Abstract
Objective:
To report the case of a fisherman who developed chronic mercury poisoning due to excessive consumption of tuna while working on a pelagic fishing vessel.
Case report:
A 48-year-old male deep-sea fisherman developed paresthesia and pain in both legs while working at sea. He continued working for over 4 months on a pelagic fishing vessel but was eventually unable to function normally as his condition deteriorated. Upon arrival on land, he received specialist treatment, including imaging studies, for 2 months; however, the cause of the symptoms was not identified. An examination of his occupational history revealed that he had worked as a crew member on a pelagic fishing vessel catching tuna for the last 2 years and consumed tuna for two or more meals per day, every day. Two months after discontinuation of tuna consumption, he was tested for mercury. The result showed an elevated blood mercury level (BML) of 21.79 μg/l. Based on the half-life of mercury, the BML was evaluated as 38.70-53.20 μg/l when he was on board. Four months after discontinuing tuna consumption, his BML decreased to 14.18 μg/l, and the symptoms were almost ameliorated. The person responsible for preparing meals on a pelagic fishing ship should be aware that fish may contain high levels of heavy metals and should prepare meals for crew members according to the recommended levels. Crew members should also be aware that fish and shellfish may contain mercury, and hence, they should consume only an appropriate amount.
Keywords: Consumption, Heavy metal poisoning, Korea, Mercury poisoning, Tuna
Introduction
According to a 2012 report, 158 million tons of fish, including 7 million tons of tuna, are caught annually1). There are approximately 3,000 deep-sea commercial fishing vessels for tuna fishing; tuna is consumed worldwide as raw or cooked fish, or after being processed and canned2). Fish is an excellent source of protein and contains omega-3 fatty acids, vitamin D, and selenium, which are reported to help lower the prevalence and mortality of cerebrovascular and coronary heart diseases3-8). Tuna consumption also promotes the health of a baby if a pregnant or breastfeeding woman consumes a suitable amount of fish9,10). Furthermore, dietary fish intake may be a lifestyle factor that can serve as a resource for work engagement11).
However, overconsumption of fish with high levels of organic mercury, such as tuna, can cause methylmercury poisoning and a variety of abnormal central nervous system-related symptoms such as paresthesia, ataxia, hearing impairment, and progressive constriction of the visual fields12-15). In the present study, we report the case of a fisherman who developed chronic mercury poisoning following excessive consumption of tuna while working on a pelagic fishing vessel for 2 years.
Case History
A 48-year-old man experienced paresthesia and pain in both legs for 6 months before presenting to the hospital (October 2015). The patient complained that the symptoms were more severe on the right side, and they were felt under the right thigh and left knee. Symptoms worsened mainly during nighttime or when he was physically tired. Because the symptoms continued to deteriorate, the patient returned to land (February 2016). He had no significant past medical history. He quit smoking in 2000 with a 10-year smoking history of smoking a pack per day, and he drank 700 ml of beer once weekly. His height was 179 cm and weight 75 kg. After admission, the patient was treated in the departments of neurosurgery and rehabilitation as a musculoskeletal disease was suspected, such as herniation of the nucleus pulposus. However, lesions or findings that could be linked to the aforementioned symptoms were not identified on physical examination or magnetic resonance imaging. Nerve conduction velocity findings were normal except for a prolonged F-wave latency in the right peroneal and tibial nerves.
When investigating his occupational history, it was found that the patient had worked in the pelagic fishing industry for approximately 15 years and consumed an excessive amount of tuna while at sea. He had worked on pelagic fishing vessels since 2000. Typically, he worked for a year once on board and took a 3-6-month break after arriving on land. On his last job onboard a tuna fishing vessel, he embarked in February 2015 and disembarked in February 2016. His professional responsibilities were driving a 45-ton skiff and maintaining and repairing the engine. In 2015, after a new vessel chef was employed, he consistently consumed albacore or yellowfin tuna twice a day, almost every day (over 500 g daily), while on board. The level of mercury in albacore and yellowfin has been estimated to be 0.358 ppm and 0.354 ppm, respectively16). Under the assumption of approximately 0.35 ppm in the tuna that he consumed, his daily mercury consumption was estimated to be over 175 μg/day, which was just over the World Health Organization (WHO) tolerable intake of 2 μg/kg/day17).
The blood mercury level (BML) of the patient when he visited the hospital on March 29, 2016 was 21.79 μg/l; consequently, he was diagnosed with mercury poisoning. The serum half-life of organic mercury is approximately 45-70 days18). Accordingly, his BML was estimated to be higher when he was on board (BML: 38.70-53.20 μg/l), because about 2 months had passed since he had disembarked and discontinued tuna consumption. The blood levels of other heavy metals, e.g., cadmium (2.25 μg/l), manganese (4.88 μg/l), and lead (2.60 μg/dl), were normal. On April 5, 2016, the urine mercury level (UML) was 6.715 μg/l, and creatinine level was 111.3 mg/dl, with a modified UML of 6.03 μg/g crea. UML was measured to exclude the possibility of inorganic mercury exposure. Measurements of mercury in whole blood or hair are metrics used to reflect body burden of the short-chain alkyl mercury compounds (predominantly methylmercury). For reasons outlined previously, urinary levels are not useful in assessing exposure to short-chain alkyl mercury compounds19). Methylmercury is well absorbed from the gastrointestinal tract. About 95% of methylmercury ingested from fish is absorbed and distributed to all tissues in about 30 hours. About 10% of absorbed methylmercury is distributed to the brain, whereas 5% remains in blood20). Methylmercury readily accumulates in hair, and although the concentration of methylmercury in hair is proportional to that in blood, they are about 250-fold higher in hair. Thus, hair mercury level is often used as an indicator of exposure. Methylmercury undergoes extensive enterohepatic recycling, which can be interrupted to enhance fecal excretion. Methylmercury is slowly metabolized to inorganic mercury by microflora in the intestine (about 1% of the body burden per day), In contrast to inorganic mercury, 90% of methylmercury is eliminated from the body in the feces, and less than 10% is in the urine, with a half-life of 45-70 days20). Thus, substantial seafood consumption may result in high BML and low UML21).
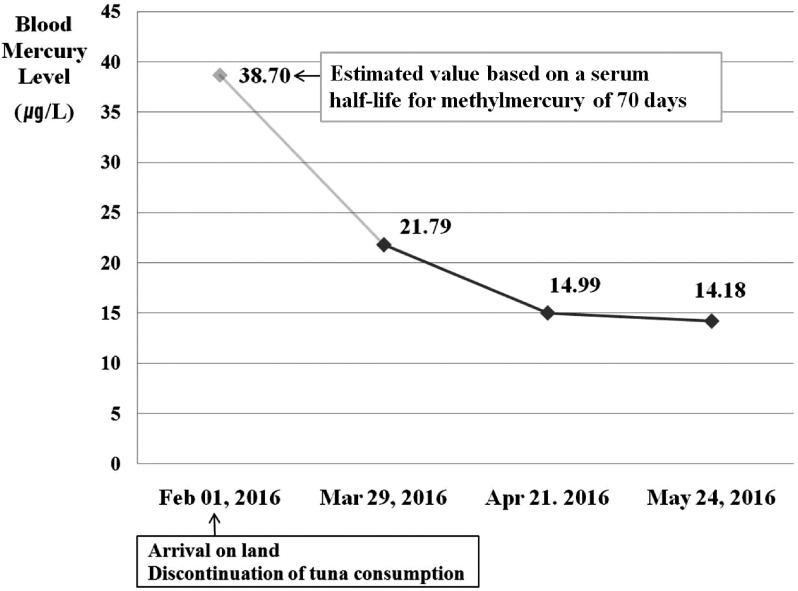
A normal BML is under 10 μg/l18). The main symptoms seen in a person with mercury toxicity are central nervous system symptoms18). Because the patient's symptoms improved, and no damages to the kidneys and nervous system were found, a chelation treatment was not commenced. Instead, he was forbidden to consume fish with a high mercury level, such as tuna, and given education concerning fish that contain large amounts of heavy metals. In addition, he was recommended to perform aerobic exercise on a regular basis and have a balanced diet focusing on vegetables. Subsequently, his BML reduced to 14.99 μg/l on April 21, 2016 and to 14.18 μg/l on May 24, 2016 (Fig. 1). His symptoms were largely ameliorated.
Fig. 1.
Changes in the blood mercury level of the deep-sea fisherman who consumed a large quantity of tuna.
BML and UML were measured in the following manner. BML: 400 μl of EDTA whole blood or heparinized whole blood was diluted with 3% acetic acid to 20 ml; 40 μl of 5% KMnO4 and 50 μl of 1-octanol were then added. We used 3% HCl and 0.2% NaBH4 as the carrier and reductant solutions, respectively. This diluted solution was analyzed using a mercury analyzer (FIMS 400, Perkin Elmer, USA). UML: 500 μl of urine was diluted with 3% acetic acid to 10 ml; 1 ml of 5% KMnO4 was then added, followed by 500 μl of 20% Na2OH・HCl 3 hours later. This diluted solution was kept overnight at room temperature. We used 3% HCl and 0.2% NaBH4 as the carrier and reductant solutions, respectively. The next day, this diluted solution was analyzed using a mercury analyzer (FIMS 400, Perkin Elmer, USA). The first author explained the purpose of this case study, and the patient agreed and signed the written informed consents.
Discussion
Since ancient times, humans have consumed fish as an essential source of energy. However, as industrialization rapidly progressed from the beginning of the 20th century and a great number of power stations and factories began to operate, a wide range of hazardous substances have polluted the entire earth. Mercury is one such hazardous substance, and the WHO currently considers mercury as a top-10 chemical element affecting public health22). Mercury is classified in terms of its form as either elemental mercury, inorganic mercury, or organic mercury. The general population is exposed mostly to methylmercury, a type of short-chain organic mercury, via the consumption of fish and shellfish, and the level of mercury in fish has been reported to be steadily increasing23). Methylmercury can pass through the blood-brain barrier and placenta, potentially affecting the brain and/or fetus. Therefore, additional care is required for children and pregnant women to minimize exposure24-26).
The present study reported the case of a 48-year-old deep-sea fisherman who presented to the hospital with paresthesia and pain in the lower limbs. He began experiencing the symptoms 6 months prior to presentation while working on a pelagic fishing vessel and consuming a large quantity of tuna, resulting in chronic mercury poisoning. The symptoms improved without the administration of chelation treatment and following education and discontinuation of the consumption of fish with high mercury levels. Mercury poisoning through fish consumption is uncommon in the general population, although a case study reported that two health-conscious men developed mercury poisoning by consuming tuna and shark products for several months27). Moreover, a 1-year survey of an internal medicine practice in San Francisco, California, showed that a substantial fraction of patients had diets high in fish consumption. Of these patients, a high proportion had BMLs exceeding the maximum level recommended by the United States Environmental Protection Agency and National Academy of Science28).
On a fishing boat at sea for a long time, it is possible that a large proportion of the food for the crew will be fish caught during that time. Accordingly, mercury intoxication in the crew should always be guarded against on fishing boats that catch fish containing a high level of mercury, such as tuna in this case. To prevent mercury poisoning, the person responsible for preparing meals for the crew of a ship at sea for long periods should receive training in order to develop a menu for the crew according to international standards regarding consumption of fish with high levels of heavy metals, especially mercury.
In the current case, we initially considered administering a chelation treatment using 2,3-dimercaptopropane-1-sulfonate. However, chelation treatment was not administered after excessive consumption of tuna was identified as the root cause because cessation of exposure had occurred weeks earlier, and his symptoms improved with follow-up. The decision to administer chelation treatment in such cases depends on the severity of symptoms and on the presence of evidence of neurologic or renal toxicity. Physicians should carefully determine whether to administer a chelation treatment by considering the causes of poisoning, patient conditions, anticipated disease course, and possible complications29).
Fishing crews at sea for long periods should undergo testing for heavy metal levels before embarking and after disembarking the boat. People working at restaurants serving tuna or other pelagic species should also be aware of the possibility of mercury poisoning due to overconsumption of tuna. Additionally, an examination of a patient's occupational history during clinical examination will help physicians promptly and accurately diagnose patients with heavy metal poisoning.
Conclusions
The person responsible for preparing meals on a pelagic fishing ship should be aware of fish containing high levels of heavy metals and prepare meals for crew members according to the recommended levels. Crew members should also be aware that fish and shellfish may contain mercury, and hence, they should consume only an appropriate amount.
Conflicts of interest: There are no financial or other issues that might lead to conflict of interests.
References
- 1). Food and Agriculture Organization of the United Nations. The State of World Fisheries and Aquaculture. [Online]. 2014 [cited 2017 Aug. 24]; Available from: URL: http://www.fao.org/3/a-i3720e.pdf
- 2). Western and Central Pacific Fisheries Commission. Tuna Fishery Yearbook. [Online]. 2014 [cited 2017 Aug. 24]; Available from: URL: https://www.wcpfc.int/system/files/YB_2014.pdf
- 3). Djoussé L, Akinkuolie AO, Wu JH, et al. Fish consumption, omega-3 fatty acids and risk of heart failure: a meta-analysis. Clinical Nutrition 2012; 31 (6): 846-853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4). Zheng J, Huang T, Yu Y, et al. Fish consumption and CHD mortality: an updated meta-analysis of seventeen cohort studies. Public Health Nutrition 2012; 15 (4): 725-737. [DOI] [PubMed] [Google Scholar]
- 5). Chowdhury R, Stevens S, Gorman D, et al. Association between fish consumption, long chain omega 3 fatty acids, and risk of cerebrovascular disease: systematic review and meta-analysis. BMJ 2012; 345: e6698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Buscemi S, Nicolucci A, Lucisano G, et al. Habitual fish intake and clinically silent carotid atherosclerosis. Nutrition Journal 2014; 13 (1): 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7). Virtanen JK, Mozaffarian D, Chiuve SE, et al. Fish consumption and risk of major chronic disease in men. The American Journal of Clinical Nutrition 2008; 88 (6): 1618-1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8). Kris-Etherton PM, Harris WS, Appel LJ. American Heart Association. Nutrition Committee. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation 2002; 106 (21): 2747-2757. [DOI] [PubMed] [Google Scholar]
- 9). Axelrad DA, Bellinger DC, Ryan LM, et al. Dose-response relationship of prenatal mercury exposure and IQ: an integrative analysis of epidemiologic data. Environmental Health Perspectives 2007; 115 (4): 609-615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10). Al-Saleh I, Nester M, Abduljabbar M, et al. Mercury (Hg) exposure and its effects on Saudi breastfed infant's neurodevelopment. International Journal of Hygiene and Environmental Health 2016; 219 (1): 129-141. [DOI] [PubMed] [Google Scholar]
- 11). Nishi D, Suzuki Y, Nishida J, et al. Personal lifestyle as a resource for work engagement. Journal of Occupational Health 2017; 59 (1): 17-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Agency for Toxic Substances and Disease Registry. Toxicological profile for mercury. [Online]. [cited 2017 Aug. 24]; Available from: URL: https://www.atsdr.cdc.gov/toxprofiles/tp46.pdf
- 13). Ye BJ, Kim BG, Jeon MJ, et al. Evaluation of mercury exposure level, clinical diagnosis and treatment for mercury intoxication. Annals of Occupational Environmental Medicine 2016; 28 (1): 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14). Nakamura M, Hachiya N, Murata KY, et al. Methylmercury exposure and neurological outcomes in Taiji residents accustomed to consuming whale meat. Environmental International 2014; 68: 25-32. [DOI] [PubMed] [Google Scholar]
- 15). Park GI, Byun YS, Jeon MJ, et al. The associations between blood mercury levels and shark meat intake among workers in Gyeongsangbuk-do. Annals of Occupational Environmental Medicine 2017; 29 (1): 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16). United States Food and Drug Administration. Mercury Levels in Commercial Fish and Shellfish (1990-2010). [Online]. [cited 2017 Aug. 24]; Available from: URL: http://www.fda.gov/Food/FoodborneIllnessContaminants/metals/ucm115644.htm
- 17). World Health Organization. Exposure to mercury. [Online]. [cited 2017 Aug. 24]; Available from: URL: http://www.who.int/phe/news/Mercury-flyer.pdf
- 18). Clarkson TW, Magos L, Myers GJ. The toxicology of mercury-current exposures and clinical manifestations. New England Journal of Medicine 2003; 349: 1731-1737. [DOI] [PubMed] [Google Scholar]
- 19). Franzblau A, Fromes MC. Mercury. In: Rosenstock L. Textbook of Clinical Occupational and Environmental Medicine. 2nd ed, Philadelphia: ELSEVIER SAUNDERS; 2005. p. 981. [Google Scholar]
- 20). Tokar EJ, Boyd WA, Freedman JH, et al. The effects of metals. In: Klaassen CD. Casarett and Doull's toxicology: The basic science of poisons. 8th ed, New York: McGraw-Hill; 2013. p. 998. [Google Scholar]
- 21). Lewis R, Kosnett MJ. Metals. In: LaDou J. Current occupational & Environmental medicine. 5th ed, New York: McGraw-Hill; 2014. p. 476-477. [Google Scholar]
- 22). World Health Organization. Mercury and health fact sheet. [Online]. [cited 2017 Aug. 24]; Available from: URL: http://www.who.int/mediacentre/factsheets/fs361/en/
- 23). Drevnick PE, Lamborg CH, Horgan MJ. Increase in mercury in Pacific yellowfin tuna. Environmental Toxicology and Chemistry 2015; 34 (4): 931-934. [DOI] [PubMed] [Google Scholar]
- 24). Kuhnert PM, Kuhnert BR, Erhard P. Comparison of mercury levels in maternal blood, fetal cord blood, and placental tissues. American Journal of Obstetrics and Gynecology 1981; 139 (2): 209-213. [DOI] [PubMed] [Google Scholar]
- 25). Yin Z, Jiang H, Syversen T, et al. The methylmercury-L-cysteine conjugate is a substrate for the L-type large neutral amino acid transporter. Journal of Neurochemistry 2008; 107 (4): 1083-1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26). Chang JY, Park JS, Shin S, et al. Mercury exposure in healthy Korean weaning-age infants: association with growth, feeding and fish intake. International Journal of Environmental Research and Public Health 2015; 12 (11): 14669-14689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27). Pereira LMP, Teelucksingh S. Fish faddism causing low-level mercury poisoning in the Caribbean: two case reports. Cases Journal 2009; 2 (1): 7009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28). Hightower JM, Moore D. Mercury levels in high-end consumers of fish. Environmental Health Perspectives 2003; 111 (4): 604-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29). Cao Y, Skaug MA, Andersen O, et al. Chelation therapy in intoxications with mercury, lead and copper. Journal of Trace Elementsin Medicine and Biology 2015; 31: 188-192. [DOI] [PubMed] [Google Scholar]