Abstract
Background and Objective
Teamwork may affect clinical care in the neonatal intensive care unit (NICU) setting. The objective of this study was to assess teamwork climate across NICUs and to test scale level and item level associations with healthcare-associated infection (HAI) rates in very low birth weight (VLBW) infants.
Methods
Cross-sectional study of the association between HAI rates, defined as any bacterial or fungal infection during the birth hospitalization, among 6663 VLBW infants cared for in 44 NICUs between 2010 and 2012. NICU HAI rates were correlated with teamwork climate ratings obtained in 2011 from 2073 of 3294 eligible (response rate 63%) NICU health professionals. The relation between HAI rates and NICU teamwork climate was assessed using logistic regression models including NICU as a random effect.
Results
Across NICUs, 36 to 100% (mean 66%) of respondents reported good teamwork. HAI rates were significantly and independently associated with teamwork climate (OR [95% CI] 0.82 [0.73-0.92], p = 0.005), such that the odds of an infant contracting a HAI decreased by 18% with each 10% rise in NICU respondents reporting good teamwork.
Conclusion
Improving teamwork may be an important element in infection control efforts.
Keywords: Infant, newborn, teamwork, safety culture, neonatal intensive care unit, infection
INTRODUCTION
In the United States, medical errors account for nearly 100,000 avoidable deaths annually.1,2 In complex, fast-paced care settings such as the neonatal intensive care unit (NICU), patients are particularly vulnerable to medical errors. Adverse events are common for very low birth weight infants (VLBW; <1500 gram birth weight), are frequently preventable, and occur with great (10-fold) variation among NICUs.3 High reliability, originally described by Weick and Sutcliffe, refers to an environment of “collective mindfulness” in which all workers look for, and report, problems or unsafe conditions before they pose a substantial risk to the organization.4 It is a key strategy favored by the Joint Commission to prevent medical errors and complications of health care delivery, such as health care-associated infections (HAI).5,6 The term high reliability organization was originally attributed to high-risk and complex industries such as nuclear power or maritime aviation, which achieve substantially lower than predicted accident rates given their inherent risk. These organizations exhibit exemplary safety norms and share five core characteristics: sensitivity to operations, reluctance to simplify, preoccupation with failure, deference to expertise, and resilience.7
Teamwork is a critical pre-requisite to several of these core characteristics. For example, deference to expertise implies that team leaders must transcend traditional physician/nurse hierarchies to create teamwork and safety at the bedside, harnessing knowledge and information most relevant to solving a given clinical problem. Team performance is especially important in the NICU setting where fragile infants may require emergency care at a moment’s notice.8-10 A Joint Commission sentinel event investigation found poor communication as a root cause in over 72% of perinatal deaths and injuries.11 In another study, poor teamwork and communication contributed to 30% of voluntary error reports.12 A growing body of evidence is linking teamwork to improvements in care, such as reduced medication errors, length of stay, central line associated bloodstream infections13, and higher quality newborn resuscitations.14 However, while teamwork climate as a component of safety culture has been linked to clinical outcomes in adults, little is known regarding its role in preterm infants. In addition, the contribution of individual components of the teamwork scale, and characteristics of survey respondents have not been studied. In this paper, we explored variation in teamwork ratings among a large sample of NICUs and tested their associations with healthcare associated infections (HAI) in VLBW infants.
The objectives of this study were to
describe and test for variation in teamwork climate among NICUs, and
examine the association of NICU teamwork climate and its individual items with healthcare-associated infection (HAI) rates.
METHODS
Sample and procedure
Selection of NICUs
A cross-sectional survey of caregiver perceptions of teamwork was performed among a voluntary sample of NICUs participating in a Quality Improvement Collaborative organized by the California Perinatal Quality Care Collaborative (CPQCC).15 Of 61 NICUs who participated in the improvement initiative, 44 agreed to participate in the survey, which was administered at the onset of the initiative (between June and September 2011). Of the 44 NICUs, 10 were regional NICUs, 28 community NICUs, and 6 intermediate NICUs as defined by the California Department of Healthcare Services.16 These designations are roughly equivalent with American Academy of Pediatrics levels 4, 3, and 2 respectively.17
Staff with a 0.5 full time equivalent or greater time commitment to the NICU for at least the four weeks prior to survey administration were invited to participate. Paper-based surveys were administered during routine departmental and staff meetings. Surveys were returned to a locked box or sealable envelope to maintain confidentiality. Individuals not present in routine meetings were hand-delivered a survey, pencil and return envelope. This administration technique has generated high response rates.18,19 CPQCC administered the survey and transmitted a de-identified data set to Dr. Profit for analysis. The study was approved by the Institutional Review Boards at Stanford University and Baylor College of Medicine.
Selection of Patients
Clinical data routinely submitted to the CPQCC by Collaborative members reflecting VLBW infants born between January 1, 2010 and December 31, 2012 were linked to the survey data using unique identifiers for NICUs and patients. We excluded infants with severe congenital anomalies to reduce systematic bias in infection rates between NICUs that are the result of the need for prolonged parenteral nutrition and surgical intervention. We used multiyear analysis due to the small number of VLBW infants cared for in some institutions.
Measures
Survey Data
For this study, we used the teamwork climate scale of the Safety Attitudes Questionnaire (SAQ),18,20 which measures caregiver perceptions of teamwork using six items with response scales ranging from 1 (disagree strongly) to 5 (agree strongly).
The six teamwork items were: 1) “Nurse input is well received in this NICU”, 2) ”In this NICU, it is difficult to speak up if I perceive a problem with patient care”, 3) “Disagreements in this NICU are appropriately resolved”, 4) “I have the support I need from others in this NICU to care for patients”, 5) “It is easy for personnel here to ask questions when there is something they do not understand”, and 6) “The physicians and nurses here work together as a well-coordinated team.” The second item is reverse coded.
NICU-level teamwork climate scores were calculated as the percent of respondents within a NICU that had a mean score across all six items of “slightly agree” or “strongly agree.” For this purpose, individual responses are transformed onto a 100-point scale score according to the following formula:
In order to calculate the percent of respondents who are positive (i.e., percent agreement), one calculates the percent of respondents within a NICU who received a teamwork score of 75 or higher.18,21,22 We call this “percentage agree” or “percentage reporting good teamwork.” We recommend a threshold NICU-level teamwork climate score of 60%, with a goal of 80 to 100%. The 60% threshold came from our anecdotal experience using the SAQ, in which units with <60% of respondents reporting good safety climate had the most to gain from quality improvement efforts, and were substandard in clinical and operational outcomes, such as adult ventilator-associated pneumonia rates and adult ICU length of stay.23,24
The survey also captured respondent characteristics including job position, years in specialty, primary work area (pediatric, adult, or both), gender, and predominant work shift. Job positions included attending physicians (MDs), subspecialty residents, neonatal nurse practitioners (NNPs), registered nurse (RNs), respiratory care practitioners (RTs), and other.
Clinical Data
CPQCC prospectively collects clinical data for infants born at 136 member hospitals utilizing the standard definitions developed by the Vermont Oxford Network.25 Data undergo a series of quality checks to ensure completeness and accuracy. HAI rates for each NICU were calculated using CPQCC definitions which include the proportion of VLBW infants with any bacterial or fungal infection acquired after three days of age during the birth hospitalization. The measure is a binary “Yes”/“No”. We adjusted HAI rates according to a severity of illness model we developed in a previous study.26 The variables included sex, gestational age at birth (strata of 25 0/7 to 27 6/7, 28 0/7 to 29 6/7, and 30 0/7 or more weeks), 5 minute Apgar score (categorized as three or below, between four and six, and above six), small for gestational age (<10th percentile), and birth at the NICU under investigation (inborn) or outborn.
Analyses
Objective 1 - Describe and test for variation in teamwork climate among NICUs
We used descriptive statistics including frequencies, means, and standard deviations to describe teamwork climate overall and between groups. We used a logistic regression model with respondent job position as a predictor based on findings from previous studies.20 In keeping with prior research, we grouped respondent job position into physician versus non-physician categories.27
Objective 2 - Examine the association of NICU teamwork climate and its individual items with HAI rates
Descriptive analyses examined the variation in unadjusted HAI rates across NICUs. Pearson correlation coefficient was used to examine the relation between HAI rates and NICU-level teamwork. We also used infant-level multivariable mixed models with NICU as a random effect for teamwork item and scale level associations with risk-adjusted HAI rates. Marginal and conditional R2 were computed to assess the variation explained by fixed and random factors within each model.28
All statistical analyses were performed using SAS version 9.4. The study was approved by the Institutional Review Boards at Stanford University and Baylor College of Medicine.
RESULTS
Objective 1 - Describe and test for variation in teamwork climate among NICUs
Forty-four NICUs participated in this study. Of 3294 administered surveys, 2073 were returned for an overall response rate of 62.9%. Response rates within NICUs ranged from 21.7% to 100% with an average of 69.7% (SD = 19.8%). Respondent characteristics are listed in Table 1. Of the 1962 respondents who indicated their position and length of experience, 1175 (59.9%) reported at least 11 years and 47 (2.4%) reported less than one year in their specialty. Attending physicians were predominantly male (58.8%). All other positions were predominantly female (subspecialty residents 61.3%, RNs 94.1%, NNPs 100%, RTs 53.5%).
Table 1.
Description of survey respondents and clinical sample
| n (%) or mean (SD) | Missing n (%) | |
|---|---|---|
| NICU Level (n = 44) | ||
| Level of care | 0 | |
| Regional | 10 (22.7) | |
| Community | 28 (63.6) | |
| Intermediate | 6 (13.6) | |
| Respondent Level (n = 2073) | ||
| Gender | 71 (3.4) | |
| Female | 1697 (84.8) | |
| Male | 305 (15.2) | |
| Typical Shift | 205 (10.0) | |
| Days | 894 (47.9) | |
| Evenings | 79 (4.2) | |
| Nights | 602 (32.2) | |
| Variable | 293 (15.7) | |
| Position | 32 (1.5) | |
| Attending physician | 204 (10.0) | |
| Subspecialty resident | 31 (1.5) | |
| Neonatal nurse practitioner | 35 (1.7) | |
| Registered nurse | 1464 (71.7) | |
| Respiratory care practitioner | 286 (14.0) | |
| Other* | 21 (1.0) | |
| Years in specialty | 103 (5.0) | |
| Less than 6 months | 20 (1.0) | |
| 6-11 months | 27 (1.4) | |
| 1-2 years | 74 (3.8) | |
| 3-4 years | 192 (9.7) | |
| 5-10 years | 476 (24.2) | |
| 11-20 years | 538 (27.3) | |
| 21 years or more | 643 (32.6) | |
| Infant Level (n = 6663) | ||
| Gestational age at birth | 28.3 (2.8) | 0 |
| Birth weight | 1072 (280) | 0 |
| Small Gestational Age | 0 | |
| No | 5447 (81.7) | |
| Yes | 1216 (18.3) | |
| Patient gender | 1 (0.01) | |
| Female | 3313 (49.7) | |
| Male | 3349 (50.3) | |
| 5-minute Apgar score | 28 (0.4) | |
| <4 | 319 (4.8) | |
| 4-6 | 1105 (16.7) | |
| >6 | 5211 (78.5) | |
| Inborn without transfer | 0 | |
| No | 1764 (26.5) | |
| Yes | 4899 (73.5) | |
| Healthcare associated infection | 0 | |
| No | 6009 (90.2) | |
| Yes | 654 (9.8) |
The 21 survey respondents identified as “other” consisted of licensed vocational nurses, clinical nurse leads, research nurses, and nurse aides.
Item level results for teamwork across all respondents are shown in Table 2. Across all units the majority of respondents express slightly or strongly favorable views of teamwork across the 6 items. However, significant variation across NICUs is demonstrated in Figure 1. At the NICU level, the percentage of respondents reporting good teamwork ranged from 36 to 100 with a mean of 66. Physician participation varied across the NICUs as shown in the graph. Even after adjusting for variation in respondent job position, we found significant variation in teamwork climate across NICUs (p < 0.01). Physicians experience teamwork as significantly better than RNs, NNPs, and RTs ((mean physicians = 84.3, mean non-physicians = 59.4, p < 0.001) (Figure 2). The odds of a physician reporting good teamwork are 3.7 times higher than for a non-physician.
Table 2.
Teamwork items frequency distribution (n = 2073 respondents in 44 NICUs)
| Respondent Level | ||||||
|---|---|---|---|---|---|---|
| Teamwork item | Disagree Strongly | Disagree Slightly | Neutral | Agree Slightly | Agree Strongly | Mean PPR |
| n (%) | n (%) | n (%) | n (%) | n (%) | % (SD) | |
| Nurse input is well received in this NICU. | 63 (3.1) | 169 (8.3) | 242 (11.9) | 687 (33.8) | 874 (43.0) | 76.7 (10.5) |
| In this NICU, it is difficult to speak up if I perceive a problem with patient care.* | 828 (40.3) | 610 (29.7) | 225 (11.0) | 278 (13.5) | 113 (5.5) | 69.6 (9.5) |
| Disagreements in this NICU are appropriately resolved (i.e., not who is right but what is best for the patient). | 89 (4.4) | 250 (12.3) | 427 (20.9) | 639 (31.3) | 636 (31.2) | 62.2 (11.3) |
| I have the support I need from others in this NICU to care for patients. | 38 (1.8) | 77 (3.7) | 150 (7.3) | 562 (27.3) | 1235 (59.9) | 87.6 (7.2) |
| It is easy for personnel here to ask questions when there is something that they do not understand. | 30 (1.5) | 117 (5.7) | 155 (7.5) | 576 (28.0) | 1183 (57.4) | 85.3 (7.6) |
| The physicians and nurses here work together as a well-coordinated team. | 54 (2.6) | 169 (8.2) | 211 (10.2) | 778 (37.7) | 852 (41.3) | 79.5 (13.4) |
| Teamwork Scale Score | 65.8 (13.8) | |||||
Teamwork items derived from the Safety Attitudes Questionnaire. Calculations of percent positive responses (PPR) included agree slightly, and agree strongly. PPR – Percent positive response, SD – standard deviation,
reverse scored for PPR.
Figure 1.

Distribution of teamwork climate across 44 NICUs. Mean teamwork rating was 66%. A unit-level rating below 60% implies the need for intervention. Goal is a unit-level rating above 80%. Diamonds indicate the proportion of physician respondents in each NICU.
Figure 2.
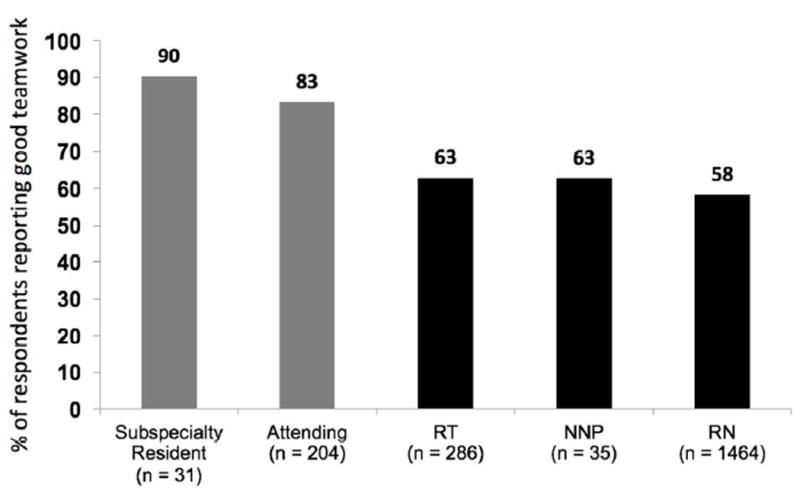
Teamwork by job position in 44 NICUs. Physicians in grey bars. RT – Respiratory Care Provider, NNP – Neonatal Nurse Practitioner, RN – Registered Nurse Physicians rated teamwork higher than non-physicians (84.3% vs 59.4%). The odds of rating teamwork good was 3.8 times greater for physicians.
Objective 2 - Examine relations between item and scale-level NICU teamwork climate scores and HAI
The unadjusted characteristics of the clinical sample are displayed in Table 1. Of the 6663 infants included in the study, 654 (9.8%) of VLBW infants experienced an infection during the study period. About three quarters of the infants were cared for at their birth hospital.
Patient-level associations of teamwork items and the teamwork climate scale after adjustment for clinical characteristics are shown in Table 3. All parameter estimates pointed in the direction of lower HAI rates with better teamwork and were independently associated with HAI in fixed models. However, after accounting for NICU as a random effect, items 1 through 5 were not independently associated with HAI rates (although item 3 (“Disagreements in this NICU are appropriately resolved”; p = 0.069) showed a trend towards significance). Item 6 (“The physicians and nurses here work together as a well-coordinated team”; p = 0.005) and the overall teamwork climate scale (p = 0.005) remained significantly and independently associated with HAI rates. Item 6 showed the strongest association with HAI, such that the odds of an infant contracting a HAI was 19% lower with each 10% increase in NICU respondents reporting good teamwork. In the safety culture literature, a 10% increase has been regarded as a significant improvement.24 The additional variance explained by the teamwork items and scale was small (<2%). The relation between absence of HAI and teamwork climate by NICU is illustrated in Figure 3.
Table 3.
Relation between healthcare associated infection rates and teamwork climate items and scale
| Fixed Models | Mixed Models | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Teamwork item | Model | PE | SE | P | OR* (95%CI) | PE | SE | P | OR* (95%CI) | R2 |
| 1. Nurse input is well received in this NICU. | CF + Q1 | -1.20 | 0.44 | 0.007 | 0.89 (0.81-0.97) | -1.01 | 0.99 | 0.310 | 0.90 (0.77-1.06) | 0.204 |
| 2. It is difficult to speak up if I perceive a problem with patient care.** | CF + Q2r | -1.60 | 0.46 | <0.001 | 0.85 (0.78-0.93) | -0.84 | 1.07 | 0.431 | 0.92 (0.77-1.10) | 0.202 |
| 3. Disagreements in this NICU are appropriately received. | CF + Q3 | -1.67 | 0.41 | <0.001 | 0.85 (0.78-0.92) | -1.57 | 0.86 | 0.069 | 0.85 (0.74-0.99) | 0.209 |
| 4. I have the support I need from others in this NICU to care for patients. | CF + Q4 | -1.64 | 0.67 | 0.014 | 0.85 (0.74-0.97) | -0.62 | 1.49 | 0.680 | 0.94 (0.74-1.20) | 0.201 |
| 5. It is easy for personnel here to ask questions when there is something they do not understand. | CF + Q5 | -2.59 | 0.57 | <0.001 | 0.77 (0.69-0.86) | -2.09 | 1.34 | 0.118 | 0.81 (0.65-1.01) | 0.207 |
| 6. The physicians and nurses here work together as a well-coordinated team. | CF + Q6 | -1.94 | 0.35 | <0.001 | 0.82 (0.77-0.88) | -2.09 | 0.74 | 0.005 | 0.81 (0.72-0.92) | 0.218 |
| 1.-6. Teamwork Scale Score | CF + Q1-6 | -2.30 | 0.36 | <0.001 | 0.79 (0.74-0.85) | -2.02 | 0.72 | 0.005 | 0.82 (0.73-0.92) | 0.217 |
n = 2073 respondents in 44 NICUs. HAI – Healthcare associated infection, CF – Clinical factors; included sex, small for gestational age, gestational age in weeks, outborn and APGAR score at 5 minutes, PE - Parameter estimate, SE – Standard error, OR – Odds ratio,
Odds ratio calculated as the change in odds of infection of an infant for every 10% absolute difference in respondents reporting good teamwork.
Reverse scored. Mixed models with NICU as random effect. R2 is calculated as a marginal R2 representing the variance explained by fixed factors. Marginal R2 for a model fitting clinical factors only was 0.201. Teamwork scale conditional R2, which takes into account both fixed and random factors, was 0.262.
Figure 3.
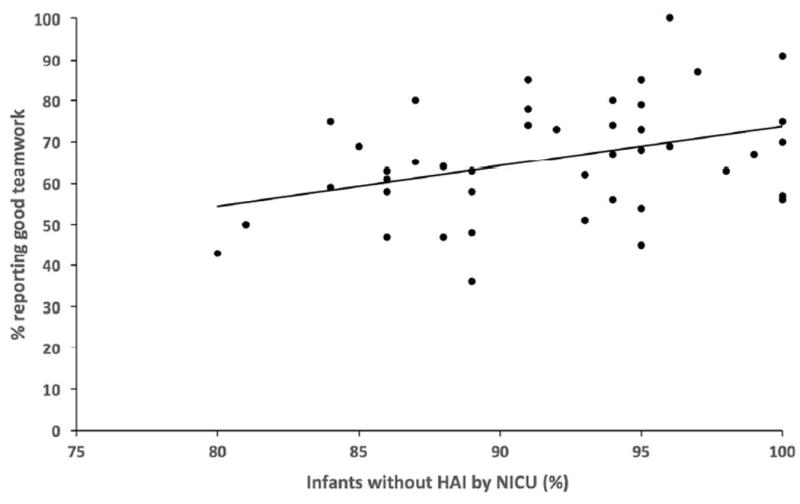
Teamwork climate and absence of infection by NICU Teamwork climate presented as percent positive response. Pearson correlation coefficient r = 0.33, p = 0.03.
DISCUSSION
Our study yields two principal findings:
Teamwork climate varies significantly across NICUs and providers.
Teamwork climate is inversely associated with HAI rates among VLBW infants.
Physicians perceived teamwork climate as much better than nurses, NNPs, and RTs. These results validate similar findings in previous smaller studies of 12 NICUs, the labor and delivery setting and the operating room.20,29-31 One of these studies demonstrated that provider characteristics (personal attributes, reputation and expertise/seniority) influenced the ability of critical caregivers to work together.30 These factors may have similarly influenced perceptions in our study sample.
Findings from this research elucidate how the seven principal components of teamwork identified by Salas et al, perceived variably across NICUs, are linked to HAI rates. The seven components are: (1) Cooperation, dependent upon mutual trust and team-oriented mindset. (2) Coordination, requiring shared performance monitoring, adaptability, and support. (3) Communication, which must be clear, precise, and timely. (4) Cognition, specifically a shared understanding of roles and abilities of teammates. (5) Coaching, referring to team leadership and clear expectations. (6) Conflict and resolution, requiring interpersonal skills and a culture of “psychological safety.” (7) Conditions, particularly a supportive context for teams, recognition of teamwork’s importance, and positive reinforcement for good performance.32,33
The link between teamwork and low HAI rates has been reported in other intensive care settings34,35 and offers an intriguing window into how culture factors may affect quality of care. Teamwork items most highly associated with HAI focused on physician nurse coordination, communication, and perceptions of nurse input. These areas may be specifically relevant for team-based decisions about placement and discontinuation of central venous catheters, feeding advancement, and weaning from ventilator support, all of which may influence catheter dwell time. The item “The physicians and nurses work together as a well-coordinated team” showed the strongest association with HAI, lending support for team-training interventions as a target of infection reduction initiatives. For example, the Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) focuses on team leadership, situation monitoring, mutual support, and communication.36 This approach has been used in multiple health care settings37,38 and has demonstrated an improvement in perceptions of teamwork among NICU providers.39 Overall, team training has been shown to have a beneficial effect on care quality40 and it may be similarly useful for prevention of HAI.
Interestingly, support from others to care for patients was not significantly associated with teamwork. Providing additional support for nurses for sterile line changes has been one of the solutions promoted for reducing HAI, but at least among these providers might not yield the desired benefit. However, we caution against over-interpretation, because providers were not asked to specifically consider HAI when completing the survey.
The results of this study must be viewed in the context of its design. We included data from 44 NICUs in California, the largest study on teamwork climate in the NICU setting to date, representing all levels of acuity and varied patient populations. Participation in this collaborative effort was limited and available on a first come basis, potentially leading to selection bias. The direction of bias is unpredictable without teamwork ratings for non-participant NICUs. Our findings may plausibly generalize to other settings because they are consistent with the extant literature.14,18,29,41-43
While teamwork climate in NICUs was significantly associated with HAI in this study, a broader exploration of relations between teamwork climate and other clinical outcomes is needed. While there may be aspects that are specific to infections, the nature of the teamwork items focusing on coordination, uninterrupted information flow, and avoidance of hierarchical barriers to communication appear to be broadly relevant to many NICU-related tasks and interventions.
Our study does not evaluate whether teamwork climate is sensitive to change after exposure to training or an intervention. However, emerging evidence from operating room studies demonstrates that teamwork climate can be improved, and result in impressive clinical and operational improvements.10
CONCLUSIONS
We found significant variation and scope for improvement in teamwork climate among this sample of NICUs. Teamwork climate was independently associated with HAI rates in VLBW infants. Interventions to improve teamwork may be critical to promote safe care for these most vulnerable patients.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Health worker surveys on teamwork show large variation across NICUs
In adult ICU settings higher teamwork ratings have been associated with lower healthcare-associated infection rates
WHAT THIS STUDY ADDS
Teamwork climate is associated with healthcare-associated infection rates in VLBW infants. Most of this association is accounted for by an item on physicians and nurses working together as a well-coordinated team.
Acknowledgments
We would like to thank the NICU personnel at the following CPQCC member hospitals:
Antelope Valley Hospital, Lancaster
Arrowhead Regional Medical Center, Colton
California Pacific Medical Center, San Francisco
Cedars-Sinai Medical Center, Los Angeles
Children’s Hospital Central California, Madera
Children’s Hospital of Orange County, Orange
Community Regional Medical Center - Fresno, Fresno
Doctors Medical Center - Modesto, Modesto
El Camino Hospital-Mountain View, Mountain View
Garfield Medical Center, Monterey Park
Good Samaritan Hospital of Santa Clara Valley–San Jose, San Jose
Harbor-UCLA Medical Center, Torrance
Hoag Memorial Hospital Presbyterian, Newport Beach
Hollywood Presbyterian Medical Center, Los Angeles
Huntington Memorial Hospital, Pasadena
John Muir Medical Center, Walnut Creek
Kaiser Permanente Oakland Medical Center, Oakland
Kaiser Permanente Walnut Creek Medical Center, Walnut Creek
Kaweah Delta Health Care District: Visalia Hospital, Visalia
Mercy Medical Center Redding, Redding
Mercy San Juan Medical Center, Carmichael
Methodist Hospital of Southern California, Arcadia
Miller Children’s Hospital at Long Beach Memorial Medical Center, Long Beach
Orange County Global Medical Center, Santa Ana
Pomona Valley Hospital Medical Center, Pomona
Providence Saint Joseph Medical Center, Burbank
Providence Tarzana Medical Center, Tarzana
Rady Children’s Hospital at Palomar Medical Center, Escondido
Redlands Community Hospital, Redlands
Regional Medical Center of San Jose, San Jose
Riverside County Regional Medical Center, Moreno Valley
Salinas Valley Memorial Healthcare System, Salinas
Scripps Memorial Hospital-La Jolla, La Jolla
Sequoia Hospital, Redwood City
Sharp Chula Vista Medical Center, Chula Vista
Sharp Mary Birch Hospital for Women & Newborns, San Diego
St. Bernardine Medical Center, San Bernardino
St. Jude Medical Center, Fullerton
Sutter Alta Bates Summit Medical Center, Berkeley
Sutter Medical Center-Sacramento, Sacramento
Tri-City Medical Center, Oceanside
University of California Davis Medical Center, Sacramento
University of California San Francisco Medical Center, San Francisco
Valley Presbyterian Hospital, Van Nuys
Funding source: This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development [R01 HD084679-01, Co-PI: Sexton and Profit and K24 HD053771-01, PI: Thomas], Texas Children’s Hospital [Pediatrics Pilot Research Fund 33-126, PI: Profit] where Dr. Profit worked at the time of this research. Dr. Tawfik’s effort was supported by the Jackson Vaughan Critical Care Research Fund.
Abbreviations
- CPQCC
California Perinatal Quality Care Collaborative
- MD
physician
- NICU
neonatal intensive care unit
- NNPs
neonatal nurse practitioners
- RNs
registered nurse
- RCPs
respiratory care practitioners
- SAQ
Safety Attitudes Questionnaire
- VLBW
very low birth weight
Footnotes
Conflict of Interest: The other authors have no conflicts of interest to disclose.
Financial Disclosure: The other authors have no financial relationships relevant to this article to disclose.
AUTHOR CONTRIBUTIONS
Drs. Profit and Sexton had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Individual author contributions: ICMJE criteria for authorship read and met: JP PJS MB JR MD CCN EJT HCL JBS. Agree with the manuscript’s results and conclusions: JP PJS MB JR MD CCN EJT HCL JBS. Designed the experiments/the study: JP MB HCL JBS. Analyzed the data: MB JBS. Wrote the first draft of the paper: JP JBS. Assisted with approach and selection of data inputs: JP PJS EJT HCL JBS. Assisted with interpretation of results: JP PJS MB JR MD CCN EJT HCL JBS. Contributed to revision of the paper: JP PJS MB JR MD DST CCN EJT HCL JBS.
References
- 1.Thomas EJ, Studdert DM, Burstin HR, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care. 2000;38(3):261–71. doi: 10.1097/00005650-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. 1991. Qual Saf Health Care. 2004;13(2):145–51. doi: 10.1136/qshc.2002.003822. discussion 51-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharek PJ, Horbar JD, Mason W, et al. Adverse events in the neonatal intensive care unit: development, testing, and findings of an NICU-focused trigger tool to identify harm in North American NICUs. Pediatrics. 2006;118(4):1332–40. doi: 10.1542/peds.2006-0565. [DOI] [PubMed] [Google Scholar]
- 4.Weick KE, Sutcliffe KM. Managing the unexpected : resilient performance in an age of uncertainty. 2. San Francisco: Jossey-Bass; 2007. [Google Scholar]
- 5.Chassin MR, Loeb JM. The ongoing quality improvement journey: next stop, high reliability. Health Aff. 2011;30(4):559–68. doi: 10.1377/hlthaff.2011.0076. [DOI] [PubMed] [Google Scholar]
- 6.Chassin MR, Loeb JM. High-reliability health care: getting there from here. Milbank Q. 2013;91(3):459–90. doi: 10.1111/1468-0009.12023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weick K, Sutcliffe KM. Managing the Unexpected: Reslient Performance in an Age of Uncertainty. 2. San Francisco, CA: Jossey-Bass; 2007. [Google Scholar]
- 8.Clarke S, Aiken L. Failure to rescue. Am J Nurs. 2003;103:42–47. doi: 10.1097/00000446-200301000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Simpson K. Failure to rescue. Implications for evaluating quality of care during labor and birth. J Perinat Neonat Nurs. 2005;19:24–34. doi: 10.1097/00005237-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Thomas EJ, Williams AL, Reichman EF, et al. Team training in the neonatal resuscitation program for interns: teamwork and quality of resuscitations. Pediatrics. 2010;125(3):539–46. doi: 10.1542/peds.2009-1635. [DOI] [PubMed] [Google Scholar]
- 11.Commission TJ. Sentinel Event Alert Issue #30. [May 12, 2014]; Available from: http://www.jointcommission.org/assets/1/18/SEA_30.PDF.
- 12.Suresh G, Horbar JD, Plsek P, et al. Voluntary anonymous reporting of medical errors for neonatal intensive care. Pediatrics. 2004;113(6):1609–18. doi: 10.1542/peds.113.6.1609. [DOI] [PubMed] [Google Scholar]
- 13.Pronovost PJ, Berenholtz SM, Goeschel C, et al. Improving patient safety in intensive care units in Michigan. J Crit Care. 2008;23(2):207–21. doi: 10.1016/j.jcrc.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Thomas EJ, Taggart B, Crandell S, et al. Teaching teamwork during the Neonatal Resuscitation Program: a randomized trial. J Perinatol. 2007;27(7):409–14. doi: 10.1038/sj.jp.7211771. [DOI] [PubMed] [Google Scholar]
- 15.Gould JB. The role of regional collaboratives: the California Perinatal Quality Care Collaborative model. Clin Perinatol. 2010;37(1):71–86. doi: 10.1016/j.clp.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Regional Perinatal Programs of California: California Department of Public Health. [7/29/2015];2014 Available from: http://www.cdph.ca.gov/programs/rppc/Pages/default.aspx.
- 17.Stark AR. Levels of neonatal care. Pediatrics. 2012;130(3):587–97. doi: 10.1542/peds.2012-1999. [DOI] [PubMed] [Google Scholar]
- 18.Sexton JB, Helmreich RL, Neilands TB, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res. 2006;6(1):44. doi: 10.1186/1472-6963-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Profit J, Etchegaray J, Petersen LA, et al. The Safety Attitudes Questionnaire as a tool for benchmarking safety culture in the NICU. Arch Dis Child Fetal Neonatal Ed. 2012;97(2):F127–32. doi: 10.1136/archdischild-2011-300612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Profit J, Etchegaray J, Petersen LA, et al. Neonatal intensive care unit safety culture varies widely. Arch Dis Child Fetal Neonatal Ed. 2012;97(2):F120–6. doi: 10.1136/archdischild-2011-300635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sexton J, Thomas E, Pronovost P. The Context of Care and the Patient Care Team: The Safety Attitudes Questionnaire. In: Proctor P, Compton W, Grossman J, et al., editors. Building a Better Delivery System: A New Engineering/Health Care Partnership. Washington, DC: National Academies Press; 2005. pp. 119–24. [Google Scholar]
- 22.Pronovost PJ, Thompson DA, Holzmueller CG, et al. Defining and measuring patient safety. Critical care clinics. 2005;21(1):1–19. vii. doi: 10.1016/j.ccc.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 23.Hudson DW, Berenholtz SM, Thomas EJ, et al. A safety culture primer for the critical care clinician: the role of culture in patient safety and quality improvement. Contemporary Critical Care. 2009;7(5):1–12. [Google Scholar]
- 24.Sexton JB, Berenholtz SM, Goeschel CA, et al. Assessing and improving safety climate in a large cohort of intensive care units. Crit Care Med. 2011;39(5):934–39. doi: 10.1097/CCM.0b013e318206d26c. [DOI] [PubMed] [Google Scholar]
- 25.Horbar JD, Soll RF, Edwards WH. The Vermont Oxford Network: a community of practice. Clin Perinatol. 2010;37(1):29–47. doi: 10.1016/j.clp.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 26.Profit J, Kowalkowski MA, Zupancic JA, et al. Baby-MONITOR: a composite indicator of NICU quality. Pediatrics. 2014;134(1):74–82. doi: 10.1542/peds.2013-3552. published Online First: 2014/06/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Profit J, Sharek PJ, Amspoker AB, et al. Burnout in the NICU setting and its relation to safety culture. BMJ Qual Saf. 2014;23(10):806–13. doi: 10.1136/bmjqs-2014-002831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nakagawa S, Schielzeth H. A general and simple method for obtaining R2 from generalized linear mixed-effects models. Methods Ecol Evol. 2013;4(2):133–42. [Google Scholar]
- 29.Sexton JB, Holzmueller CG, Pronovost PJ, et al. Variation in caregiver perceptions of teamwork climate in labor and delivery units. J Perinatol. 2006;26(8):463–70. doi: 10.1038/sj.jp.7211556. [DOI] [PubMed] [Google Scholar]
- 30.Thomas EJ, Sexton JB, Helmreich RL. Discrepant attitudes about teamwork among critical care nurses and physicians. Crit Care Med. 2003;31(3):956–59. doi: 10.1097/01.CCM.0000056183.89175.76. [DOI] [PubMed] [Google Scholar]
- 31.Wiles R. Teamwork in primary care: the views and experiences of nurses, midwives and health visitors. J Advanced Nurs. 1994;20:324–30. doi: 10.1046/j.1365-2648.1994.20020324.x. [DOI] [PubMed] [Google Scholar]
- 32.Salas E, Rosen MA. Building high reliability teams: progress and some reflections on teamwork training. BMJ Qual Saf. 2013;22(5):369–73. doi: 10.1136/bmjqs-2013-002015. [DOI] [PubMed] [Google Scholar]
- 33.Salas E, Almeida SA, Salisbury M, et al. What are the critical success factors for team training in health care? Jt Comm J Qual Patient Saf. 2009;35(8):398–405. doi: 10.1016/s1553-7250(09)35056-4. [DOI] [PubMed] [Google Scholar]
- 34.Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. NEnglJMed. 2006;355(26):2725–32. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- 35.Pronovost PJ, Goeschel CA, Colantuoni E, et al. Sustaining reductions in catheter related bloodstream infections in Michigan intensive care units: observational study. BMJ. 2010;340:c309. doi: 10.1136/bmj.c309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Clancy CM, Tornberg DN. TeamSTEPPS: assuring optimal teamwork in clinical settings. Am J Med Qual. 2007;22(3):214–7. doi: 10.1177/1062860607300616. [DOI] [PubMed] [Google Scholar]
- 37.Mayer CM, Cluff L, Lin WT, et al. Evaluating efforts to optimize TeamSTEPPS implementation in surgical and pediatric intensive care units. Jt Comm J Qual Patient Saf. 2011;37(8):365–74. doi: 10.1016/s1553-7250(11)37047-x. [DOI] [PubMed] [Google Scholar]
- 38.Sawyer T, Laubach VA, Hudak J, et al. Improvements in teamwork during neonatal resuscitation after interprofessional TeamSTEPPS training. Neonatal Netw. 2013;32(1):26–33. doi: 10.1891/0730-0832.32.1.26. [DOI] [PubMed] [Google Scholar]
- 39.Beitlich P. TeamSTEPPS implementation in the LD/NICU settings. Nurs Manage. 2015;46(6):15–8. doi: 10.1097/01.NUMA.0000465404.30709.a5. [DOI] [PubMed] [Google Scholar]
- 40.Hughes AM, Gregory ME, Joseph DL, et al. Saving lives: A meta-analysis of team training in healthcare. J Appl Psychol. 2016;101(9):1266–304. doi: 10.1037/apl0000120. [DOI] [PubMed] [Google Scholar]
- 41.Sexton JB, Makary MA, Tersigni AR, et al. Teamwork in the operating room: frontline perspectives among hospitals and operating room personnel. Anesthesiology. 2006;105(5):877–84. doi: 10.1097/00000542-200611000-00006. [DOI] [PubMed] [Google Scholar]
- 42.Thomas EJ, Sexton JB, Lasky RE, et al. Teamwork and quality during neonatal care in the delivery room. J Perinatol. 2006;26(3):163–69. doi: 10.1038/sj.jp.7211451. [DOI] [PubMed] [Google Scholar]
- 43.Thomas EJ. Improving teamwork in healthcare: current approaches and the path forward. BMJ Qual Saf. 2011;20(8):647–50. doi: 10.1136/bmjqs-2011-000117. [DOI] [PubMed] [Google Scholar]


