Abstract
Humor, or the perception or elicitation of mirth and funniness, is distinguishable from laughter and can be differentially disturbed by neuropsychiatric disease. We present two patients with constant joking, or Witzelsucht, in the absence of pseudobulbar affect and review the literature on pathological humor. These patients had involvement of frontal structures, impaired appreciation of non-simple humor, and a compulsion for disinhibited joking. Current neuroscience suggests impaired humor integration from right lateral frontal injury and disinhibition from orbitofrontal damage results in disinhibited humor preferentially activating limbic and subcortical reward centers. Additional frontal-subcortical circuit dysfunction may promote pathological joking as a compulsion.
INTRODUCTION
… So with the mind, something unexpected—a novel or incongruous idea which breaks through an habitual train of thought—appears to be a strong element in the ludicrous. (Darwin, 1872) {(1)}
Compared to other animals, humans are uniquely endowed with the ability to detect, decipher, and delight in humor. Charles Darwin and others suggested an evolutionary significance for the experiencing of something as funny or for finding something amusing {1}. An evolutionary basis compels a neurobiological explanation of humor, and suggests that disturbances in humor can result from neuropsychiatric disease. Importantly, humor is not the same as laughter. Although humor tends to elicit laughter, the processes for humor are distinct from the ability to laugh and, hence, from pseudobulbar affect (PBA) or pathological laughter in neurological disease {2, 3}.
Humor is a broad term that refers to anything that people say or do that is considered funny and that tends to make others laugh. Humor also includes the neurocognitive mechanisms for creating and perceiving humor and for responding to it with amusement {4}. The concept of “funny” is more limited and refers to anything that can lead to laughter, mirth, or amusement. In neuropsychiatric disease, humor is often impaired and, although usually decreased, in some conditions it leads to abnormal and compulsive joking, punning, or pranks.
We present two patients with brain disorders and alterations in the sense of humor characterized by intractable joking, and we review the growing neuroscience literature pertinent to this phenomenon. One patient had right frontal encephalomalacia plus a stroke of the left caudate, and the other had behavioral variant frontotemporal dementia (bvFTD) and prominent right frontal Pick bodies on autopsy. These patients had Witzelsucht, or excessive and often inappropriate joking and facetious humor {5}, and moria of Jastrowitz, or a childish or silly excitement {6}. Previously described from brain tumors, strokes, infections, and other lesions involving the frontal lobe, particularly the right orbitofrontal region {7}, Witzelsucht and moria can also be prominent manifestations of behavioral variant frontotemporal dementia (bvFTD) {8, 9}.
CASE REPORT No. 1
A 69 year-old right-handed man presented for a neuropsychiatric evaluation because of a 5-year history of compulsive joking. Ten years prior to presentation, he had a subarachnoid hemorrhage (SAH) of undetermined etiology. The SAH was complicated by hydrocephalus, placement of a right ventriculoperitoneal (VP) shunt, and a small area of perishunt encephalomalacia in the right frontal region (Figure 1a). Afterwards, he was left with a personality change. He became compulsive, with a fixation on recycling to the point where he would go through dumpsters searching for recyclable items, and he developed hoarding behaviors, collecting napkins and utensils from restaurants and other locations.
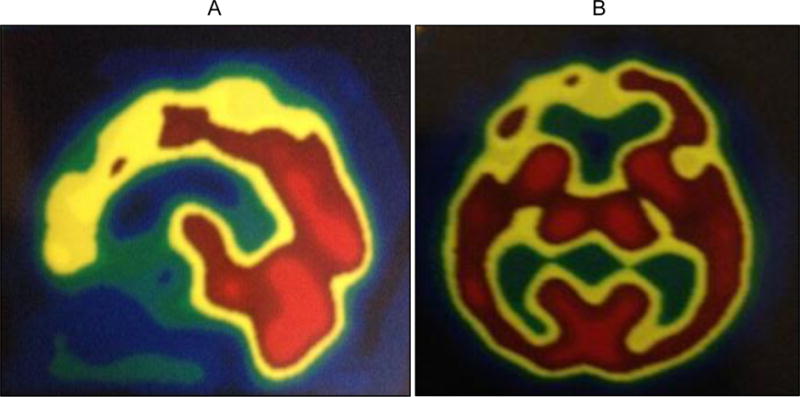
FIGURE 1.

Brain MRI scan (FLAIR sequences). A) Right trans-frontal ventriculoperitoneal shunt, with the tip in the region of the right foramen of Monro. There is a focus of hypodensity in the right frontal lobe, including the superior frontal gyrus (SFG) and extending to the anterior body of the right lateral ventricle. It is adjacent to a small right frontal surgical burr-hole. B) More recent lacunar infarction in the head of the left caudate nucleus, a structure that mediates frontal-subcortical tracts.
Five years after this event, he again had a fairly abrupt behavioral change, this time with the development of constant joking along with disinhibition. He became affectionate towards younger females, hugging them for “too long”, made borderline offensive comments, and took candy from stores without paying, getting caught on several occasions. A repeat neurological evaluation with magnetic resonance imaging (MRI) revealed a new lacunar stroke in the head of the left caudate nucleus (Figure 1b).
On interview, the patient reported feeling generally joyful, but his compulsive need to make jokes and create humor had become an issue of contention with his wife. He would wake her up in the middle of the night bursting out in laughter, just to tell her about the jokes he had come up with. Upon the request of his wife, he started writing down these jokes as a way to avoid waking her; he brought to our office approximately 50 pages filled with his jokes, most of which were either puns or silly jokes with a sexual or scatological content (Table 1). His past medical history was positive for prior depression, absent for the preceding 10 years.
Table 1.
Examples of jokes for case report No.1
| STORYLINE | PUNCHLINE |
|---|---|
| 1) How do you cure hunger? | Step away from the buffet table. |
| 2) What is a pill-popping sexual molester guilty of? | Rape and pillage. |
| 3) What did the proctologist say to his therapist? | All day long I am dealing with A**holes. |
| 4) Went to the Department of Motor Vehicles to get my driver’s license. They gave me an eye exam and here is what they said: | ABCDEFG, HIJKMNLOP, QRS, TUV, WXY and Z; now I know my ABC’s, can I have my license please. |
On examination, he had frequent episodes of joking with prominent laughter. Although he would laugh at his own jokes or witticisms, his laughter was neither uncontrollable nor involuntary. His Mini-Mental State Examination (MMSE) score was 29/30 (missed one recall item). The language examination was normal, and he generated a list of 25 animals/minute and 24 “F” words/minute (including expletives). On memory testing he was able to recall 7 out of 10 words on 15-minute delayed recall. He was intact on calculations, praxis, and frontal system tasks, but he misplaced the hands on a clock drawing test. He was normal on idiom and proverb interpretation, and he had full insight into his excessive joking behavior and humor. His neurological examination was remarkable for some difficulty with tandem gait manifested as a subtle loss of balance. Neuropsychological testing showed difficulties in frontal-executive functions, such as response inhibition, self-monitoring, and task-monitoring.
On further testing, he showed increased humor production, normal identification of humor in jokes, but a decreased affective appreciation of “funniness”. On a 24-point self-descriptive scale for sense of humor, the patient’s scores suggested significantly elevated humor creativity. On the “Joke and Story Completion Test”, a multiple choice test of humor appreciation {10, 11}, the patient was able to correctly identify the punchlines of 16 jokes. Despite his correct recognition of the funny endings, he did not laugh or report them as feeling funny. Additional testing with other jokes confirmed the same ability to identify the funny line but without laughing or experiencing it as funny.
He did not respond to selective serotonin reuptake inhibitor (SSRI) medications and trazodone, but he had a partial response to dextromethorphan 20mg/quinidine 10 mg titrated to twice a day. On this medication, the patient had a significant reduction in the frequency and duration of his episodes of laughter but without any effects on his compulsive need to constantly make and tell jokes. He remained stable, without progression, on this regimen.
CASE REPORT No. 2
A 57-year-old right-handed man presented for evaluation of a three-year history of the insidious onset and progression of behavioral changes. The patient had become a “jokester”, always making childish jokes or comments and laughing easily at his own comments. He had also become disinhibited, saying or doing things that were inappropriate and demonstrating excessive familiarity with strangers. He lost his job after blurting out, “Who the hell chose this God-awful place?” In addition, without invitations, he would walk into his coworkers’ offices and defrag their computers and walk into a neighbor’s home and play their piano.
Further changes included prominent compulsive behavior along with dietary changes and a decline in his hygiene. His wife found dozens of coffee grinders and almost two dozen Hawaiian shirts accumulated in their garage. He had changes in his eating behavior where he would eat the exact same thing over and over again and became obsessed with certain fast foods. At one point he had not bathed for at least six weeks and when he was asked to do so, his response was, “Chinese people don’t have body odor” (he was of Asian descent). Past medical history was negative except for an appendectomy and tonsillectomy, and his family history was otherwise unremarkable.
On examination, he would frequently break out in laughter, almost cackling, at his own comments, opinions, or jokes, many of which were borderline sexual or political in content. On the MMSE, he scored 29 out of 30, missing only the exact day of the week. Language was fluent with good auditory comprehension, repetition, and confrontational naming. He generated a word list of 20 animals in a minute and 19 “F” words in a minute. On memory testing, he got 0 out of 10 words spontaneously at 15 minutes, but all 10 on a recognition task. He had very good memory for current events. The patient had normal performances on visuospatial, simple calculation, and ideomotor praxis tasks. He was concrete on some proverb interpretations, and he showed no insight into his disease or behavioral changes. Neuropsychological testing found executive deficits and decreased memory retrieval. The rest of the neurologic examination was normal.
This patient had progressive behavioral changes consistent with bvFTD. Although his MRI was within normal limits, brain single photon emission tomography (SPECT) imaging showed relative frontal hypoperfusion (Figure 2). On subsequent follow-up visits, he continued to make frequent comments and jokes, at times acting quite silly, childish, and inappropriate. For example, on one clinic visit he began disco dancing; on another he publicly discussed his sexual situation; and at a third visit he grabbed the examiner’s tie and that of a passing physician and started to compare them. Throughout these behaviors, the patient would quickly lapse into laughter. Yet, he did not laugh or consider funny any jokes or witticisms presented to him, despite being able to recognize most of the punchlines. He remained jovial despite trials of SSRI medications, and he continued to deteriorate in cognition and developed parkinsonism.
FIGURE 2.
A) Brain single photon emission tomography (SPECT) imaging (sagittal view) showing frontal hypometabolism, and B) SPECT imaging (axial view) showing asymmetrical frontal hypometabolism, right > left.
The patient died 11-12 years into his course, and his autopsy showed Pick’s disease (a form of bvFTD). He had asymmetric frontotemporal atrophy, severe in frontal lobes and moderate in temporal lobes, affecting the right more than the left side. He had tau-immunoreactive intracytoplasmic inclusions consistent with Pick bodies in neurons involving frontal and temporal neocortex, along with associated overwhelming neuronal loss and severe gliosis.
DISCUSSION
“Humor can be dissected as a frog can, but the thing dies in the process and the innards are discouraging to any but the pure scientific mind.” (E.B. White, 1941) {12}
These two patients had pathological humor or compulsive need for joking from bifrontal dysfunction, most critically from involvement of the right frontal lobe. Both patients had bifrontal damage, suggesting that both right and left frontal involvement is necessary for pathological humor. In the first case it followed a stroke in the head of the left caudate nucleus, an area which mediates frontosubcortical tracts, in a patient with prior compulsive behavior associated with right frontal encephalomalacia. The other patient had bvFTD with right greater than left frontotemporal Pick’s disease on neuropathology. Both patients were consumed with a compulsive tendency for disinhibited jokes to the point of disturbing their families and others. On examination, both were able to detect jokes and identify them as funny, but they did not experience or feel others’ jokes as funny or amusing. In essence, their humor was entirely internally-driven.
These patients’ compulsive need to make inappropriate jokes and to act childishly are consistent with “Witzelsucht”, from the German words for joke (Witz) and addiction (Sucht), and “moria”, or inappropriate cheerfulness. In the late 1880’s, Herman Oppenheim described an addiction to trivial, excessive and often sarcastic joking among four patients with right frontal lobe tumors {5}, and Moritz Jastrowitz described silly and excited behavior in a patient with a large right frontal tumor {6}. At the time, neuropathological studies of patients with similar acquired changes in personality showed involvement of the orbitofrontal and mesial frontal regions bilaterally, but particularly on the right {13}. More recent reports have also emphasized involvement of the right hemisphere with Witzelsucht {14}. The paradox of Witzelsucht and moria is that these patients are actually insensitive to non-self generated humor. Even when they recognize and understand a joke, they do not affectively respond with a sense of mirth or with laughter. In other words, they do not feel the punchline as humorously connected to the storyline, yet simple forms of humor that do not require integration of a punchline, such as slapstick and puns, may still be experienced as funny.
There are many neuropsychiatric causes of pathological humor or Witzelsucht. Frontal lesions, like those described in our two patients, may result from brain trauma and other neurodegenerative diseases as well as from focal lesions. Dementias, particularly if frontally-predominant, can increase the production of humor, as well as decrease the sense of humor. In particular, patients with bvFTD, especially if right predominant, may have a tendency to Witzelsucht, moria, slapstick, scatological jokes or compulsive punning, along with decreased comprehension of complex or unfamiliar humor {8, 9, 15}. There are also developmental or genetic causes for pathological humor, such as Angelman or the “happy puppet’ syndrome, Williams syndrome, and Down’s syndrome. In autism, although there is deficient humor processing linked to social or socioemotional aspects of humor, there can be a prominently retained predilection for physical humor and slapstick.
On initial presentation, clinicians must distinguish pathological humor or Witzelsucht from pathological laughter or pseudobulbar affect (PBA) {2, 3}. PBA may result in episodic, paroxysmal laughing, crying or mixed, from release of the dorsal upper pons laughter-coordinating center by bilateral upper motor neuron disease from strokes, amyotrophic lateral sclerosis, multiple sclerosis, traumatic brain injury, Parkinson’s Disease, multisystem atrophy, or progressive supranuclear palsy {2}. PBA is distinguishable from pathological humor in that its laughter is triggered by trivial or minimal stimuli and is often excessive and incongruent with the underlying mood and the extent of the patient’s emotional experience. A related unilateral condition is “fou rire prodromique”, or unmotivated, inappropriate, uncontrollable hearty laughter as the first symptom of cerebral ischemia that affects the inhibitory neurons for laughter in ventral pons, left internal capsule-thalamus, left basal ganglia, or left parahipppocampal gyrus. Finally, epilepsy and electrical stimulation can lead to gelastic seizures or brief, stereotyped (mechanical, unnatural) epileptic laughter, usually from the left hypothalamic hamartomas, hypothalamic extension of other tumors, or left frontal or temporal lobe foci {16–18}.
Understanding the origin and nature of humor facilitates understanding the origin of pathological humor. In observing the relaxed, open-mouth display in primates during rough-and-tumble play in chimpanzees, Darwin suggested that a novel or incongruous experience that surprises but is not a real threat leads to humor {19}. In a psychoanalytic elaboration of this idea, Sigmund Freud suggested that humor is an attitude (defense) by which people refuse to suffer by emphasizing the invincibility of their egos to provocation or reality {20}. It involves the superego in the moment of humor reassuring the ego that the world is not dangerous, an occasion to gain pleasure and reassert the pleasure principle. Several subsequent theories propose that humor is a “stress antagonist” able to enhance the immune, cardiovascular and endocrine systems and decrease stress-induced cortisol levels {21–23}; a signal detector of “false alarms” that communicates non-threatening deviations from the rules or mistakes in reasoning {24, 25}; a mechanism for social gain, promoting social exploration {26, 27}, social superiority {27}, or even sexual selection of a mate {26, 28, 29}. All of these theories, however, lack a neurocognitive explanation.
The most prominent neurocognitive theory of humor is the “Incongruity Theory” (Figure 3), which begins with detection and resolution of conflicting alternatives in the frontal lobes followed by humor appreciation in pleasure/reward areas {30–32}. First, one must “get the joke” (humor comprehension), which involves detection of the incongruity of the punchline with the joke. The experience of surprise signals that the joke expectations are incongruent with the punchline. Surprise then precipitates a search for alternative explanations, or incongruity resolution. The arrival at a new explanation is the trigger to humor elaboration or appreciation, the emotionally pleasurable responses that are experienced as amusement or laughter {10, 24, 30, 31, 33}.
FIGURE 3.
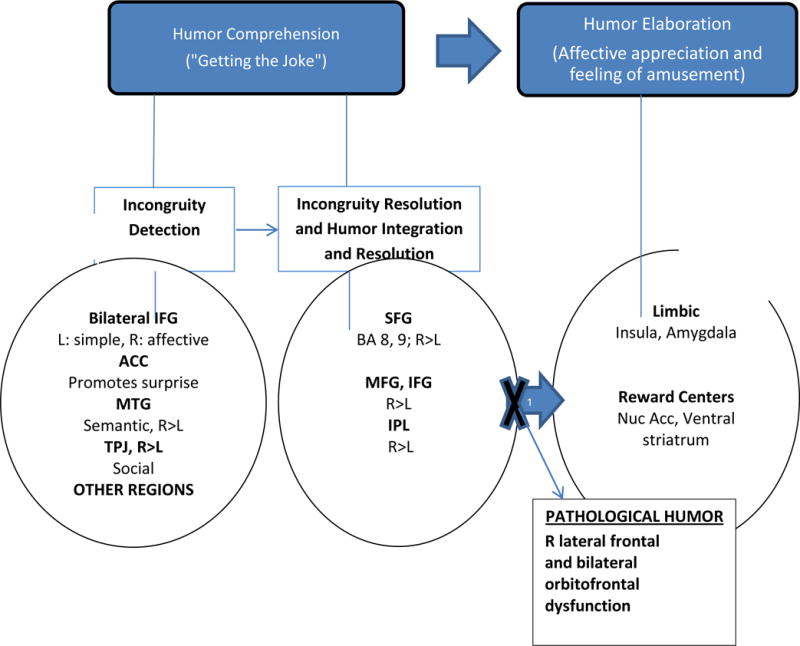
The comprehension-elaboration theory of humor. R = right; L = left; MTG = middle temporal gyrus; MFG = medial frontal gyrus; IFG = inferior frontal gyrus; SFG = superior frontal gyrus; ACC = anterior cingulate cortex; IPL = inferior parietal lobule; vmPFC = ventromedial prefrontal gyrus; PHG = parahippocampal gyrus; Amg = amygdala; TPJ = temporoparietal junction; BA = Broca’s area; Nuc Acc = Nucleus accumbens.
Arrow No. 1: Incongruity detection and resolution leads to humor elaboration, i.e., getting the joke and triggering amusement, respectively.
Pathological Humor: Right frontal defect in humor resolution and/or appreciation plus compulsive, disinhibited humor from bilateral OFC lesion.
Significantly modified from: Towards a neural circuit model of verbal humor processing: An fMRI study of the neural substrates on incongruity detection and resolution, Chan Y-C, et al. Neuroimage 2013;66: 169-176.
Neuroscience and functional neuroimaging suggest that many brain regions can be involved in the incongruity theory of humor {26, 31, 34, 35}. It is likely that both left and right frontal lobes have a role in incongruity detection and incongruity resolution, with the left frontal lobe more responsive to simple humor and the right engaged with more externally-generated, complex humor {30, 34}. Simple humor engages the left frontal lobe [the inferior frontal gyri (IFG)], with input from the medial temporal gyri (MTG) {11,15, 32, 36}. Examples of “simple humor” include the early detection of basic norm violations and plausibility, physical humor, slapstick, puns, familiar humor, and congruent but unfunny endings. Complicated humor, such as verbal semantic jokes requiring reconciliation with stored knowledge, also activates the right frontal and right MTG regions {38, 39}. In addition, humor that specifically involves deviations from social expectations engages the left frontal lobe [the superior frontal gyri (SFG)] and the temporoparietal junction (TPJ) on the right {26, 35, 37}, part of the circuitry involved in taking another’s perspective, or Theory of Mind (ToM). Finally, investigators agree that all types of humor require the right frontal lobe, including the ventromedial prefrontal cortex (vmPFC) and adjacent anterior cingulate cortex (ACC) for surprise when something is unexpected {26, 40}, and the triggering of humor appreciation through frontal connections with limbic (insulae, amygdalae) and dopaminergic reward (nucleus accumbens, ventral striatum) areas {26, 30–32, 38, 41, 42}.
Although bifrontal injury is usually present, damage to the right frontal lobe appears critical for pathological humor. Patients with right frontal lesions remain sensitive to simple jokes, slapstick, or puns {43, 44}, but they are impaired in appreciating externally-generated, non-simple, or novel jokes. They may not appreciate the relationship of their punchlines to their storylines and do not experience their funniness, prefering non-funny endings {10, 11, 43–45}. Hence, patients with right frontal lesions, like those with bvFTD {15}, are prone to simple, silly jokes {46}. These findings suggest that damage to the right dorsolateral/ventrolateral frontal lobe, possibly SFG but also MFG and IFG, impairs the integration of externally-generated humor so that it can be experienced as funny {35, 36, 45, 47}. In patients with the joking disease, concomitant disinhibition from orbitofrontal cortex (OFC) damage {48} permits self-generated and disinhibited jokes, rather than externally-generated humor, to be the main trigger of limbic and reward areas for humor appreciation, implying a self vs. other referential network for humor, as in ToM. Moreover, these patients appear compulsively driven to make jokes, suggesting additional damage to frontal (OFC-ACC)-striatal circuits involved in inhibitory control {49}.
There are no evidence-based pharmacological treatments for pathological humor, but published data on the treatment of disinhibition in different psychiatric and neurological conditions may apply to the treatmento of patients with Witzelsucht. The first medications to try are the SSRI’s, which were unsuccessful in decreasing pathological humor in these two patients, followed by psychoactive antiseizure medications such as valproate, carbamazepine, and lamotrigine. The use of dextromethorphan/quindine, a combination indicated for pathological laugther, may reduce the amount of laughter without altering the need for humor, as was the case with our first patient. Finally, when these medications fail and further treatment trials are indicated, clinicians may resort to low dose atypical antipsychotics to relieve the impact of the pathological humor {50}.
We conclude that pathological humor is a compulsion for disinhibited humor. In our first patient, the compulsive drive developed after the initial right frontal lesion, but the focus of his compulsions on disinhibited jokes did not occur until after OFC-subcortical tract dysfunction from his left caudate stroke. Both patients had decreased appreciation of externally-generated jokes associated with right lateral frontal dysfunction, and a compulsive drive for disinhibited, self-generated joking and humor associated with OFC disease {51, 52}. Future research can further clarify the mechanism and suggest management of Witzelsucht and moria in neuropsychiatric disease.
Acknowledgments
This work was supported by U.S. National Institute on Aging (NIA) grant R01AG034499.
References
- 1.Darwin C. The expression of emotions in man and animals. London: Julian Friedmann, New York, St. Martin’s Press; 1979. p. xiii, 374. p 6 leaves of plates. [Google Scholar]
- 2.Parvizi J, et al. Neuroanatomy of pathological laughing and crying: a report of the American Neuropsychiatric Association Committee on Research. J Neuropsychiatry Clin Neurosci. 2009;21(1):75–87. doi: 10.1176/jnp.2009.21.1.75. [DOI] [PubMed] [Google Scholar]
- 3.Lauterbach EC, Cummings JL, Kuppuswamy PS. Toward a more precise, clinically–informed pathophysiology of pathological laughing and crying. Neurosci Biobehav Rev. 2013;37(8):1893–916. doi: 10.1016/j.neubiorev.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Martin RA. The Psychology of Humor: An Integrative Approach. Elsevier Academic Press; 2007. [Google Scholar]
- 5.Oppenheim H. Zur patholologie der grosshirngeschwülste. Arch Psychiat. 1889;21:560–578. [Google Scholar]
- 6.Jastrowitz M. Beiträge zur Localisation im Grosshirn and über deren praktische Verwerthung. Dtsch Med Wochenschr. 1888;14:81. [Google Scholar]
- 7.Vardi J, et al. L’homme qui rit: inappropriate laughter and release phenomena of the frontal subdominant lobe. Behav Med. 1994;20(1):44–6. doi: 10.1080/08964289.1994.9934615. [DOI] [PubMed] [Google Scholar]
- 8.Mendez MF. Moria and Witzelsucht from frontotemporal dementia. J Neuropsychiatry Clin Neurosci. 2005;17(3):429–30. doi: 10.1176/jnp.17.3.429. [DOI] [PubMed] [Google Scholar]
- 9.Ehrle N, et al. Assessment of sociocognitive functions in neurological patients Presentation of a French adaptation of two tools and implementation in frontal dementia} Geriatr Psychol Neuropsychiatr Vieil. 2011;9(1):117–28. doi: 10.1684/pnv.2010.0252. [DOI] [PubMed] [Google Scholar]
- 10.Brownell HH, et al. Surprise but not coherence: sensitivity to verbal humor in right-hemisphere patients. Brain Lang. 1983;18(1):20–7. doi: 10.1016/0093-934x(83)90002-0. [DOI] [PubMed] [Google Scholar]
- 11.Bihrle AM, et al. Comprehension of humorous and nonhumorous materials by left and right brain-damaged patients. Brain Cogn. 1986;5(4):399–411. doi: 10.1016/0278-2626(86)90042-4. [DOI] [PubMed] [Google Scholar]
- 12.White EB, White KSA. A subtreasury of American humor. New York: Coward-McCann; 1941. pp. 3–814. xxxii p, 2 l. [Google Scholar]
- 13.Welt L. Über Charakterveränderungen des Menschen infolge von Läsionen des Stirnhirns. Deutsch Arch f Klin Med. 1888;42:339–390. [Google Scholar]
- 14.Chen YC, Tseng CY, Pai MC. Witzelsucht after right putaminal hemorrhage: a case report. Acta Neurol Taiwan. 2005;14(4):195–200. [PubMed] [Google Scholar]
- 15.Clark CN, et al. Humour processing in frontotemporal lobar degeneration: A behavioural and neuroanatomical analysis. Cortex. 2015;69:47–59. doi: 10.1016/j.cortex.2015.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tran TP, et al. Different localizations underlying cortical gelastic epilepsy: case series and review of literature. Epilepsy Behav. 2014;35:34–41. doi: 10.1016/j.yebeh.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 17.Fernandez-Baca Vaca G, et al. Mirth and laughter elicited during brain stimulation. Epileptic Disord. 2011;13(4):435–40. doi: 10.1684/epd.2011.0480. [DOI] [PubMed] [Google Scholar]
- 18.Yamao Y, et al. Neural correlates of mirth and laughter: a direct electrical cortical stimulation study. Cortex. 2015;66:134–40. doi: 10.1016/j.cortex.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 19.Darwin C. The Expression of Emotion in Man and Animals. United Kingdom: John Murray; 1872. [Google Scholar]
- 20.Freud S. Jokes and their relation to the unconscious. F. Deuticke; 1905. [Google Scholar]
- 21.Bennett MP, et al. The effect of mirthful laughter on stress and natural killer cell activity. Altern Ther Health Med. 2003;9(2):38–45. [PubMed] [Google Scholar]
- 22.Berk LS, et al. Neuroendocrine and stress hormone changes during mirthful laughter. Am J Med Sci. 1989;298(6):390–6. doi: 10.1097/00000441-198912000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Fredrickson BL, Levenson RW. Positive Emotions Speed Recovery from the Cardiovascular Sequelae of Negative Emotions. Cogn Emot. 1998;12(2):191–220. doi: 10.1080/026999398379718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramachandran VS. The neurology and evolution of humor, laughter, and smiling: the false alarm theory. Med Hypotheses. 1998;51(4):351–4. doi: 10.1016/s0306-9877(98)90061-5. [DOI] [PubMed] [Google Scholar]
- 25.Hurley MM, Dennett DC, Adams RB. Inside Jokes: Using Humor to Reverse-Engineer the Mind. MIT Press; 2011. [Google Scholar]
- 26.Vrticka P, Black JM, Reiss AL. The neural basis of humour processing. Nat Rev Neurosci. 2013;14(12):860–8. doi: 10.1038/nrn3566. [DOI] [PubMed] [Google Scholar]
- 27.Wilkins J, Eisenbraun AJ. Humor theories and the physiological benefits of laughter. Adv Mind Body Med. 2009;24(2):8–12. [PubMed] [Google Scholar]
- 28.Gervais M, Wilson DS. The evolution and functions of laughter and humor: a synthetic approach. Q Rev Biol. 2005;80(4):395–430. doi: 10.1086/498281. [DOI] [PubMed] [Google Scholar]
- 29.Wilbur CJ, Campbell L. Humor in romantic contexts: do men participate and women evaluate? Pers Soc Psychol Bull. 2011;37(7):918–29. doi: 10.1177/0146167211405343. [DOI] [PubMed] [Google Scholar]
- 30.Chan YC, et al. Towards a neural circuit model of verbal humor processing: an fMRI study of the neural substrates of incongruity detection and resolution. Neuroimage. 2013;66:169–76. doi: 10.1016/j.neuroimage.2012.10.019. [DOI] [PubMed] [Google Scholar]
- 31.Chan YC, et al. Segregating the comprehension and elaboration processing of verbal jokes: an fMRI study. Neuroimage. 2012;61(4):899–906. doi: 10.1016/j.neuroimage.2012.03.052. [DOI] [PubMed] [Google Scholar]
- 32.Moran JM, et al. Neural correlates of humor detection and appreciation. Neuroimage. 2004;21(3):1055–60. doi: 10.1016/j.neuroimage.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 33.Wyer RS, Jr, Collins JE., 2nd A theory of humor elicitation. Psychol Rev. 1992;99(4):663–88. doi: 10.1037/0033-295x.99.4.663. [DOI] [PubMed] [Google Scholar]
- 34.Wild B, et al. Neural correlates of laughter and humour. Brain. 2003;126(Pt 10):2121–38. doi: 10.1093/brain/awg226. [DOI] [PubMed] [Google Scholar]
- 35.Clark C, Warren J. The Neurology of Humour. Advances in Clinical Neuroscience and Rehabilitation. 2014;13(7):9–11. [Google Scholar]
- 36.Marinkovic K, et al. Right hemisphere has the last laugh: neural dynamics of joke appreciation. Cogn Affect Behav Neurosci. 2011;11(1):113–30. doi: 10.3758/s13415-010-0017-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Samson AC, Zysset S, Huber O. Cognitive humor processing: different logical mechanisms in nonverbal cartoons–an fMRI study. Soc Neurosci. 2008;3(2):125–40. doi: 10.1080/17470910701745858. [DOI] [PubMed] [Google Scholar]
- 38.Goel V, Dolan RJ. The functional anatomy of humor: segregating cognitive and affective components. Nat Neurosci. 2001;4(3):237–8. doi: 10.1038/85076. [DOI] [PubMed] [Google Scholar]
- 39.Gold BT, Buckner RL. Common prefrontal regions coactivate with dissociable posterior regions during controlled semantic and phonological tasks. Neuron. 2002;35(4):803–12. doi: 10.1016/s0896-6273(02)00800-0. [DOI] [PubMed] [Google Scholar]
- 40.Egner T. Surprise! A unifying model of dorsal anterior cingulate function? Nat Neurosci. 2011;14(10):1219–20. doi: 10.1038/nn.2932. [DOI] [PubMed] [Google Scholar]
- 41.Mobbs D, et al. Humor modulates the mesolimbic reward centers. Neuron. 2003;40(5):1041–8. doi: 10.1016/s0896-6273(03)00751-7. [DOI] [PubMed] [Google Scholar]
- 42.Shibata M, Terasawa Y, Umeda S. Integration of cognitive and affective networks in humor comprehension. Neuropsychologia. 2014;65:137–45. doi: 10.1016/j.neuropsychologia.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 43.Heath RL, Blonder LX. Spontaneous humor among right hemisphere stroke survivors. Brain Lang. 2005;93(3):267–76. doi: 10.1016/j.bandl.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 44.Gardner H, et al. Comprehension and appreciation of humorous material following brain damage. Brain. 1975;98(3):399–412. doi: 10.1093/brain/98.3.399. [DOI] [PubMed] [Google Scholar]
- 45.Shammi P, Stuss DT. Humour appreciation: a role of the right frontal lobe. Brain. 1999;122(Pt 4):657–66. doi: 10.1093/brain/122.4.657. [DOI] [PubMed] [Google Scholar]
- 46.Gainotti G. Emotional behavior and hemispheric side of the lesion. Cortex. 1972;8(1):41–55. doi: 10.1016/s0010-9452(72)80026-1. [DOI] [PubMed] [Google Scholar]
- 47.Daffner KR, et al. Disruption of attention to novel events after frontal lobe injury in humans. J Neurol Neurosurg Psychiatry. 2000;68(1):18–24. doi: 10.1136/jnnp.68.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Starkstein SE, Robinson RG. Mechanism of disinhibition after brain lesions. J Nerv Ment Dis. 1997;185(2):108–14. doi: 10.1097/00005053-199702000-00007. [DOI] [PubMed] [Google Scholar]
- 49.de Wit SJ, et al. Multicenter voxel-based morphometry mega-analysis of structural brain scans in obsessive-compulsive disorder. Am J Psychiatry. 2014;171(3):340–9. doi: 10.1176/appi.ajp.2013.13040574. [DOI] [PubMed] [Google Scholar]
- 50.Arciniegas DB, Wortzel HS. Emotional and behavioral dyscontrol after traumatic brain injury. Psychiatr Clin North Am. 2014;37(1):31–53. doi: 10.1016/j.psc.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 51.Bechara A, Damasio H, Damasio AR. Emotion, decision making and the orbitofrontal cortex. Cereb Cortex. 2000;10(3):295–307. doi: 10.1093/cercor/10.3.295. [DOI] [PubMed] [Google Scholar]
- 52.Hornberger M, Geng J, Hodges JR. Convergent grey and white matter evidence of orbitofrontal cortex changes related to disinhibition in behavioural variant frontotemporal dementia. Brain. 2011;134(Pt 9):2502–12. doi: 10.1093/brain/awr173. [DOI] [PubMed] [Google Scholar]


