Abstract
There is substantial evidence that polyunsaturated fatty acids (PUFAs) such as n-3 and n-6 fatty acids (FAs) play an important role in prevention of atherosclerosis. In vitro and in vivo studies focusing on the interactions between monocytes and endothelial cells have explored the molecular effects of FAs on these interactions. Epidemiological surveys, followed by large, randomized, control trials have demonstrated a reduction in major cardiovascular events with supplementation of n-3 FAs in secondary prevention settings. The evidence of beneficial effects specific to patients with peripheral artery disease (PAD) remains elusive, and is the focus of this review.
Keywords: lipids, nutrition, peripheral arterial disease, peripheral vascular diseases, review
Introduction
Peripheral artery disease (PAD) is a condition with significant impact on the health of our society. Population-based studies suggest that PAD affects more than 12% of people aged > 65 years, and more than 20% of those aged > 75 years.1 A more recent study suggests that in a primary care population, nearly one-third of patients > 70 years suffer from PAD.2 Overall, the public is poorly informed about PAD, with major knowledge gaps as to the definition of PAD, the risk factors and symptoms of the disease, as well as the associated risks of amputation or mortality.3 In the International Reduction of Atherothrombosis for Continued Health (REACH) Registry, PAD treatment was associated with higher annual mean medication and hospitalization costs than coronary artery disease (CAD) or cerebrovascular disease (CVD).4 The need for cost-effective therapies to prevent and treat PAD is great.
Nutritional intake of n-3 fatty acids (FAs) has long been recognized to correlate with cardiovascular health. Greenland Eskimos who consume a diet rich in whale, seal, and fish have a very low incidence of CAD,5 pointing toward the ability of n-3 FAs, a compound found in fish and fish oils, to reduce cardiovascular risk.5,6 In fact, n-3 FAs have been considered to act as natural HMG-CoA reductase and ACE enzyme inhibitors, anti-arrhythmic, anti-hypertensive, anti-atherosclerotic, anti-inflammatory, cytoprotective, and cardioprotective molecules.7 Although several randomized trials and meta-analyses have demonstrated beneficial effects in CAD, this type of evidence remains sparse for PAD. The importance and timeliness of this clinical research question was highlighted by a recent editorial.8 In this review, we summarize the cellular, physiological, and clinical evidence reporting possible associations of n-3 FAs and PAD, and discuss the controversy surrounding the dietary intake of n-6 FAs.
Historical perspectives
Human diet has changed substantially over the past 10,000 years, particularly in Western countries. Important societal changes that began with the development of agriculture and animal husbandry have been followed more recently by the industrial revolution, agribusiness, and modern food-processing techniques. Hypotheses abound that these profound nutritional changes in food quality have led to many of the diseases of our Western civilization, including atherosclerosis (CAD, CVD, PAD), diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), colon cancer, essential hypertension, obesity, diverticulosis, and dental caries.9–11 These conditions have appeared in the last 100 years and are still unknown in some of the remaining hunter-gatherer populations whose lifestyles reflect those of the pre-agricultural human beings.10 These hypotheses are balanced, however, by the fact that the life expectancy of our population has increased.
Compared to the Paleolithic period, our Western diet is characterized by (1) an increase in energy intake and decrease in energy expenditure; (2) a decrease in protein, antioxidants, and calcium intake; (3) a decrease in complex carbohydrates and fibers; (4) an increase in processed cereal grains and a decrease in fruits and vegetables; (5) an increase in saturated fat (SFA), trans fat and n-6 FAs; and (6) a decrease in n-3 FAs.12 Two main technological processes have led to the changes in FA consumption: animal husbandry and agri-business, practices of processing cheap and altered food stocks. In addition, the increase in grain harvests and the subsequent feeding of grain (primarily corn) to cattle have led to ‘marbled meat’ made up of excessive triglyceride fat accumulation in muscle interfascicular adipocytes, which contain an increase in SFA content, more n-6 FAs, and less n-3 FAs.13 Furthermore, with the advent of the oil-seed processing industry ca. 1950, there was a significant increase in the total intake of vegetable cooking oil high in n-6 FAs.
Overall, these societal and environmental changes have directly increased the dietary level of n-6 FAs at the expense of lowered levels of n-3 FAs, leading to n-6:n-3 dietary ratios close to 15:1, compared with hunter-gatherer diets, which were estimated to be around 2:1.13,14 The total intake of n-3 FAs in the US is 1.6 g/day (0.7% of energy intake).14 Of this, α-linolenic acid (ALA) accounts for 1.4 g/day and only 0.1–0.2 g/day comes from eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). The conversion of ALA to EPA and DHA, the more biologically active molecules, remains low (0.2–15%).15,16 The average US intake of linoleic acid (LA) is 14.8 g/day,17 while arachidonic acid (AA) is consumed at the amount of 0.15 g/day. The conversion of LA to AA is ~0.2%.18 It is likely that the higher ratio of n-6:n-3 impacts processes in atherogenesis at the molecular, physiological, and clinical levels. These concepts are reviewed in the next sections.
Molecular and biological responses
FAs are part of the larger group of lipids including fats, waxes, sterols, fat-soluble vitamins, phospholipids, and others. Lipids are generally classified as fatty acyls, glycerolipids, glycerophospholipids, sphingolipids, sterol lipids, prenol lipids, saccharolipids, and polyketides.19 Lipids play an important role in energy storage, structure of the cell membrane, and signaling pathways. With regards to FAs, animal fats are stored in the body as triglycerides, compounds in which three FA molecules (the acyl group) are linked to a glycerol molecule by an ester bond. There are three main categories of FAs: (1) the SFAs, (2) the mono-unsaturated fatty acids (MUFAs), and (3) the polyunsaturated fatty acids (PUFAs) (Figure 1). The PUFAs (all of which are essential FAs) are further subdivided into n-6 PUFAs and n-3 PUFAs. They are referred to as n-3 FAs and n-6 FAs in this article.
Figure 1.
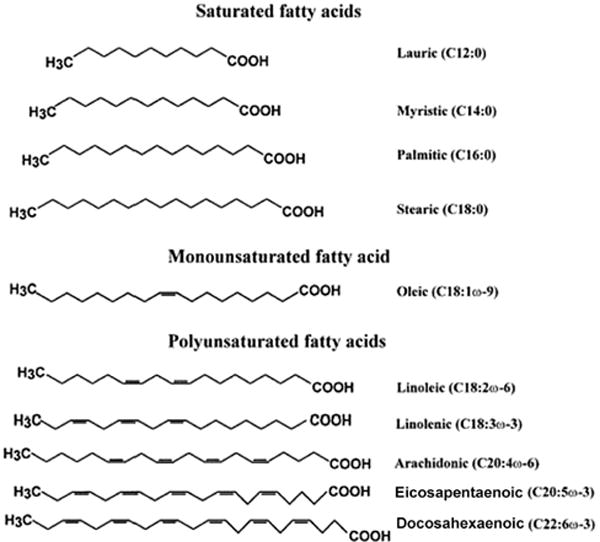
Chemical structure of different fatty acids including saturated fatty acids, monounsaturated fatty acids, and polyunsaturated fatty acids.
The names of PUFAs are derived from their molecular structure, with the n-3 FA family having the first double-bond on the third carbon, counting from the terminal methyl end of the FA, and the n-6 FA family having the first double-bond on the sixth carbon, counting from the terminal methyl end of the FA. These differences give these FAs different biochemical properties (Table 1). The chemical nomenclature describes the number of carbon atoms and the number of double-bounds in the carbon chain. For example, a C18:3 PUFA has 18 carbon atoms and three double-bonds in the carbon chain.
Table 1.
Differences between n-3 and n-6 fatty acids
| n-6 Fatty acids | n-3 Fatty acids | |
|---|---|---|
| Molecular structure | First double-bond on the 6th carbon counting from the methyl end (the ‘n’th carbon) | First double-bond on the 3rd carbon counting from the methyl end (the ‘n’th carbon) |
| Types | Linoleic acid (LA) [C18:2] Arachidonic acid (AA) [C20:4] |
α-Linolenic acid (ALA) [C18:3] Eicosapentaenoic acid (EPA) [C20:5] Docosahexaenoic acid (DHA) [C22:6] |
| Food sources | Corn oil (LA) Soybean oil (LA) Safflower oil (LA) Sunflower oil (LA) Poultry (AA) Meats (AA) |
Flaxseed oil (ALA) Canola oil (ALA) Soybean oil (ALA) Oily fish (EPA/DHA) Fish oil capsules (EPA/DHA) |
| Examples of end mediators | Lipoxins Aspirin-triggered lipoxins Thromboxanes Prostacyclins Leukotrienes |
Resolvins type D Resolvins type E Protectins |
The most prevalent n-3 FA is ALA, an n-3 FA (C18:3) that is found in large quantities in flaxseed oil (about 55%) and to lesser extents in canola (about 10%) and unhydrogenated soybean oil (about 7%). A very small fraction (< 5%, perhaps < 1%) of ingested ALA is converted into EPA (20:5), one of the long-chain n-3 FAs, and even less is converted into the 22-carbon DHA. EPA and DHA are found in fish oil, which is derived from the tissues and gut of oily fish (as compared to whitefish, which contain oil mostly in the liver). Fish, like other animals, do not manufacture EPA and DHA; they accumulate these molecules from feeding on plant species such as microalgae. Hence, n-3 FAs can be considered as ‘phyto oils’ which are simply harvested from fish.
The biological effects of n-3 FAs are divided in three broad categories, recently reviewed by De Caterina:20 direct effects on ion channels modulating arrhythmias, direct effects on membranes requiring incorporation into cell phospholipids, and effects mediated by the release of bioactive mediators. The latter two are discussed here.
Incorporation of n-3 FAs into the cell membranes leads to several molecular and cellular events. At the molecular level, several effects have been reported, including: (1) a reduction in production of cytokines (interleukin-1 (IL-1) and tumor necrosis factor (TNF) in lipopolysaccharide (LPS)-stimulated monocytes);21 (2) a reduction in the production of platelet-derived growth factor (PDGF)-A and -B protein and mRNA;22,23 (3) a decrease in tissue factor production by monocytes;24 (4) an increase in the bioavailability of endothelial nitric oxide;25 (5) down-regulation of gene expression of monocyte-chemoattractant protein-1 (MCP)-1,26,27 a monocyte-chemoattractant protein; and (6) inhibition of IL-8.27 Several of the anti-inflammatory effects of n-3 FAs seem to be at least partly mediated through peroxisome proliferator-activated receptor (PPAR)-alpha.28 The nuclear factor (NF)-κB27,28 system of transcription factors, which controls the coordinated expression of adhesion molecules and of leukocyte-specific chemoattractants upon cytokine stimulation,29,30 also appears to be involved,31 with a decrease in nuclear translocation of the NF-κB subunit p65.32 Other nuclear factors are likely to be involved and are reviewed elsewhere in greater detail.33,34 It also appears that n-3 FAs lead to a reduction in expression of endothelial adhesion molecules (vascular cell adhesion protein-1 (VCAM-1), E-selectin, and intercellular adhesion molecule-1 (ICAM-1)).35–37 The consequences of such changes include a reduction in leukocyte adhesion to the endothelium, a critical early step in atherogenesis.28,32,36 Recent studies have also suggested a decrease in the migration of neutrophils across the endothelium.38 Several of their actions may be related to cell membrane phospholipid makeup and cell signaling.39,40 Furthermore, it appears that n-3 FAs may modulate the cellular and structural composition of the atherosclerotic plaque, in a manner to reduce rupture or ulceration41 and overall regression of the plaque.42
Related to the release of a bioactive mediator, and also at the level of the cell membrane, there is evidence that in the presence of n-3 FAs, prostaglandin (PG) D3 replaces PGD2,38 leading to competitive inhibition at the COX-2 level. This likely leads to replacement of AA with the prostanoid derivatives of EPA, potentially less pro-thrombotic and vasoconstrictive than AA derivatives.43 More recently, Serhan et al. discovered novel mechanisms in inflammation related to the ‘resolution-phase interaction products’ (resolvins) pathways.44–46 This new paradigm describes the transition from acute to chronic inflammation as involving the loss of endogenously operative resolution processes. This response aims to re-establish homeostasis through resolution of an acute inflammatory response. Lipid autacoids such as n-3 and n-6 FAs are at the core of these responses.47 As described by Stables and Gilroy, the classic tale of inflammation describes a process of resolution of inflammation that is passive, mediated by a decrease in the pro-inflammatory cytokines, prostaglandins, and oxygen species, with no active contribution of pro-resolving lipid mediators.48 An alternative pathway for inflammation now describes resolution as an active process involving changes in the phenotypes of cells such as endothelial cells, macrophages, and monocytes leading to the production of lipid mediators such as resolvins, protectins, lipoxins, aspirin-triggered lipoxins, and newly identified maresins (Table 2). Hence, while cyclooxygenase (COX) and lipoxygenase (LOX)-derived lipid mediators such as the prostaglandins and leukotrienes promote inflammation,49 anti-inflammatory and pro-resolving lipid mediators such as lipoxins and resolvins45 are generated to actively turn off inflammation. Lipoxins and resolvins are thought to be bioactive products of n-3 and n-6 FAs.44,50 Of interest, it was recently demonstrated that plasma levels of pro-resolving mediator 15-epimeric lipoxin are significantly lower in patients with symptomatic PAD than in healthy volunteers, suggesting a ‘resolution deficit’ in PAD.51
Table 2.
New concepts on resolution of inflammation
| Classic view regarding inflammation | Alternative view regarding resolution of inflammation | |
|---|---|---|
| Resolution is… | A passive process | An active process |
| Lipid mediators | No active participation | Active participation |
| Critical components | Decrease cytokines Decrease prostaglandins Decrease oxygen species |
Resolvins Protectins Lipoxins Aspirin-triggered lipoxins Maresins |
Physiological studies
The clinically relevant benefits of fish-oil and n-3 supplementation (discussed below) are thought to be at least partially due to improvement in endothelial function and reduction in inflammation. Supporting evidence of this proposition includes an improvement in endothelial function in healthy volunteers (both acute and chronic administration of n-3 FAs; response measured with flow-mediated brachial artery vasodilation (FMD), laser Doppler imaging, or strain-gauge phlethysmography),52–54 in obese adolescents (3-month treatment with n-3 FAs; response measured with peripheral artery tonometry),55 and in patients with chronic heart failure (6-week treatment with n-3 FAs; response measured by venous occlusion strain-gauge plethysmography).56 Furthermore, a reduction in inflammation as measured by C-reactive protein (CRP) was found in healthy individuals,57–63 male smokers,64 obese adolescents,55 and in patients with rheumatoid arthritis65 or CAD.66 However, these benefits are more controversial in the elderly population. One prospective study conducted in a nursing home population, where a diet enriched with mackerel was given to the patients, increased FMD compared with a control group.67 Conversely, a study assessing the postprandial response to a single fish oil-enriched meal in older versus younger men found no improvement in FMD in the older men and a significant increase in FMD in younger men.68 Clinically, n-3 FAs reduce serum triglycerides at pharmacological doses (typically 3 g of EPA/DHA).69–71
Clinical evidence
Trials in coronary artery disease
Studies report that n-3 FAs derived from fish oil reduce cardiovascular disease,6,72 with a high tissue ratio of n-3:n-6 FAs leading to a reduced risk of coronary events.73 Greenland Eskimos, who consume a diet very high in n-3 FAs, have a very low incidence of CAD.5 Several different clinical trials have investigated the effects of fish consumption or fish oil supplementation for the prevention of cardiovascular events. Patients from three large trials, the Diet and Reinfarction trial (DART trial), the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico trial (GISSI-Prevenzione trial), and the Japan EPA Lipid Intervention Study (JELIS trial) account for 95% of individuals demonstrating an overall decrease in total mortality, decrease in cardiovascular death, decrease in sudden cardiac death, and a reduction in non-fatal cardiovascular events.74–76 These trials are described in great detail in several well-written reviews and meta-analyses.20,77–84 The omega-3 index, used in some CAD trials, is defined as the percentage of EPA + DHA in red blood cells (RBCs) and reflects FA dietary intake. It has been proposed as a marker and risk factor for CAD, especially sudden cardiac death.85–89 To the authors’ knowledge, this marker has not been correlated thus far with PAD.
Marik and Varon, in their meta-analysis on the beneficial cardiovascular effects of n-3 FAs, identified 11 prospective, randomized, placebo-controlled clinical trials evaluating clinical cardiovascular endpoints.77 These studies included 39,044 patients with recent myocardial infarction (MI), with an implanted cardioverter defibrillator, patients with heart failure (HF), PAD, and hypercholesterolemia. The main dose used was 1.8 g/day for 2.2 ± 1.2 years. The authors reported an overall reduction in the risk of cardiovascular death, sudden cardiac death (SCD), all-cause mortality, and non-fatal cardiovascular events. The authors concluded that dietary supplementation with n-3 FAs should be considered in the secondary prevention of cardiovascular events.
It is worth mentioning that the OMEGA trial, not included in this most recent meta-analysis, became the first randomized study to assess the effects of highly purified n-3 acid ethyl ester at 1 g/day for 1 year (460 mg EPA, 380 mg DHA), in addition to the current guideline therapy. It was a double-blinded, multicenter trial that randomized a total of 3851 patients.90 The primary endpoint was SCD and the secondary endpoints included total mortality and non-fatal events. There were no significant differences between the two groups in both the primary or secondary endpoints. Although the findings were unexpected in view of the results from other large trials, it is possible that with current therapies including statins, anti-platelets, angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, aspirin with or without a second anti-platelet drug if indicated, and beta-blocker, the effects of fish oil have less of an impact. However, a more likely explanation is that the study was underpowered (with the initial power calculations based on the GISSI-Prevenzione trial – a different era with regard to CAD medical therapy), the dose was too low to see a real effect, and fish consumption post-MI increased from 30% to 45%, which could have blunted a response difference.
Also notable was the 2007 publication of the results of the JELIS trial.76 This study used a prospective, randomized open-label, blinded endpoint evaluation and recruited 18,645 patients with total cholesterol of 6.5 mmol/l or greater between 1996 and 1999 (both a primary and secondary prevention trial). The patients were randomized to either 1800 mg of EPA daily with statin (n = 9326) or statin alone (n = 9319), with a 5-year follow-up. Analysis was done in an intention-to-treat fashion, with the primary endpoint being any major coronary event (sudden cardiac death, fatal and non-fatal MI, and other non-fatal events including unstable angina, angioplasty, stenting or coronary artery bypass grafting). At 4.6 years, there was a 19% relative reduction in major coronary events (p = 0.011), with the primary endpoint occurring in 2.8% of the patients in the EPA group and 3.5% of patients in the control group. Serum low-density lipoprotein (LDL) cholesterol was not a significant factor in a reduction of risk for major coronary events. The EPA group had significantly reduced unstable angina and non-fatal coronary events, but no change was seen in sudden cardiac death and coronary death. In the secondary prevention subgroup (patients with a history of CAD), major coronary events were reduced by 19% (p = 0.048). In the primary prevention subgroup, EPA reduced major coronary events by 18% but this was not significant. More interestingly, in a later sub-study analysis of the JELIS trial, n-3 supplementation was associated with a 55% reduction in major coronary events in the PAD subgroup, compared with an 18% relative reduction in the patients without PAD, corresponding to a numbers needed to treat (NNT) of 11 and pointing to a significant benefit to the PAD population of EPA supplementation (hazard ratio (95% confidence interval (CI)): 0.44 (0.19–0.97); p = 0.041).91 However, the JELIS trial was an open-label trial that was not focused on PAD, and was done in a Japanese population that eats a significant amount of fish at baseline. A related editorial entitled ‘Eicosapentaenoic acid as the gold standard for patients with peripheral artery disease?’ summarized some of these major questions.8 The evidence from studies focused on PAD is described below.
Trials in peripheral artery disease
Although there is some evidence suggesting that consumption of an n-3 FA diet may be associated with a decreased prevalence of PAD,92 the effects of n-3 FAs on PAD have not been as thoroughly investigated as their effects in the CAD patient population. In a cross-sectional study using the National Health and Nutrition Examination Survey, Lane et al. demonstrated that better nutrition (particularly a higher consumption of n-3 FAs) was associated with a reduced prevalence of PAD in the US population, irrespective of traditional cardiovascular risk factors.92 Using patients with PAD sampled from the Edinburgh Artery Study, Leng et al. attempted to determine the levels of plasma FAs in patients with PAD versus control subjects.93 In 113 cases and 122 control subjects, FA levels were measured in three plasma fractions (triglyceride, cholesteryl ester, and phospholipid), and smoking habits and dietary antioxidant intake were determined by questionnaire. AA, EPA, DHA, and docosapentaenoic acid (DPA; 20:5; n-3) were significantly lower in cases than in controls (p < 0.01). By logistic regression adjustment for smoking and vitamin C intake, DPA (odds ratio (95% CI): 0.19 (0.08–0.56); p < 0.01) and AA (odds ratio: 0.44 (0.19–0.98); p < 0.05) remained significantly related to the presence of disease. Only DPA reduced the risk associated with smoking. The authors concluded that in subjects with PAD compared with healthy controls, the largest benefits occurred in FAs of the n-3 series, particularly DPA.
Several smaller prospective studies have aimed to assess the effects of fish oil and n-3 FAs on different parameters related to PAD. They are summarized in Table 3. In a double-blinded, randomized, placebo-controlled study, Woodcock et al. assessed the effects of 1.8 g/day of n-3 FAs for 7 weeks in 19 patients with intermittent claudication (IC). They assessed walking distance, Doppler ultrasound, ankle–brachial index (ABI), platelets, blood viscosity, cholesterol, and triglycerides. The authors demonstrated an overall decrease in blood viscosity and serum triglycerides, but no significant changes in other parameters.94
Table 3.
Previous studies on n-3 fatty acids and patients with peripheral artery disease
| Authors | Year | Type of study | Patients | n | Fish oil treatment (PUFA content) | Variables measured | Findings | Ref. |
|---|---|---|---|---|---|---|---|---|
| Woodcock et al. | 1984 | Double-blind, randomized, placebo-controlled study | M/F IC |
19 | 1.8 g/day × 7 weeks (1.8 g EPA) |
|
|
94 |
| Gans et al. | 1990 | Double-blind, randomized, placebo-controlled study | M/F IC |
32 | 3 g/day × 4 months (1.8 g EPA + 1.2 g DHA) |
|
|
95 |
| Mori et al. | 1992 | Double-blind, randomized, placebo-controlled study | M PAD based on symptoms and angiogram |
32 | 15 g/day × 1 month (2.8 g EPA + 1.8 g DHA) |
|
|
96 |
| Leng et al. | 1998 | Double-blind, randomized, placebo-controlled study | M/F IC |
120 (total) | 1.95 g/day × 2 yearsa (1.68 g γ-linolenic acid + 0.27 g EPA) |
|
|
97 |
| Carrero et al. | 2005 | Double-blind, randomized, placebo-controlled study | M IC and controls |
60 | Enriched dairy product × 12 months |
|
|
98 |
| Conway et al. | 2005 | Double-blind, randomized, placebo-controlled study | M/F IC |
50 | 10 g/day fish oils × 16 weeks (1.7 g EPA + 1.15 g DHA) |
|
|
99 |
| Luu et al. | 2007 | Prospective study | IC and controls | 16 | 6 g/day × 12 weeks (1.02 g EPA + 0.69 g DHA) |
|
|
104 |
| Madden et al. | 2007 | Prospective study | M IC |
69 | 6 g/day × 12 weeks (1.02 g EPA + 0.69 g DHA) |
|
|
102 |
| Schiano et al. | 2008 | Single-blind, randomized trial | M/F IC |
32 | 2 g/day × 3 months (EPA:DHA 0.9:1.5) |
|
|
101 |
| Madden et al. | 2009 | Prospective study | M IC and controls |
205 | 6 g/day × 12 weeks (1.02 g EPA + 0.69 g DHA) |
|
|
103 |
Two capsules BID × 2 weeks, then three capsules BID for remainder of trial; capsules made of linolenic acid (280 mg) and EPA (45 mg).
ABI, ankle–brachial index; CRP, C-reactive protein; DHA, docosahexaenoic acid; EPA, eicosapentaenoic acid; F, female; FMD, flow-mediated brachial artery vasodilation; IC, intermittent claudication; M, male; PAD, peripheral artery disease; QOL, quality of life; SBP, systolic blood pressure; TG, triglycerides.
Gans et al., in a double-blinded, randomized fashion, also studied the effects of fish oil supplementation in patients with IC. Thirty-two patients were randomized to 3 g/day of n-3 FAs versus placebo for 4 months. The authors were interested in outcomes including blood pressure, ABI, pain-free and maximal walking distance, blood and plasma viscosity, cholesterol and triglycerides. They demonstrated a decrease in blood viscosity, improvement in lipid profile, but no changes in walking distance or ABIs.95
Mori et al. performed a study of 32 patients with symptomatic and angiographically demonstrated PAD.96 The randomized, controlled, double-blinded trial provided 4 g/day of n-3 FAs (EPA and DHA) or placebo for 4 weeks. Endpoints of interest included cholesterol, triglycerides, and platelet count. Fish oil treatment reduced serum triglyceride levels, but increased total cholesterol levels. Platelet aggregation was significantly reduced after fish oil treatment.
Leng et al. performed a randomized, controlled trial on the effects of γ-linolenic and EPA treatment over 2 years in 84 men and 36 women with lower limb atherosclerosis presenting with IC.97 The patients were treated with 1.68 g of γ-linolenic acid and 0.27 g of EPA per day versus placebo. The outcomes measured included fatal and non-fatal cardiovascular events, cholesterol, blood and plasma viscosity, blood pressure, ABI, and pain-free walking distance. The authors found that treatment produced a statistically significant reduction in systolic blood pressure, but no other significant benefits except from a trend toward fewer coronary events in patients taking FAs.
Carrero et al. conducted a study of 60 patients with IC and randomized them in a double-blinded, controlled fashion to skimmed milk containing 200 mg EPA and 130 mg of DHA plus oleic acid, folic acid, and vitamins or to a placebo-milk.98 The patients received the treatment or placebo for 12 months. The outcomes of interest included ABI, pain-free walking distance, triglycerides, and cholesterol. The authors found that the plasma concentrations of EPA and DHA increased after treatment with supplements. Interestingly, there was a decrease in cholesterol, and a decrease in total homocysteine in patients in which this value was initially high. Furthermore, walking distance and ABIs increased in the treatment group. The authors concluded that the inclusion of certain nutrients in the diet improves cardiovascular health.
Conway et al. conducted a randomized, controlled, double-blinded trial in 35 men and 15 women with IC.99 The treatment included a much higher concentration of fish oil (10 g/day of EPA and DHA) versus placebo for 16 weeks. The authors assessed quality of life, ABI, and pain-free and walking distance. They found no difference in ABI, absolute walking distance, or quality of life outcomes between the groups. There was, however, an improvement in initial walking distance.
One meta-analysis studied the effects of n-3 FAs in IC.100 The study identified six randomized controlled trials assessing the effects of n-3 FAs in patients with IC, representing 313 participants. All studies assessed n-3 dietary supplementation versus placebo, with the treatment duration lasting between 4 weeks and 2 years. Blood viscosity decreased; however, there were no significant differences between ABI, systolic blood pressure (SBP), plasma viscosity, or walking distance (pain-free or maximum walking distance). Gastrointestinal side effects were observed in two studies. It is important to note that despite the administration of fish oil or oily fish, which increases the amount of n-3 FAs in the diet, the consumption of n-6 FAs may remain high, thereby minimally altering the ratio of n-6:n-3. The impact of an intervention may then have less of an effect and may explain the discrepancies among the included studies.
More recent studies not included in the above meta-analysis are worth mentioning. Schiano et al., in a single-blinded study, assessed the effects of n-3 supplementation at the dose of 2 g/day in 32 men and women with IC. Their outcomes of interest were endothelial function with FMD and inflammation. They demonstrated significant improvement in FMD, with no changes in inflammatory markers such as CRP.101
Lastly, Madden et al., in a prospective study, demonstrated an increase in both ABI and walking distance with 1.7 g of n-3 FAs for 12 weeks in male patients with claudication.102 Using the same cohort, the authors investigated changes in CD44 expression in the monocytes of patients.103 CD44 is known to increase cellular recruitment to the endothelium during inflammation. They demonstrated that CD44 expression was decreased in PAD patients after administration of fish oil for 12 weeks. Yet another study by the same group demonstrated that fish oil supplementation reduced the potency of monocytes to stimulate endothelial cells in normal subjects, but not those from patients with PAD.104
Fatty acids intake recommendations
The American Heart Association (AHA) Diet and Lifestyle Recommendations specify that the general population should aim to consume fish, especially oily fish, at least twice a week.105 This should be coupled with the limitation of saturated fat intake to < 7% of energy, trans fat to < 1% of energy, and cholesterol to < 300 mg/day.105 These recommendations are based on findings that the consumption of two servings per week of fish high in EPA and DHA is associated with a reduced risk of both sudden death and death from CAD.84, 106 Furthermore, this specific requirement for fish consumption may displace the consumption of other foods that are high in saturated and trans FAs from the diet (such as fatty meats and full-fat dairy products). For patients without CAD, the AHA also recommends including oils and foods rich in ALA (flaxseed, canola and soybean oils; flaxseeds and walnuts).106
For patients with documented CAD, the AHA recommendations suggest consumption of ~1 g of EPA + DHA per day, preferably from oily fish. The AHA also states that EPA + DHA supplements could be considered, in consultation with the patient’s physician. For patients with hypertriglyceridemia, the AHA recommends that 2–4 g of EPA + DHA per day should be provided as capsules under a physician’s care.106 More recent evidence suggests doses in the amount of 3–4 g/day for hypertriglyceridemia.82,107
No specific recommendations exist for patients with PAD. Since the first n-3 FA advisory, the FDA has ruled that intakes of up to 3 g/day of marine n-3 FAs are ‘generally recognized as safe’ (GRAS) in the diet.108 The only prescription drug available in the US, and approved by the FDA, is Lovaza®, an n-3 acid ethyl ester, approved for the treatment of hypertriglyceridemia at 4 g/day.
It is worth mentioning that the most common side effect of fish oil supplementation is a fishy aftertaste. In the GISSI Prevention study, 0.85 g of omega-3 FAs per day for 3.5 years, 3.8% of patients discontinued taking their supplements (compared with 2.1% for the vitamin E group).75 Gastrointestinal disturbances (4.9%) and nausea (1.4%) were the most commonly reported side effects. In the HARP Research Group study, 12 capsules containing 6 g of omega-3 FAs were given to 41 patients for 2.4 years.109 Three patients dropped out of the study claiming intolerance to the capsules. In a study by Leaf et al., a 6-month trial provided 275 patients with 6.9 g of EPA/DHA daily.110 There was no difference between the fish oil and corn oil control groups for adverse events, with gastrointestinal upset reported by 8% of the fish oil patients and 7% in the placebo group. Lastly, a study by von Schacky et al. administered fish oil at a dose of 6 g/day for 3 months, then 3 g/day for 21 months (111 patients).111 Four fish oil patients and three placebo patients had mild gastrointestinal discomfort, one patient in the fish oil group had an itchy rash (unlikely related to the study medication as per the authors), and one had a minor hematoma after a second angioplasty.
The n-6 controversy
The role of n-6 FAs in outcomes of patients with cardiovascular disease is more controversial. The primary dietary n-6 FA is LA, which has 18 carbons and two double-bonds (C18:2 n-6). It is found in abundance in liquid vegetable oils, with safflower oil containing about 75% linoleic by weight and corn oil about 50%. AA is found in the greatest amounts in the phospholipids of grain-fed animals and in eggs. Although humans and other mammals (except some carnivores, such as lions) can convert LA to AA, the conversion is slow.112 However, mammalian cells cannot convert n-6 to n-3 FAs because they lack the converting enzyme, n-3 desaturase.
The n-6 FAs have been found to directly stimulate pro-inflammatory gene expression in endothelial113 and smooth muscle cells,114 and augment the effect of pro-inflammatory cytokines. An increase in the LA content of LDL increases the sensitivity to oxidation,115 and oxidized LDL is involved in atherosclerosis plaque growth. AA is the precursor for an extensive array of eicosanoids (20-carbon FA metabolites), including all of the 2-series prostaglandins, thromboxane A2, prostacyclin (PGI2), the 4-series leukotrienes, and a variety of cytochrome P-450 metabolites. These compounds are bioactive and several mediate inflammatory responses, stimulate platelet aggregation, and produce vasoconstriction. It is important to remember that ‘pro-inflammatory’ FAs are necessary for proper immune functioning. Although in excess and unopposed they may promote atherosclerotic disease and thrombus formation, there is at this time no universal belief or high-level evidence that n-6 promote CAD.
The evidence for a beneficial role of dietary n-6 FAs is less convincing. A Science Advisory Subcommittee of the AHA published a report on the effects of n-6 FAs and the risk of CAD.17 Based on a few small studies, the report suggests an increase in the consumption of n-6 FAs to 5–10% of energy intake, in order to reduce the risk of CAD related to lower intakes. It states that reducing n-6 FA intake would likely increase more than decrease the risk of CAD.17 This area has been quite controversial,12,116–119 with particular debate focused on the quality of evidence from which the recommendations were derived. A more recent meta-analysis by Ramsden et al. reviewing trials of n-6 FAs suggested that the advice regarding increase in n-6 consumption was based on evidence from trials administering both n-3 and n-6 FAs, and not n-6 in isolation,120 blurring the evidence for the AHA recommendations.120,121 In fact, the authors state: “Advice to specifically increase n-6 PUFA intake, based on mixed n-3/n-6 RCT data, is unlikely to provide the intended benefits, and may actually increase the risks of CHD and death”. Overall, the question of an association or effect of n-6 FAs and CAD remains unsettled. In view of a lack of evidence for lower extremity artery disease, dietary recommendations for n-6 cannot be given for patients with PAD.
Conclusions and future directions
PUFAs, particularly n-3 FAs, have proven to have considerable beneficial health effects, particularly in the secondary prevention of CAD. Although PAD is another atherosclerotic syndrome, the evidence for beneficial effects of n-3 FAs in that population is present, but weaker. We are presently conducting a clinical trial randomizing patients with IC to 4.4 g of EPA/DHA or placebo (NCT01310270), with the primary endpoint being improvement in endothelial function measured with FMD, and the secondary endpoint being a change in the inflammatory profile. We expect this trial to better characterize the effects of dietary supplementation of n-3 FAs in patients with PAD.
Acknowledgments
We thank Amy J Markowitz for her editorial comments on the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Funding
This work was supported by funds from the Department of Surgery, University of California, San Francisco and the Northern California Institute for Research and Education. The project described was supported by Award Number KL2RR024130 from the National Center for Research Resources.
Footnotes
Conflict of interest
None declared.
Dr Jorge Plutzky was the guest editor for this article.
References
- 1.Criqui MH, Fronek A, Barrett-Connor E, Klauber MR, Gabriel S, Goodman D. The prevalence of peripheral arterial disease in a defined population. Circulation. 1985;71:510–515. doi: 10.1161/01.cir.71.3.510. [DOI] [PubMed] [Google Scholar]
- 2.Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286:1317–1324. doi: 10.1001/jama.286.11.1317. [DOI] [PubMed] [Google Scholar]
- 3.Hirsch AT, Murphy TP, Lovell MB, et al. Gaps in public knowledge of peripheral arterial disease: the first national PAD public awareness survey. Circulation. 2007;116:2086–2094. doi: 10.1161/CIRCULATIONAHA.107.725101. [DOI] [PubMed] [Google Scholar]
- 4.Mahoney EM, Wang K, Cohen DJ, et al. One-year costs in patients with a history of or at risk for atherothrombosis in the United States. Circ Cardiovasc Qual Outcomes. 2008;1:38–45. doi: 10.1161/CIRCOUTCOMES.108.775247. [DOI] [PubMed] [Google Scholar]
- 5.Bang HO, Dyerberg J, Nielsen AB. Plasma lipid and lipoprotein pattern in Greenlandic west-coast Eskimos. Lancet. 1971;i:1143–1145. doi: 10.1016/s0140-6736(71)91658-8. [DOI] [PubMed] [Google Scholar]
- 6.Daviglus ML, Stamler J, Orencia AJ, et al. Fish consumption and the 30-year risk of fatal myocardial infarction. N Engl J Med. 1997;336:1046–1053. doi: 10.1056/NEJM199704103361502. [DOI] [PubMed] [Google Scholar]
- 7.Das UN. Essential fatty acids and their metabolites could function as endogenous HMG-CoA reductase and ACE enzyme inhibitors, anti-arrhythmic, anti-hypertensive, anti-atherosclerotic, anti-inflammatory, cytoprotective, and cardioprotective molecules. Lipids Health Dis. 2008;7:37. doi: 10.1186/1476-511X-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamanouchi D, Komori K. Eicosapentaenoic acid as the gold standard for patients with peripheral artery disease? – subanalysis of the JELIS trial. Circ J. 2010;74:1298–1299. doi: 10.1253/circj.cj-10-0449. [DOI] [PubMed] [Google Scholar]
- 9.Eaton SB, Konner M. Paleolithic nutrition. A consideration of its nature and current implications. N Engl J Med. 1985;312:283–289. doi: 10.1056/NEJM198501313120505. [DOI] [PubMed] [Google Scholar]
- 10.Konner M, Eaton SB. Paleolithic nutrition: twenty-five years later. Nutr Clin Pract. 2010;25:594–602. doi: 10.1177/0884533610385702. [DOI] [PubMed] [Google Scholar]
- 11.Eaton SB, Konner M, Shostak M. Stone agers in the fast lane: chronic degenerative diseases in evolutionary perspective. Am J Med. 1988;84:739–749. doi: 10.1016/0002-9343(88)90113-1. [DOI] [PubMed] [Google Scholar]
- 12.Simopoulos AP. The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp Biol Med (Maywood) 2008;233:674–688. doi: 10.3181/0711-MR-311. [DOI] [PubMed] [Google Scholar]
- 13.Cordain L, Watkins BA, Florant GL, Kelher M, Rogers L, Li Y. Fatty acid analysis of wild ruminant tissues: evolutionary implications for reducing diet-related chronic disease. Eur J Clin Nutr. 2002;56:181–191. doi: 10.1038/sj.ejcn.1601307. [DOI] [PubMed] [Google Scholar]
- 14.Kris-Etherton PM, Taylor DS, Yu-Poth S, et al. Polyunsaturated fatty acids in the food chain in the United States. Am J Clin Nutr. 2000;71:179S–188S. doi: 10.1093/ajcn/71.1.179S. [DOI] [PubMed] [Google Scholar]
- 15.Emken EA, Adlof RO, Gulley RM. Dietary linoleic acid influences desaturation and acylation of deuterium-labeled linoleic and linolenic acids in young adult males. Biochim Biophys Acta. 1994;1213:277–288. doi: 10.1016/0005-2760(94)00054-9. [DOI] [PubMed] [Google Scholar]
- 16.Pawlosky RJ, Hibbeln JR, Novotny JA, Salem N., Jr Physiological compartmental analysis of alpha-linolenic acid metabolism in adult humans. J Lipid Res. 2001;42:1257–1265. [PubMed] [Google Scholar]
- 17.Harris WS, Mozaffarian D, Rimm E, et al. Omega-6 fatty acids and risk for cardiovascular disease: a science advisory from the American Heart Association Nutrition Subcommittee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Cardiovascular Nursing; and Council on Epidemiology and Prevention. Circulation. 2009;119:902–907. doi: 10.1161/CIRCULATIONAHA.108.191627. [DOI] [PubMed] [Google Scholar]
- 18.Hussein N, Ah-Sing E, Wilkinson P, Leach C, Griffin BA, Millward DJ. Long-chain conversion of [13C]linoleic acid and alpha-linolenic acid in response to marked changes in their dietary intake in men. J Lipid Res. 2005;46:269–280. doi: 10.1194/jlr.M400225-JLR200. [DOI] [PubMed] [Google Scholar]
- 19.Fahy E, Subramaniam S, Murphy RC, et al. Update of the LIPID MAPS comprehensive classification system for lipids. J Lipid Res. 2009;50(suppl):S9–14. doi: 10.1194/jlr.R800095-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.De Caterina R. n-3 fatty acids in cardiovascular disease. N Engl J Med. 2011;364:2439–2450. doi: 10.1056/NEJMra1008153. [DOI] [PubMed] [Google Scholar]
- 21.Endres S, Ghorbani R, Kelley VE, et al. The effect of dietary supplementation with n-3 polyunsaturated fatty acids on the synthesis of interleukin-1 and tumor necrosis factor by mononuclear cells. N Engl J Med. 1989;320:265–271. doi: 10.1056/NEJM198902023200501. [DOI] [PubMed] [Google Scholar]
- 22.Fox PL, DiCorleto PE. Fish oils inhibit endothelial cell production of platelet-derived growth factor-like protein. Science. 1988;241:453–456. doi: 10.1126/science.3393911. [DOI] [PubMed] [Google Scholar]
- 23.Kaminski WE, Jendraschak E, Kiefl R, von Schacky C. Dietary omega-3 fatty acids lower levels of platelet-derived growth factor mRNA in human mononuclear cells. Blood. 1993;81:1871–1879. [PubMed] [Google Scholar]
- 24.Hansen JB, Olsen JO, Wilsgard L, Osterud B. Effects of dietary supplementation with cod liver oil on monocyte thromboplastin synthesis, coagulation and fibrinolysis. J Intern Med Suppl. 1989;731:133–139. doi: 10.1111/j.1365-2796.1989.tb01447.x. [DOI] [PubMed] [Google Scholar]
- 25.Shimokawa H, Vanhoutte PM. Dietary omega 3 fatty acids and endothelium-dependent relaxations in porcine coronary arteries. Am J Physiol. 1989;256:H968–973. doi: 10.1152/ajpheart.1989.256.4.H968. [DOI] [PubMed] [Google Scholar]
- 26.Baumann KH, Hessel F, Larass I, et al. Dietary omega-3, omega-6, and omega-9 unsaturated fatty acids and growth factor and cytokine gene expression in unstimulated and stimulated monocytes. A randomized volunteer study. Arterioscler Thromb Vasc Biol. 1999;19:59–66. doi: 10.1161/01.atv.19.1.59. [DOI] [PubMed] [Google Scholar]
- 27.Mishra A, Chaudhary A, Sethi S. Oxidized omega-3 fatty acids inhibit NF-kappaB activation via a PPARalpha-dependent pathway. Arterioscler Thromb Vasc Biol. 2004;24:1621–1627. doi: 10.1161/01.ATV.0000137191.02577.86. [DOI] [PubMed] [Google Scholar]
- 28.Sethi S, Ziouzenkova O, Ni H, Wagner DD, Plutzky J, Mayadas TN. Oxidized omega-3 fatty acids in fish oil inhibit leukocyte-endothelial interactions through activation of PPAR alpha. Blood. 2002;100:1340–1346. doi: 10.1182/blood-2002-01-0316. [DOI] [PubMed] [Google Scholar]
- 29.Collins T. Endothelial nuclear factor-kappa B and the initiation of the atherosclerotic lesion. Lab Invest. 1993;68:499–508. [PubMed] [Google Scholar]
- 30.Collins T, Read MA, Neish AS, Whitley MZ, Thanos D, Maniatis T. Transcriptional regulation of endothelial cell adhesion molecules: NF-kappa B and cytokine-inducible enhancers. FASEB J. 1995;9:899–909. [PubMed] [Google Scholar]
- 31.Weber C, Erl W, Pietsch A, Danesch U, Weber PC. Docosahexaenoic acid selectively attenuates induction of vascular cell adhesion molecule-1 and subsequent monocytic cell adhesion to human endothelial cells stimulated by tumor necrosis factor-alpha. Arterioscler Thromb Vasc Biol. 1995;15:622–628. doi: 10.1161/01.atv.15.5.622. [DOI] [PubMed] [Google Scholar]
- 32.Yamada H, Yoshida M, Nakano Y, et al. In vivo and in vitro inhibition of monocyte adhesion to endothelial cells and endothelial adhesion molecules by eicosapentaenoic acid. Arterioscler Thromb Vasc Biol. 2008;28:2173–2179. doi: 10.1161/ATVBAHA.108.171736. [DOI] [PubMed] [Google Scholar]
- 33.De Caterina R, Massaro M, Scoditti E, Annunziata Carluccio M. Pharmacological modulation of vascular inflammation in atherothrombosis. Ann N Y Acad Sci. 2010;1207:23–31. doi: 10.1111/j.1749-6632.2010.05784.x. [DOI] [PubMed] [Google Scholar]
- 34.Massaro M, Scoditti E, Carluccio MA, Campana MC, De Caterina R. Omega-3 fatty acids, inflammation and angiogenesis: basic mechanisms behind the cardioprotective effects of fish and fish oils. Cell Mol Biol (Noisy-le-grand) 2010;56:59–82. [PubMed] [Google Scholar]
- 35.De Caterina R, Cybulsky MI, Clinton SK, Gimbrone MA, Jr, Libby P. The omega-3 fatty acid docosahexaenoate reduces cytokine-induced expression of proatherogenic and proinflammatory proteins in human endothelial cells. Arterioscler Thromb. 1994;14:1829–1836. doi: 10.1161/01.atv.14.11.1829. [DOI] [PubMed] [Google Scholar]
- 36.De Caterina R, Cybulsky MA, Clinton SK, Gimbrone MA, Jr, Libby P. Omega-3 fatty acids and endothelial leukocyte adhesion molecules. Prostaglandins Leukot Essent Fatty Acids. 1995;52:191–195. doi: 10.1016/0952-3278(95)90021-7. [DOI] [PubMed] [Google Scholar]
- 37.Goua M, Mulgrew S, Frank J, Rees D, Sneddon AA, Wahle KW. Regulation of adhesion molecule expression in human endothelial and smooth muscle cells by omega-3 fatty acids and conjugated linoleic acids: involvement of the transcription factor NF-kappaB? Prostaglandins Leukot Essent Fatty Acids. 2008;78:33–43. doi: 10.1016/j.plefa.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 38.Tull SP, Yates CM, Maskrey BH, et al. Omega-3 fatty acids and inflammation: novel interactions reveal a new step in neutrophil recruitment. PLoS Biol. 2009;7:e1000177. doi: 10.1371/journal.pbio.1000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De Caterina R, Massaro M. Omega-3 fatty acids and the regulation of expression of endothelial pro-atherogenic and pro-inflammatory genes. J Membr Biol. 2005;206:103–116. doi: 10.1007/s00232-005-0783-2. [DOI] [PubMed] [Google Scholar]
- 40.Massaro M, Habib A, Lubrano L, et al. The omega-3 fatty acid docosahexaenoate attenuates endothelial cyclooxygenase-2 induction through both NADP(H) oxidase and PKC epsilon inhibition. Proc Natl Acad Sci U S A. 2006;103:15,184–15,189. doi: 10.1073/pnas.0510086103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thies F, Garry JM, Yaqoob P, et al. Association of n-3 polyunsaturated fatty acids with stability of atherosclerotic plaques: a randomised controlled trial. Lancet. 2003;361:477–485. doi: 10.1016/S0140-6736(03)12468-3. [DOI] [PubMed] [Google Scholar]
- 42.Nakajima K, Yamashita T, Kita T, et al. Orally administered eicosapentaenoic acid induces rapid regression of atherosclerosis via modulating the phenotype of dendritic cells in LDL receptor-deficient mice. Arterioscler Thromb Vasc Biol. 2011;31:1963–1972. doi: 10.1161/ATVBAHA.111.229443. [DOI] [PubMed] [Google Scholar]
- 43.Dyerberg J, Bang HO, Stoffersen E, Moncada S, Vane JR. Eicosapentaenoic acid and prevention of thrombosis and atherosclerosis? Lancet. 1978;ii:117–119. doi: 10.1016/s0140-6736(78)91505-2. [DOI] [PubMed] [Google Scholar]
- 44.Serhan CN, Hong S, Gronert K, et al. Resolvins: a family of bioactive products of omega-3 fatty acid transformation circuits initiated by aspirin treatment that counter proinflammation signals. J Exp Med. 2002;196:1025–1037. doi: 10.1084/jem.20020760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Serhan CN, Chiang N, Van Dyke TE. Resolving inflammation: dual anti-inflammatory and pro-resolution lipid mediators. Nat Rev Immunol. 2008;8:349–361. doi: 10.1038/nri2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Serhan CN, Yang R, Martinod K, et al. Maresins: novel macrophage mediators with potent antiinflammatory and proresolving actions. J Exp Med. 2009;206:15–23. doi: 10.1084/jem.20081880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Serhan CN, Brain SD, Buckley CD, et al. Resolution of inflammation: state of the art, definitions and terms. FASEB J. 2007;21:325–332. doi: 10.1096/fj.06-7227rev. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stables MJ, Gilroy DW. Old and new generation lipid mediators in acute inflammation and resolution. Prog Lipid Res. 2011;50:35–51. doi: 10.1016/j.plipres.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 49.Yedgar S, Krimsky M, Cohen Y, Flower RJ. Treatment of inflammatory diseases by selective eicosanoid inhibition: a double-edged sword? Trends Pharmacol Sci. 2007;28:459–464. doi: 10.1016/j.tips.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 50.Arita M, Bianchini F, Aliberti J, et al. Stereochemical assignment, antiinflammatory properties, and receptor for the omega-3 lipid mediator resolvin E1. J Exp Med. 2005;201:713–722. doi: 10.1084/jem.20042031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ho KJ, Spite M, Owens CD, et al. Aspirin-triggered lipoxin and resolvin E1 modulate vascular smooth muscle phenotype and correlate with peripheral atherosclerosis. Am J Pathol. 2010;177:2116–2123. doi: 10.2353/ajpath.2010.091082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tousoulis D, Papageorgiou N, Antoniades C, et al. Acute effects of different types of oil consumption on endothelial function, oxidative stress status and vascular inflammation in healthy volunteers. Br J Nutr. 2010;103:43–49. doi: 10.1017/S0007114509991346. [DOI] [PubMed] [Google Scholar]
- 53.Khan F, Elherik K, Bolton-Smith C, et al. The effects of dietary fatty acid supplementation on endothelial function and vascular tone in healthy subjects. Cardiovasc Res. 2003;59:955–962. doi: 10.1016/s0008-6363(03)00395-x. [DOI] [PubMed] [Google Scholar]
- 54.Fahs CA, Yan H, Ranadive S, et al. The effect of acute fish-oil supplementation on endothelial function and arterial stiffness following a high-fat meal. Appl Physiol Nutr Metab. 2010;35:294–302. doi: 10.1139/H10-020. [DOI] [PubMed] [Google Scholar]
- 55.Dangardt F, Osika W, Chen Y, et al. Omega-3 fatty acid supplementation improves vascular function and reduces inflammation in obese adolescents. Atherosclerosis. 2010;212:580–585. doi: 10.1016/j.atherosclerosis.2010.06.046. [DOI] [PubMed] [Google Scholar]
- 56.Morgan DR, Dixon LJ, Hanratty CG, et al. Effects of dietary omega-3 fatty acid supplementation on endothelium-dependent vasodilation in patients with chronic heart failure. Am J Cardiol. 2006;97:547–551. doi: 10.1016/j.amjcard.2005.08.075. [DOI] [PubMed] [Google Scholar]
- 57.Bloomer RJ, Larson DE, Fisher-Wellman KH, Galpin AJ, Schilling BK. Effect of eicosapentaenoic and docosahexaenoic acid on resting and exercise-induced inflammatory and oxidative stress biomarkers: a randomized, placebo controlled, cross-over study. Lipids Health Dis. 2009;8:36. doi: 10.1186/1476-511X-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.He K, Liu K, Daviglus ML, et al. Associations of dietary long-chain n-3 polyunsaturated fatty acids and fish with biomarkers of inflammation and endothelial activation (from the Multi-Ethnic Study of Atherosclerosis [MESA]) Am J Cardiol. 2009;103:1238–1243. doi: 10.1016/j.amjcard.2009.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lopez-Garcia E, Schulze MB, Manson JE, et al. Consumption of (n-3) fatty acids is related to plasma biomarkers of inflammation and endothelial activation in women. J Nutr. 2004;134:1806–1811. doi: 10.1093/jn/134.7.1806. [DOI] [PubMed] [Google Scholar]
- 60.Micallef MA, Munro IA, Garg ML. An inverse relationship between plasma n-3 fatty acids and C-reactive protein in healthy individuals. Eur J Clin Nutr. 2009;63:1154–1156. doi: 10.1038/ejcn.2009.20. [DOI] [PubMed] [Google Scholar]
- 61.Poudel-Tandukar K, Nanri A, Matsushita Y, et al. Dietary intakes of alpha-linolenic and linoleic acids are inversely associated with serum C-reactive protein levels among Japanese men. Nutr Res. 2009;29:363–370. doi: 10.1016/j.nutres.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 62.Niu K, Hozawa A, Kuriyama S, et al. Dietary long-chain n-3 fatty acids of marine origin and serum C-reactive protein concentrations are associated in a population with a diet rich in marine products. Am J Clin Nutr. 2006;84:223–229. doi: 10.1093/ajcn/84.1.223. [DOI] [PubMed] [Google Scholar]
- 63.Murakami K, Sasaki S, Takahashi Y, et al. Total n-3 polyunsaturated fatty acid intake is inversely associated with serum C-reactive protein in young Japanese women. Nutr Res. 2008;28:309–314. doi: 10.1016/j.nutres.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 64.Ohsawa M, Itai K, Onoda T, et al. Dietary intake of n-3 polyunsaturated fatty acids is inversely associated with CRP levels, especially among male smokers. Atherosclerosis. 2008;201:184–191. doi: 10.1016/j.atherosclerosis.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 65.Sundrarjun T, Komindr S, Archararit N, et al. Effects of n-3 fatty acids on serum interleukin-6, tumour necrosis factor-alpha and soluble tumour necrosis factor receptor p55 in active rheumatoid arthritis. J Int Med Res. 2004;32:443–454. doi: 10.1177/147323000403200501. [DOI] [PubMed] [Google Scholar]
- 66.Farzaneh-Far R, Harris WS, Garg S, Na B, Whooley MA. Inverse association of erythrocyte n-3 fatty acid levels with inflammatory biomarkers in patients with stable coronary artery disease: The Heart and Soul Study. Atherosclerosis. 2009;205:538–543. doi: 10.1016/j.atherosclerosis.2008.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.De Berrazueta JR, Gomez de Berrazueta JM, Amado Senaris JA, et al. A diet enriched with mackerel (Scomber scombrus)-derived products improves the endothelial function in a senior population (Prevención de las Enfermedades Cardiovasculares: Estudio Santoña–PECES project) Eur J Clin Invest. 2009;39:165–173. doi: 10.1111/j.1365-2362.2008.02072.x. [DOI] [PubMed] [Google Scholar]
- 68.Jackson KG, Armah CK, Doman I, James L, Cheghani F, Minihane AM. The impact of age on the postprandial vascular response to a fish oil-enriched meal. Br J Nutr. 2009;102:1414–1419. doi: 10.1017/S0007114509990742. [DOI] [PubMed] [Google Scholar]
- 69.Leaf A, Weber PC. Cardiovascular effects of n-3 fatty acids. N Engl J Med. 1988;318:549–557. doi: 10.1056/NEJM198803033180905. [DOI] [PubMed] [Google Scholar]
- 70.Harris WS. n-3 fatty acids and serum lipoproteins: human studies. Am J Clin Nutr. 1997;65:1645S–1654S. doi: 10.1093/ajcn/65.5.1645S. [DOI] [PubMed] [Google Scholar]
- 71.Sadovsky R, Kris-Etherton P. Prescription omega-3-acid ethyl esters for the treatment of very high triglycerides. Postgrad Med. 2009;121:145–153. doi: 10.3810/pgm.2009.07.2020. [DOI] [PubMed] [Google Scholar]
- 72.Kromhout D, Bosschieter EB, de Lezenne Coulander C. The inverse relation between fish consumption and 20-year mortality from coronary heart disease. N Engl J Med. 1985;312:1205–1209. doi: 10.1056/NEJM198505093121901. [DOI] [PubMed] [Google Scholar]
- 73.Harris WS, Poston WC, Haddock CK. Tissue n-3 and n-6 fatty acids and risk for coronary heart disease events. Atherosclerosis. 2007;193:1–10. doi: 10.1016/j.atherosclerosis.2007.03.018. [DOI] [PubMed] [Google Scholar]
- 74.Burr ML, Fehily AM, Gilbert JF, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART) Lancet. 1989;ii:757–761. doi: 10.1016/s0140-6736(89)90828-3. [DOI] [PubMed] [Google Scholar]
- 75.Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico. Lancet. 1999;354:447–455. [PubMed] [Google Scholar]
- 76.Yokoyama M, Origasa H, Matsuzaki M, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet. 2007;369:1090–1098. doi: 10.1016/S0140-6736(07)60527-3. [DOI] [PubMed] [Google Scholar]
- 77.Marik PE, Varon J. Omega-3 dietary supplements and the risk of cardiovascular events: a systematic review. Clin Cardiol. 2009;32:365–372. doi: 10.1002/clc.20604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Breslow JL. n-3 fatty acids and cardiovascular disease. Am J Clin Nutr. 2006;83:1477S–1482S. doi: 10.1093/ajcn/83.6.1477S. [DOI] [PubMed] [Google Scholar]
- 79.Hansen SN, Harris WS. New evidence for the cardiovascular benefits of long chain omega-3 fatty acids. Curr Atheroscler Rep. 2007;9:434–440. doi: 10.1007/s11883-007-0058-8. [DOI] [PubMed] [Google Scholar]
- 80.Harris WS, Miller M, Tighe AP, Davidson MH, Schaefer EJ. Omega-3 fatty acids and coronary heart disease risk: clinical and mechanistic perspectives. Atherosclerosis. 2008;197:12–24. doi: 10.1016/j.atherosclerosis.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 81.Von Schacky C, Harris WS. Cardiovascular benefits of omega-3 fatty acids. Cardiovasc Res. 2007;73:310–315. doi: 10.1016/j.cardiores.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 82.Hoy SM, Keating GM. Omega-3 ethylester concentrate: a review of its use in secondary prevention post-myocardial infarction and the treatment of hypertriglyceridaemia. Drugs. 2009;69:1077–1105. doi: 10.2165/00003495-200969080-00008. [DOI] [PubMed] [Google Scholar]
- 83.Roth EM, Harris WS. Fish oil for primary and secondary prevention of coronary heart disease. Curr Atheroscler Rep. 2010;12:66–72. doi: 10.1007/s11883-009-0079-6. [DOI] [PubMed] [Google Scholar]
- 84.Wang C, Harris WS, Chung M, et al. n-3 Fatty acids from fish or fish-oil supplements, but not alpha-linolenic acid, benefit cardiovascular disease outcomes in primary- and secondary-prevention studies: a systematic review. Am J Clin Nutr. 2006;84:5–17. doi: 10.1093/ajcn/84.1.5. [DOI] [PubMed] [Google Scholar]
- 85.Harris WS. The omega-3 index: clinical utility for therapeutic intervention. Curr Cardiol Rep. 2010;12:503–508. doi: 10.1007/s11886-010-0141-6. [DOI] [PubMed] [Google Scholar]
- 86.Harris WS. The omega-3 index: from biomarker to risk marker to risk factor. Curr Atheroscler Rep. 2009;11:411–417. doi: 10.1007/s11883-009-0062-2. [DOI] [PubMed] [Google Scholar]
- 87.Aarsetoey H, Aarsetoey R, Lindner T, Staines H, Harris WS, Nilsen DW. Low levels of the omega-3 index are associated with sudden cardiac arrest and remain stable in survivors in the subacute phase. Lipids. 2011;46:151–161. doi: 10.1007/s11745-010-3511-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Harris WS. The omega-3 index as a risk factor for coronary heart disease. Am J Clin Nutr. 2008;87:1997S–2002S. doi: 10.1093/ajcn/87.6.1997S. [DOI] [PubMed] [Google Scholar]
- 89.Von Schacky C, Harris WS. Cardiovascular risk and the omega-3 index. J Cardiovasc Med (Hagerstown) 2007;8(suppl 1):S46–49. doi: 10.2459/01.JCM.0000289273.87803.87. [DOI] [PubMed] [Google Scholar]
- 90.Rauch B, Schiele R, Schneider S, et al. OMEGA, a randomized, placebo-controlled trial to test the effect of highly purified omega-3 fatty acids on top of modern guideline-adjusted therapy after myocardial infarction. Circulation. 2010;122:2152–2159. doi: 10.1161/CIRCULATIONAHA.110.948562. [DOI] [PubMed] [Google Scholar]
- 91.Ishikawa Y, Yokoyama M, Saito Y, et al. Preventive effects of eicosapentaenoic acid on coronary artery disease in patients with peripheral artery disease. Circ J. 2010;74:1451–1457. doi: 10.1253/circj.cj-09-0520. [DOI] [PubMed] [Google Scholar]
- 92.Lane JS, Magno CP, Lane KT, Chan T, Hoyt DB, Greenfield S. Nutrition impacts the prevalence of peripheral arterial disease in the United States. J Vasc Surg. 2008;48:897–904. doi: 10.1016/j.jvs.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 93.Leng GC, Horrobin DF, Fowkes FG, et al. Plasma essential fatty acids, cigarette smoking, and dietary antioxidants in peripheral arterial disease. A population-based case–control study. Arterioscler Thromb. 1994;14:471–478. doi: 10.1161/01.atv.14.3.471. [DOI] [PubMed] [Google Scholar]
- 94.Woodcock BE, Smith E, Lambert WH, et al. Beneficial effect of fish oil on blood viscosity in peripheral vascular disease. Br Med J (Clin Res Ed) 1984;288:592–594. doi: 10.1136/bmj.288.6417.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gans RO, Bilo HJ, Weersink EG, et al. Fish oil supplementation in patients with stable claudication. Am J Surg. 1990;160:490–495. doi: 10.1016/s0002-9610(05)81012-8. [DOI] [PubMed] [Google Scholar]
- 96.Mori TA, Vandongen R, Mahanian F, Douglas A. Plasma lipid levels and platelet and neutrophil function in patients with vascular disease following fish oil and olive oil supplementation. Metabolism. 1992;41:1059–1067. doi: 10.1016/0026-0495(92)90286-j. [DOI] [PubMed] [Google Scholar]
- 97.Leng GC, Lee AJ, Fowkes FG, et al. Randomized controlled trial of gamma-linolenic acid and eicosapentaenoic acid in peripheral arterial disease. Clin Nutr. 1998;17:265–271. doi: 10.1016/s0261-5614(98)80318-x. [DOI] [PubMed] [Google Scholar]
- 98.Carrero JJ, Lopez-Huertas E, Salmeron LM, Baro L, Ros E. Daily supplementation with (n-3) PUFAs, oleic acid, folic acid, and vitamins B-6 and E increases pain-free walking distance and improves risk factors in men with peripheral vascular disease. J Nutr. 2005;135:1393–1399. doi: 10.1093/jn/135.6.1393. [DOI] [PubMed] [Google Scholar]
- 99.Conway K, Dillon M, Evans J, et al. Yearbook 2005. London: The Vascular Society of Great Britain & Ireland; 2005. A doubled-blinded, randomized study to determine the effect of omega-3-marine triglycerides on intermittent claudication. Abstract 86. [Google Scholar]
- 100.Sommerfield T, Price J, Hiatt WR. Omega-3 fatty acids for intermittent claudication. Cochrane Database Syst Rev. 2007:CD003833. doi: 10.1002/14651858.CD003833.pub3. [DOI] [PubMed] [Google Scholar]
- 101.Schiano V, Laurenzano E, Brevetti G, et al. Omega-3 polyunsaturated fatty acid in peripheral arterial disease: effect on lipid pattern, disease severity, inflammation profile, and endothelial function. Clin Nutr. 2008;27:241–247. doi: 10.1016/j.clnu.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 102.Madden J, Brunner A, Dastur ND, et al. Fish oil induced increase in walking distance, but not ankle brachial pressure index, in peripheral arterial disease is dependent on both body mass index and inflammatory genotype. Prostaglandins Leukot Essent Fatty Acids. 2007;76:331–340. doi: 10.1016/j.plefa.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 103.Madden J, Shearman CP, Dunn RL, et al. Altered monocyte CD44 expression in peripheral arterial disease is corrected by fish oil supplementation. Nutr Metab Cardiovasc Dis. 2009;19:247–252. doi: 10.1016/j.numecd.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 104.Luu NT, Madden J, Calder PC, et al. Dietary supplementation with fish oil modifies the ability of human monocytes to induce an inflammatory response. J Nutr. 2007;137:2769–2774. doi: 10.1093/jn/137.12.2769. [DOI] [PubMed] [Google Scholar]
- 105.Lichtenstein AH, Appel LJ, Brands M, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 106.Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation. 2002;106:2747–2757. doi: 10.1161/01.cir.0000038493.65177.94. [DOI] [PubMed] [Google Scholar]
- 107.Gupta A, Guyomard V, Zaman MJ, Rehman HU, Myint PK. Systematic review on evidence of the effectiveness of cholesterol-lowering drugs. Adv Ther. 2010;27:348–364. doi: 10.1007/s12325-010-0033-6. [DOI] [PubMed] [Google Scholar]
- 108.Department of Health and Human Services, US Food and Drug Administration. Substances affirmed as generally recognized as safe: menhaden oil. http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=184.1472 (revised 1 April 2011, accessed 3 October 2011)
- 109.Sacks FM, Stone PH, Gibson CM, Silverman DI, Rosner B, Pasternak RC. Controlled trial of fish oil for regression of human coronary atherosclerosis. HARP Research Group. J Am Coll Cardiol. 1995;25:1492–1498. doi: 10.1016/0735-1097(95)00095-l. [DOI] [PubMed] [Google Scholar]
- 110.Leaf A, Jorgensen MB, Jacobs AK, et al. Do fish oils prevent restenosis after coronary angioplasty? Circulation. 1994;90:2248–2257. doi: 10.1161/01.cir.90.5.2248. [DOI] [PubMed] [Google Scholar]
- 111.Von Schacky C, Angerer P, Kothny W, Theisen K, Mudra H. The effect of dietary omega-3 fatty acids on coronary atherosclerosis. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1999;130:554–562. doi: 10.7326/0003-4819-130-7-199904060-00003. [DOI] [PubMed] [Google Scholar]
- 112.De Gomez Dumm IN, Brenner RR. Oxidative desaturation of alpha-linoleic, linoleic, and stearic acids by human liver microsomes. Lipids. 1975;10:315–317. doi: 10.1007/BF02532451. [DOI] [PubMed] [Google Scholar]
- 113.Woo Lee Y, Joo Park H, Hennig B, Toborek M. Linoleic acid induces MCP-1 gene expression in human microvascular endothelial cells through an oxidative mechanism. J Nutr Biochem. 2001;12:648–654. doi: 10.1016/s0955-2863(01)00186-3. [DOI] [PubMed] [Google Scholar]
- 114.Bousserouel S, Brouillet A, Bereziat G, Raymondjean M, Andreani M. Different effects of n-6 and n-3 polyunsaturated fatty acids on the activation of rat smooth muscle cells by interleukin-1 beta. J Lipid Res. 2003;44:601–611. doi: 10.1194/jlr.M200092-JLR200. [DOI] [PubMed] [Google Scholar]
- 115.Tsimikas S, Philis-Tsimikas A, Alexopoulos S, Sigari F, Lee C, Reaven PD. LDL isolated from Greek subjects on a typical diet or from American subjects on an oleate-supplemented diet induces less monocyte chemotaxis and adhesion when exposed to oxidative stress. Arterioscler Thromb Vasc Biol. 1999;19:122–130. doi: 10.1161/01.atv.19.1.122. [DOI] [PubMed] [Google Scholar]
- 116.Fritsche KL. Too much linoleic acid promotes inflammation—doesn’t it? Prostaglandins Leukot Essent Fatty Acids. 2008;79:173–175. doi: 10.1016/j.plefa.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 117.Kris-Etherton P, Fleming J, Harris WS. The debate about n-6 polyunsaturated fatty acid recommendations for cardiovascular health. J Am Diet Assoc. 2010;110:201–204. doi: 10.1016/j.jada.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 118.Ramsden CE, Hibbeln JR, Lands WE. Letter to the Editor re: Linoleic acid and coronary heart disease. Prostaglandins Leukot Essent Fatty Acids (2008), by WS Harris. Prostaglandins Leukot Essent Fatty Acids. 2009;80:77. doi: 10.1016/j.plefa.2008.12.002. author reply 77–78. [DOI] [PubMed] [Google Scholar]
- 119.Tribole E. What happened to do no harm? The issue of dietary omega-6 fatty acids. Prostaglandins Leukot Essent Fatty Acids. 2009;80:78–79. doi: 10.1016/j.plefa.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 120.Ramsden CE, Hibbeln JR, Majchrzak SF, Davis JM. n-6 fatty acid-specific and mixed polyunsaturate dietary interventions have different effects on CHD risk: a meta-analysis of randomised controlled trials. Br J Nutr. 2010;104:1586–1600. doi: 10.1017/S0007114510004010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Calder PC. The American Heart Association advisory on n-6 fatty acids: evidence based or biased evidence? Br J Nutr. 2010;104:1575–1576. doi: 10.1017/S0007114510004253. [DOI] [PubMed] [Google Scholar]


