Abstract
Mucosal-associated invariant T (MAIT) cells are an abundant class of innate T cells restricted by the MHC I-related molecule MR1. MAIT cells can recognize bacterially-derived metabolic intermediates from the riboflavin pathway presented by MR1 and are postulated to play a role in innate antibacterial immunity through production of cytokines and direct bacterial killing. MR1 tetramers, typically stabilized by the adduct of 5-amino-6-D-ribitylaminouracil (5-A-RU) and methylglyoxal (MeG), are important tools for the study of MAIT cells. A long-standing problem with 5-A-RU is that it is unstable upon storage. Herein we report an efficient synthetic approach to the HCl salt of this ligand, which has improved stability during storage. We also show that synthetic 5-A-RU•HCl produced by this method may be used in protocols for the stimulation of human MAIT cells and production of both human and mouse MR1 tetramers for MAIT cell identification.
Introduction
The study of mucosal-associated invariant T cells (MAIT cells) represents an intriguing frontier in immunology [1–10]. MAIT cells are prevalent within the human peripheral T cell compartment, gut, lung and liver with large inter-individual variability associated with age and disease states, composing as little as <1% to >10% of peripheral blood CD3+ cells [11–14]. Despite such abundance in human donors, their specific roles during the innate immune response are incompletely understood. MAIT cells canonically express a semi-invariant T-cell receptor (TCR) composed of TRAV1-2-TRAJ33 α-chain pairing predominantly with TRBV6 and TRBV20 β-chains [15–17]. Upon activation, MAIT cells can produce granzyme B, interferon-γ, tumor necrosis factor-α, interleukin-17, and kill bacterially infected cells [11, 18, 19]. There is mounting evidence that MAIT cells may play a key role in the detection and response to infectious pathogens, including Mycobacterium tuberculosis (Mtb) [12, 20–22].
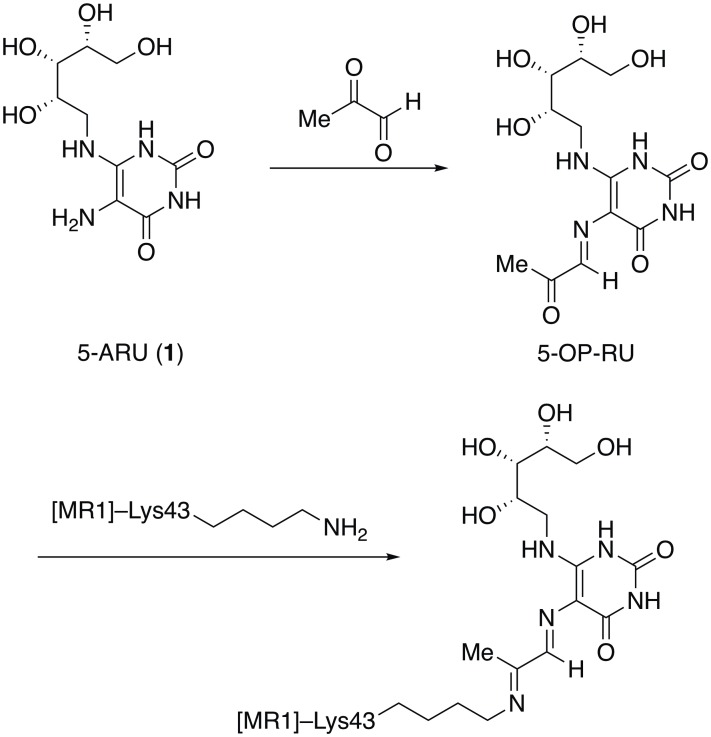
An enabling advance in MAIT cell biology was the discovery that the MAIT cell TCR recognizes microbially-derived vitamin B metabolites presented by the major histocompatibility (MHC)-related protein MR1 [7, 23]. A number of stabilizing ligands were initially discovered, some of which were reported to activate MAIT cells, while others (notably 6-formylpterin) bound tightly to MR1 but had minimal stimulatory activity [16, 24]. In addition to providing a molecular basis for the detection of MAIT cells, these observations also enabled the construction of antigen-loaded MR1 tetramers, first using reduced 6-hydroxymethyl-8-D-ribityllumazine as a stabilizing ligand [16]. In later work, intermediates for riboflavin biosynthesis such as 5-amino-6-D-ribitylaminouracil (5-A-RU, 1, Fig 1), modified in situ by methylglyoxal (MeG), were discovered to be potent activators of MAIT cells and also allowed generation of MR1 tetramers [24]. In the latter case, Corbett et al. demonstrated that 5-A-RU forms a Schiff base adduct 5-OP-RU with MeG, thus presenting a highly activated ketone to Lys43 of MR1 for covalent attachment, which stabilizes MR1 and permits the formation of stable complexes [24]. The resulting tetramers have proved capable of binding MAIT cells directly and as such have emerged as the gold standard for identification of MAIT cells, replacing less specific approaches such as staining for TRAV1-2 in combination with the C-type lectin receptor, CD161.
Fig 1. Chemical structures.
Structures of 5-A-RU (1), the Schiff base it forms with methylglyoxal (5-OP-RU), and the covalent attachment of the latter to MR1.
5-A-RU has been known for many years due to its role as an intermediate in the biosynthesis of riboflavin [25, 26]. Accordingly, syntheses of 5-A-RU and congeners have been reported since the late 1950s, with key early advances registered by Plaut [27, 28], Katagiri [29], Masuda [30], and Wood [31–33]. These procedures were largely adapted by later investigators [34–37]; in addition, an enzymatic approach has also been reported [38]. Consistently, these investigators have remarked on the difficulty of working with 5-A-RU once it has been synthesized, citing stability problems that necessitated some combination of avoiding light, air, or concentrated solutions. In some cases, these problems were minimized by directly using freshly prepared solutions of 5-A-RU in the intended subsequent reaction, but even this workaround has the disadvantage of needing to prepare 1 on each occasion of use. The specific nature of the instability of 1 has not been established, although it has been described as prone to oxidation [36]. We have confirmed that the material does decompose to unidentified byproducts when left for even a few hours (see below).
The use of 1 as a ligand for MR1 folding reactions requires the in situ reaction of 1 with MeG to afford the active species 5-OP-RU. Left standing, this initial Schiff base is known to cyclize to afford the corresponding lumazine [39]. In this situation, having a stable store of 5-A-RU is desirable, but the aforementioned stability problems complicate this approach. An alternative approach, published by Mak et al. when the present manuscript was in preparation, involves the preparation of solutions of 5-OP-RU in DMSO, which were reported to be stable [37].
In this paper, we report that the stability and convenience of 1 can be enhanced through the simple expedient of making and storing it as its HCl salt. In the course of this work, we combined the best features of existing syntheses of 1 into a practical route. Finally, we show that 1•HCl, when reacted with MeG, performs comparably to 5-OP-RU made by other routes as demonstrated by upregulation of the surface expression of MR1, activation of MAIT cells, and the construction of MR1 tetramers.
Materials and methods
Chemistry
The syntheses of (2R,3S,4S)-5-aminopentane-1,2,3,4-tetraol (2) [29], 6-chloro-5-nitropyrimidine-2,4(1H,3H)-dione (3b) [31, 40], and 5-nitro-6-(((2S,3S,4R)-2,3,4,5-tetrahydroxypentyl)amino)pyrimidine-2,4(1H,3H)-dione (4c) [31] were carried out by previously reported routes. They are included in Supporting Information S1 File along with full characterization of the intermediates.
5-Amino-6-D-ribitylaminouracil hydrochloride (1•HCl, 5-A-RU•HCl)
To a solution of 5-nitro-6-(((2S,3S,4R)-2,3,4,5-tetrahydroxypentyl)amino)-pyrimidine-2,4(1H,3H)-dione (4c, 0.327 mmol, 100 mg) in water (4 mL) was added 2 drops of 2N aqueous KOH followed by sodium hydrosulfite (1.96 mmol, 0.341 g). The light-yellow solution turned colorless within 20 minutes and a white precipitate formed; the reaction was monitored by HPLC-MS until starting material was consumed (ca. 1 hour). The mixture was purified via reverse phase chromatography and 0.18 mL of 1N HCl was added to the combined fractions containing product. Upon concentration, the title compound was obtained as a red tar, which solidified upon standing (70.0 mg, 69%). 1H NMR (400 MHz, D2O) δ 4.01 (ddd, J = 7.5, 6.0, 2.8 Hz, 1H), 3.87–3.77 (m, 2H), 3.76–3.71 (m, 1H), 3.71–3.64 (m, 2H), 3.56 (dd, J = 14.7, 7.5 Hz, 1H). 13C NMR (101 MHz, D2O) δ 160.9, 150.8, 150.4, 82.6, 72.2, 72.0, 70.3, 62.3, 44.5. HRMS (m/z): calculated for C9H17N4O6 ([M+H]+) 277.1143; found 277.1143.
MAIT cell activation assay
Human MR1 was sub-cloned from a plasmid expressing human MR1 (Origene) into retroviral vector MSCV-IRES-GFP-R1 (MIG-R1; addgene plasmid # 27490) [41]. C1R (ATCC) cells, a human B cell lymphoblastoid cell line lacking major-histocompatibility proteins, were transduced with this construct. GFP+MR1+ cells were isolated by fluorescence activated cell sorting and cultured in IMDM media (ATCC) 10% FBS for 72 hours to confluence prior to activation. Synthetic 5-A-RU•HCl was stored at 4°C in solid form until dissolving in sterile, distilled H2O and freezing at –80°C in 200 μM stock solutions (referred to here as 5-A-RU•H2O solutions). Stock solutions of 2 μM 5-A-RU•H2O and 50 μM MeG•H2O were prepared as needed for cell culture. C1R GFP MR1 cells were directly incubated with 2 μM 5-A-RU•H2O and 50 μM MeG•H2O for 15 hours at 37°C and stained with Zombie Red Viability dye (Biolegend) and PE MR1 antibody (26.5, Biolegend) for 30 minutes at 4°C, as previously reported [24]. Following Mak et al. [37], cryopreserved healthy donor peripheral blood mononuclear cells (PBMCs) were thawed and cultured in RPMI 1640 media (ATCC) 10% FBS and directly incubated with 2 μM 5-A-RU•H2O/50 μM MeG•H2O for 15 hours at 37°C. No toxicity to C1R GFP or PBMCs was observed with 5-A-RU or MeG alone, or in combination. PBMCs were stained with Zombie Red Viability stain, Alexa 700 CD3 antibody (UCHT1, Biolegend), APC CD161 antibody (DX12, BD), and PE MR1/5-OP-RU tetramer for 30 minutes at 4°C. Cells were permeabilized and fixed for 40 minutes at 4°C with FoxP3/Transcription factor Staining Buffer Set (eBioscience) and stained with FITC granzyme B (GB11, Biolegend) for 1 hour at 4°C. Blocking experiments were performed by incubating PBMCs directly with 5 μg/mL anti-MR1 antibody (26.5, Biolegend) for one hour prior to incubation with 5-A-RU/MeG. Human CD3/CD28 T cell activator Dynabeads (Gibco) were incubated with PBMCs for 15 hours at a 1:2 bead to cell ratio as a positive control for T cell activation. All cells were analyzed on a Fortessa Flow Cytometer (BD).
Tetramer formation
Production of MR1/5-OP-RU tetramers followed published methods with slight modifications [24]. We prepared an expression construct consisting of DNA coding for residues 1–280 of the mature human MR1 subunit followed by a Gly-Ser linker and the BirA substrate peptide 85 [42]; all codons were optimized for expression in E. coli, the synthetic gene was obtained from IDT (https://www.idtdna.com), and the insert was cloned into a pET derived vector developed in the NIH Tetramer Facility [43]. The MR1 subunit was expressed in BL21(DE3) cells and the inclusion bodies were washed and solubilized in freshly prepared 8M urea as described [43]. Folding of the MR1 subunit with human β2m, 5-A-RU, and MeG and subsequent purification followed published protocols [24]. Purified MR1/5-OP-RU was enzymatically biotinylated as described [43] and free biotin was removed by gel filtration chromatography. Tetramers were prepared with R-phycoerythrin (Prozyme, http://www.prozyme.com) as described [43].
Results and discussion
Chemistry
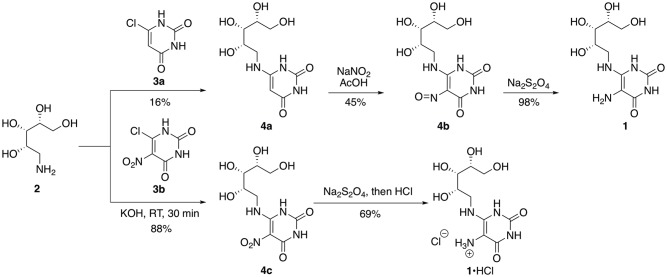
The synthesis of 1 requires (1) the preparation of ribitylamine, (2) attachment of ribitylamine to a uracil derivative, and (3) functional group conversions in the assembled compound to afford 1 (Fig 2). A satisfactory literature-based procedure for the conversion of (–)-ribose to ribitylamine via an intermediate oxime, which is then reduced, has been used in most reported syntheses of 5-A-RU [25, 29]. Two alternatives for the nucleophilic aromatic substitution (SNAr) reaction appear in the literature. The first is a reaction of amine 2 with 6-chloropyrimidine-2,4-dione 4a, followed by nitrosylation to afford 4b [25]. In general, material was stored as 4b and reduced immediately before the amine was needed. For example, amine 1 was prepared and used as a stock solution for the specific application of MR1 tetramer formation [24].
Fig 2. Synthetic routes to 5-A-RU 1 and its salt 1•HCl.
The conversion of 3a to 4b was originally reported to proceed in 50–70% yields for both the SNAr and nitrosylation steps [25]. We briefly examined a modification whereby the original SNAr conditions (neat, 95–110°C, 3 hours) were replaced by microwave conditions (180°C, 10 minutes), but in our hands the yields topped out at about 16% prior to nitrosylation. We were accordingly drawn to an alternative route initially reported by Cresswell and Wood [31], whereby the displacement was carried out on the more highly activated nitrouracil 3b [40], which afforded 4c smoothly in very high yield, was stable indefinitely, and could be used without additional purification.
The reduction of 4c proceeds smoothly using either Na2S2O4 [31, 33] or catalytic hydrogenation [35, 44–46] to afford 1 as reported. Although these procedures been reported in acidic media [32, 35], the isolation of the unstable amine as its salt as a means of stabilizing pure material has not been previously disclosed. Since doing so would remove potential nucleophilic or single-electron-transfer proclivities from the compound, we explored salt formation of material obtained from chromatographic purification of 1. Accordingly, addition of aqueous HCl to newly-chromatographed 1 afforded the corresponding HCl salt as a reddish solid. This material was amenable to full characterization and storage in the solid state (the NMR spectrum indicated minimal decomposition after 19 days of storage in D2O at room temperature without light protection or after 37 days in solid form at room temperature (wrapped in foil); see Supporting Information, S1 and S2 Figs). In comparison, we observed substantial decomposition to unknown byproducts in the NMR spectra of samples of neutral 1 kept in DMSO–d6 or D2O in as little as after one day of storage (Supporting Information, S3 and S4 Figs, respectively). We have prepared 1•HCl on 200 mg scale using this approach (50% yield on this scale).
Functional evaluation of synthetic 5-A-RU•HCl
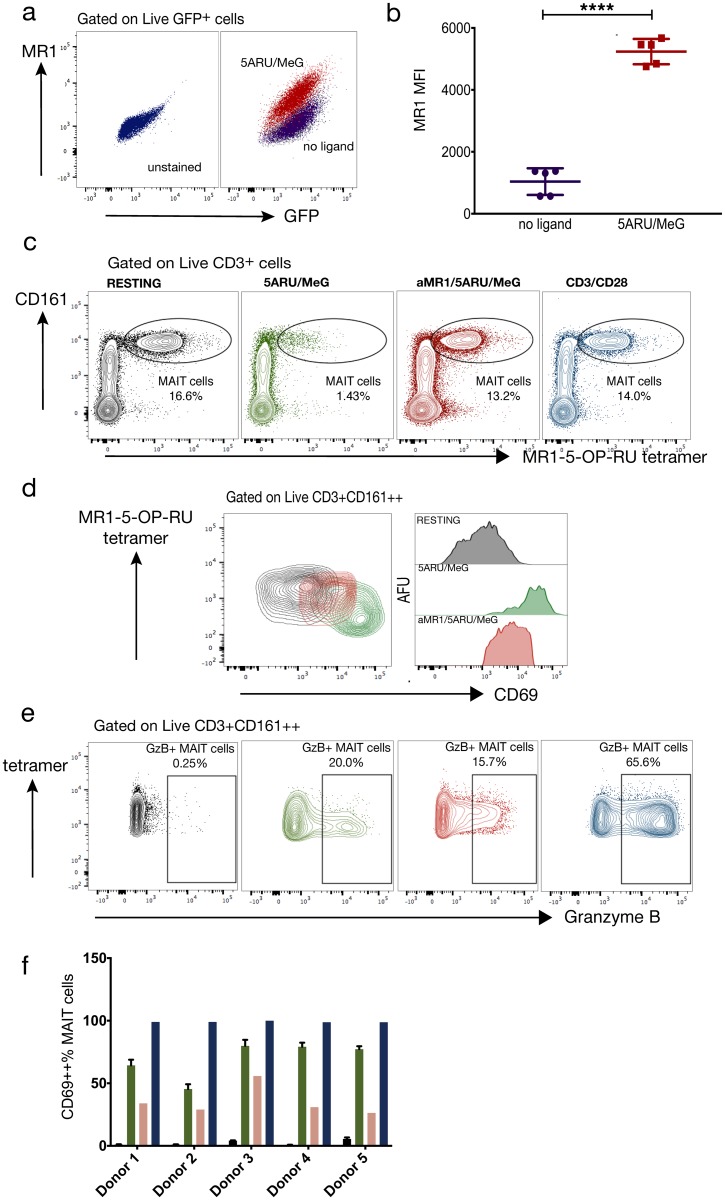
To functionally validate our synthetic 5-A-RU, we tested the compound for its ability to upregulate surface MR1 in C1R lymphoblastoid cells engineered to express human MR1, as previously reported [16]. Direct incubation with 2 μM 5-A-RU•H2O and 50 μM MeG•H2O strongly upregulated surface MR1 expression as measured by MR1 antibody staining and flow cytometry (Fig 3a and 3b).
Fig 3. Functional studies.
5-Amino-6-(D-ribitylamino)uracil (5-A-RU) reacted with methylglyoxal (MeG) upregulates MR1 and activates human mucosal-associated invariant T (MAIT) cells. (a, b) 2 μM 5-A-RU•H2O and 50 μM MeG•H2O were directly incubated with the human C1R GFP MR1 expressing cell line for 15 hours. MR1 mean fluorescence intensity (MFI) was compared to resting C1R GFP by unpaired t-test. Graphed values are five technical replicates from two independent experiments; violet = no ligand, red = 2 μM 5ARU/50 μM MeG. **** p<0.001 (c) Human MAIT cells identified by flow cytometry as Live CD3+ MR1 tetramer+ CD161++ cells after 15 hours under the following conditions: black = no ligand, green = 2 μM 5ARU/50 μM MeG, red = αMR1/2 μM 5ARU/50 μM, blue = anti-CD3/CD28. Color code also applies to (d)-(f). (d) Contour plots and histograms representing MR1-dependent CD69 expression of MAIT cells in one human donor (e) Contour plots of MAIT cell granzyme B production under the same conditions in panel (c). (f) Mean and SD of MR1-dependent MAIT cell CD69 expression in five human donors. Mean and SD for resting and 5-A-RU/MeG conditions represent two technical replicates per condition. SD: standard deviation.
We produced MR1/5-OP-RU tetramers from human MR1 and β2m folded with synthetic 5-A-RU•HCl and MeG using slight modifications of published protocols as described in the Methods section [24]. Fig 3c is a representative panel of human MR1/5-OP-RU tetramer staining of human peripheral blood mononuclear cells (PBMCs). The tetramer clearly identifies a distinct CD161 high cell population that comprised 16.6% of live CD3+ cells. In five healthy donors tested, the mean tetramer+CD161++% of T cells was 8.2% (Range: 3.05–16.6%). Greater than 88% of MR1 tetramer positive cells among T cells co-stained for Vα7.2 (range: 81–97%) whereas >50% of Vα7.2+ cells among T cells co-stained with tetramers (range: 21–84%) (Supporting Information, S5a Fig). Among CD3+CD161++ cells, we observed that >90% of tetramer+CD161++ T cells were identified by anti-Vα7.2 (range: 87–98%), whereas >80% of Vα7.2+CD161++ were identified by tetramers (range: 71–82%) (Supporting Information, S5 Fig). These data highlight the importance of using MR1 tetramers to identify human MAIT cells due to the presence of both Vα7.2 negative MR1-restricted cells as well as TRAV1-2 usage among naive αβ T cells [47, 48].
To determine whether synthetic 5-A-RU•HCl is able to activate MAIT cells, we employed a functional assay using human PBMCs as previously reported [37]. Although in vitro activation of MAIT cells was previously achieved using immortalized cell lines [16, 37, 47, 49, 50], sorted primary cells [11, 49, 50], bacteria/bacterial products [16, 21, 22, 37, 47, 49] or pan-T cell mitogen [12, 21] these assays are limited by allo-reactivity, ligand abundance/specificity, and often cannot easily be applied without additional manipulations of clinical samples. To simplify these approaches, it has been reasoned that MR1-expressing cells such as monocytes and B cells [49, 51] within the PBMC aliquot are abundant and could directly present synthetic ligand to MAIT cells without the need for culturing cell lines or performing cell-sorting [37, 52]. We directly incubated PBMCs with 2 μM 5-A-RU•H2O and 50 μM MeG•H2O and assayed upregulation of the T cell surface activation marker CD69. Synthetic 5-A-RU/MeG strongly induced MAIT TCR downregulation, accompanied by upregulation of CD69, and both responses were reversed by MR1 blockade, indicating their specificity for MR1 antigen presentation (Fig 3d). We note that Mak et al. obtained analogous activation using 1.26 nM solutions of pre-formed 5-OP-RU [37].
To confirm that TCR downregulation occurred with activation, we titrated the concentration of activation ligand and stained with tetramer or anti-Vα7.2 (Supporting Information, S5 Fig). We observed a dose-dependent loss of both surface markers, suggesting that MAIT cell activation results in TCR downregulation, as has been noted with other T cells [53]. While no toxicity was observed in PBMCs after incubation with 5-A-RU/MeG, we did observe dose-dependent depletion of MAIT cells from the tetramer positive gate, which is likely attributable to TCR downregulation and possibly activation-dependent cell death [48, 54].
We also observed upregulation of granzyme B in MAIT cells with ligand stimulation (Fig 3e). We next applied this assay to 5 independent healthy donors and observed MR1-dependent MAIT cell activation in all donors (Fig 3f). Our data confirm the functionality of the synthetic MR1 ligand precursor and establish a whole PBMC assay which can be applied to clinical samples to interrogate human MAIT cell function.
Conclusions
These data indicate that synthetic 5-A-RU•HCl is a stable replacement of the free base in a variety of protocols. Besides improving the convenience of using of using 1 in the study of riboflavin biosynthesis [38], this synthetic method can provide abundant amounts of this MR1 ligand precursor in stable form and has facilitated construction of human and mouse MR1/5-OP-RU tetramers now available through the NIH Tetramer Core facility (http://tetramer.yerkes.emory.edu/reagents/mr1). Further, the availability of this purified MR1 ligand precursor has enabled the development of an ex vivo MAIT cell activation assay using human PBMCs to directly interrogate inter-individual differences in MAIT cell function in an antigen-specific, MR1-dependent manner. Overall, the development of a reproducible synthesis of 1•HCl greatly enhances the practicality of using this ligand in the study of MAIT cell biology by increasing the stability of the reagent in a convenient solid form.
Supporting information
A sample of 1•HCl was dissolved in D2O and stored in an NMR tube without light protection. The 1H NMR spectra shown were collected at (a) 0 days, (b) 4 days, (c) 12 days and (d) 19 days.
(TIF)
A portion of sample of 1•HCl was taken at (a) 0 days, (b) 4 days, (c) 11 days and (d) 37 days, dissolved in D2O and analyzed by 1H NMR without light protection.
(TIF)
(a) 0 h, (b) 21 h, (c) 5 days, and (d) 23 days. Analyzed by 1H NMR without light protection.
(TIF)
(a) 0 h, (b) 21 h, (c) 5 days, and (d) 23 days. Analyzed by 1H NMR without light protection.
(TIF)
(a) Co-staining of resting human T cells using anti-Vα7.2 (left panel) or MR1/5-OP-RU tetramers (right panel). Results represent density plots from one donor and mean% +SD in three donors. SD: standard deviation. (b) Co-staining of resting human CD161++ T cells comparing tetramer+ cells among Vα7.2+CD161++ cells (left panel) to Vα7.2+cells among tetramer+CD161++ cells (right panel). Results represent density plots from one donor and mean% + SD in three donors. (c) Human MAIT cells were identified by flow cytometry using anti-Vα7.2 (left column) or MR1/5-OP-RU tetramers (right column) after 15 hours of rest or 5-A-RU dose titration (20 μM, 2 μM, 200 nM, 20 nM) + 50 μM MeG and demonstrate 5ARU dose-dependent TCR downregulation.
(TIF)
Includes synthesis details, copies of 1H and 13C NMR spectra of known compounds, and references for the experimental section.
(PDF)
Acknowledgments
We thank Phil Wong, Erika Ritter, and Matthew Adamow of the MSKCC Immune Monitoring Core for their expert consultation during the development of the MAIT cell activation assay. We also acknowledge UNC Department of Chemistry Mass Spectrometry Core Laboratory for HR-MS analysis.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Support from the National Institute of Allergy and Infectious Disease (niaid.nih.gov) is gratefully acknowledged: U19 AI11143, Carl Nathan, PI (supported work by KL, CKV, MSG, and JA); U19 AI111211, Henry M. Blumberg, PI (supported work by DLB, RAW, JDA); HHSN 272201300006C (supported work by DLB, RAW, JDA); and T32AI007613-18, Roy M. Gulick, PI (supported CKV). In addition support from the National Cancer Institute (nci.nih.gov) is acknowledged, through P30 CA008748 (supported AC and AR). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Treiner E, Duban L, Bahram S, Radosavljevic M, Wanner V, Tilloy F, et al. Selection of evolutionarily conserved mucosal-associated invariant T cells by MR1. Nature. 2003;422(6928):164–9. doi: 10.1038/nature01433 [DOI] [PubMed] [Google Scholar]
- 2.Treiner E, Duban L, Moura IC, Hansen T, Gilfillan S, Lantz O. Mucosal-associated invariant T (MAIT) cells: an evolutionarily conserved T cell subset. Microbes Infect. 2005;7(3):552–9. doi: 10.1016/j.micinf.2004.12.013 [DOI] [PubMed] [Google Scholar]
- 3.Treiner E, Lantz O. CD1d- and MR1-restricted invariant T cells: Of mice and men. Curr Opin Immunol. 2006;18(5):519–26. doi: 10.1016/j.coi.2006.07.001 [DOI] [PubMed] [Google Scholar]
- 4.Gapin L. Where do MAIT cells fit in the family of unconventional T cells? PLOS Biol. 2009;7(3):e70 doi: 10.1371/journal.pbio.1000070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le Bourhis L, Guerri L, Dusseaux M, Martin E, Soudais C, Lantz O. Mucosal-associated invariant T cells: unconventional development and function. Trends Immunol. 2011;32(5):212–8. doi: 10.1016/j.it.2011.02.005 [DOI] [PubMed] [Google Scholar]
- 6.Le Bourhis L, Mburu YK, Lantz O. MAIT cells, surveyors of a new class of antigen: development and functions. Curr Opin Immunol. 2013;25(2):174–80. doi: 10.1016/j.coi.2013.01.005 [DOI] [PubMed] [Google Scholar]
- 7.Birkinshaw RW, Kjer-Nielsen L, Eckle SBG, McCluskey J, Rossjohn J. MAITs, MR1 and vitamin B metabolites. Curr Opin Immunol. 2014;26:7–13. doi: 10.1016/j.coi.2013.09.007 [DOI] [PubMed] [Google Scholar]
- 8.Edholm E-S, Grayfer L, Robert J. Evolution of nonclassical MHC-dependent invariant T cells. Cell Mol Life Sci. 2014;71(24):4763–80. doi: 10.1007/s00018-014-1701-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gapin L. Check MAIT. J Immunol. 2014;192(10):4475–80. doi: 10.4049/jimmunol.1400119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gold MC, Napier RJ, Lewinsohn DM. MR1-restricted mucosal associated invariant T (MAIT) cells in the immune response to Mycobacterium tuberculosis. Immunol Rev. 2015;264(1):154–66. doi: 10.1111/imr.12271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dusseaux M, Martin E, Serriari N, Péguillet I, Premel V, Louis D, et al. Human MAIT cells are xenobiotic-resistant, tissue-targeted, CD161 IL-17–secreting T cells. Blood. 2011;117(4):1250 doi: 10.1182/blood-2010-08-303339 [DOI] [PubMed] [Google Scholar]
- 12.Kwon Y-S, Cho Y-N, Kim M-J, Jin H-M, Jung H-J, Kang J-H, et al. Mucosal-associated invariant T cells are numerically and functionally deficient in patients with mycobacterial infection and reflect disease activity. Tuberculosis. 2015;95(3):267–74. doi: 10.1016/j.tube.2015.03.004 [DOI] [PubMed] [Google Scholar]
- 13.Ussher JE, Bilton M, Attwod E, Shadwell J, Richardson R, de Lara C, et al. CD161++CD8+T cells, including the MAIT cell subset, are specifically activated by IL-12+IL-18 in a TCR-independent manner. European Journal of Immunology. 2014;44(1):195–203. doi: 10.1002/eji.201343509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keller AN, Corbett AJ, Wubben JM, McCluskey J, Rossjohn J. MAIT cells and MR1-antigen recognition. Current Opinion in Immunology. 2017;46(Supplement C):66–74. doi: 10.1016/j.coi.2017.04.002 [DOI] [PubMed] [Google Scholar]
- 15.Tilloy F, Treiner E, Park S-H, Garcia C, Lemonnier F, de la Salle H, et al. An Invariant T Cell Receptor α Chain Defines a Novel TAP-independent Major Histocompatibility Complex Class Ib–restricted α/β T Cell Subpopulation in Mammals. J Exp Med. 1999;189(12):1907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reantragoon R, Corbett AJ, Sakala IG, Gherardin NA, Furness JB, Chen Z, et al. Antigen-loaded MR1 tetramers define T cell receptor heterogeneity in mucosal-associated invariant T cells. J Exp Med. 2013;210(11):2305–20. doi: 10.1084/jem.20130958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eckle SBG, Birkinshaw RW, Kostenko L, Corbett AJ, McWilliam HEG, Reantragoon R, et al. A molecular basis underpinning the T cell receptor heterogeneity of mucosal-associated invariant T cells. J Exp Med. 2014;211(8):1585 doi: 10.1084/jem.20140484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Le Bourhis L, Dusseaux M, Bohineust A, Bessoles S, Martin E, Premel V, et al. MAIT Cells Detect and Efficiently Lyse Bacterially-Infected Epithelial Cells. PLoS Pathog. 2013;9(10):e1003681 doi: 10.1371/journal.ppat.1003681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kurioka A, Ussher JE, Cosgrove C, Clough C, Fergusson JR, Smith K, et al. MAIT cells are licensed through granzyme exchange to kill bacterially sensitized targets. Mucosal Immunol. 2015;8(2):429–40. doi: 10.1038/mi.2014.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gold MC, Cerri S, Smyk-Pearson S, Cansler ME, Vogt TM, Delepine J, et al. Human Mucosal Associated Invariant T Cells Detect Bacterially Infected Cells. PLOS Biol. 2010;8(6):e1000407 doi: 10.1371/journal.pbio.1000407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jiang J, Wang X, An H, Yang B, Cao Z, Liu Y, et al. Mucosal-associated Invariant T-Cell Function Is Modulated by Programmed Death-1 Signaling in Patients with Active Tuberculosis. Am J Respir Crit Care Med. 2014;190(3):329–39. doi: 10.1164/rccm.201401-0106OC [DOI] [PubMed] [Google Scholar]
- 22.Jiang J, Yang B, An H, Wang X, Liu Y, Cao Z, et al. Mucosal-associated invariant T cells from patients with tuberculosis exhibit impaired immune response. J Infect. 2016;72(3):338–52. doi: 10.1016/j.jinf.2015.11.010 [DOI] [PubMed] [Google Scholar]
- 23.Kjer-Nielsen L, Patel O, Corbett AJ, Le Nours J, Meehan B, Liu L, et al. MR1 presents microbial vitamin B metabolites to MAIT cells. Nature. 2012;491(7426):717–23. doi: 10.1038/nature11605 . [DOI] [PubMed] [Google Scholar]
- 24.Corbett AJ, Eckle SB, Birkinshaw RW, Liu L, Patel O, Mahony J, et al. T-cell activation by transitory neo-antigens derived from distinct microbial pathways. Nature. 2014;509(7500):361–5. doi: 10.1038/nature13160 . [DOI] [PubMed] [Google Scholar]
- 25.Plaut GWE, Harvey RA. [157] The enzymatic synthesis of riboflavin Methods in Enzymology. Volume 18, Part B: Academic Press; 1971. p. 515–38. [Google Scholar]
- 26.Bacher A, Eberhardt S, Eisenreich W, Fischer M, Herz S, Illarionov B, et al. Biosynthesis of riboflavin. Vitam Horm. 2001;61:1–49. [DOI] [PubMed] [Google Scholar]
- 27.Maley GF, Plaut GWE. Isolation, Synthesis, and Metabolic Properties of 6,7-Dimethyl-8-ribityllumazine. J Biol Chem. 1959;234(3):641–7. [PubMed] [Google Scholar]
- 28.Winestock CH, Plaut GWE. Synthesis and Properties of Certain Substituted Lumazines. J Org Chem. 1961;26(11):4456–62. doi: 10.1021/jo01069a063 [Google Scholar]
- 29.Katagiri H, Takeda I, Imai K. Synthesis of Riboflavin by Microorganisms. VII. The Enzymic Riboflavin Synthesis from 4-N-Ribitylamino-5-aminouracil. J Vitaminology. 1959;5(4):287–97. [DOI] [PubMed] [Google Scholar]
- 30.Masuda T, Kishi T, Asai M, Kuwada S. Application of Chromatography. XXXVII. Total Synthesis of 6,7-Dimethylribolumazine. Bull Chem Pharm Sci. 1959:361–5. [Google Scholar]
- 31.Cresswell RM, Wood HCS. 928. The biosynthesis of pteridines. Part I. The synthesis of riboflavin. J Chem Soc. 1960:4768–75. doi: 10.1039/JR9600004768 [Google Scholar]
- 32.Rowan T, Wood HCS. The biosynthesis of pteridines. Part V. The synthesis of riboflavin from pteridine precursors. J Chem Soc C. 1968:452 doi: 10.1039/j39680000452 [DOI] [PubMed] [Google Scholar]
- 33.Al-Hassan SS, Kulick RJ, Livingstone DB, Suckling CJ, Wood HCS, Wrigglesworth R, et al. Specific enzyme inhibitors in vitamin biosynthesis. Part 3. The synthesis and inhibitory properties of some substrates and transition state analogues of riboflavin synthase. J Chem Soc, Perkin Trans 1. 1980;(0):2645–56. doi: 10.1039/P19800002645 [Google Scholar]
- 34.Nielsen P, Bacher A. Biosynthesis of riboflavin. A simple synthesis of the substrate and product of the pyrimidine deaminase and of structural analogs. Z Naturforsch, B: Chem Sci. 1988;43(10):1358–64. [Google Scholar]
- 35.Cushman M, Patrick DA, Bacher A, Scheuring J. Synthesis of epimeric 6,7-bis(trifluoromethyl)-8-ribityllumazine hydrates. Stereoselective interaction with the light riboflavin synthase of Bacillus subtilis. J Org Chem. 1991;56(15):4603–8. doi: 10.1021/jo00015a009 [Google Scholar]
- 36.Cushman M, Yang D, Kis K, Bacher A. Design, Synthesis, and Evaluation of 9-D-Ribityl-1,3,7-trihydro-2,6,8-purinetrione, a Potent Inhibitor of Riboflavin Synthase and Lumazine Synthase. J Org Chem. 2001;66(25):8320–7. doi: 10.1021/jo010706r [DOI] [PubMed] [Google Scholar]
- 37.Mak JYW, Xu W, Reid RC, Corbett AJ, Meehan BS, Wang H, et al. Stabilizing short-lived Schiff base derivatives of 5-aminouracils that activate mucosal-associated invariant T cells. 2017;8:14599 doi: 10.1038/ncomms14599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Decamps L, Philmus B, Benjdia A, White R, Begley TP, Berteau O. Biosynthesis of F0, Precursor of the F420 Cofactor, Requires a Unique Two Radical-SAM Domain Enzyme and Tyrosine as Substrate. J Am Chem Soc. 2012;134(44):18173–6. doi: 10.1021/ja307762b [DOI] [PubMed] [Google Scholar]
- 39.Keller AN, Eckle SBG, Xu W, Liu L, Hughes VA, Mak JYW, et al. Drugs and drug-like molecules can modulate the function of mucosal-associated invariant T cells. Nat Immunol. 2017;18(4):402–11. doi: 10.1038/ni.3679 [DOI] [PubMed] [Google Scholar]
- 40.Zee-Cheng KY, Cheng CC. Synthesis of 5,7-dioxo-3-methyl-5,6,7,8-tetrahydropyrimido[5,4-e]-as-triazine. J Med Chem. 1968;11(5):1107–8. . [DOI] [PubMed] [Google Scholar]
- 41.Pear WS, Miller JP, Xu L, Pui JC, Soffer B, Quackenbush RC, et al. Efficient and Rapid Induction of a Chronic Myelogenous Leukemia-Like Myeloproliferative Disease in Mice Receiving P210 bcr/abl-Transduced Bone Marrow. Blood. 1998;92(10):3780 [PubMed] [Google Scholar]
- 42.Schatz PJ. Use of peptide libraries to map the substrate specificity of a peptide-modifying enzyme: a 13 residue consensus peptide specifies biotinylation in Escherichia coli. Nature Biotechnology. 1993;11(10):1138–43. [DOI] [PubMed] [Google Scholar]
- 43.Altman JD, Davis MM. MHC-Peptide Tetramers to Visualize Antigen-Specific T Cells Current Protocols in Immunology: John Wiley & Sons, Inc.; 2001. [DOI] [PubMed] [Google Scholar]
- 44.Gerhardt S, Haase I, Steinbacher S, Kaiser JT, Cushman M, Bacher A, et al. The Structural Basis of Riboflavin Binding to Schizosaccharomyces pombe 6,7-Dimethyl-8-ribityllumazine Synthase. J Mol Biol. 2002;318(5):1317–29. doi: 10.1016/s0022-2836(02)00116-x [DOI] [PubMed] [Google Scholar]
- 45.Schaefer K, Albers J, Sindhuwinata N, Peters T, Meyer B. A New Concept for Glycosyltransferase Inhibitors: Nonionic Mimics of the Nucleotide Donor of the Human Blood Group B Galactosyltransferase. ChemBioChem. 2012;13(3):443–50. doi: 10.1002/cbic.201100642 [DOI] [PubMed] [Google Scholar]
- 46.Schaefer K, Sindhuwinata N, Hackl T, Kotzler MP, Niemeyer FC, Palcic MM, et al. A nonionic inhibitor with high specificity for the UDP-Gal donor binding site of human blood group B galactosyltransferase: design, synthesis, and characterization. J Med Chem. 2013;56(5):2150–4. doi: 10.1021/jm300642a . [DOI] [PubMed] [Google Scholar]
- 47.Meermeier EW, Laugel BF, Sewell AK, Corbett AJ, Rossjohn J, McCluskey J, et al. Human TRAV1-2-negative MR1-restricted T cells detect S. pyogenes and alternatives to MAIT riboflavin-based antigens. Nat Commun. 2016;7:12506 doi: 10.1038/ncomms12506 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kurioka A, Jahun AS, Hannaway RF, Walker LJ, Fergusson JR, Sverremark-Ekström E, et al. Shared and Distinct Phenotypes and Functions of Human CD161++ Vα7.2+ T Cell Subsets. Frontiers in Immunology. 2017;8:1031 doi: 10.3389/fimmu.2017.01031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sharma PK, Wong EB, Napier RJ, Bishai WR, Ndung'u T, Kasprowicz VO, et al. High expression of CD26 accurately identifies human bacteria-reactive MR1-restricted MAIT cells. Immunology. 2015;145(3):443–53. doi: 10.1111/imm.12461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lepore M, Kalinichenko A, Calogero S, Kumar P, Paleja B, Schmaler M, et al. Functionally diverse human T cells recognize non-microbial antigens presented by MR1. eLife. 2017;6:e24476 doi: 10.7554/eLife.24476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lamichhane R, Ussher JE. Expression and trafficking of MR1. Immunology. 2017;151(3):270–9. doi: 10.1111/imm.12744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nerdal PT, Peters C, Oberg H-H, Zlatev H, Lettau M, Quabius ES, et al. Butyrophilin 3A/CD277–Dependent Activation of Human γδ T Cells: Accessory Cell Capacity of Distinct Leukocyte Populations. The Journal of Immunology. 2016;197(8):3059 doi: 10.4049/jimmunol.1600913 [DOI] [PubMed] [Google Scholar]
- 53.Gallegos AM, Xiong H, Leiner IM, Sušac B, Glickman MS, Pamer EG, et al. Control of T cell antigen reactivity via programmed TCR downregulation. Nature Immunology. 2016;17:379 doi: 10.1038/ni.3386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gérart S, Sibéril S, Martin E, Lenoir C, Aguilar C, Picard C, et al. Human iNKT and MAIT cells exhibit a PLZF-dependent proapoptotic propensity that is counterbalanced by XIAP. Blood. 2013;121(4):614 doi: 10.1182/blood-2012-09-456095 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A sample of 1•HCl was dissolved in D2O and stored in an NMR tube without light protection. The 1H NMR spectra shown were collected at (a) 0 days, (b) 4 days, (c) 12 days and (d) 19 days.
(TIF)
A portion of sample of 1•HCl was taken at (a) 0 days, (b) 4 days, (c) 11 days and (d) 37 days, dissolved in D2O and analyzed by 1H NMR without light protection.
(TIF)
(a) 0 h, (b) 21 h, (c) 5 days, and (d) 23 days. Analyzed by 1H NMR without light protection.
(TIF)
(a) 0 h, (b) 21 h, (c) 5 days, and (d) 23 days. Analyzed by 1H NMR without light protection.
(TIF)
(a) Co-staining of resting human T cells using anti-Vα7.2 (left panel) or MR1/5-OP-RU tetramers (right panel). Results represent density plots from one donor and mean% +SD in three donors. SD: standard deviation. (b) Co-staining of resting human CD161++ T cells comparing tetramer+ cells among Vα7.2+CD161++ cells (left panel) to Vα7.2+cells among tetramer+CD161++ cells (right panel). Results represent density plots from one donor and mean% + SD in three donors. (c) Human MAIT cells were identified by flow cytometry using anti-Vα7.2 (left column) or MR1/5-OP-RU tetramers (right column) after 15 hours of rest or 5-A-RU dose titration (20 μM, 2 μM, 200 nM, 20 nM) + 50 μM MeG and demonstrate 5ARU dose-dependent TCR downregulation.
(TIF)
Includes synthesis details, copies of 1H and 13C NMR spectra of known compounds, and references for the experimental section.
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.