Abstract
Little is known about the occurrence of Cryptosporidium and Giardia in recreational water in China. A total of 52 samples were collected from recreational lakes in Tianjin during a high-occurrence season (June–October) for the waterborne cryptosporidiosis and giardiasis, and the occurrence and genotypes of Cryptosporidium and Giardia were investigated. The results showed that 82.7% (43) and 98.1% (51) of samples were positive for Cryptosporidium oocyst and Giardia cysts, respectively. The mean concentration of parasites was 3.65 oocysts/10 L and 12.58 cysts/10 L, respectively. Molecular characterization revealed that the presence of Cryptosporidium parvum, C. andersoni, C. hominis, C. meleagridis, C. fragile, C. ubiquitum, and Giardia lamblia assemblage A, B and D. The protozoan contamination in the studied lakes may originate from animal feces on ground, which was washed into the lake by stormwater runoff. Nevertheless, there is a potential risk of infection during recreational activities in the lake because the dominant detected protozoan genotypes are common human pathogens. Moreover, microbial indicators analysis does not adequately indicate the protozoan contamination in recreational water. The information from this study will be valuable for future protozoan source tracking, and any further control interventions against Cryptosporidium and/or Giardia infection associated with recreational water.
Introduction
Recreational water has been well documented through outbreaks and epidemiologic studies as a transmission vehicle for pathogens1. Because of their high resistance to the environment and their high infectivity, Cryptosporidium and Giardia are the key etiological agents of waterborne disease2,3. At least 176 recreational water-associated outbreaks attributed to the two parasites have been documented in the five-year period between January 2011 and December 2016 in developed countries, while no outbreak is reported in developing countries2. The distortion reflecting the global pattern of distribution may be resulted from the substantial improvement in data reporting and the establishment of surveillance systems in developed countries4. In fact, it is well known that the highest infection prevalence of parasitic protozoa occurred in developing countries, due to their low economic status and poor sanitation5. The public health implications of the environmental transport of Cryptosporidium and Giardia in these countries, consequently, should be estimated considering that both agents are transmitted by the fecal-oral route and have caused foodborne and waterborne outbreaks.
In the most populous developing country, China, the existence of human cryptosporidiosis and giardiasis has been confirmed by a number of epidemiological investigations6–8, but only one cryptosporidiosis outbreak, which occurred in a pediatric hospital, has so far been reported2,9. This could be a picture of underreporting, as neither of the parasites is listed as a routine inspection item for diarrhea cases in the country. In spite of this, Cryptosporidium and Giardia have been widely reported in various animals, including wildlife, zoo animals, laboratory animals, farm animals, and house pets10–15. On the other hand, both protozoa have also been found in urban wastewater16, surface drinking water sources17–19 and recently in treated recreational waters (i.e. swimming pool waters)20. However, little is known about their occurrence in untreated recreational water. Additionally, more and more people in China are involved in water-related activities. Therefore, it is urgent for the protection of public health to investigate the occurrence of Cryptosporidium and Giardia in recreational water.
In addition, the species/genotype of the protozoa is another important factor that affects the outbreak of cryptosporidiosis and giardiasis, which has been often overlooked in the health risk assessment of Cryptosporidium and Giardia in environmental waters. In effect, not all Cryptosporidium and Giardia species can infect human21–24. Furthermore, the most common causative agents for cryptosporidiosis are C. hominis, C. parvum, C. ubiquitum, and C. meleagridis, though nearly 20 Cryptosporidium species and genotypes have been reported in humans21,22. Likewise, the only known Giardia species that causes human giardiasis is Giardia lamblia, in which subgroups of assemblages A and B are the main etiologies of diarrhea23,24. Consequently, understanding the species or assemblage of the parasites in environmental water is necessary to identify public health risk.
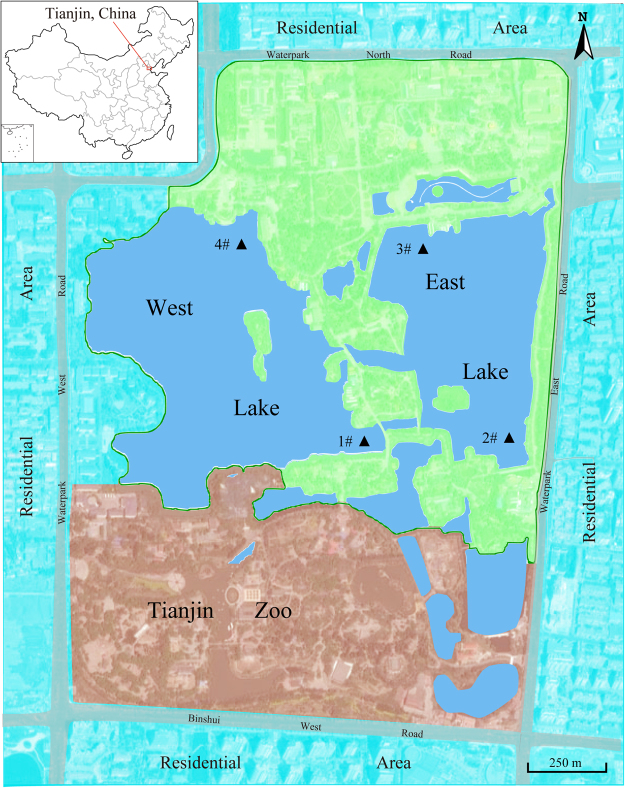
This study was conducted to evaluate the presence and molecular characterization of Cryptosporidium and Giardia in untreated recreational water in the largest urban park of Tianjin, China (Fig. 1), during the high-occurrence season for the waterborne cryptosporidiosis and giardiasis1,2,25–27. The relationships between protozoan concentration and basic water quality indicator such as total coliforms, turbidity and pH, were also explored. The present preliminary survey is believed to be the first attempt to simultaneously detect and genotype the oocyst of Cryptosporidium and cyst of Giardia in recreational water in China, and will be helpful for the identification of public health risk and taking appropriate preventative measures.
Figure 1.
Recreational sampling sites (▲) in Tianjin Waterpark (Arabic numbers represent the sampling sites). The map was created by the authors using software of Adobe Illustrator CS4 (version 14.0.0, http://www.adobe.com/cn/products/illustrator.html).
Results
Precision of the method
The recovery efficiencies from the four replicates using the method involved filtration, flotation, labeling with monoclonal antibody, and microscopy, ranged between 32.50% and 50.83%, with a mean of 41.25%, for Cryptosporidium oocyst, whereas the average recovery rate for Giardia cyst was 38.32%, ranged from 27.01% to 47.45% (Table S1).
Prevalence of Cryptosporidium and Giardia in water samples
Of the 52 tested recreational lake water samples, 43 (82.7%) were positive for Cryptosporidium, with 92.3% (12/13), 84.6% (11/13), 84.6% (11/13), and 69.2% (9/13) in samples from sites 1#, 2#, 3#, and 4#, respectively. Giardia cysts were detected in all samples (98.1%, 51/52) except for the one collected on October 5, 2015 from site 4#. The counts of parasites ranged from 0 to 15 oocysts with a mean of 3.65 oocysts, and 0 to 43 cysts with an average of 12.58 cysts per 10 liters (Table 1). The positive rate for both parasites in samples collected from sampling site 4# was lower than those from other sites. Nevertheless, the difference of concentration of Cryptosporidium oocyst or Giardia cyst among all of the sampling sites was not significant (P > 0.05).
Table 1.
Occurrence of Cryptosporidium oocyst and Giardia cyst in water samples collected from recreational lakesa.
| Sampling sites | No. of sample | Cryptosporidium (no. of oocysts/10 L) | Giardia (no. of cysts/10 L) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of positive (%) | Mean ± SD | Min. − Max. | 95% UCL | No. of positive (%) | Mean ± SD | Min. − Max. | 95% UCL | ||
| 1# | 13 | 12 (92.3%) | 3.54 ± 2.85 | (0–8) | 5.08 | 13 (100%) | 14.54 ± 7.57 | (3–24) | 18.57 |
| 2# | 13 | 11 (84.6%) | 3.85 ± 4.20 | (0–15) | 6.36 | 13 (100%) | 12.23 ± 10.26 | (3–43) | 18.60 |
| 3# | 13 | 11 (84.6%) | 3.46 ± 3.64 | (0–12) | 5.56 | 13 (100%) | 12.38 ± 8.82 | (2–30) | 17.25 |
| 4# | 13 | 9 (69.2%) | 3.77 ± 3.77 | (0–12) | 5.90 | 12 (92.3%) | 11.15 ± 7.01 | (0–27) | 15.10 |
| Total | 52 | 43 (82.7%) | 3.65 ± 3.54 | (0–15) | 4.63 | 51 (98.1%) | 12.58 ± 8.35 | (0–43) | 14.90 |
aSD, standard deviation; UCL, upper confidence limit which was calculated based on 10,000 bootstrap samples using PASW statistics 18 software.
Variations of the concentrations of Cryptosporidium oocyst and Giardia cyst in different times are shown in Fig. 2. Except the peak in late July, the average counts of (oo)cysts in water samples showed a general downtrend during the survey.
Figure 2.

Cryptosporidium oocyst (blue continuous line) and Giardia cyst (red dashed line) concentrations in water samples collected from recreational lakes between June and October, 2015.
Genotyping of protozoa
Nested PCR amplifications were performed for Cryptosporidium and Giardia, respectively, on all the water samples and the expected size of amplicons were produced in 25% (13 out of 52) water samples. DNA sequencing of PCR products confirmed the presence of C. parvum, C. andersoni, C. fragile, C. ubiquitum and Giardia assemblage D in samples collected from site 1#; C. parvum, C. andersoni, C. meleagridis, C. hominis and Giardia assemblage A from site 2#; C. andersoni and Giardia assemblage A from site 3#; and Giardia assemblage B from site 4#. Cryptosporidium parvum, C. andersoni, and Giardia assemblage A were the most commonly detected protozoan species/assemblage (Table 2).
Table 2.
Distribution of Cryptosporidium species and Giardia assemblage in water samples collected from recreational lakes.
| Sample sites | Species of Cryptosporidium (no. of samples) | Assemblage of Giardia lamblia (no. of samples) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| C. parvum | C. andersoni | C. hominis | C. meleagridis | C. ubiquitum | C. fragile | A | B | D | |
| 1# | 2 | 1 | 1 | 1 | 1 | ||||
| 2# | 1 | 1 | 1 | 1 | 2 | ||||
| 3# | 1 | 1 | |||||||
| 4# | 1 | ||||||||
| All sites | 3 | 3 | 1 | 1 | 1 | 1 | 3 | 1 | 1 |
Correlation between protozoa and basic water quality parameters
The results of mean, median and range of the total coliforms, turbidity and pH of lake water are presented in Table 3. As expected, all of the samples were positive for total coliforms, with concentrations ranging between 2 × 103 and 6.5 × 105 most probable numbers (MPN) per liter. Nonparametric Spearman’s correlation two-tailed test showed there was a significant positive correlation between Cryptosporidium and Giardia as well as between them and turbidity (P < 0.01). Neither of the parasites displayed significant correlations with the total coliforms, which are commonly used to indicate microbial contamination (Table 4).
Table 3.
Total coliforms, turbidity and pH of water samples collected from recreational lakes.
| Sample sites | Statistics | Total coliforms (×10 3 MPN/L) | Turbidity (NTU) | pH |
|---|---|---|---|---|
| 1# | Mean ± SD | 66.87 ± 72.18 | 46.09 ± 25.45 | 8.87 ± 0.43 |
| Median | 60 | 38 | 8.81 | |
| Range | 5–290 | 19–106 | 8.27–9.87 | |
| 2# | Mean ± SD | 81.47 ± 133.06 | 52.35 ± 19.36 | 8.86 ± 0.39 |
| Median | 40 | 500 | 8.76 | |
| Range | 2–530 | 28–99 | 8.44–9.76 | |
| 3# | Mean ± SD | 73.04 ± 147.74 | 54.18 ± 26.03 | 8.86 ± 0.41 |
| Median | 22 | 47 | 8.78 | |
| Range | 6–590 | 31–129 | 8.41–9.82 | |
| 4# | Mean ± SD | 93.47 ± 159.1 | 50.26 ± 31.82 | 8.84 ± 0.39 |
| Median | 54 | 41 | 8.79 | |
| Range | 7–650 | 22–134 | 8.24–9.83 | |
| All sites | Mean ± SD | 78.71 ± 129.32 | 50.72 ± 25.59 | 8.86 ± 0.39 |
| Median | 41 | 43 | 8.79 | |
| Range | 2–650 | 19–134 | 8.24–9.87 |
Table 4.
Correlations between the concentration of parasitic pathogens, total coliforms, turbidity and pH of the water analyzeda.
| Cryptosporidium | Giardia | Total coliforms | Turbidity | pH | |
|---|---|---|---|---|---|
| Cryptosporidium | — | 0.669** | 0.179 | 0.383** | −0.054 |
| Giardia | 0.669** | — | 0.303 | 0.363** | 0.134 |
| Total coliforms | 0.179 | 0.303 | — | 0.176 | 0.208 |
| Turbidity | 0.383** | 0.363** | −0.176 | — | −0.574** |
| pH | −0.054 | 0.134 | 0.208 | −0.574** | — |
aSpearman’s correlation coefficient (two-tailed test), *P < 0.05, **P < 0.01.
Discussion
Currently, the monitoring of Cryptosporidium oocyst and Giardia cyst in water is largely performed by using the United States Environmental Protection Agency (USEPA) Method 1623, which involved filtration, isolation of (oo)cysts by immunomagnetic separation, immunofluorescence assay28. However, the high cost of Method 1623 has restricted its usage in most developing countries. A recent review found that only 5% of publications on Cryptosporidium and Giardia detection in water from Central/South America and Africa adopted the Method 162328. Similar testing methods from the United Kingdom and other countries have been involved as alternatives19. In this study, we employed a concentration and purification method adopted by Japan29. As shown in Table S1, this method permitted mean recoveries of 41.25% (relative standard deviation (RSD), 21.54%) for Cryptosporidium and 38.32% (RSD, 26.09%) for Giardia, which could meet the acceptable levels of the Method 1623 (38–100% (RSD < 37%) for Cryptosporidium, 27–100% (RSD < 39%) for Giardia)30.
Oocysts of Cryptosporidium and cysts of Giardia have been reported in recreational water in many previous studies. In Spain, the concentration of Cryptosporidium in recreational rivers varied from 10 to 600 oocysts/10 L and Giardia ranged between 10 and 1600 cysts/10 L31. Each of them was much higher than that reported in the present study (3.46–3.85 oocysts/10 L and 11.15–14.54 cysts/10 L, respectively), while slightly lower protozoan contamination (1–4 Cryptosporidium oocysts and 1–8 Giardia cysts per 10 liters) was reported in some recreational lake waters from the Netherlands32. No Cryptosporidium oocyst was found in samples from a Malaysia recreational lake but a density of 1.7–11 cysts per 10 liters for Giardia was detected33. So the contamination of Cryptosporidium oocysts and Giardia cysts in the recreational lakes herein is within the range those reported elsewhere.
The occurrence of protozoa in environmental water samples is influenced by many factors, including the timing, frequency and site of sampling34. Sampling once in the dry season and the rainy season, respectively, was adopted in many previous studies35,36. However, given that summer and early autumn are the high-occurrence season for the waterborne cryptosporidiosis and giardiasis1,2,25–27, and there was no water recreation in the park in winter, the present study therefore focused on the presence of Cryptosporidium oocyst and Giardia cyst in the hot season. Due to their small size, slow settling velocity, and resistance to environmental stress, oocyst and cyst contamination can persist in water for a long time27. Additionally, the lake water was disturbed by boating and the sampling intervals were relatively short. These factors resulted in a high detection rate of parasites for all samples and no significant differences in protozoan positive rate or densities at different sampling sites.
Genotyping demonstrates that a total of 6 species of Cryptosporidium and 3 assemblages of Giardia lamblia present in this study (Table 2). Most of them have been well reported in animals across China, such as C. parvum in many kinds of animals13, C. meleagridis in chicken37, C. ubiquitum in deer and sheep38, C. andersoni in cattle12,13, and Giardia lamblia in dogs, cats and cattle10,11. Nevertheless, it is noteworthy that all the detected protozoan species/assemblages except C. fragile have been reported in humans21,23,39, and the dominant genotypes, i.e. C. parvum, C. andersoni, and Giardia assemblage A, are the common human pathogens in China8,16, showing their potential public threat and requiring the attention of public health authorities.
Several studies have shown that main sources for protozoan contamination of surface water identified were the intrusion of animal feces or wastewater due to heavy rains40–42. In this study, the replenishment patterns of the lakes depend mainly on tap water and occasional heavy rainfall, so the discharge of storm water may be the major contribution of parasitic pathogens contamination. This is consistent with the variations of concentrations of Cryptosporidium oocyst and Giardia cyst. That is, the downtrend of concentration over time suggesting that no continuous protozoa was discharged into the lake, whereas the peak in late July may be attributed to the wash from fecal-polluted ground by the heavy rainfall on 19 July, 2015 (http://tj.weather.com.cn, Fig. S1). Indeed, the number of oocyst and cyst shed by infected animals was believed to be as high as 106–108 per gram of feces27,43. Considering that all detected Cryptosporidium species and Giardia assemblages have been found in animals, particularly C. fragile has only been found in amphibians, the protozoa in this study appears to be derived from animals and may be associated to the nearby zoo since there are many animals including amphibians. Thus, it is one of the important questions for future studies to determine the source of protozoa in the lakes.
Physical-chemical properties such as turbidity and bacteria such as total coliforms are commonly used as indicators for monitoring water quality. Significant correlations were observed between turbidity and parasites, and between parasites themselves in the present study. These findings are in agreement with previous studies observed in a recreational river in Taiwan, China44, in the Three Gorges Reservoir in China36, and in a reservoir in Spain35. Nevertheless, no parasite was related to indicator bacteria in this study. In contrast, Graczyk, et al.45 found that bacteria count was a good indicator for the presence of Giardia and Cryptosporidium in marine recreational beach water. Meanwhile, they noted that water sample should be collected during times when bather numbers are high and tested in time. The strong resistance of Cryptosporidium and Giardia to environmental stress and long-term viability may be the main cause of different results of the above studies46. Previous study also found that fecal bacterial indicator was not an appropriate index to monitor the presence of Cryptosporidium or Giardia in treated recreational water20. Consequently, the analysis of microbial indicators does not adequately characterize contamination of protozoa in recreational water, especially if the sampling is not timely.
In conclusion, Cryptosporidium and Giardia were commonly detected in the recreational lakes, and their concentration levels are similar to those reported elsewhere. The protozoan contamination may be attributed to heavy rains that wash ground-polluted feces into the lake, and was related to the nearby zoo animals. As the dominant detected protozoan genotypes are common human pathogens, their potential threat requires the attention of public health authorities. In addition, microbial indicators analysis does not adequately indicate the protozoan contamination in recreational water. Future studies should therefore include follow-up work designed to assess the occurrence of protozoa of feces from residents nearby and the zoo animal, allowing a full evaluation of its public health.
Material and Methods
Study site
The studied lakes are located in the Tianjin Waterpark (39.080° to 39.095° N, 117.159° to 117.174°E), which is the largest comprehensive park within the city boundaries of Tianjin, China. All the lakes are connected together and the surface area is about 750,000 square meters. Apart from the surface runoff during storm, the lakes depend mainly on tap water for its replenishment. It is an aquatic venue used for rowing, interactive fountain, wading, and other water recreation activities. There were hundreds of people, mainly the elderly residents nearby, swim in the early morning and evening in summer, even though swimming is banned here.
Sample collection and processing
During the period between June and October, which was the high-occurrence season for waterborne cryptosporidiosis and giardiasis26,27,47,48, water samples were collected from 4 sampling sties (as shown in Fig. 1) at ten-day intervals and a total of 52 samples were obtained. The sampling site 1# is close to the zoo in the south of the West lake and site 4# in the north, site 2# is located in the swimming area in the East lake and site 3# is near the cruise ship terminal. Each sample was collected using a 20-L plastic container. After collection, the samples were transported on ice to the laboratory immediately and parasitic pathogens in the samples were concentrated by a membrane filter dissolution method described previously49. Briefly, water samples were filtered and then the mixed cellulose ester membrane filter (diameter, 142 mm; pore size, 1 μM; Advantec MFS, Inc. Japan) was dissolved in acetone solutions, followed by centrifugation at 1,050 × g for 10 min at 4 °C. The packed pellets were resuspended in a suitable volume (2–10 mL) of distilled water. Half of the resuspension from each sample was used for protozoan enumeration and the other half for DNA extraction.
Morphological examination and enumeration for protozoa
The recovered Cryptosporidium oocysts and/or Giardia cysts in the pellet were separated from debris by flotation on Percoll-sucrose gradients (specific gravity, 1.10)49. Each purified sample was stained with 100 μL of combined fluorescein isothiocyanate (FITC) conjugated anti-Cryptosporidium and anti-Giardia monoclonal antibodies (Waterborne, Inc., New Orleans, LA) in a humid dark chamber at room temperature for 30 min, and then stained with 50 μL of 4′,6′-diamidino-2-phenylindole (DAPI, Waterborne) solution (0.4 μg/mL) for 10 min. The prepared slides were subsequently examined microscopically at 400× magnification using fluorescence microscopy (Olympus, Japan) for the detection and enumeration of Cryptosporidium oocysts and Giardia cysts according the USEPA Method 162330.
To evaluate the recovery efficiency of the method used, the initial precision and recovery efficiency was determined by spiking four 10 L of purified water samples with suspension containing enumerated oocysts and cysts50. Furthermore, a negative control assay, in which all the procedures were performed using deionized water instead of the water sample, was performed on each batch of samples to determine if any contamination occurred during the analysis. All negative control analyzes were negative for oocysts or cysts.
Genotyping of Cryptosporidium and Giardia
Genomic DNA was extracted from each of the sample concentrates using the FastDNA SPIN kit for soil (MP Biomedicals, France) and eluted into 50 μL of reagent-grade water according to previous study51. Small subunit (SSU) rRNA-based nested PCR followed by sequencing techniques were employed to determine the species/genotypes of the protozoa according to previous study52. Briefly, a 435-bp fragment of Cryptosporidium SSU rRNA locus and a 292-bp fragment of Giardia SSU rRNA gene were amplified by two nested PCR, respectively. The sequence of all primers and PCR conditions are specified in Table S2. All positive secondary PCR products were sent to Beijing Augct Co., Ltd. for direct sequencing with the secondary PCR primers using ABI 3730 automated DNA sequencer (BigDye Terminator Chemistry). Nucleotide sequences obtained in the study were aligned with reference SSU rRNA sequences downloaded from the Genbank using the Clustal W programs and analyzed to determine Cryptosporidium species/genotypes and Giardia assemblages using phylogenetic trees.
Microbiological analysis, turbidity and pH measurement
According to the Chinese standard examination method for drinking water-microbiological parameters, five-tube most probable numbers (MPN) procedure was used to enumerate total coliforms53. Briefly, after ten-fold serial dilution, 1.0 mL of each serial dilution was transferred to five tubes of lactose peptone broth containing inverted Durham tubes, and then incubated at 37 °C for 24 ± 2 h. All positive presumptive tubes that demonstrated an acidic reaction or gas production were submitted to the confirmed phase with total coliform test by using eosin methylene blue agar medium53. The turbidity and pH were measured on site for each sample with portable photometer.
Statistical analysis
The paired-samples t-test was employed to evaluate the relationship between the concentrations of Cryptosporidium oocyst and Giardia cyst. The association between total coliform, turbidity, pH and protozoan concentrations was correlated using the nonparametric Spearman’s correlation two-tailed test. Differences with P values of <0.05 were defined as being statistically significant. All statistical tests were performed using PASW Statistics 18 computer software package.
Data availability
All relevant data are fully available without restriction.
Electronic supplementary material
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (No. 51278174), the Natural Science Foundation of Tianjin City (No. 15JCQNJC44000 and No. 15JCZDJC40100), and the Research Found of Tianjin Key Laboratory of Aquatic Science and Technology (No. TJKLAST-PT-2014-4).
Author Contributions
S.X., L.S., and S.H. conceived and designed the experiments; Y.Z. and X.Z. performed the experiments; Y.Z., S.X. and S.H. analyzed the data; Y.Z., S.X., and S.H. wrote the paper. All authors read and approved the final manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-20902-3.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shumin Xiao, Email: xiaoshumin@tcu.edu.cn.
Sike Hu, Email: husike@126.com.
References
- 1.Perkins A, Trimmier M. Recreational Waterborne Illnesses: Recognition, Treatment, and Prevention. Am. Fam. Physician. 2017;95:554–560. [PubMed] [Google Scholar]
- 2.Efstratiou A, Ongerth JE, Karanis P. Waterborne transmission of protozoan parasites: Review of worldwide outbreaks - An update 2011-2016. Water Res. 2017;114:14–22. doi: 10.1016/j.watres.2017.01.036. [DOI] [PubMed] [Google Scholar]
- 3.Hlavsa MC, et al. Outbreaks of Illness Associated with RecreationalWater - United States, 2011-2012. MMWR-MORBID MORTAL W. 2015;64:668–672. [PMC free article] [PubMed] [Google Scholar]
- 4.Baldursson S, Karanis P. Waterborne transmission of protozoan parasites: review of worldwide outbreaks - an update 2004-2010. Water Res. 2011;45:6603–6614. doi: 10.1016/j.watres.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 5.WHO & UNICEF. Progress on drinking water, sanitation and hygiene: 2017 update and SDG baselines. (World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF), 2017).
- 6.Yang Y, et al. Prevalence of and risk factors associated with Cryptosporidium infection in an underdeveloped rural community of southwest China. Infectious diseases of poverty. 2017;6:2. doi: 10.1186/s40249-016-0223-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang, C. et al. Environmental transport of emerging human-pathogenic Cryptosporidium species and subtypes through combined sewer overflow and wastewater. Appl Environ Microbiol (2017). [DOI] [PMC free article] [PubMed]
- 8.Wang R, et al. Genetic characterizations of Cryptosporidium spp. and Giardia duodenalis in humans in Henan, China. Exp Parasitol. 2011;127:42–45. doi: 10.1016/j.exppara.2010.06.034. [DOI] [PubMed] [Google Scholar]
- 9.Feng Y, et al. Extended outbreak of cryptosporidiosis in a pediatric hospital, China. Emerg Infect Dis. 2012;18:312–314. doi: 10.3201/eid1802.110666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu H, et al. Genotypes of Cryptosporidium spp., Enterocytozoon bieneusi and Giardia duodenalis in dogs and cats in Shanghai, China. Parasite Vector. 2016;9:121. doi: 10.1186/s13071-016-1409-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang XX, et al. Occurrence and multilocus genotyping of Giardia intestinalis assemblage C and D in farmed raccoon dogs, Nyctereutes procyonoides, in China. Parasite Vector. 2016;9:471. doi: 10.1186/s13071-016-1771-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li G, et al. Molecular identification and characterization of Cryptosporidium spp. from mainland China. Agric Sci Chin. 2005;4:59–64. [Google Scholar]
- 13.Wang R, et al. Characteristics of Cryptosporidium transmission in preweaned dairy cattle in Henan, China. J Clin Microbiol. 2011;49:1077–1082. doi: 10.1128/JCM.02194-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lv C, et al. Cryptosporidium spp. in wild, laboratory, and pet rodents in China: prevalence and molecular characterization. Appl Environ Microbiol. 2009;75:7692–7699. doi: 10.1128/AEM.01386-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karanis P, et al. Molecular characterization of Cryptosporidium from animal sources in Qinghai province of China. Parasitol Res. 2007;101:1575–1580. doi: 10.1007/s00436-007-0681-x. [DOI] [PubMed] [Google Scholar]
- 16.Liu A, et al. Molecular identification and distribution of Cryptosporidium and Giardia duodenalis in raw urban wastewater in Harbin, China. Parasitol Res. 2011;109:913–918. doi: 10.1007/s00436-011-2333-4. [DOI] [PubMed] [Google Scholar]
- 17.Xiao S, et al. The burden of drinking water-associated cryptosporidiosis in China: The large contribution of the immunodeficient population identified by quantitative microbial risk assessment. Water Res. 2012;46:4272–4280. doi: 10.1016/j.watres.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 18.Hu Y, Feng Y, Huang C, Xiao L. Occurrence, source, and human infection potential of Cryptosporidium and Enterocytozoon bieneusi in drinking source water in Shanghai, China, during a pig carcass disposal incident. Environ Sci Technol. 2014;48:14219–14227. doi: 10.1021/es504464t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feng Y, et al. Occurrence, source, and human infection potential of Cryptosporidium and Giardia spp. in source and tap water in Shanghai, China. Appl Environ Microbiol. 2011;77:3609–3616. doi: 10.1128/AEM.00146-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xiao S, Yin P, Zhang Y, Hu S. Occurrence of Cryptosporidium and Giardia and the Relationship between Protozoa and Water Quality Indicators in Swimming Pools. Korean J. Parasitol. 2017;55:129–135. doi: 10.3347/kjp.2017.55.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ryan U, Fayer R, Xiao L. Cryptosporidium species in humans and animals: current understanding and research needs. Parasitology. 2014;141:1667–1685. doi: 10.1017/S0031182014001085. [DOI] [PubMed] [Google Scholar]
- 22.Zahedi A, et al. Zoonotic Cryptosporidium Species in Animals Inhabiting Sydney Water Catchments. PLoS One. 2016;11:e0168169. doi: 10.1371/journal.pone.0168169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Laishram S, Kang G, Ajjampur SS. Giardiasis: a review on assemblage distribution and epidemiology in India. Indian J. Gastroenterol. 2012;31:3–12. doi: 10.1007/s12664-012-0161-9. [DOI] [PubMed] [Google Scholar]
- 24.Moore, C. E. et al. Molecular Characterization of Cryptosporidium Species and Giardia duodenalis from Symptomatic Cambodian Children. PLoS Negl. Trop. Dis. 10 (2016). [DOI] [PMC free article] [PubMed]
- 25.Rosado-Garcia FM, Guerrero-Florez M, Karanis G, Hinojosa MDC, Karanis P. Water-borne protozoa parasites: The Latin American perspective. Int J Hyg Environ Health. 2017;220:783–798. doi: 10.1016/j.ijheh.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 26.Hopkins J, Hague H, Hudgin G, Ross L, Moore D. An Outbreak of Cryptosporidium at a Recreational Water Park in Niagara Region, Canada. J. Environ. Health. 2013;75:28–33. [PubMed] [Google Scholar]
- 27.Loganthan S, Yang R, Bath A, Gordon C, Ryan U. Prevalence of Cryptosporidium species in recreational versus non-recreational water sources. Exp Parasitol. 2012;131:399–403. doi: 10.1016/j.exppara.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 28.Efstratiou A, Ongerth J, Karanis P. Evolution of monitoring for Giardia and Cryptosporidium in water. Water Res. 2017;123:96–112. doi: 10.1016/j.watres.2017.06.042. [DOI] [PubMed] [Google Scholar]
- 29.Japanese Ministry of Health Labor and Welfare. Methods for the Detection of Cryptosporidium, Giardia and Indicator Microorganisms in Water Supply Systems. Preprint at http://www.mhlw.go.jp/topics/bukyoku/kenkou/suido/kikikanri/dl/ks-0330006.pdf (2018).
- 30.USEPA. Method 1623: Cryptosporidium and Giardia in water by filtration/IMS/FA. EPA 815-R-05-002. (Office ofWater. U.S. Government Printing Office, 2005).
- 31.Castro-Hermida JA, Garcia-Presedo I, Gonzalez-Warleta M, Mezo M. Cryptosporidium and Giardia detection in water bodies of Galicia, Spain. Water Res. 2010;44:5887–5896. doi: 10.1016/j.watres.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 32.Schets FM, van Wijnen JH, Schijven JF, Schoon H. & de Roda Husman, A. M. Monitoring of waterborne pathogens in surface waters in amsterdam, the Netherlands, and the potential health risk associated with exposure to Cryptosporidium and Giardia in these waters. Appl Environ Microbiol. 2008;74:2069–2078. doi: 10.1128/AEM.01609-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lim YA, Ramasame SD, Mahdy MA, Sulaiman WY, Smith HV. Detection and molecular characterization of Giardia isolated from recreational lake water in Malaysia. Parasitol Res. 2009;106:289–291. doi: 10.1007/s00436-009-1602-y. [DOI] [PubMed] [Google Scholar]
- 34.Wilkes G, et al. Bacteria, viruses, and parasites in an intermittent stream protected from and exposed to pasturing cattle: prevalence, densities, and quantitative microbial risk assessment. Water Res. 2013;47:6244–6257. doi: 10.1016/j.watres.2013.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carmena D, Aguinagalde X, Zigorraga C, Fernandez-Crespo JC, Ocio JA. Presence of Giardia cysts and Cryptosporidium oocysts in drinking water supplies in northern Spain. J Appl Microbiol. 2007;102:619–629. doi: 10.1111/j.1365-2672.2006.03193.x. [DOI] [PubMed] [Google Scholar]
- 36.Xiao G, et al. Occurrence and potential health risk of Cryptosporidium and Giardia in the Three Gorges Reservoir, China. Water Res. 2013;47:2431–2445. doi: 10.1016/j.watres.2013.02.019. [DOI] [PubMed] [Google Scholar]
- 37.Wang R, et al. Avian Pathol. 2010. Large-scale survey of Cryptosporidium spp. in chickens and Pekin ducks (Anas platyrhynchos) in Henan, China: prevalence and molecular characterization; pp. 447–451. [DOI] [PubMed] [Google Scholar]
- 38.Wang R, et al. Molecular characterization of the Cryptosporidium cervine genotype from a sika deer (Cervus nippon Temminck) in Zhengzhou, China and literature review. Parasitol Res. 2008;103:865–869. doi: 10.1007/s00436-008-1069-2. [DOI] [PubMed] [Google Scholar]
- 39.Ryan U, Cacciò SM. Zoonotic potential of Giardia. Int. J. Parasitol. 2013;43:943–956. doi: 10.1016/j.ijpara.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 40.Gorham TJ, Lee J. Pathogen Loading From Canada Geese Faeces in Freshwater: Potential Risks to Human Health Through Recreational Water Exposure. Zoonoses Public Health. 2016;63:177–190. doi: 10.1111/zph.12227. [DOI] [PubMed] [Google Scholar]
- 41.Sterk A, Schijven J, de Roda Husman AM, de Nijs T. Effect of climate change on runoff of Campylobacter and Cryptosporidium from land to surface water. Water Res. 2016;95:90–102. doi: 10.1016/j.watres.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 42.Moreira NA, Bondelind M. Safe drinking water and waterborne outbreaks. J Water Health. 2017;15:83–96. doi: 10.2166/wh.2016.103. [DOI] [PubMed] [Google Scholar]
- 43.Ralston BJ, McAllister TA, Olson ME. Prevalence and infection pattern of naturally acquired giardiasis and cryptosporidiosis in range beef calves and their dams. Vet Parasitol. 2003;114:113–122. doi: 10.1016/S0304-4017(03)00134-1. [DOI] [PubMed] [Google Scholar]
- 44.Hsu BM, Huang C, Jiang GY, Hsu CL. The prevalence of Giardia and Cryptosporidium in Taiwan water supplies. J. Toxicol. Environ. Health A. 1999;57:149–160. doi: 10.1080/009841099157728. [DOI] [PubMed] [Google Scholar]
- 45.Graczyk TK, et al. Relationships among bather density, levels of human waterborne pathogens, and fecal coliform counts in marine recreational beach water. Parasitol Res. 2010;106:1103–1108. doi: 10.1007/s00436-010-1769-2. [DOI] [PubMed] [Google Scholar]
- 46.WHO. Risk assessment of Cryptosporidium in drinking water. (World Health Organization, 2009).
- 47.Yoder JS, Gargano JW, Wallace RM, Beach MJ. Giardiasis surveillance - United States, 2009-2010. MMWR-MORBID MORTAL W. 2012;61:13–23. [PubMed] [Google Scholar]
- 48.Hlavsa MC, et al. Surveillance for waterborne disease outbreaks and other health events associated with recreational water–United States, 2007–2008. MMWR-MORBID MORTAL W. 2011;60:1–32. [PubMed] [Google Scholar]
- 49.Aldom JE, Chagla AH. Recovery of Cryptosporidium oocysts from water by a membrane filter dissolution method. Lett. Appl. Microbiol. 1995;20:186–187. doi: 10.1111/j.1472-765X.1995.tb00423.x. [DOI] [PubMed] [Google Scholar]
- 50.Sato MI, et al. Assessing the infection risk of Giardia and Cryptosporidium in public drinking water delivered by surface water systems in Sao Paulo State, Brazil. Sci Total Environ. 2013;442:389–396. doi: 10.1016/j.scitotenv.2012.09.077. [DOI] [PubMed] [Google Scholar]
- 51.Xiao S, et al. Occurrences and genotypes of Cryptosporidium oocysts in river network of southern-eastern China. Parasitol Res. 2012;110:1701–1709. doi: 10.1007/s00436-011-2688-6. [DOI] [PubMed] [Google Scholar]
- 52.Plutzer J, Karanis P, Domokos K, Torokne A, Marialigeti K. Detection and characterisation of Giardia and Cryptosporidium in Hungarian raw, surface and sewage water samples by IFT, PCR and sequence analysis of the SSUrRNA and GDH genes. Int J Hyg Environ Health. 2008;211:524–533. doi: 10.1016/j.ijheh.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 53.GB/T5750.12–2006. Standard Examination Methods for Drinking Water-microbiological Parameters. (Standards Press of China, 2007).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data are fully available without restriction.