 1.0-12.8 | 100.0 |
| GED and HS (n = 135) | 82.5 | 77.2-86.7 | 12.3 | 8.8-16.9 | 5.3 | 2.9-9.6 | 100.0 |
| Baccalaureate (n = 45) | 82.3 | 67.6-91.2 | 9.4 | 3.3-24.1 | 8.3 | 3.0-20.8 | 100.0 |
| Postbaccalaureate (n = 30) | 78.4 | 62.7-88.6 | 14.6 | 6.7-29.0 | 7.0 | 2.6-17.6 | 100.0 |
| Total (n = 239) | 80.4 | 75.9-84.3 | 13.6 | 10.5-17.5 | 6.0 | 3.8-9.1 | 100.0 |
| Pearson: Uncorrected χ2(6) = 6.3618 | |||||||
| Design-based F(5.31, 307.81) = 1.1658 Pr = 0.326 | |||||||
| Marital status | |||||||
| Married (n = 120) | 82.8 | 75.9-88.0 | 11.7 | 7.5-17.8 | 5.5 | 2.9-10.2 | 100.0 |
| Widowed (n = 59) | 84.1 | 74.0-90.8 | 13.6 | 7.8-22.7 | 2.3 | 0.6-7.9 | 100.0 |
| Divorced (n = 45) | 70.3 | 57.7-80.4 | 18.3 | 10.6-29.8 | 11.4 | 5.7-21.7 | 100.0 |
| Never married (n = 15) | 71.6 | 46.1-88.2 | 17.8 | 7.4-36.9 | 10.6 | 2.1-40.0 | 100.0 |
| Total (n = 239) | 80.4 | 75.9-84.3 | 13.6 | 10.5-17.5 | 6.0 | 3.8-9.1 | 100.0 |
| Pearson: Uncorrected χ2(6) = 6.7887 | |||||||
| Design-based F(5.29, 306.65) = 1.2890 Pr = 0.267 | |||||||
| Family income as % of poverty line | |||||||
| Low income (n = 83) | 74.3 | 65.2-81.7 | 17.7 | 12.1-25.2 | 8.0 | 4.0-15.3 | 100.0 |
| Middle income (n = 75) | 80.1 | 71.3-86.7 | 13.9 | 8.7-21.5 | 6.0 | 2.7-12.7 | 100.0 |
| High income (n = 81) | 85.0 | 76.4-90.9 | 10.5 | 5.7-18.6 | 4.5 | 1.9-10.0 | 100.0 |
| Total (n = 239) | 80.4 | 75.9-84.3 | 13.6 | 10.5-17.5 | 6.0 | 3.8-9.1 | 100.0 |
| Pearson: Uncorrected χ2(4) = 3.5717 | |||||||
| Design-based F(3.76, 217.95) = 1.0212 Pr = 0.395 | |||||||
| Census region | |||||||
| Northeast (n = 35) | 70.2 | 53.1-83.1 | 19.0 | 9.9-33.3 | 10.8 | 4.9-22.3 | 100.0 |
| Midwest (n = 56) | 89.8 | 79.5-95.2 | 9.8 | 4.4-20.2 | 0.4 | 0.1-3.1 | 100.0 |
| South (n = 109) | 76.6 | 68.3-83.2 | 16.2 | 11.1-23.0 | 7.2 | 3.6-13.8 | 100.0 |
| West (n = 39) | 85.7 | 74.8-92.4 | 7.5 | 3.2-16.4 | 6.8 | 2.7-16.3 | 100.0 |
| Total (n = 239) | 80.4 | 75.9-84.3 | 13.6 | 10.5-17.5 | 6.0 | 3.8-9.1 | 100.0 |
| Pearson: Uncorrected χ2(6) = 10.7998 | |||||||
| Design-based F(5.18, 300.46) = 2.3096 Pr = 0.042 | |||||||
| Number of population | 2 437 882 | 412 887 | 180 534 | 3 031 305 | |||
Note. MEPS = Medical Expenditure Panel Survey; GED = General Education Development; HS = high school; CI = confidence interval.
P < .1. **P < .05. ***P < .01, indicates t-test P-value significance for mean differences of the continuous variables across.
In Table 2, we see an interesting contrast in the value of the composite scores for the quality of patient-provider information sharing variables. The mean composite score on quality of patient-provider information sharing is highest for Hispanics (11.05). The mean for non-Hispanic blacks is 10.11 and for non-Hispanic whites is 9.48. The quality of patient-provider information sharing composite score is significantly higher for Hispanics, compared with non-Hispanic blacks and non-Hispanic whites.
There are statistically significant differences by race/ethnicity (at the .05 level or better) for 3 of the 4 quality of patient-provider information sharing variables (follow-up, side effects, lifestyle change), and the fourth (social effects) is significant at the .10 level. Surprisingly, non-Hispanic black and Hispanic breast cancer survivors are most likely to report that their doctor discussed in detail the need for regular follow-up care and monitoring after completing treatment and that their doctor discussed in detail the long-term side effects of cancer treatment. In contrast, non-Hispanic whites are most likely to say their doctor discussed briefly the need for regular follow-up care and monitoring after completing treatment and discussed briefly the long-term side effects of cancer treatment. Non-Hispanic white breast cancer survivors are most likely to report that their doctor did not discuss social needs related to cancer, while non-Hispanic blacks report that social needs were discussed in detail and Hispanics report they were discussed briefly. Non-Hispanic blacks and Hispanics are most likely to say that lifestyle changes were discussed in detail, while non-Hispanic whites report that they were discussed briefly. Several sociodemographic factors also vary significantly by race/ethnicity, and thus, we include such factors in our regression models.
Multivariate Results
Table 3 reports the OLS and logistic regressions for patient-provider communication using the CAHPS composite and specific communication measures as the dependent variables. In the composite patient-provider communication regression, race/ethnicity and age were statistically significant. Hispanics have lower composite patient-provider communication scores than non-Hispanic whites (–1.121 [P = .04]). Older patients have higher patient-provider communication scores (0.0322 [P = .031]). Marginally significant in the composite patient-provider communication regressions are the variables non-Hispanic black (–0.727 [P = .06]), uninsured (–1.464 [P = .071]), and widowhood (–0.762 [P = .096]).
Table 3.
OLS and Ordered Logit Models Results: Patient-Provider Communication—MEPS 2011.
| Variables | (OLS) |
(OL) |
(OL) |
(OL) |
(OL) |
|---|---|---|---|---|---|
| Composite score | Respect | Listen | Explain | Spend time | |
| Race/ethnicity (non-Hispanic whitea) | |||||
| Non-Hispanic black | –0.72* | 0.60** | 0.75 | 0.64** | 0.45* |
| (0.38) | (0.24) | (0.27) | (0.27) | (0.18) | |
| [–1.48 to 0.02] | [0.27-1.34] | [0.37-1.53] | [0.28-1.47] | [0.20-1.00] | |
| Hispanics | –1.12** | 0.54 | 0.63 | 0.43* | 0.19*** |
| (0.55) | (0.29) | (0.37) | (0.21) | (0.11) | |
| Health insurance (private insurancea) | |||||
| Public insurance | [–2.21 to –0.03] | [0.19-1.58] | [0.20-2.05] | [0.17-1.12] | [0.07-0.6] |
| –0.48 | 0.41** | 0.71 | 0.85 | 0.84 | |
| (0.33) | (0.14) | (0.27) | (0.26) | (0.21) | |
| [–1.14 to 0.18] | [0.21-0.83] | [0.40-1.58] | [0.46-1.56] | [0.41-1.7] | |
| Uninsured | –1.46* | 0.23*** | 0.33 | 0.21*** | 0.6 |
| (0.75) | (0.11) | (0.24) | (0.11) | (0.34) | |
| Education level (some educationa) | |||||
| GED and HS | [–2.96 to 0.04] | [0.09-0.51] | [0.08-1.41] | [0.07-0.6] | [0.17-1.87] |
| –0.39 | 0.6 | 0.78 | 0.43 | 0.70 | |
| (0.6) | (0.4) | (0.49) | (0.22) | (0.34) | |
| [–1.5 to 0.72] | [0.17-2.4] | [0.21-2.77] | [0.16-1.19] | [0.26-1.85] | |
| Baccalaureate | –0.21 | 0.60 | 1.05 | 0.41 | 0.53 |
| (0.6) | (0.42) | (0.71) | (0.28) | (0.30) | |
| [–1.47 to 0.9] | [0.15-2.40] | [0.28-4.04] | [0.10-1.51] | [0.17-1.6] | |
| Postbaccalaureate | –0.32 | 0.92 | 0.67 | 0.294** | 0.73 |
| (0.56) | (0.68) | (0.42) | (0.17) | (0.40) | |
| Marital status (marrieda) | |||||
| Widowed | [–1.4 to 0.8] | [0.21-4.0] | [0.19-2.34] | [0.091-0.95] | [0.24-2.19] |
| –0.76* | 0.36** | 0.83 | 0.59 | 0.55 | |
| (0.44) | (0.18) | (0.35) | (0.27) | (0.24) | |
| [–1.64 to 0.12] | [0.14-0.10] | [0.35-1.93] | [0.24-1.46] | [0.24-1.3] | |
| Divorced | 0.25 | 1.17 | 1.76 | 0.94 | 1.25 |
| (0.36) | (0.52) | (0.69) | (0.39) | (0.49) | |
| [–0.47 to 0.97] | [0.48-2.84] | [0.80-3.86] | [0.42-2.14] | [0.57-2.74] | |
| Never married | –0.27 | 1.15 | 1.49 | 0.59 | 0.56 |
| (0.547) | (0.7) | (1.10) | (0.29) | (0.38) | |
| [–1.4 to 0.83] | [0.4-3.7] | [0.34-6.57] | [0.22-1.57] | [0.14-2.2] | |
| Family income as % of poverty line (low incomea) | |||||
| Middle income | 0.46 | 1.35 | 1.42 | 2.06* | 1.11 |
| (0.33) | (0.47) | (0.51) | (0.75) | (0.31) | |
| [–0.19 to 1.11] | [0.68-2.70] | [0.69-2.91] | [0.1-4.3] | [0.62-2.33] | |
| High income | 0.15 | 1.01 | 1.02 | 1.95* | 0.81 |
| (0.37) | (0.44) | (0.44) | (0.76) | (0.26) | |
| Census regions (Northeasta) | |||||
| Midwest | [–0.60 to 0.89] | [0.43-2.39] | [0.43-2.43] | [0.81-4.3] | [0.43-1.54] |
| 0.02 | 1.18 | 1.16 | 0.31 | 1.008 | |
| (0.48) | (0.67) | (0.54) | (0.23) | (0.51) | |
| [–0.94 to 0.98] | [0.38-3.61] | [0.46-2.94] | [0.12-1.28] | [0.31-3.28] | |
| South | –0.17 | 1.06 | 1.59 | 0.28** | 0.79 |
| (0.45) | (0.57) | (0.65) | (0.16) | (0.43) | |
| [–1.08 to 0.73] | [0.36-3.13] | [0.70-3.51] | [0.09-0.88] | [0.27-2.33] | |
| West | –0.79 | 0.45 | 0.82 | 0.185** | 0.71 |
| (0.60) | (0.27) | (0.38) | (0.12) | (0.47) | |
| [–1.91 to 0.41] | [0.14-1.46] | [0.33-2.08] | [0.049-0.70] | [0.19-2.69] | |
| Woman’s age | 0.03** | 1.053*** | 1.04** | 1.003 | 1.01 |
| (0.02) | (0.02) | (0.02) | (0.018) | (0.017) | |
| [0.002-0.062] | [1.02-1.09] | [1.003-1.08] | [0.97-1.04] | [0.98-1.05] | |
| No. of comorbidities | –0.09 | 0.772** | 0.96 | 1.056 | 0.85 |
| (0.092) | (0.08) | (0.10) | (0.103) | (0.09) | |
| [–0.27 to 0.09] | [0.63-0.95] | [0.78-1.19] | [0.87-1.28] | [0.69-1.05] | |
| Constant cut1 | — | 0.47 | 1.04 | 0.0108*** | 0.074** |
| — | (0.64) | (1.45) | (0.016) | (0.094) | |
| [0.03-6.97] | [0.07-16.9] | [0.001-0.19] | [0.006-0.94] | ||
| Constant cut2 | — | 2.73 | 5.15 | 0.12 | 0.37 |
| — | (3.62) | (7.29) | (0.16) | (0.45) | |
| [0.19-38.50] | [0.30-87.11] | [0.007-1.86] | [0.03-4.32] | ||
| Constant | 9.15*** | ||||
| (1.15) | |||||
| [6.86-11.4] | |||||
| Observations | 293 | 293 | 293 | 293 | 293 |
| R 2 | 0.097 | ||||
| F statistics | 2.19*** | 2.76*** | 1.92** | 1.67* | 2.47*** |
| Design df | 62 | 62 | 62 | 62 | 62 |
| No. of primary sampling unit | 194 | 194 | 194 | 194 | 194 |
| No. of strata | 132 | 132 | 132 | 132 | 132 |
| No. of population | 3 110 390 | 3 110 390 | 3 110 390 | 3 110 390 | 3 110 390 |
Note. Standard errors in parentheses, with significance noted as *P < .1. **P < .05. ***P < .01. Odds ratios are reported for all ordered logit models and confidence interval is reported in the square brackets. OLS = ordinary least squares; MEPS = Medical Expenditure Panel Survey; OL = ordered logit; GED = General Education Development; HS = high school.
Indicates the excluded categories.
From the ordered logistic regressions that use the individual CAHPS questions as the dependent variables, race/ethnicity is statistically significant in 3 of the patient-provider communication regressions after controlling for other variables of influence. For non-Hispanic blacks, the odds that providers will always respond respectfully versus usually or sometimes/never are 0.60 times lower than for non-Hispanic whites. There was no statistically significant difference between Hispanics and non-Hispanic whites in perceptions of being treated with respect. For non-Hispanic blacks, the odds that providers always explain things in a way that the patient understands versus usually or sometimes/never are 0.64 times lower than for non-Hispanic whites. There was no statistically significant difference between Hispanics and non-Hispanic whites in perceptions that providers always explained so that they could understand. For Hispanics, the odds that providers always spend adequate time interacting with them versus usually or sometimes/never are 0.19 times lower than for non-Hispanic whites. Also note that the variable Hispanic is marginally significant in the explain regression and non-Hispanic black is marginally significant in the spend time regression.
Breast cancer survivors who are uninsured or covered by public insurance have odds of always being treated with respect versus usually or sometimes/never that are 0.23 and 0.41 times lower, respectively, than privately insured survivors. In addition, for uninsured survivors, the odds that providers always explain things in a way that they understand versus usually or sometimes/never are 0.21 times lower than for privately insured survivors. Residents of the South or West have odds providers always explain things in a way that they are understood versus usually or sometimes/never that are 0.28 and 0.185 times lower than residents of the North. For each year increase in age, the odds that providers always treat survivors with respect and always listen to them versus usually or sometimes/never are 1.053 and 1.04 times greater. However, for widowed women, the odds that they are always treated with respect are 0.359 times lower than for married women. For each additional comorbidity, the odds that providers always treat patients with respect versus usually or sometimes/never are 0.772 times lower.
Table 4 reports the OLS and ordered logistic regression results for quality of patient-provider information sharing using the composite and individual information sharing variables as the dependent variables. In the composite quality of patient-provider information sharing regression, the Hispanic ethnicity coefficient is positive and marginally significant (1.04, P = .076). Having a baccalaureate education or postbaccalaureate education are associated with lower composite information sharing scores than that scored for those with less than a high school education or those with GED/high school education (–1.66 [P = .031] and –1.683 [P = .0299] for baccalaureate and postbaccalaureate, respectively). The regression indicates a marginally significant and negative association between age and information sharing, with older age associated with lower composite information sharing scores (–0.041 [P = .061]).
Table 4.
OLS and Ordered Logistic Models: Quality of Provider Information Sharing—MEPS.
| Variables | (OLS) |
(OL) |
(OL) |
(OL) |
(OL) |
|---|---|---|---|---|---|
| Composite score | Follow-up | Side effect | Social effects | Lifestyle change | |
| Race/ethnicity (non-Hispanic whitesa) | |||||
| Non-Hispanic black | 0.33 | 1.09 | 1.53 | 1.24 | 1.44 |
| (0.48) | (0.57) | (0.65) | (0.51) | (0.65) | |
| [–0.63 to 1.30] | [0.38-3.11] | [0.65-3.59] | [0.55-2.83] | [0.58-3.59] | |
| Hispanics | 1.044* | 4.37 | 3.51** | 2.37 | 4.24** |
| (0.52) | (3.91) | (2.06) | (1.26) | (2.88) | |
| Health insurance (private insurancea) | |||||
| Public insurance | [0.76-2.09] | [0.72-26.5] | [1.07-11.5] | [0.81-6.89] | [1.08-16.68] |
| –0.61 | 0.91 | 1.003 | 1.53 | 1.08 | |
| (0.511) | (0.49) | (0.40) | (0.64) | (0.39) | |
| [–1.64 to 0.2] | [0.37-2.66] | [0.45-2.25] | [0.66-3.53] | [0.52-2.23] | |
| Uninsured | 0.336 | 0.78 | 0.82 | 0.87 | 3.11 |
| (0.85) | (0.94) | (0.85) | (0.83) | (2.62) | |
| Education level (some educationa) | |||||
| GED and HS | [–1.37 to 2.04] | [0.061-8.82] | [0.10-6.58] | [0.127-5.95] | [0.57-17.11] |
| –0.79 | 1.12 | 0.83 | 0.54 | 0.97 | |
| (0.63) | (0.70) | (0.41) | (0.34) | (0.53) | |
| [–2.06 to 0.48] | [0.31-3.97] | [0.31-2.26] | [0.15-1.92] | [0.32-2.92] | |
| Baccalaureate | –1.66** | 0.66 | 0.56 | 0.27* | 0.305* |
| (0.76) | (0.47) | (0.36) | (0.2) | (0.1) | |
| [–3.18 to –0.13] | [0.16-2.8] | [0.15-2.08] | [0.06-1.20] | [0.08-1.14] | |
| Postbaccalaureate | –1.68** | 0.41 | 0.38 | 0.145** | 0.52 |
| (0.82) | (0.32) | (0.26) | (0.11) | (0.36) | |
| Marital status (marrieda) | |||||
| Widowed | [–3.32 to –0.05] | [0.09-1.95] | [0.09-1.49] | [0.02-0.7] | [0.13-2.12] |
| 0.15 | 0.71 | 0.89 | 0.93 | 2.05 | |
| (0.55) | (0.34) | (0.47) | (0.37) | (0.92) | |
| [–0.94 to 1.25] | [0.27-1.87] | [0.31-2.57] | [0.42-2.06] | [0.82-5.09] | |
| Divorced | 0.25 | 0.96 | 0.81 | 1.71 | 2.412** |
| (0.52) | (0.51) | (0.42) | (0.74) | (1.04) | |
| [–0.79 to 1.30] | [0.33-2.81] | [0.29-2.29] | [0.71-4.08] | [1.01-5.76] | |
| Never married | –0.01 | 3.04 | 0.95 | 0.64 | 0.81 |
| (0.58) | (2.52) | (0.52) | (0.42) | (0.46) | |
| Family income as % of poverty line (low incomea) | |||||
| Middle income | [–1.26 to 1.07] | [0.57-16.2] | [0.31-2.87] | [0.17-2.41] | [0.26-2.56] |
| 0.37 | 0.99 | 0.81 | 0.94 | 1.36 | |
| (0.45) | (0.42) | (0.34) | (0.36) | (0.50) | |
| [–0.54 to 1.28] | [0.43-2.30] | [0.42-1.91] | [0.438-2.017] | [0.64-2.87] | |
| High income | 0.73 | 2.07 | 1.6 | 1.626 | 2.54** |
| (0.52) | (1.02) | (0.76) | (0.694) | (1.05) | |
| Census regions (Northeasta) | |||||
| Midwest | [–0.32 to 1.77] | [0.76-5.51] | [0.60-4.18] | [0.69-3.84] | [1.09-5.88] |
| 0.03 | 1.10 | 0.75 | 1.03 | 1.01 | |
| (0.55) | (0.65) | (0.35) | (0.41) | (0.61) | |
| [–1.08 to 1.15] | [0.33-3.63] | [0.29-1.92] | [0.39-2.73] | [0.29-3.44] | |
| South | 0.41 | 1.01 | 1.57 | 1.71 | 1.76 |
| (0.46) | (0.53) | (0.63) | (0.73) | (0.91) | |
| [–0.52 to 1.34] | [0.35-2.92] | [0.7-3.52] | [0.73-4.04] | [0.63-4.97] | |
| West | 0.39 | 1.15 | 1.28 | 0.74 | 1.43 |
| (0.63) | (0.78) | (0.72) | (0.45) | (0.84) | |
| [–0.88 to 1.67] | [0.29-4.47] | [0.41-3.99] | [0.22-2.52] | [0.44-4.65] | |
| Age, y | –0.041* | 0.99 | 0.959* | 0.98 | 0.95*** |
| (0.0216) | (0.02) | (0.021) | (0.02) | (0.019) | |
| [–0.0843-0.00] | [0.95-1.03] | [0.92-1.002] | [0.94-1.02] | [0.91-0.99] | |
| No. of comorbidities | 0.001 | 1.03 | 1.01 | 1.06 | 1.11 |
| (0.14) | (0.13) | (0.12) | (0.12) | (0.14) | |
| [–0.26 to 0.28] | [0.71-1.3] | [0.8-1.27] | [0.85-1.32] | [0.87-1.42] | |
| Constant cut1 | — | 0.016** | 0.013*** | 0.06* | 0.02*** |
| — | (0.026) | (0.019) | (0.095) | (0.03) | |
| [0.001-0.42] | [0.001-0.27] | [0.003-1.46] | [0.001-0.2] | ||
| Constant cut2 | — | 0.17 | 0.0552* | 0.19 | 0.10 |
| — | (0.28) | (0.08) | (0.3) | (0.14) | |
| [0.01-4.5] | [0.002-1.17] | [0.01-4.34] | [0.01-1.62] | ||
| Constant | 12.35*** | ||||
| (1.64) | |||||
| [9.05-15.6] | |||||
| Observations | 239 | 232 | 224 | 216 | 225 |
| R 2 | 0.10 | ||||
| F | 3.14*** | 1.66* | 1.93** | 1.28 | 2.28*** |
| Design df | 49 | 47 | 45 | 44 | 43 |
| No. of primary sampling unit | 166 | 161 | 158 | 157 | 157 |
| No. of strata | 117 | 114 | 113 | 113 | 114 |
| Number of population | 2 648 006 | 2 566 072 | 2 448 017 | 2 378 417 | 2 457 290 |
Note. Standard errors in parentheses, with significance noted as *P < .1. **P < .05. ***P < .01. Odds ratios are reported for all ordered logit models and confidence interval is reported in the square brackets. OLS = ordinary least squares; MEPS = Medical Expenditure Panel Survey; OL = ordered logit; GED = General Education Development; HS = high school.
Indicates the excluded categories.
From the ordered logistic regressions that use the individual quality of patient-provider information sharing questions as the dependent variables, Hispanic ethnicity is statistically significant in 2 of the 4 patient-provider information sharing strategies. For Hispanics, the odds their provider discusses in detail the long-term side effects of their treatment versus briefly discusses or doesn’t discuss are 3.51 times greater than for non-Hispanic whites. Similarly, for Hispanics, the odds their provider discusses in detail the lifestyle changes related to their cancer versus briefly discusses or doesn’t discuss are 4.24 times higher than for non-Hispanic whites. There was no statistically significant difference between non-Hispanic blacks and non-Hispanic whites in perceptions of whether providers always discussed side effects and always discussed lifestyle changes.
Health insurance coverage was not a statistically significant variable in any of the quality of patient-provider information sharing regressions. For those with postbaccalaureate education, the odds that their provider discussed in detail emotional and social needs related to their cancer versus briefly discussed or didn’t discuss were 0.145 times lower than for those with less than a high school education or GED. Those divorced had odds their provider explained in detail the lifestyle changes related to their cancer versus briefly discussed or didn’t discuss that were 2.41 times higher than those who were married. Also interesting, for survivors with high incomes, the odds their provider discussed in detail the necessary lifestyle changes associated with their treatment versus briefly discussed or didn’t discuss were 2.54 times higher than for those with low income. For each year increase in age, the odds that a provider would discuss in detail needed lifestyle changes versus briefly discuss or didn’t discuss were 0.95 times lower.
Discussion
To our knowledge, no previous research has used a national data sample to examine differences in patient-provider communication that are experienced by ethnically diverse breast cancer patients. Studies have examined patient-provider communication and patient outcomes. For example, there have been regional studies that have used CAHPS measures to understand quality of follow-up cancer care.16 And we were able to find one statewide study that explored breast cancer adherence among low-income women with breast cancer and its relationship to CAHPS measures.17 In one national study, researchers explored the role of obesity in influencing physician-patient communication using CAHPS measures.11 Our findings provide unique insights regarding specific characteristics of patient-provider communication that are differently experienced by breast cancer patients who are of different racial/ethnic backgrounds, recognizing that their experiences have implications for breast cancer treatment and mortality outcomes.
Our findings confirm our central hypothesis that quality of patient-provider communication with breast cancer patients varies by race/ethnicity, examining indicators of statistical significance at the .05 level or better. These differences occur for specific dimensions of patient-provider communication, derived from the CAHPS measures and the quality of information sharing measures. Specifically, in the regression of whether patients perceived they were treated with respect, non-Hispanic blacks were significantly less likely than non-Hispanic whites to perceive they were always treated with respect. There was no statistically significant difference between Hispanics and non-Hispanic whites in perceptions of being treated with respect. Thus, the regression indicates that among the 3 ethnic/racial groups, non-Hispanic blacks were least likely to perceive they were always treated with respect.
In the regression of whether patients perceived providers explained so that you could understand, non-Hispanic blacks were significantly less likely than non-Hispanic whites to perceive providers always explained so that they understood. There was no statistically significant difference between Hispanics and non-Hispanic whites in perceptions that providers always explained so that they could understand. Again, non-Hispanic blacks were least likely to perceive that they always received this form of communication.
In the provider discussed side effects and provider discussed lifestyle changes regressions, Hispanics were significantly more likely than non-Hispanic whites to perceive that providers always discussed these concerns. There was no statistically significant difference between non-Hispanic blacks and non-Hispanic whites in perceptions of whether providers always discussed side effects and always discussed lifestyle changes. In these regressions, non-Hispanic blacks and non-Hispanic whites were less likely to always receive these forms of communication.
Altogether, we find that in 4 of the 8 regression models of patient-provider communication (whether the patient perceived respect, provider explained so that you could understand, provider discussed side effects, and provider discussed lifestyle changes), non-Hispanic blacks had lower odds of receiving detailed communication than Hispanics. In 2 of the 8 regression models of patient-provider communication (whether the patient perceived respect and provider explained so that you could understand), non-Hispanic blacks had lower odds of always receiving detailed communication than did non-Hispanic whites. In only 1 regression, provider spent adequate time with you, Hispanics had lower odds of always receiving adequate time than non-Hispanic whites and non-Hispanic blacks. No regression model indicated that non-Hispanic blacks had higher odds of receiving detailed patient-provider communication than non-Hispanic whites. To some extent, these racial/ethnic gaps in patient-provider communication correspond with the racial/ethnic disparities in mortality. Non-Hispanic blacks face the highest mortality rates from breast cancer and also the greatest patient-provider communication deficit. While our central hypothesis predicted that Hispanic patients would receive the most patient-provider communication, but this was not always the case.
Equally important to note, in 3 of the 8 regressions (whether providers listened carefully to them, discussed need for regular follow-up care and monitoring after completing treatment, and discussed emotional or social needs related to cancer), there were no statistically significant racial/ethnic differences in patient-provider communication.
Knowing the specific communication areas where there are racial/ethnic gaps is informative in understanding processes that are associated with mortality outcomes. We know from the literature that women who are likely to delay follow-up care have reported that dissatisfaction with communication of results and perceptions of being treated disrespectfully are root causes of delays.18 The probability of breast cancer survival decreases with delays in care. The research results reported in this article indicate that non-Hispanic black women are least likely to always experience respectful communication and communication at a level that they do not understand. Linking these findings with the existing literature provides additional insights about the relatively higher mortality rates experienced by non-Hispanic black women compared with rates experienced by Hispanic and non-Hispanic white women. Together, the findings predict that because non-Hispanic black women are least likely to always receive respectful and understandable communication, they are more likely to delay follow-up and to die from breast cancer.
From a survey perspective, another interesting contrast in our findings pertains to the difference in our results as we contrast the regressions using the MEPS CAHPS indicators versus the quality of information sharing measures. In the quality of information sharing regressions, the differences identified relate to the higher odds of greater communication for Hispanics, compared with non-Hispanic whites and non-Hispanic blacks. Using the MEPS CAHPS measures, in 2 cases non-Hispanic blacks have lower odds of always receiving high levels of patient-provider communication and in one case Hispanics receive lower odds of always receiving high levels of patient-provider communication. It is unclear why ethnic minorities are found to receive equal or lower communication as whites when the MEPS CAHPS indicators are used, while ethnic minorities are found to have equal or more patient-provider communication compared with whites in the quality of provider information sharing regressions. This contrast is particularly striking for Hispanics who are less likely than non-Hispanic whites to receive adequate time (a MEPS CAHPS indicator) and more likely to receive explanations that are detailed to the point where the patient understands regarding side effects and lifestyle changes (quality of provider information sharing indicators). Qualitative findings from Ashing-Giwa et al19 indicate that Hispanic patients do not think providers provide adequate time, particularly in circumstances when patients speak limited English or do not think they have the authority to ask their providers questions to help them better understand their disease. Further investigation of this contrast is needed.
In addition to the statistically significant association between race/ethnicity and patient-provider communication, health insurance coverage also had an association with quality of patient-provider communication. Having public insurance was associated with a 0.41 lower odds of being treated with respect. Uninsured breast cancer patients had a 0.23 lower odds of being treated with respect and a 0.21 lower odds that the provider explained things in detail so that they understood. While it is widely perceived that insurance opens the door to health care access, it is a concern that the quality of communication received after obtaining access to the door varies based on the type of insurance held. Indeed, the analysis reported herein indicates that publicly insured patients receive less respect than patients who are uninsured. This also is an area for further inquiry.
Conclusions and Implications
This study enhances our understanding of the ways in which patient-provider communication is associated with the quality of care for breast cancer patients. It leads one to question whether the relatively higher health outcomes, that is, lower mortality rates, for Hispanic breast cancer patients compared with non-Hispanic white and non-Hispanic black patients are in part due to their receipt of higher quality patient-provider communication. This question is generated by an observation from our regression models indicating that Hispanic patients were more likely to receive greater communication. This occurred in 4 of 8 regressions when comparing non-Hispanic blacks and Hispanics and in 2 of the 8 regressions when comparing non-Hispanic whites and Hispanics. This study also leads one to question whether the association of non-Hispanic blacks with the highest breast cancer mortality rates is related to their receipt of less provider communication. Non-Hispanic blacks experienced the greatest patient-provider communication deficit; non-Hispanic blacks were never more likely than non-Hispanic whites and only once in 8 regressions more likely to receive greater communication than Hispanics.
This research suggests that interventions directed toward enhancing the quality of patient-provider communication may reduce disparities in breast cancer outcomes. Such interventions might include cultural competency training for preprofessionals and for practitioners who have achieved provider status. For example, such training might include strategies to assess whether the provider has spent adequate time interacting with breast cancer patients of different racial/ethnic backgrounds. Gaps in communication may present circumstances where some patient concerns may not be addressed. Specific areas for additional communication and patient-centered communication with non-Hispanic black breast cancer patients are respectful communication, explaining in detail to a point where the patient understands, and explaining side effects and lifestyle or health recommendations. Research has shown that such training has led to increases in the length of time doctors spend with patients and effects that last for about 5 years.20,21
Another possible intervention strategy to enhance patient-provider communication is patient activation. Because of their cultural backgrounds, ethnic minority patients have been noted to be less verbally expressive and less assertive in demanding that providers deliver the most effective communication meeting their needs.22 Thus, patient-provider communication time periods have been noted to be shorter and focused on what the provider wants to communicate, rather than to reflect patient-centered communication.21 Patient activation interventions would focus on training patients to ask questions of providers and seek information that is important to them.21
This article has provided new insights about racial/ethnic differences in patient-provider communication with breast cancer patients, and how that communication can be enhanced. It also illustrates that minority breast cancer patients are not always disadvantaged with respect to patient-provider communication, specifically Hispanic patients who have higher odds of detailed patient-provider communication than non-Hispanic white patients in 2 of the 8 analyses of communication.
One limitation of our analysis was the lack of detailed provider supply-side variables, such as site of delivery of breast care services. Another limitation was the small sample size of Hispanics. Although a national database was used in the analysis, our focus on the breast cancer sample resulted in having a small sample size for analysis. The concern was partially addressed by applying sample weights, generating population estimates, and performing weighted regression analysis. Nonetheless, results from the subgroup analyses reported in Tables 1 and 2 might not be accurate due to the small sample size for Hispanics.
Because we do not have a measure of cultural differences in expectations of physicians, our regression coefficients for race/ethnicity in the patient-provider communication models may jointly reflect differences in the extent of communication by race/ethnicity and differences in expectations by race/ethnicity. That is because culture may influence how provider communication is perceived. Three factors that may influence perceptions of communication are the willingness to accept unequal power relations, a present versus future orientation, and communication in an explicit versus implicit way.22 Patient submissiveness is more likely for Latino patients. Non-Hispanic blacks have been found to be more present oriented. Hispanics prefer implicit communication that is less direct, with more meaning found in what is not said and warm personal interactions.23
This research poses an important implication for future research that explores how patient-provider communication is related to patient outcomes. As we find that the quality of patient-provider communication varies by race/ethnicity, future research should consider the use of interaction terms of race/ethnicity and communication scores to explore whether the impact of patient-provider communication on outcomes varies by race/ethnicity.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Centers for Disease Control and Prevention. Breast cancer rates by race and ethnicity. http://www.cdc.gov/cancer/breast/statistics/race.htm. Published August 20, 2015. Updated June 15, 2016. Accessed July 7, 2017.
- 2. Hunt BR, Whitman S, Hurlbert MS. Increasing black: white disparities in breast cancer mortality in the 50 largest cities in the United States. Cancer Epidemiol. 2014;38(2):118-123. [DOI] [PubMed] [Google Scholar]
- 3. Susan G. The who, what, where, when and sometimes, why. http://ww5.komen.org/BreastCancer/DisparitiesInBreastCancerScreening.html. Updated June 6, 2017. Accessed July 7, 2017.
- 4. American Cancer Society. Breast Cancer Facts & Figures 2013-2014. Atlanta, GA: American Cancer Society; 2013. [Google Scholar]
- 5. Chen L, Li CI. Racial disparities in breast cancer diagnosis and treatment by hormone receptor and her2 status. Cancer Epidemiol Biomarkers Prev. 2015;24(11):1666-1672. doi: 10.1158/1055-9965.EPI-15-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wheeler SB, Reeder-Hayes KE, Carey LA. Disparities in breast cancer treatment and outcomes: biological, social, and health system determinants and opportunities for research. Oncologist. 2013;18:986-993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Daly B, Olopade OI. A perfect storm: how tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J Clin. 2015;65(3):221-238. [DOI] [PubMed] [Google Scholar]
- 8. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. National Health Interview Survey: The Principal Source of Information on the Health of the US Population. Hyattsville, MD: National Center for Health Statistics; http://www.cdc.gov/nchs/data/nhis/brochure2010january.pdf. Published 2010. Accessed July 7, 2017. [Google Scholar]
- 9. Ezzati-Rice TM, Rohde F, Greenblatt J. Sample design of the Medical Expenditure Panel Survey household component, 1998–2007. Rockville, MD: Agency for Healthcare Research and Quality; http://www.meps.ahrq.gov/mepsweb/data_files/publications/mr22/mr22.shtml. Methodology report no. 22. Published March 2008. Accessed July 7, 2017. [Google Scholar]
- 10. Greene WH. LIMDEP 7.0. Bellport, NY: Econometric Software, Inc; 1995. [Google Scholar]
- 11. Richard P, Ferguson C, Lara AS, Leonard J, Younis M. Disparities in physician-patient communication by obesity status. Inquiry. 2014;51. doi: 10.1177/0046958014557012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hargraves JL, Hays RD, Cleary PD. Psychometric properties of the Consumer Assessment of Health Plans Study (CAHPS) 2.0 adult core survey. Health Serv Res. 2003;38:1509-1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Manfredi C, Kaiser K, Matthews AK, Johnson TP. Are racial differences in patient-physician cancer communication and information explained by background, predisposing, and enabling factors? J Health Commun. 2010;15(3):272-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: disparities in information-giving and affective behaviors. Patient Educ Couns. 2006;62:355-360. [DOI] [PubMed] [Google Scholar]
- 15. Cleary PD, McNeil BJ. Patient satisfaction as an indicator of quality care. Inquiry. 1988;25(1):25-36. [PubMed] [Google Scholar]
- 16. Arora NK, Reeve BB, Hays RD, Clauser SB, Oakley-Girvan I. Assessment of quality of cancer-related follow-up care from the cancer survivor’s perspective. J Clin Oncol. 2011;29:280-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liu Y, Malin JL, Diamant AL, Thind A, Maly RC. Adherence to adjuvant hormone therapy in low-income women with breast cancer: the role of provider-patient communication. Breast Cancer Res Treat. 2013;137(3):829-836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Allen JD, Shelton RC, Harden E, Goldman RE. Follow-up of abnormal screening mammograms among low-income ethnically diverse women: findings from a qualitative study. Patient Educ Couns. 2008;72:283-292. [DOI] [PubMed] [Google Scholar]
- 19. Ashing-Giwa KT, Padilla GV, Bohorquez DE, Tejero JS, Garcia M. Understanding the breast cancer experience of Latina women. J Psychosoc Oncol. 2006;24(3):19-52. [DOI] [PubMed] [Google Scholar]
- 20. Schouten B, Meeuwesen L, Harmsen HA. The impact of an intervention in intercultural communication on doctor-patient interaction in the Netherlands. Patient Educ Couns. 2005;58(3):288-295. [DOI] [PubMed] [Google Scholar]
- 21. Institute of Medicine, Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Patient-provider communication: the effect of race and ethnicity on process and outcomes of healthcare. In: Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. https://www.ncbi.nlm.nih.gov/books/NBK220354/. Accessed July 7, 2017. [PubMed] [Google Scholar]
- 22. Schouten B, Meeuwesen L. Cultural differences in medical communication: a review of the literature. Patient Educ Couns. 2006;64:21-34. [DOI] [PubMed] [Google Scholar]
- 23. Gao G, Burke N, Somkin CP, Pasick R. Considering culture in physician-patient communication during colorectal cancer screening. Qual Health Res. 2009;19(6):778-789. [DOI] [PMC free article] [PubMed] [Google Scholar]