Abstract
Juvenile justice involved youth face disproportionate rates of sexual abuse, which increases the risk for Post-Traumatic Stress Disorder (PTSD) and substance use disorders (SUDs), both of which are associated with poor long-term outcomes. The present study tested two mediation and moderation models, controlling for age, race, and history of physical abuse, with gender as a moderator, to determine if PTSD symptoms serve as a risk factor and/or mechanism in the relationship between sexual abuse and substance use. Data were examined for 197 juvenile justice involved youth (mean age = 15.45, 68.9% non-white, 78.4% male) that completed court-ordered psychological assessments. Results indicated that PTSD symptoms significantly mediated the relationship between sexual abuse and drug (β = 3.44, CI 0.26 to 7.41; Test for indirect effect z = 2.41, p = .02) and alcohol use (β = 1.42, CI 0.20 to 3.46; Test for indirect effect z = 2.23, p = .03). PTSD symptoms and gender were not significant moderators. Overall, PTSD symptoms mediate the relationship between sexual abuse and SUDs in juvenile justice involved youth, which suggests viability of targeting PTSD symptoms as a modifiable risk factor to reduce the effects of sexual abuse on substance use in this high-risk population.
Keywords: sexual abuse, substance use, PTSD, youth, juvenile justice
1. Introduction
Substance use disorders (SUDs) occur in approximately 60% of juvenile justice involved youth (SAMHSA, 2016; Teplin et al., 2005). This is particularly problematic as juvenile justice involved youth with SUDs face a host of negative outcomes, some of which include increased likelihood of having a co-occurring severe mental illness (e.g., manic episode and psychosis; Teplin, Abram, McClelland, Dulcan, & Mericle, 2002), increased likelihood of recidivism (McClelland et al., 2009; Conrad, Tolou-Shams, Rizzo, Placella, & Brown, 2014), and increased likelihood of engagement in sexual risk taking behaviors, compared to youth in the general population (Teplin et al., 2005). Although there are multiple potential explanations for the high prevalence of SUDs in this population, such as genetic risk or social norms in line with substance use (Kendler, Prescott, Myers, & Neale, 2003), emerging research suggests sexual abuse victimization may be one risk factor for the development of SUDs in juvenile justice involved youth.
The prevalence of sexual abuse victimization in juvenile justice involved youth is high, with 31% of girls and 15% of boys (Baglivio, et al., 2014; Dierkhising et al., 2013) in the juvenile justice system reporting a history of sexual abuse. Extensive research on adolescent and adult populations demonstrate that a history of sexual abuse is associated with a host of negative outcomes (Finkelhor, Cross, & Cantor, 2005; Mullers & Dowling, 2008), including increased engagement in risky sexual behaviors (Townsend, 2013; Ruffolo, Sarri, & Goodkind, 2004; Saar, Epstein, Rosenthal, & Vafa, 2015; Smith, Leve, & Chamberlain, 2006), a greater vulnerability to re-victimization (Townsend, 2013), and increased rates of delinquency and criminal behavior (Widom & Maxfield, 2001; Baglivio et al., 2014; Townsend, 2013; Asscher, Van der Put, & Stams, 2015).
Importantly, sexual abuse is related to problematic substance use (Townsend, 2013). Adolescents with a history of sexual abuse are four times more likely to have a SUD and nearly three times more likely to report problematic substance use in adulthood in comparison to members of the general population (Townsend, 2013). In addition, victims of sexual abuse begin experimenting with drugs at a younger age (13.7 years old) compared to those adolescents who are not victims of sexual abuse (15.1 years old; Kingston & Raghavan, 2009; Townsend, 2013), and this earlier onset of substance use is associated with a higher likelihood of developing a SUD (Moss, Chen, & Yi, 2014). Furthermore, substance use among sexual abuse victims increases the likelihood of engaging in criminal activity (Widom & White, 1997) and further exacerbates already high recidivism rates among juvenile justice involved youth (Conrad et al., 2014).
One way in which sexual abuse may be related to substance use in juvenile justice involved youth is through the experience of PTSD symptoms. It is possible that PTSD symptoms strengthen the relationship between sexual abuse and substance use, as the experience of PTSD symptoms could lead to substance use via self-medication (e.g. Wolitzky-Taylor, 2012) in sexually abused juvenile justice involved youth. Thus, PTSD symptoms in sexually abused juvenile justice involved youth could serve as a risk indicator for subsequent substance use. Additionally, PTSD symptoms could have a mechanistic role between sexual abuse and substance use in juvenile justice involved youth, by which decreasing PTSD symptoms could also serve to mitigate substance use risk associated with sexual abuse. Regardless if PTSD symptoms serve as a risk factor or mechanism of the sexual abuse and substance use relationship in juvenile justice involved youth, PTSD symptoms are a modifiable factor that could be targeted through treatment, potentially decreasing the sexual abuse and substance use relationship and associated negative outcomes.
Importantly, there is a burgeoning area of research which specifically aims to reduce PTSD symptoms in juvenile justice involved youth. Treatments, such as Trauma Affect Regulation: Guide for Education and Therapy (TARGET; Ford et al., 2013) and Cognitive Processing Therapy (CPT; Matulis et al., 2014) show initial promise in reducing PTSD symptoms in juvenile justice involved youth, including those who have experienced sexual abuse. An unexplored benefit of such treatments, however, is if reductions in PTSD symptoms serve to mitigate substance use risk associated with sexual abuse in juvenile justice involved youth. Determining if PTSD symptoms serve to strengthen or mediate the sexual abuse and substance use relationship in juvenile justice involved youth is an important step in clarifying treatment models for sexual abuse victims in this high-risk population.
The goal of the current study was to test two alternative models to better understand the way in which PTSD symptoms might influence the relationship between sexual abuse and substance use in juvenile justice involved youth. Specifically, we examined the following research questions: 1) Is the relationship between sexual abuse and substance use stronger in the presence of PTSD symptoms (i.e., moderation) and 2) Is sexual abuse related to substance use through PTSD symptoms (i.e., mediation). Additionally, we examined each research question with gender as a moderator. Differing base-rates of study variables by gender, such as sexual abuse (Baglivio, et al., 2014; Dierkhising et al., 2013), and varying mechanisms thought to underlie post-traumatic stress responses by gender (Norr et al., 2016), for example, could result in varying relationships between sexual abuse, PTSD symptoms, and substance use by gender. We also controlled for history of physical abuse, as poly-victimization, particularly through multiple forms of abuse, is related to psychological disorders and problems (e.g. substance use, PTSD symptoms; Ford, et al., 2010).
This study is the first step in a program of research that seeks to examine PTSD as a modifiable risk factor to reduce the effects of sexual abuse on substance use in this high-risk population. We chose to examine PTSD as a moderator and mediator in the current sample, as opposed to alternative causal models, given data that 1) sexual abuse typically temporally precedes PTSD development (although PTSD does increase the risk for re-victimization) and 2) substance use is often a symptom or result of PTSD.
2. Methods
2.1 Participants
Data were taken from existing charts of 247 juvenile justice involved youth in a Midwestern city who were court ordered to complete a psychological assessment between 2009 and 2016. Youth completed integrated assessments and a subset of that data is included in the current report. Data from the assessments were de-identified, and analysis of this archival data was approved by the Institutional Review Board.
2.2 Materials
Demographics
Youth reported their age, gender (girl or boy), and race.
PTSD
First, PTSD symptoms were assessed through the Youth Self-Report (YSR; Achenbach & Rescorla, 2001). The YSR is self-report assessment in which youth rate themselves on various behavioral and emotional problems. Response options range from 0 (not true) to 2 (very often or often true) and scores are converted to t-scores. For the PTSD scale, t-scores < 65 are considered to fall in the “normal” range, and t-scores over 65 correspond with increases in symptom severity. The YSR has shown good reliability (e.g. Ebesutani, Berstein, Martinez, & Chorpita, 2011). Further, the YSR has been validated for use in samples of juvenile justice involved youth (Vreugdenhil, et al., 2006). PTSD symptoms were used as a variable in analyses for the present study.
Second, PTSD diagnosis (distinct from the YSR PTSD scale score) was made by a licensed clinical psychologist conducting or supervising each youth’s assessment. Diagnoses were based on a structured clinical interview and YSR correspondence with DSM-IV-TR (American Psychiatric Association, 2000) or DSM-5 (American Psychiatric Association, 2013). Due to differences in diagnostic criteria between DSM versions and limited variability in dichotomous diagnoses, our analyses focused on the YSR PTSD score. PTSD diagnosis was used as a descriptive measure for the present study and not examined in study analyses.
Substance Use
First, substance use (illicit drug use and alcohol use) was assessed through the Adolescent Substance Use Subtle Screening Inventory (SASSI-A2; Miller & Lazowski, 2001). The SASSI-A2 is a self-report questionnaire for which youth self-report various substance use related behaviors. The present study examined substance use using the Face Valid Other Drugs (FVOD; e.g. “Taken drugs to improve your thinking and feeling”, “Taken drugs so you could enjoy sex more”; Miller, Renn, & Lazowski, 2001) scale and the Face Valid Alcohol (FVA; e.g. “Tried to kill yourself while drunk”, “Drank alcohol during the day”; Miller et al., 2001) scale of the SASSI-A2, with each scale assessing substance use related problems on a scale from 0 (never) to 3 (repeatedly). Results are provided as t-scores based on norms derived from an adolescent sample (mean age = 15, SD = 1.9) across addiction treatment centers, inpatient psychiatric hospitals, outpatient behavioral health facilities, and juvenile corrections programs. The SASSI-A2 FVA and FVOD scales have demonstrated acceptable to excellent reliability (alpha=0.61 and 0.95, respectively; Perera-Diltz & Perry, 2011) and test-retest reliability (r’s 0.71- and 0.92, respectively; Miller & Lazowski, 2001; Stein et al., 2005).
Second, a SUD diagnosis (distinct from the SASSI-A2 scales) was made by a licensed clinical psychologist conducting or supervising each youth’s assessment. Diagnoses were based on a structured clinical interview and SASSI-A2 correspondence with DSM-IV-TR (American Psychiatric Association, 2000) or DSM-5 (American Psychiatric Association, 2013). Due to differences in diagnostic criteria between DSM versions and limited variability in dichotomous diagnoses, our analyses focused on the SASSI-A2 scores. A SUD diagnosis was used as a descriptive measure for the present study and not examined in study analyses.
Sexual Abuse
Youth self-reported their history of sexual abuse through a structured clinical interview. Sexual abuse was coded as either reporting or not reporting sexual abuse. Additionally, the relationship of alleged perpetrator to the victim of sexual abuse was recorded (e.g. parent, paramour, relative).
Physical Abuse
Youth self-reported their history of physical abuse through a structured clinical interview. Physical abuse was coded as either reporting or not reporting physical abuse and used as a co-variate in analyses.
2.3 Procedure
Youth in the present sample were involved with the juvenile court (e.g. through arrest, probation violation) and referred to complete a court-ordered psychological assessment. Following the referral, a licensed clinical psychologist or supervised doctoral student reported to the Juvenile Detention Center or the youth’s current placement (e.g. group home, family home) to complete the assessment. Clinicians conducted a structured clinical interview and administered assessment measures, including the YSR, SASSI-A2, and other measures unrelated to the present study and not reported elsewhere. Clinicians used assessment information to compile an integrated report for each youth, which was submitted to the Marion County Juvenile Court upon completion. Trained research assistants entered YSR and SASSI-A2 data taken directly from the assessment reports for each youth. Additionally, research assistants coded whether or not the youth reported ever experiencing sexual abuse (any form of illegal sex act conducted against the youth) or physical abuse (any form of illegal physical act conducted against the youth, not including physical altercations between peers) based on the background information provided in the assessment report. Twenty percent of the data were recoded for inter-rater reliability. There were no discrepancies between coders on study variables.
Analysis Plan
First, we examined sample characteristics stratified across sexual abuse and gender. Second, we conducted moderated regression analyses using Andrew Hayes’ process macro (Hayes, 2013), controlling for age, race, and history of physical abuse (0-no abuse, 1-abuse), with sexual abuse (0-no abuse, 1-abuse) entered as the independent variable, PTSD symptoms (YSR PTSD scale) entered as the moderator, and gender (0-boys, 1-girls) entered as a second moderator (3-way interaction). Two analyses were conducted with drug use and alcohol use as dependent variables in separate models. Third, we conducted moderated mediation analyses using Andrew Hayes’ process macro (Hayes, 2013), controlling for age, race, and history of physical abuse, with sexual abuse entered as the independent variable, PTSD symptoms entered as the mediator, and gender entered as a moderator of the relationship between the independent and dependent variable. Two analyses were conducted with drug use and alcohol use as dependent variables in separate models.
3. Results
3.1 Descriptive Statistics
Of the 247 youth completing court-ordered psychological assessments, 197 provided data for PTSD scales, drug use, and alcohol use, making the final sample N = 197 (mean age = 15.45, SD = 1.31, range 13–18; 61.6% Black, 21.6% White, 3.2% Hispanic, 4.1% multiracial; 9.5% not specified; 78.4% male). Those youth that were not administered measures of PTSD, drug use, or alcohol use did not differ significantly in age or gender from youth that completed these measures. Those completing the drug and alcohol use scales were more likely to have a cannabis use disorder diagnosis, compared to those not completing (χ2 = 7.29, p = .007). The majority of the sample was non-white (68.9%) and male (79.5%). The majority of assessments were conducted at the juvenile detention center (82.1%) with youths having an average of 6 (SD = 3.80) criminal referrals to the court. Of the 197 youth, 17.3% were diagnosed with PTSD, and 44.7% were diagnosed with a cannabis use disorder, with a small proportion meeting criteria for alcohol use disorder (3%) and stimulant use disorder (1.5%).
Average drug use score was 56.32 (SD = 12.67; range 6 – 96), average alcohol use score was 45.75 (SD = 7.10; range 39 – 95), and average PTSD score was 60.49 (SD = 9.99; range 50 – 95). Alcohol use, drug use, & PTSD scales were all significantly correlated (r’s 0.31 to 0.52, p’s < .05; see Table 2).
Table 2.
Correlation between study variables.
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|
| 1. Age | −.06 | −.06 | .09 | .06 | .0 | .009 | −.02 | −.06 |
| 2. PTSD score | – | .18* | .31** | .10 | .41** | .06 | −.06 | .006 |
| 3. PTSD diagnosis | – | – | −.03 | −.08 | .02 | −.02 | −.02 | .09 |
| 4. FVA score | – | – | .53** | .52** | −.007 | −.04 | .03 | |
| 5. Alcohol Use Disorder diagnosis | – | – | – | – | .27** | −.002 | −.02 | −.001 |
| 6. FVOD score | – | – | – | – | – | .29** | −.04 | .06 |
| 7. Cannabis or other illicit drug Use Disorder diagnosis | – | – | – | – | – | – | −.07 | −.18* |
| 8. Sexual Abuse | – | – | – | – | – | – | – | −.03 |
| 9. Physical Abuse |
Note.
p < .05;
p < .001
A total of 13.2% of the sample reported any history of sexual abuse (7.8% of boys and 33.3% of girls in the sample) and 16% of the sample reported any history of physical abuse. A total of 2.9% of youth reported a history of both physical and sexual abuse. Girls were more likely than boys to report a history of sexual abuse (χ2 = 17.73, p < .001) and physical abuse (χ2 = 5.97, p = .02), and boys and girls were similarly likely to report a history of both physical and sexual abuse (χ2 = 2.57, p = .11; see Table 1). Youth that reported a history of sexual abuse were more likely to be diagnosed with PTSD, compared to those not reporting a history of sexual abuse (χ2 = 9.43, p < .002). Youth reporting only physical abuse (and not sexual abuse), compared to youth reporting sexual abuse (and not physical abuse) did not differ significantly in rate of PTSD diagnosis (χ2 = 1.99, p = .16), but youth reporting sexual abuse (and not physical abuse), scored higher on the PTSD scale (t(41)= −1.89), falling short of significance (p = .07).
Table 1.
Sample characteristics by sexual abuse and gender
| Boys (N=153) | Girls (N=42) | Test statistic | p | Sexual Abuse | No Sexual Abuse | Test statistic | p | |
|---|---|---|---|---|---|---|---|---|
| PTSD scale | 60.50 (10.30) | 60.45 (8.88) | 0.03 | .98 | 65.27 (12.69) | 59.77 (9.35) | −2.66 | .009 |
| FVA (alcohol use) | 45.06 (5.90) | 48.29 (10.10) | −2.65 | .009 | 47.77 (7.83) | 45.44 (6.96) | −1.57 | .12 |
| FVOD (drug use) | 56.60 (12.89) | 55.31 (11.91) | 0.59 | .56 | 56.00 (11.56) | 56.37 (12.86) | 0.14 | .89 |
| PTSD diagnosis | 13.5% | 31% | 7.01 | .008 | 38.46% | 14.03% | 9.43 | .002 |
| Sexual Abuse Only | 5.84% | 26.32% | 17.73 | <.001 | ||||
| Physical Abuse Only | 10.95% | 21.05% | 5.97 | .02 | ||||
| Sexual and Physical Abuse | 2.19% | 5.26% | 2.57 | .11 | ||||
| Cannabis Use Disorder | 46.45% | 38.09% | 0.93 | .33 | 38% | 45.6% | 0.47 | .49 |
| Stimulant Use Disorder | 1.3% | 2.4% | 0.26 | .61 | 0 | 3.5% | 0.46 | .50 |
| Alcohol Use Disorder | 3.2% | 2.4% | 0.08 | .78 | 0 | 3.5% | 0.94 | .33 |
| Sexual Abuse Perpetrator | Boys (N=14) | Girls (N=17) | ||||||
| Parent or paramour | 21.4% | 27.8% | 0.17 | .68 | ||||
| Adult relative | 14.3% | 5.6% | 0.71 | .40 | ||||
| Known adult non-relative | 28.6% | 22.2% | .17 | .68 | ||||
| Adult stranger | 7.1% | 5.6% | 0.03 | .85 | ||||
| Child relative | 28.6% | 5.6% | 3.16 | .08 | ||||
| Known child non-relative | 14.3% | 22.2% | 0.33 | .57 | ||||
Note. Ranges for scale scores were: PTSD YSR scale score, 0-95; FVA, 0-95; FVOD, 6-96. Boys reports of sexual abuse n = 14, girls reports of sexual abuse n = 17.
3.1.1 Moderation Analyses: Is the relationship between sexual abuse and substance use stronger in the presence of PTSD symptoms and variable by gender?
Drug Use
First, sexual abuse was not significantly related to drug use (β = 10.69, p = .60). Second, PTSD symptoms were significantly related to drug use (β = 0.66, p < .001). Third, PTSD symptoms did not significantly moderate the relationship between sexual abuse and drug use (β = −0.27, p = .35). Fourth, gender did not significantly moderate the overall model for drug use (β = 0.64, p = .24).
Alcohol Use
First, sexual abuse was not significantly related to alcohol use (β = 16.08, p = .18). Second, PTSD symptoms were significantly related to alcohol use (β = 0.23, p < .001). Third, PTSD symptoms did not significantly moderate the relationship between sexual abuse and alcohol use (β = −0.22, p = .17). Fourth, gender did not significantly moderate the overall model for alcohol use (β = 0.40, p = .20).
3.1.2 Moderation Mediation Analyses: Is sexual abuse related to substance use through PTSD symptoms and does this vary by gender?
Drug use
First, sexual abuse was significantly related to PTSD symptoms (β = 5.86, p = .009). Second, PTSD symptoms were significantly related to drug use (β = 0.59, p < .001). Third, sexual abuse was negatively related to drug use (β = −7.52, p = .05). Fourth, the relationship between sexual abuse and drug use was not moderated by gender (β = 9.02, p = .11). Fifth, PTSD significantly mediated the relationship between sexual abuse and drug use (β = 3.44, 95% CI 0.26 to 7.41; Test of indirect effect z=2.41, p = .02).
Alcohol Use
First, sexual abuse was significantly related to PTSD symptoms (β = 5.86, p = .009). Second, PTSD symptoms were significantly related to alcohol use (β = 0.24, p < .001). Third, sexual abuse was not significantly related to alcohol use (β = −0.57, p = .80). Fourth, the relationship between sexual abuse and alcohol use was not moderated by gender (β = 0.68, p = .80). Fifth, PTSD significantly mediated the relationship between sexual abuse and alcohol use (β = 1.42, 95% CI 0.20 to 3.46; Test of indirect effect z = 2.23, p = .03).
4. Discussion
Juvenile justice involved youth face a disproportionate amount of negative outcomes compared to their same age peers (e.g., Hershberger et al., 2016; Fazel, Doll, & Langstrom, 2008) and exhibit high rates of sexual abuse, PTSD, and substance use. Despite their high-risk nature, it is unclear how best to reduce negative outcomes associated with sexual abuse in juvenile justice involved youth. There are viable treatments targeting trauma, including sexual abuse, in this population (e.g. Ford et al., 2013, Matulis et al., 2014), which reduce PTSD symptoms; however, this study is unique in that it suggests targeting PTSD symptoms as a means of reducing sexual abuse related substance use risk in juvenile justice involved youth. These findings provide support that not only may sexual abuse serve as a risk indicator for PTSD and substance use in juvenile justice involved youth, but that PTSD may be a prime modifiable risk factor to reduce the effects of sexual abuse on subsequent substance use in this high-risk population. Once a child experiences sexual abuse, it is no longer a preventable or modifiable risk factor and intervening on substance use alone underestimates the role PTSD symptomatology plays in the onset and maintenance of substance use behaviors. PTSD symptoms appear to mediate, rather than moderate, the relationship between sexual abuse and substance use in juvenile justice involved youth, which suggests that reducing PTSD symptoms could protect against and reduce substance use in this population. This is important, given the negative outcomes associated with substance use in this high-risk group.
One likely explanation for the relationship between sexual abuse and substance use through PTSD observed in the present study is the self-medication hypothesis (Khantzian, 1987). The self-medication hypothesis (Khantzian, 1987) indicates that certain drugs are chosen deliberately by individuals who wish to suppress or avoid their negative experiences and emotions. Juvenile justice involved youth often display high rates of avoidant PTSD symptoms (Kerig & Becker, 2010), and substance use is often cited as one coping strategy used by sexually victimized youth (Kilpatrick et al., 2003). Thus, juvenile justice involved youth that are victims of sexual abuse may use substances as a means to cope with or alleviate emotional distress. Interventions designed to provide more adaptive ways to cope with or alleviate emotional distress have the potential to reduce the reliance on substance use in this population. Although previous research indicates mixed findings for the relationship between PTSD and substance use in juvenile justice involved youth (Abram et al., 2004; Kingston & Raghavan, 2009; Dierkhising et al., 2013; Danielson et al., 2010; Rosenberg et al., 2014), present findings support PTSD as a proximal factor to substance use among youth that are victims of sexual abuse.
Given that one way by which sexual abuse is related to greater substance use is through the presence of greater PTSD symptomology, it appears trauma-informed treatment could be critical to reducing substance use in juvenile justice involved youth with sexual abuse. One well-studied model of trauma-focused treatment for substance use is Seeking Safety (Najavitz, 2002), and although this evidence-based treatment has not been well-studied in juvenile justice involved youth, it certainly provides one framework for addressing issues highlighted in the present study. Such therapies are easily implemented (Najavits, Gallop, & Weiss, 2006) and provide psychoeducation on the complex interplay between trauma and substance use. Risk Reduction through Family Therapy (Danielson et al., 2010; Danielson et al., 2012) also demonstrates efficacy in reducing substance use and PTSD symptoms in adolescent victims of sexual assault, and such treatments could be expanded to examine efficacy in juvenile justice populations. Additionally, there are trauma-related treatments for juvenile justice involved youth, such as Trauma Affect Regulation: Guide for Education and Therapy (TARGET; Ford et al., 2013) and Cognitive Processing Therapy (CPT; Matulis et al., 2014) which show initial evidence of reducing PTSD symptomology in this population, and thus could serve to mitigate sexual abuse related substance use risk in this population. It is imperative that trauma treatment research in juvenile justice involved youth tracks not only changes in PTSD symptoms, but changes in substance use and related problems, to best examine the mechanistic role of trauma-informed treatment in reducing sexual abuse related substance use risk.
It is important to note that the present findings are cross-sectional, thus there are other plausible reasons for the observed relationships. For example, genetic factors may put individuals at high risk for both PTSD and substance use (Kendler et al., 2003). Although cross-sectional data are limited in making causal inferences, we view the current study as the first step in a program of research examining these temporal relationships in prospective designs and designing and testing interventions to reduce substance use and risk in this high-risk, though relatively understudied, population. It is our aim that this initial study will stimulate additional and much-needed research and intervention design and testing in this group.
Additionally interesting, gender did not significantly moderate the models examined in the present study. This may indicate that there is no differential risk by gender in juvenile justice involved youth for the impact PTSD symptoms have on sexual abuse related substance use or that the relationship between sexual abuse and substance use does not vary by gender in this population. First, although research suggests varying mechanisms, such as anxiety sensitivity, underlie post-traumatic responses by gender (Norr et al., 2016), these gender differences may not extend to reflect variable outcomes by gender, specifically sexual abuse related substance use.
Additionally, research indicates that juvenile justice involved girls experience sexual abuse at rates more than double of boys (Baglivio, et al., 2014; Dierkhising et al., 2013), but it is possible that negative outcomes, particularly substance use, associated with sexual abuse, cut across gender. It is also possible that we were underpowered to detect an effect (N=42 girls) and there are gender differences in the impact that PTSD symptoms have on sexual abuse related substance use and the direct relationship between sexual abuse and substance use. Future research should aim to clarify the role of gender in negative outcomes associated with sexual abuse in order to best tailor treatment.
Although the present study is important in that it suggests viability of a novel intervention approach to reduce substance use in high-risk, juvenile justice involved youth, there are some limitations to discuss. First, as common in many studies, data was self-report in nature, and thus subject to self-report bias. Additionally, the sample was limited in the number of youth reporting sexual abuse, thus null findings might reflect failure to find a true effect. Present data is cross-sectional and no causal pathways can be determined from our findings, although they can suggest viability of examining these relationships in temporal models in the future. For the present study, we were given access to juvenile justice involved youth’s assessment reports, which did not include individual item scores on study measures, thus we could not compute reliability for the measures; however, the YSR and SASSI-A2 demonstrate good psychometric properties across studies (e,g. Miller & Lazowski, 2001; Stein et al., 2005 Vreugdenhil, et al., 2006), increasing our confidence in these measures in the present study. The present sample had a limited number of females and non-whites, thus results may not generalize beyond the demographic makeup of the present sample, although this makeup does reflect typical juvenile justice populations (Child Trends Data Bank, 2015; Teplin et al., 2002). Last, although we controlled for history of physical abuse, there are other traumas juvenile justice involved youth often experience, such as emotional abuse, which may serve to amplify their trauma related risk for substance use. The present findings cannot determine if sexual abuse related risk for substance use through PTSD symptomology can be better accounted for by poly-victimization beyond sexual abuse and physical abuse; however, as we detected the present findings after controlling for the additional presence of physical abuse, this increases our confidence that particular attention should be paid to sexual abuse related substance use. In light of these limitations, we hope our findings will move the research field of juvenile justice involved youth forward, particularly in measuring and examining PTSD symptom change as a means of mitigating sexual abuse related substance use risk.
Conclusion
Juvenile justice involved youth face disproportionate rates of sexual abuse, which increases the risk for Post-Traumatic Stress Disorder (PTSD) and substance use disorders, both of which are associated with negative long-term outcomes. However, how best to reduce the effects of sexual abuse in this group is not yet clear. Overall, findings suggest viability that targeting PTSD symptoms in juvenile justice involved youth has potential as a prime modifiable treatment target to reduce the effects of sexual abuse on substance use in this high-risk population. We view the current study as providing key initial evidence, which should be replicated in temporal work, including the design and testing of PTSD interventions to reduce risk in this high-risk population.
Figure 1.
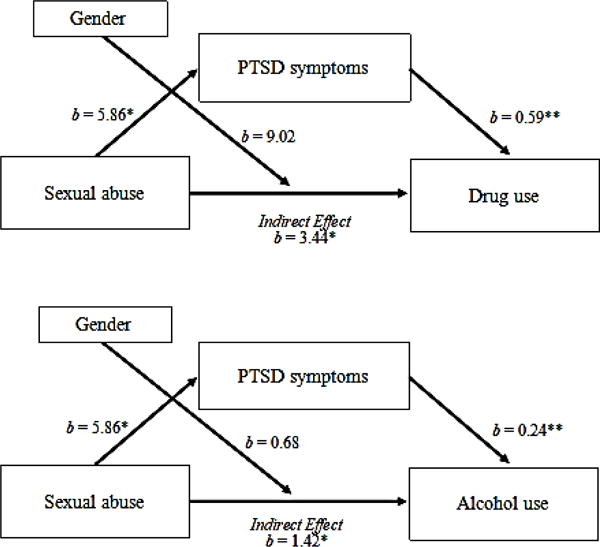
Results of mediation models run using Andrew Hayes process macro (Hayes, 2013), controlling for age, gender, and race. Top: Results indicated that the indirect effect of sexual abuse on drug use through PTSD scores was significant (β = 3.44, 95% CI 0.26 to 7.41; Test of indirect effect z=2.41, p = .02). Bottom: Results indicated that the indirect effect of sexual abuse on alcohol use through PTSD scores was significant (β = 1.42, 95% CI 0.20 to 3.46; Test of indirect effect z = 2.23, p = .03).
Acknowledgments
The authors would like to acknowledge Katie Schwartz for her coordination of the forensic psychology clinic at the Indiana University School of Medicine.
The preparation of this manuscript was supported in part by an F31 grant to Alexandra Hershberger (F31 AA024682) and fellowship to Jasmyn N. Sanders (R25 GM109432) both under the mentorship of Melissa A Cyders.
References
- Abram KM, Teplin LA, Charles DR, Longworth SL, McClelland GM, Dulcan MK. Posttraumatic stress disorder and trauma in youth in juvenile detention. Archives of General Psychiatry. 2004;61(4):403–410. doi: 10.1001/archpsyc.61.4.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achenbach TM, Rescorla L. ASEBA school-age forms & profiles 2001 [Google Scholar]
- Asscher JJ, Van der Put CE, Stams GJJM. Gender differences in the impact of abuse and neglect victimization on adolescent offending behavior. Journal of Family Violence. 2015;30(2):215–225. doi: 10.1007/s10896-014-9668-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baglivio MT, Epps N, Swartz K, Huq MS, Sheer A, Hardt NS. The prevalence of adverse childhood experiences (ACE) in the lives of juvenile offenders. Office of Juvenile Justice and Delinquency Prevention Journal of Juvenile Justice. 2014;3(2):1–14. http://www.journalofjuvjustice.org/JOJJ0302/article01.htm. [Google Scholar]
- Child Trends Data Bank. Indicators on children and youth. Juvenile Detention. 2015:1–17. Retrieved from http://www.childtrends.org/wp-content/uploads/2012/05/88_Juvenile_Detention.pdf.
- Conrad SM, Tolou-Shams M, Rizzo C, Placella N, Brown LK. Gender differences in recidivism rates for juvenile justice youth: The impact of sexual abuse. Law and Human Behavior. 2014;38(4):305–314. doi: 10.1037/lhb0000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson C, Macdonald A, Amstadter AB, Hanson R, de Arellano MA, Saunders BE, Kilpatrick DG. Risky behaviors and depression in conjunction with—or in the absence of—lifetime history of PTSD among sexually abused adolescents. Child maltreatment. 2010;15(1):101–107. doi: 10.1177/1077559509350075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson C, McCart MR, de Arellano MA, Macdonald A, Doherty LS, Resnick HS. Risk reduction for substance use and trauma-related psychopathology in adolescent sexual assault victims: Findings from an open trial. Child maltreatment. 2012;15(3):261–268. doi: 10.1177/1077559510367939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dierkhising CB, Ko SJ, Woods-Jaeger B, Briggs EC, Lee R, Pynoos RS. Trauma histories among justice-involved youth: Findings from the National Child Traumatic Stress Network. European Journal of Psychotraumatology. 2013;4:1–12. doi: 10.3402/ejpt.v4i0.20274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebesutani C, Bernstein A, Martinez JI, Chorpita BF, Weisz JR. The Youth Self Report: Applicability and validity across younger and older youths. Journal of Clinical Child & Adolescent Psychology. 2011;40(2):338–346. doi: 10.1080/15374416.2011.546041. [DOI] [PubMed] [Google Scholar]
- Fazel S, Doll H, Långström N. Mental disorders among adolescents in juvenile detention and correctional facilities: a systematic review and metaregression analysis of 25 surveys. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(9):1010–1019. doi: 10.1097/CHI.ObO13e31817eecf3. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Cross TP, Cantor EN. How the justice system responds to juvenile victims: A comprehensive model of case flow. Trauma, Violence, & Abuse. 2005;6(2):83–102. doi: 10.1177/1524838005275090. [DOI] [PubMed] [Google Scholar]
- Ford JD, Elhai JD, Connor DF, Frueh BC. Poly-victimization and risk of posttraumatic, depressive, and substance use disorders and involvement in delinquency in a national sample of adolescents. Journal of Adolescent Health. 2010;46(6):545–552. doi: 10.1016/j.jadohealth.2009.11.212. [DOI] [PubMed] [Google Scholar]
- Ford JD, Chang R, Levine J, Zhang W. Randomized clinical trial comparing affect regulation and supportive group therapies for victimization-related PTSD with incarcerated women. Behavior Therapy. 2013;44(2):262–276. doi: 10.1016/j.beth.2012.10.003. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of general psychiatry. 2003;60(9):929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kerig PK, Becker SP. From internalizing to externalizing: Theoretical models of the processes linking PTSD to juvenile delinquency. In: Egan SJ, editor. Posttraumatic stress disorder (PTSD): Causes, symptoms and treatment. Hauppauge, NY: Nova Science Publishers; 2010. pp. 33–78. [Google Scholar]
- Khantzian EJ. The cocaine crisis. Springer US; 1987. The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence; pp. 65–74. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting & Clinical Psychology. 2003;71(4):602–700. doi: 10.1037/0022-006X.71.4.692. [DOI] [PubMed] [Google Scholar]
- Kingston S, Raghavan C. The relationship of sexual abuse, early initiation of substance use, and adolescent trauma to PTSD. Journal of Traumatic Stress. 2009;22(1):65–68. doi: 10.1002/jts.20381. [DOI] [PubMed] [Google Scholar]
- Matulis S, Resick PA, Rosner R, Steil R. Developmentally adapted cognitive processing therapy for adolescents suffering from posttraumatic stress disorder after childhood sexual or physical abuse: A pilot study. Clinical Child And Family Psychology Review. 2014;17(2):173–190. doi: 10.1007/s10567-013-0156-9. [DOI] [PubMed] [Google Scholar]
- Moss HB, Chen CM, Yi HY. Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug and alcohol dependence. 2014;136:51–62. doi: 10.1016/j.drugalcdep.2013.12.011. [DOI] [PubMed] [Google Scholar]
- Miller FG, Lazowski LE. The Adolescent Substance Abuse Subtle Screening Inventory-A2 (SASSI-A2) manual. Springville, IN: SASSI Institute; 2001. [Google Scholar]
- Miller FG, Renn WR, Lazowski LE. Adolescent SASSI-A2 user’s guide. Bloomington, IN: Baugh Enterprises; 2001. [Google Scholar]
- Mullers ES, Dowling M. Mental health consequences of child sexual abuse. British Journal of Nursing. 2008;17(22):1428–1433. doi: 10.12968/bjon.2008.17.22.31871. [DOI] [PubMed] [Google Scholar]
- Najavits LM. Seeking safety: A treatment manual for PTSD and substance abuse. Guilford Press; 2002. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Gallop RJ, Weiss RD. Seeking safety therapy for adolescent girls with PTSD and substance use disorder: A randomized controlled trial. The Journal of Behavioral Health Services & Research. 2006;33(4):453–463. doi: 10.1007/s11414-006-9034-2. [DOI] [PubMed] [Google Scholar]
- Norr AM, Albanese BJ, Boffa JW, Short NA, Schmidt NB. The relationship between gender and PTSD symptoms: Anxiety sensitivity as a mechanism. Personality And Individual Differences. 2016:90210–213. doi: 10.1016/j.paid.2015.11.014. [DOI] [Google Scholar]
- Perera-Diltz DM, Perry JC. Screening for Adolescent Substance-Related Disorders Using the SASSI-A2: Implications for Nonreporting Youth. Journal of Addictions & Offender Counseling. 2011;31(2):66–79. [Google Scholar]
- Rosenberg HJ, Vance JE, Rosenberg SD, Wolford GL, Ashley SW, Howard ML. Trauma exposure, psychiatric disorders, and resiliency in juvenile-justice-involved youth. Psychological Trauma: Theory, Research, Practice, and Policy. 2014;6(4):430. [Google Scholar]
- Ruffolo MC, Sarri R, Goodkind S. Study of delinquent, diverted, and high-risk adolescent girls: Implications for mental health intervention. Social Work Research. 2004;28(4):237–245. doi: 10.1093/swr/28.4.237. [DOI] [Google Scholar]
- Saar MS, Epstein R, Rosenthal L, Vafa Y. The sexual abuse to prison pipeline: The girls’ story. Georgetown Law Center on Poverty & Inequality. 2015:1–43. Retrieved from http://rights4girls.org/wp-content/uploads/r4g/2015/02/2015_COP_sexual-abuse_layout_web-1.pdf.
- Smith DK, Leve LD, Chamberlain P. Adolescent Girls’ Offending and Health-Risking Sexual Behavior: The Predictive Role of Trauma. Child Maltreatment. 2006;11(4):346–353. doi: 10.1177/1077559506291950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LAR, Lebeau-Craven R, Martin R, Colby SM, Barnett NP, Golembeske C, Penn JV. Use of the Adolescent SASSI in a Juvenile Correctional Setting. Assessment. 2005;12(4):384–394. doi: 10.1177/1073191105279433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Criminal and Juvenile Justice: Overview. 2016 https://www.samhsa.gov/criminal-juvenile-justice.
- Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA. Psychiatric disorders in youth in juvenile detention. Archives of general psychiatry. 2002;59(12):1133–1143. doi: 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, Washburn JJ. Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatric Services. 2005;56(7):823–828. doi: 10.1176/appi.ps.56.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend C. Prevalence and consequences of child sexual abuse compared with other childhood experiences. Darkness to Light. 2013:1–19. Retrieved from www.d2l.org.
- Vreugdenhil C, van den Brink W, Ferdinand R, Wouters L, Doreleijers T. The ability of YSR scales to predict DSM/DISC–C psychiatric disorders among incarcerated male adolescents. European child & adolescent psychiatry. 2006;15(2):88–96. doi: 10.1007/s00787-006-0497-8. [DOI] [PubMed] [Google Scholar]
- Widom CS, Maxfield MG. An update on the “Cycle of Violence”. National Institute of Justice Research in Brief. 2001:1–8. Retrieved from https://www.ncjrs.gov/pdffiles1/nij/184894.pdf.
- Widom CS, White HR. Problem behaviors in abused and neglected children grown up: Prevalence and co-occurrence of substance abuse, crime, and violence. Criminal Behavior & Mental Health. 1997;7:287–310. doi: 10.1002/cbm.191. [DOI] [Google Scholar]
- Wolitzky-Taylor K, Bobova L, Zinbarg RE, Mineka S, Craske MG. Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addictive Behaviors. 2012;37(8):982–985. doi: 10.1016/j.addbeh.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]


