Abstract
Although surgical treatment is the gold standard for chronic patellar tendon rupture, the technique of patellar tendon reconstruction is still difficult. Basically, good clinical results of surgical repair for acute patellar tendon rupture have been reported. However, the results of reconstructive surgery for chronic patellar tendon rupture are still inconsistent. Some surgical options have been previously reported. For example, surgeons need to choose between 1- and 2-stage reconstruction. Furthermore, contralateral bone-tendon-bone graft, ipsilateral semitendinosus tendon graft, Achilles tendon allograft, and an artificial ligament have been used to reconstruct the patellar tendon. Generally, surgeons are concerned about postoperative complications, including loss of knee flexion, quadriceps weakness, and wound problems. One of the key points to avoid these complications is to improve proximal patellar migration. The purpose of this article is to present an easy and safe technique to bring down the patellar height with polyethylene tape and to reconstruct the patellar tendon with an artificial ligament. Although it has limitations, the described technique can facilitate reconstruction of chronic patellar tendon rupture.
Chronic patellar tendon rupture is not a common injury. However, disruption of the extensor mechanism at the knee joint will lead to deterioration of sports activity or daily life owing to the functional disability of knee extension.1 Therefore, surgical treatment is the gold standard for chronic patellar tendon rupture. Although good clinical results of surgical repair for acute patellar tendon rupture have been reported,2 the results of reconstructive surgery for chronic patellar tendon rupture are still inconsistent.3, 4 Some surgical options have been previously reported. For instance, surgeons need to choose between 1- and 2-stage reconstruction.5, 6 Furthermore, contralateral bone-tendon-bone graft,7 ipsilateral semitendinosus tendon graft,8, 9 Achilles tendon allograft,10, 11 and an artificial ligament have been used to reconstruct the patellar tendon.12 Generally, primary repair is not indicated for chronic patellar tendon rupture because of proximal patellar migration, poor quality of the remaining tendon, bone atrophy of the patella, and tissue scarring.6 However, in terms of the reconstructive surgical procedure for chronic patellar tendon rupture, orthopaedic surgeons are concerned about postoperative complications, including loss of knee flexion, quadriceps weakness, and wound problems.1, 13 For instance, wound problems were found in 6% to 14% of patients and revision surgery was performed in 25% to 50% after reconstructive surgery for chronic patellar tendon rupture, although all of the previous reports were small case series consisting of only 1 or 2 patients.1 In our experience, one of the key points of the reconstructive technique is to improve proximal patellar migration.
A safe and easy technique to bring down the patellar height using polyethylene tape during the surgical procedure and to reconstruct the patellar tendon with an artificial ligament for chronic patellar tendon rupture is described (Video 1, Table 1).
Table 1.
Indications and Surgical Steps for Procedure Based on Our Experience
| Indications |
| All chronic patellar tendon ruptures with proximal patellar migration |
| Surgical steps |
| Preparation |
| Determine the appropriate patellar height using a lateral radiograph of the contralateral unaffected knee. |
| Assess the difference in patellar height as the distance between the affected and unaffected knees. |
| Consider preoperative skeletal traction for severe proximal patellar migration. |
| Exposure |
| Use a midline longitudinal incision with careful subcutaneous dissection. |
| Technique to bring down patella (first option) |
| Insert a cannulated cancellous screw with a 6.5-mm diameter into the patella. |
| Place a cannulated cancellous screw with a 6.5-mm diameter behind the tibial tuberosity. |
| Pass a polyethylene tape with a 5-mm width through the cavity of the 2 screws. |
| Apply gradual tension to the tape with a tensioning device. |
| Confirm the patellar height with an intraoperative lateral radiograph or fluoroscopy. |
| Reconstruction of patellar tendon |
| Pass the artificial ligament through the proximal pole of the patella under the quadriceps tendon. |
| Draw a figure of 8 at the surface of the patella using the artificial ligament. |
| Create the bone tunnel using a 5.0-mm drill behind the tibial tuberosity distal to the screw. |
| Pass the artificial ligament through the bone tunnel behind the tibial tuberosity. |
| Perform double stapling on the tibial surface. |
Technique
Preparation
For preoperative preparation, lateral radiographs of the bilateral knees are taken to compare the patellar height (Fig 1). Differences in the patellar height between the affected and unaffected knees should be measured. In the case of severe proximal patellar migration, preoperative skeletal traction of the patella for 12 to 24 hours should be considered to decrease quadriceps muscle tension.
Fig 1.
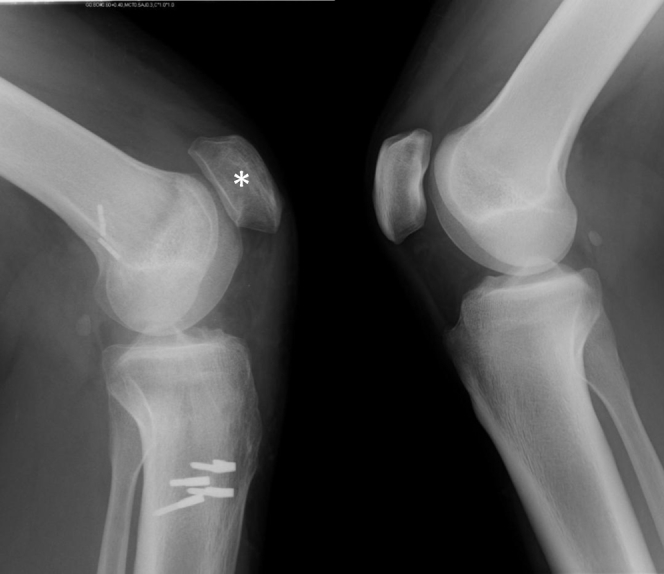
For preoperative preparation, lateral radiographs of the bilateral knees are taken to compare the patellar height. The difference in patellar height between the affected (left) and unaffected (right) knees should be measured. Atrophic change (asterisk) is seen on the affected side.
Surgical Exposure and Technique to Bring Down Patella
The patient is placed supine with a standard leg holder (Mizuho, Tokyo, Japan) allowing full range of motion under general anesthesia. First, a midline longitudinal incision is placed with careful subcutaneous dissection. Second, without releasing the quadriceps femoris, a cannulated cancellous screw (CCS; Biomet, Warsaw, IL) with a diameter of 6.5 mm is inserted into the patella perpendicular to the leg axis, and a CCS with a diameter of 6.5 mm is placed behind the tibial tuberosity (Fig 2). Another option is placement of 2 CCSs with diameters of 5.0 mm in the patella. Third, a polyethylene tape (NESPLON; Alfresa Pharma, Osaka, Japan) with a width of 5 mm is inserted into the cavity of the CCS with a diameter of 6.5 mm in the patella and into the cavity of the CCS with a diameter of 6.5 mm behind the tibial tuberosity (Fig 2). One of the key points is that we should select screws that are 5 mm shorter than the actual length of the bone tunnel to avoid cutting the tape at the edge of the screws. Thereafter, gradual tension is applied to the tapes with a tensioning device (Tighting Gun TGL; Alfresa Pharma) (Fig 3). After tensioning, the appropriate patellar height should be clinically confirmed with the distance between the distal pole of the patella and the tibial tuberosity, as well as an intraoperative lateral radiograph, with the unaffected side used as the reference. Another option is the insertion of 2 polyethylene tapes with widths of 3 mm into the cavity of 2 CCSs with diameters of 5.0 mm, both in the patella separately and behind the tibial tuberosity together.
Fig 2.
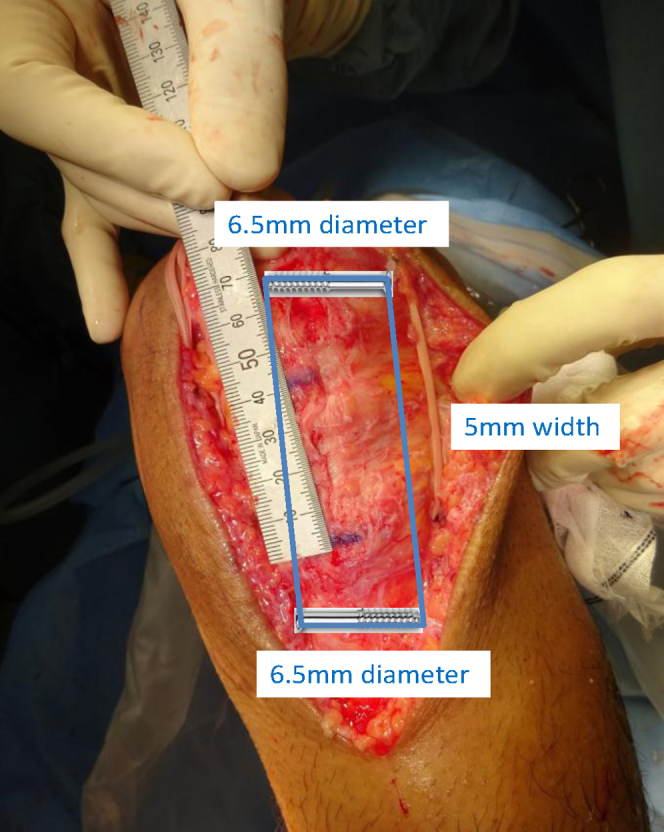
The patient is placed supine with a standard leg holder (Mizuho) allowing full range of motion under general anesthesia (left knee). A midline longitudinal incision is placed with careful subcutaneous dissection. A cannulated cancellous screw (CCS) with a diameter of 6.5 mm is inserted into the central part of the patella perpendicular to the leg axis, and a CCS with a diameter of 6.5 mm is placed behind the tibial tuberosity. Thereafter, a polyethylene tape (NESPLON) with a width of 5 mm is inserted into the cavity of the CCS with a diameter of 6.5 mm in the patella, as well as into the cavity of the CCS with a diameter of 6.5 mm behind the tibial tuberosity.
Fig 3.

Gradual tension is applied to the tapes with a tensioning device (Tighting Gun TGL). After tensioning, the appropriate patellar height should be clinically confirmed with the distance between the distal pole of the patella and the tibial tuberosity (left knee).
Reconstruction of Patellar Tendon With Artificial Ligament
The Leeds-Keio (LK) artificial ligament (LK2-DT; Neoligaments, Leeds, England) is passed through the proximal pole of the patella under the quadriceps femoris tendon and placed to draw a figure of 8 at the surface of the patella (Fig 4). Finally, after creation of the bone tunnel with a 5.0-mm drill behind the tibial tuberosity distal to the screw, the LK artificial ligament is passed through the tunnel, followed by the double-staple method on the tibial surface. The artificial ligament should be fully covered with extensor retinaculum and subcutaneous tissue. After the operation, postoperative radiographs are taken (Fig 5). In our experience, the goal for the patellar height is 3 to 4 mm lower than the unaffected side.
Fig 4.
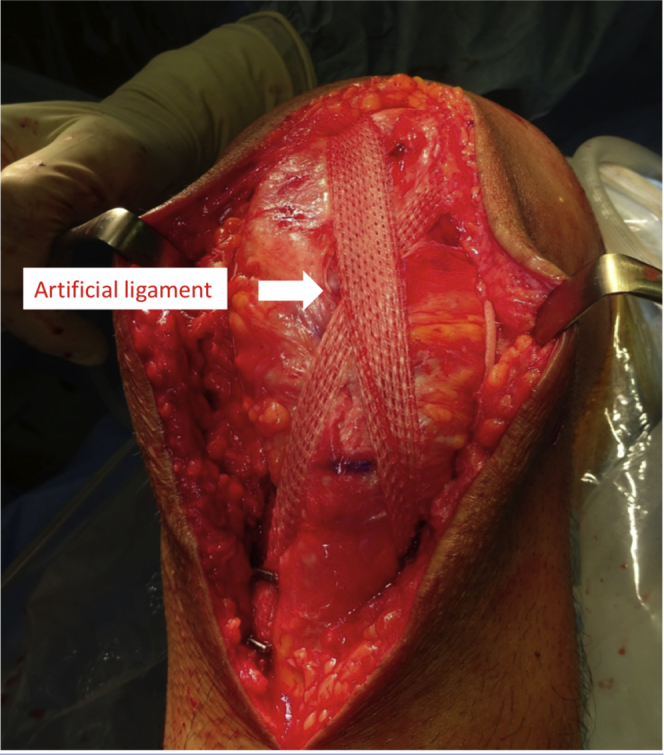
The Leeds-Keio artificial ligament (LK2-DT) is passed through the proximal pole of the patella under the quadriceps femoris tendon and placed to draw a figure of 8 at the surface of the patella (left knee). After creation of the bone tunnel with a 5.0-mm drill behind the tibial tuberosity distal to the screw, the Leeds-Keio artificial ligament is passed through the tunnel, followed by the double-staple method on the tibial surface.
Fig 5.
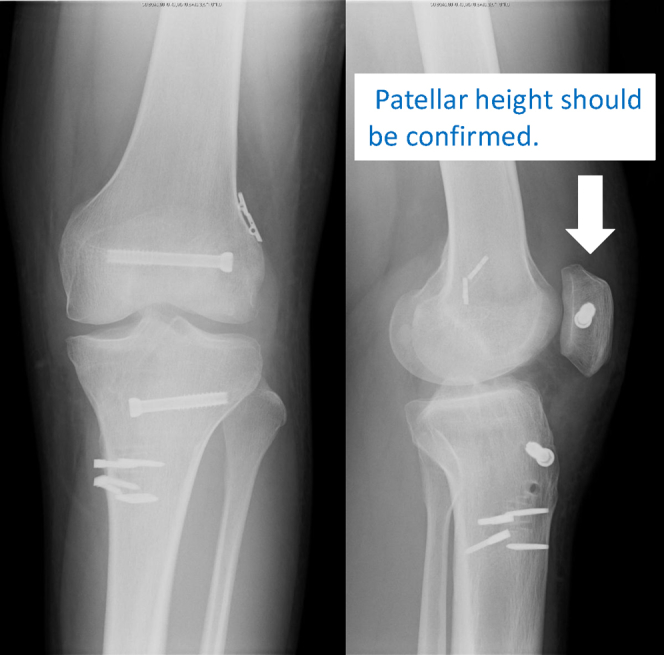
After the operation, postoperative radiographs are taken to confirm the patellar height (left knee). In our experience, the goal for the patellar height is 3 to 4 mm lower than the unaffected side.
Postoperative Rehabilitation
For postoperative rehabilitation, isometric quadriceps exercise begins on the first postoperative day. Range–of–knee motion training is performed starting at 1 week postoperatively, and partial weight bearing is allowed with a hard brace. Full weight bearing is gradually allowed after the acquisition of 70° of flexion. The brace is blocked at 90° of flexion for 2 months and 120° for 3 months after surgery. The brace is completely removed 1 year after the surgical procedure.
Discussion
Generally, chronic patellar tendon rupture occurs after misdiagnosis at the time of the first visit without treatment or with failure of the initial operation. It is common in many young persons with relatively high activity levels. Siwek and Rao14 reported that 38% of knee extensor ruptures were misdiagnosed at the time of the initial visit and that 18% had progressed to chronic cases more than 2 weeks after the injury. The physical finding in patients with chronic patellar tendon rupture is weakness of knee extension torque, which leads to deterioration of sports activity or daily life. As to treatment, primary repair is not indicated for chronic patellar tendon rupture because of proximal patellar migration, poor quality of the remaining tendon, bone atrophy of the patella, and tissue scarring.6 To bring down the patellar height, Isiklar et al.5 used Ilizarov external fixation for 4 to 6 weeks before surgery whereas Siwek and Rao performed direct skeletal traction with 5 lb (2.3 kg) for 4 to 14 days before the surgical procedure. Because these techniques are relatively difficult, a safe and easy technique to lower the patellar height using polyethylene tape for chronic patellar tendon rupture has been developed. In terms of the reconstruction method, contralateral bone-tendon-bone graft,7 ipsilateral semitendinosus tendon graft,8, 9 Achilles tendon allograft,10, 11 and an artificial ligament have been used.7, 8, 10, 11, 12, 13 In this technique, reconstruction was performed with the LK artificial ligament. An advantage of this procedure is that it is not necessary to create a bone hole in the atrophic patella and to harvest the other tendon. Moreover, the reconstructed extensor torque passes through the anterior surface of the patella and coincides with the physiological forces of the patellofemoral joint.15 Because strong initial fixation can be obtained with the artificial ligament, it is possible to start postoperative range–of–knee motion exercise on the first postoperative day.
Some key points of this technique should be noted (Table 2). First, as preoperative preparation, the relation between the diameter of the screw cavity and the width of the polyethylene tape must be confirmed. In our experience, a CCS with a diameter of 6.5 mm is appropriate for tape with a width of 5 mm. Second, assessment of the lateral radiograph of the unaffected knee is important to know the difference in patellar height between the affected and unaffected knees. Third, during the surgical procedure, cannulated screws are required to avoid erosion of the atrophic bone. Last, screws that are 5 mm shorter than the actual length of the bone tunnel should be selected to prevent cutting of the tape at the edge of the screws. The advantages of the technique are as follows: preparation for the procedure is easy, gradual tensioning can be applied while checking the patellar height, there is no need to harvest the other tendon, the procedure is safe for the patient, and the technique does not take much time.
Table 2.
Key Points, Advantages, and Limitations of Procedure Based on Our Experience
| Key points |
| The relation between the screw cavity and width of the tape should be confirmed. |
| The lateral radiograph of the unaffected knee should be assessed. |
| A cannulated screw is required to avoid erosion of the atrophic bone. |
| Screws that are 5 mm shorter than the actual length of the bone tunnel should be selected. |
| Advantages |
| Preparation for the procedure is easy. |
| Gradual tensioning can be performed while checking the patellar height. |
| Harvesting the other tendon is not necessary. |
| The procedure is safe for the patient. |
| The technique does not take much time. |
| Limitations |
| The threshold of the patellar height for this procedure is unknown. |
| It is difficult for the surgeon to loosen the tension of the tape after tensioning. |
| Our procedure pertains to possible changes in contact pressure on the patellofemoral joint. |
| The long-term effects of our technique are unknown. |
| Potential complications of this technique, such as fracture of the tubercle, polyethylene debris, peripatellar stiffness, anterior knee pain development or continuation, and wound issues, are unknown. |
Despite having numerous advantages, our technique has several limitations. First, the threshold of the patellar height for this procedure is unknown. Therefore, in cases of severe proximal patellar migration, preoperative skeletal traction of the patella for 12 to 24 hours should be considered to decrease quadriceps muscle tension. Second, it is difficult for surgeons to loosen the tension of the tape after tensioning. Gradual tensioning is thus a key issue to prevent loosening of intraoperative tension. Third, this procedure can result in changes in the contact pressure on the patellofemoral joint. In addition, the long-term effects of our technique, including clinical outcomes, are unknown. Last, potential complications of this technique, such as fracture of the tubercle, polyethylene debris, peripatellar stiffness, anterior knee pain development or continuation, and wound issues, are unknown. Nevertheless, the described technique can facilitate reconstruction of chronic patellar tendon rupture with an artificial ligament after bringing down the patellar height using polyethylene tape.
Acknowledgment
The authors thank Hiroaki Suzuki for editorial assistance in the preparation of the article.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
For preoperative preparation, lateral radiographs are taken of the bilateral knees to compare the patellar height. The difference in patellar height between the affected and unaffected knees should be measured. The patient is placed supine with a standard leg holder (Mizuho) allowing full range of motion under general anesthesia. A midline longitudinal incision is placed with careful subcutaneous dissection. To lower the patellar height, a cannulated cancellous screw (CCS) with a diameter of 6.5 mm is inserted into the patella and behind the tibial tuberosity. Then, a polyethylene tape (NESPLON) with a width of 5 mm is inserted into the cavity of each CCS with a diameter of 6.5 mm. Gradual tension is applied to the tapes with a tensioning device (Tighting Gun TGL). After tensioning, the Leeds-Keio (LK) artificial ligament (LK2-DT) is passed through the proximal pole of the patella under the quadriceps femoris tendon and placed to draw a figure of 8 at the surface of the patella. After creation of the bone tunnel with a 5.0-mm drill behind the tibial tuberosity distal to the screw, the LK artificial ligament is passed through the tunnel, followed by the double-staple method on the tibial surface (Case 1: left knee, Case 2: left knee).
References
- 1.Gilmore J.H., Clayton-Smith Z.J., Aguilar M., Pneumaticos S.G., Giannoudis P.V. Reconstruction techniques and clinical results of patellar tendon ruptures: Evidence today. Knee. 2015;22:148–155. doi: 10.1016/j.knee.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Belhaj K., El Hyaoui H., Tahir A. Long-term functional outcomes after primary surgical repair of acute and chronic patellar tendon rupture: Series of 25 patients. Ann Phys Rehabil Med. 2017;60:244–248. doi: 10.1016/j.rehab.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Greis P.E., Holmstrom M.C., Lahav A. Surgical treatment options for patella tendon rupture, Part I: Acute. Orthopedics. 2005;28:672–679. doi: 10.3928/0147-7447-20050701-15. quiz 680-681. [DOI] [PubMed] [Google Scholar]
- 4.Greis P.E., Lahav A., Holmstrom M.C. Surgical treatment options for patella tendon rupture, part II: Chronic. Orthopedics. 2005;28:765–769. doi: 10.3928/0147-7447-20050801-13. quiz 770-771. [DOI] [PubMed] [Google Scholar]
- 5.Isiklar Z.U., Varner K.E., Lindsey R.W., Bocell J.R., Lintner D.M. Late reconstruction of patellar ligament ruptures using Ilizarov external fixation. Clin Orthop Relat Res. 1996;(322):174–178. [PubMed] [Google Scholar]
- 6.Temponi E.F., Camelo N., Tuteja S. Reconstruction of chronic patellar tendon rupture with contralateral bone-tendon-bone autograft. Knee Surg Sports Traumatol Arthrosc. 2017;25:2468–2473. doi: 10.1007/s00167-015-3951-7. [DOI] [PubMed] [Google Scholar]
- 7.Frois Temponi E., de Carvalho L.H., Jr., da Silva Bernardes C.O., Presses Teixeira B. Reconstruction of chronic patellar tendon rupture using graft from contralateral patella graft together with reinforcement from flexor tendons. Case report. Rev Bras Ortop. 2016;51:378–382. doi: 10.1016/j.rboe.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen B., Li R., Zhang S. Reconstruction and restoration of neglected ruptured patellar tendon using semitendinosus and gracilis tendons with preserved distal insertions: Two case reports. Knee. 2012;19:508–512. doi: 10.1016/j.knee.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Abdou Y.E. Reconstruction of a chronic patellar tendon rupture with semitendinosus autograft. Arch Orthop Trauma Surg. 2014;134:1717–1721. doi: 10.1007/s00402-014-2080-y. [DOI] [PubMed] [Google Scholar]
- 10.Falconiero R.P., Pallis M.P. Chronic rupture of a patellar tendon: A technique for reconstruction with Achilles allograft. Arthroscopy. 1996;12:623–626. doi: 10.1016/s0749-8063(96)90204-2. [DOI] [PubMed] [Google Scholar]
- 11.McNally P.D., Marcelli E.A. Achilles allograft reconstruction of a chronic patellar tendon rupture. Arthroscopy. 1998;14:340–344. doi: 10.1016/s0749-8063(98)70154-9. [DOI] [PubMed] [Google Scholar]
- 12.Naim S., Gougoulias N., Griffiths D. Patellar tendon reconstruction using LARS ligament: Surgical technique and case report. Strategies Trauma Limb Reconstr. 2011;6:39–41. doi: 10.1007/s11751-010-0101-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mittal R., Singh D.P., Kapoor A. Neglected patellar tendon rupture: Preserve the fat pad. Orthopedics. 2011;34:134. doi: 10.3928/01477447-20101221-29. [DOI] [PubMed] [Google Scholar]
- 14.Siwek C.W., Rao J.P. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am. 1981;63:932–937. [PubMed] [Google Scholar]
- 15.Fujikawa K., Ohtani T., Matsumoto H., Seedhom B.B. Reconstruction of the extensor apparatus of the knee with the Leeds-Keio ligament. J Bone Joint Surg Br. 1994;76:200–203. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For preoperative preparation, lateral radiographs are taken of the bilateral knees to compare the patellar height. The difference in patellar height between the affected and unaffected knees should be measured. The patient is placed supine with a standard leg holder (Mizuho) allowing full range of motion under general anesthesia. A midline longitudinal incision is placed with careful subcutaneous dissection. To lower the patellar height, a cannulated cancellous screw (CCS) with a diameter of 6.5 mm is inserted into the patella and behind the tibial tuberosity. Then, a polyethylene tape (NESPLON) with a width of 5 mm is inserted into the cavity of each CCS with a diameter of 6.5 mm. Gradual tension is applied to the tapes with a tensioning device (Tighting Gun TGL). After tensioning, the Leeds-Keio (LK) artificial ligament (LK2-DT) is passed through the proximal pole of the patella under the quadriceps femoris tendon and placed to draw a figure of 8 at the surface of the patella. After creation of the bone tunnel with a 5.0-mm drill behind the tibial tuberosity distal to the screw, the LK artificial ligament is passed through the tunnel, followed by the double-staple method on the tibial surface (Case 1: left knee, Case 2: left knee).


