Abstract
A revision rotator cuff repair is a technically challenging surgical procedure. This can be further complicated by the presence of poor quality of the cuff tissue, as well as a large greater tuberosity cyst, typically located at the rotator cuff footprint. This Technical Note discusses the surgical approach to deal with a revision rotator cuff tear with a large humeral head cyst. This described arthroscopic technique is performed in a single-stage procedure using a human dermal allograft (GraftJacket) for augmentation. This technique was specifically designed to (1) address the limited area for anchor placement, (2) use a bone graft, demineralized bone matrix, for repairing the bone cyst, and (3) optimize the biology for healing by augmenting the reconstruction with GraftJacket.
Bone cysts on the proximal humerus are common pathological changes that are being increasingly reported in the literature. The literature suggests that the pathologic processes leading to the formation of these cysts could be related to aging, rotator cuff pathology, or as a reaction to previously used bioabsorbable suture anchors.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12 The cysts are commonly reported in the greater tuberosity (GT) area, located posteriorly under the infraspinatus tendon, or the anteriorly under the supraspinatus. These anterior cysts have a statistically significant correlation with rotator cuff injury.4
The key to a successful rotator cuff repair is optimizing the environment to allow for tendon healing, which is especially important in revision surgery, and also, achieving good mechanical fixation of the tendon to its footprint. Accomplishing these 2 conditions in a single-stage surgery could be technically challenging in the presence of a large GT cyst.
This described arthroscopic technique is used to treat a large GT cyst resulted from an initial rotator cuff bridging reconstruction with a human dermal allograft. This procedure, illustrated in Video 1, uses a second human dermal allograft, GraftJacket (Wright Medical Technology, Arlington, TN) in an augmentation configuration, as well as bone grafting to treat the large humeral head cyst.
Surgical Technique
Step 1: Preoperative Evaluation
Preoperative assessment for failed cuff repair begins with a detailed history and physical examination. Important findings indicating recurrence of the tear include recurrent pain and weakness that do not respond to a period of physiotherapy and anti-inflammatory pain medications. Magnetic resonance arthrogram confirms the diagnosis and helps identify humeral head cysts that could increase the difficulty of the repair (Fig 1).
Fig 1.
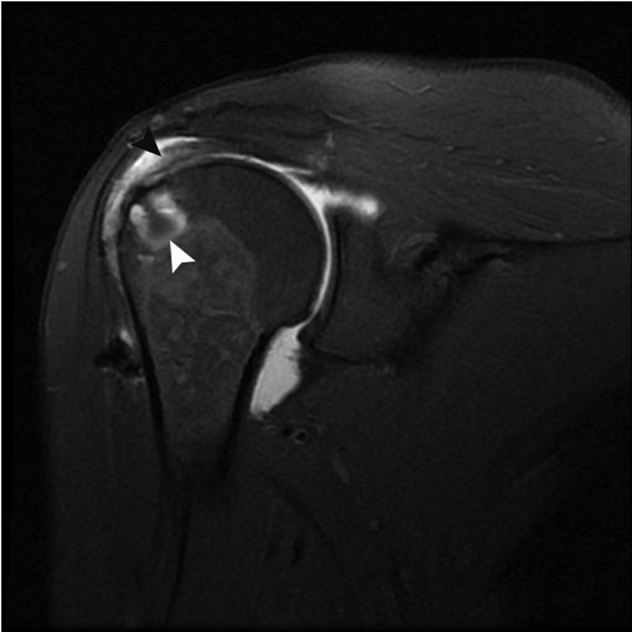
A magnetic resonance arthrography image of the right shoulder, displaying the massive retracted recurrent tear (black arrowhead), with a greater tuberosity cyst (white arrowhead).
Step 2: Positioning, Arthroscope Introduction, and Diagnostic Assessment
Under general anesthesia, the patient is positioned in the lateral decubitus position. The arm position is maintained in 45° of abduction using the SPIDER2 Arm positioner (TENET Medical Products, Smith & Nephew, Andover, MA) (Fig 2). After marking the skin for the portals, a posterior viewing portal is created. The camera is introduced through the posterior viewing portal and a diagnostic arthroscopy is performed to assess the glenohumeral joint. The rotator cuff tendons are checked for tears and retraction from the intra-articular space. The arthroscope is introduced in the subacromial space. The previous human dermal allograft healed at the tendon graft junction with good amount of neovascularization within the graft (Fig 3). The graft tore off from the GT.
Fig 2.

The lateral decubitus positioning of the patient, with the right arm secured using the SPIDER2 Limb Positioner. Note the suggested portals being used: (1) posterior; (2) posterolateral (Wilmington); (3) lateral; and (4) anterior.
Fig 3.
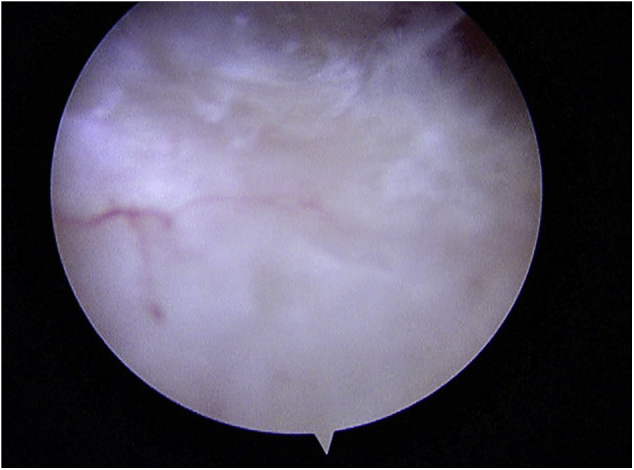
A view of the subacromial space from the posterior portal, showing the GraftJacket healed to the tendon from the previous operation with good vascularity.
An anterior portal is created using an inside-out technique followed by a lateral portal just anterior to the 50-yard line in an outside-in fashion to be used as a working portal and to pass the graft into the joint. A posterior-lateral portal is created as well and used as a visualization portal (refer back to Fig 2 for portal positioning). Two 7-mm Drydoc (Conmed/Linvatec, Largo, FL) cannulas are inserted in the anterior and posterior portals to be used as working portals for the repair. A PassPort cannula (Arthrex, Naples, FL) inserted in the lateral portal will facilitate the insertion of the GraftJacket.
Step 3: Cyst Assessment and Repair
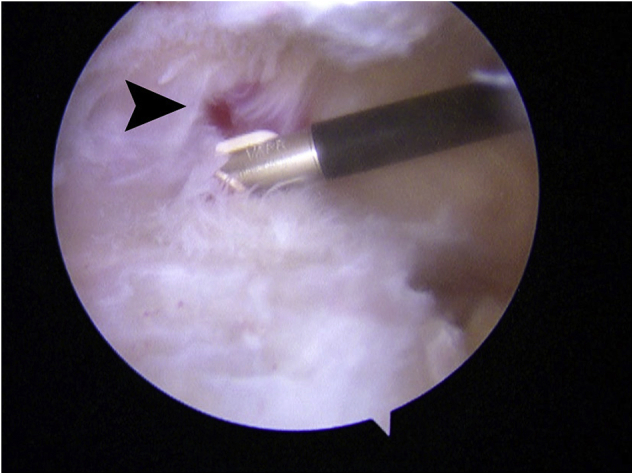
The GT is debrided using a shaver to remove the remaining cuff tissue and then using a burr to create a bleeding healthy bone surface for the rotator cuff repair (Fig 4). There is also significant scarring between the cuff and the under surface of the acromion. A radiofrequency ablation device is introduced from the lateral portal to release the scar tissue (Fig 5). A large cyst filled with gelatinous material is then identified in the GT, which is believed to represent a biological response to the previously used bioabsorbable anchor (Fig 6). The cyst here measured 3 cm in width, depth, and length. Once the contents of the cyst are removed, the bone inside the cyst is lightly burred to obtain a bleeding bone surface (Fig 7). The cuff edge is debrided to a more healthy-looking tendon (Fig 8). The cuff tendon mobility is then assessed using a grasper to determine the ability to mobilize it to the medial footprint with minimal tension for a direct repair (Fig 9). Three ThRevo metal suture anchors (Conmed/Linvatec) are placed at the articular margin of the humeral head, angled toward the subchondral bone to optimize the pullout strength of the anchors (Fig 10). Using direct observation, the anchor placement is confirmed to be outside of the cyst and not penetrating the articular surface (Fig 11).
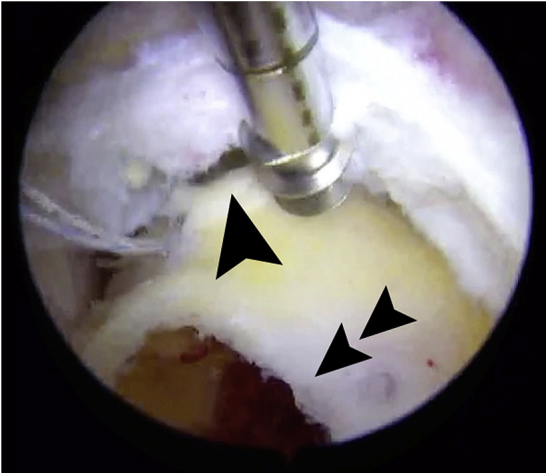
Fig 4.
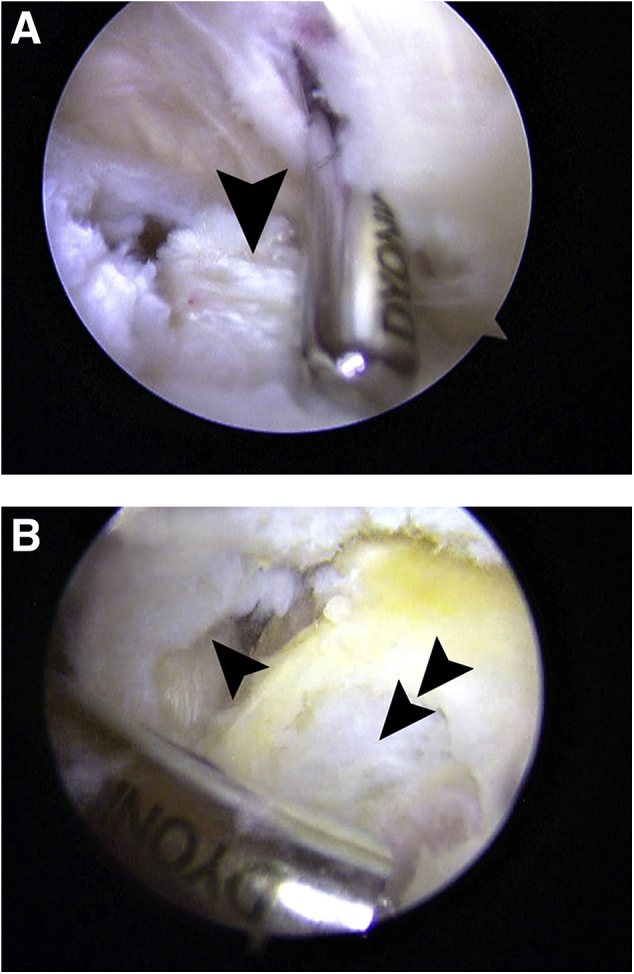
(A) The arthroscope in the posterior portal; the shaver is introduced through a laterally created portal to debride the healed GraftJacket from the GT (black arrowhead). (B) The GT being debrided using a burr from the posterior portal and viewing from the lateral portal. The cyst as starting to appear as the thin covering bone is deroofed. Single arrowhead points out the cuff tear, and the double arrowhead is pointing to the cyst. (GT, greater tuberosity.)
Fig 5.
The radiofrequency ablation device is introduced from the lateral portal to release the adhesions formed between the cuff tissue and the under surface of the acromion. Note the black arrowhead pointing to one of these adhesions.
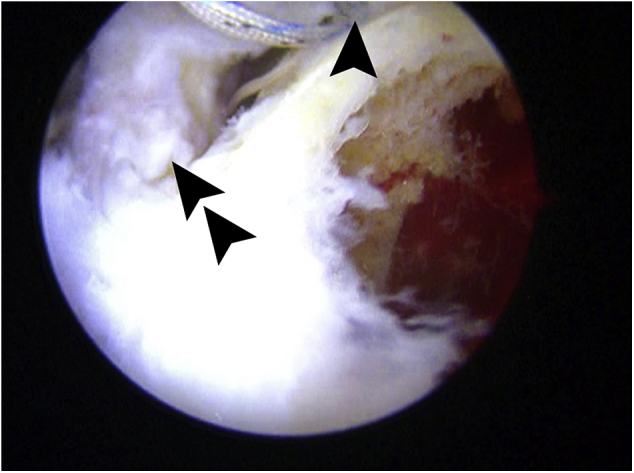
Fig 6.
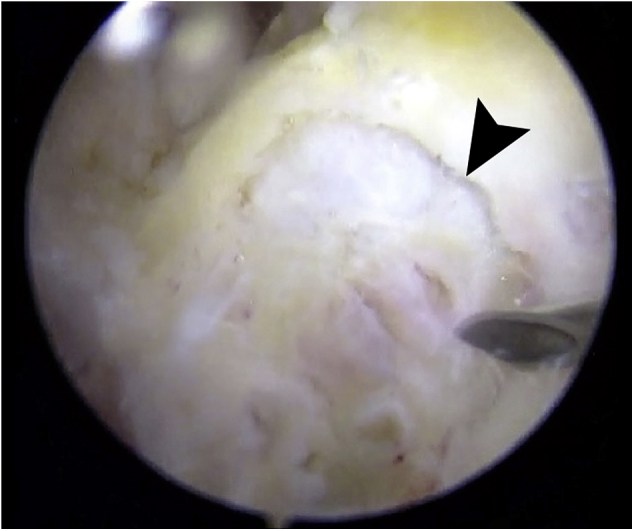
The lateral portal view of the humeral head cyst (black arrowhead) identified, after debriding the greater tuberosity with its gelatinous content.
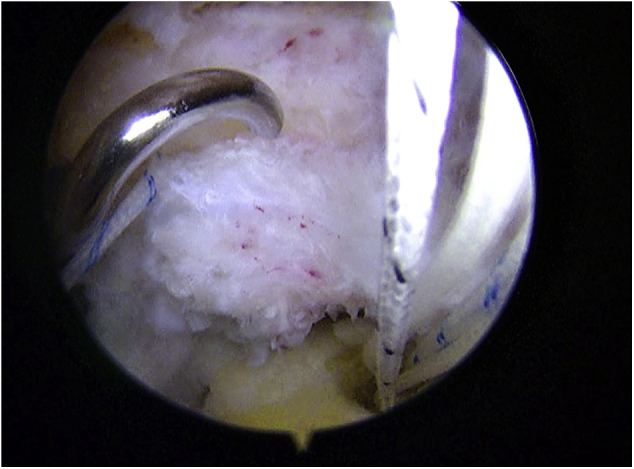
Fig 7.
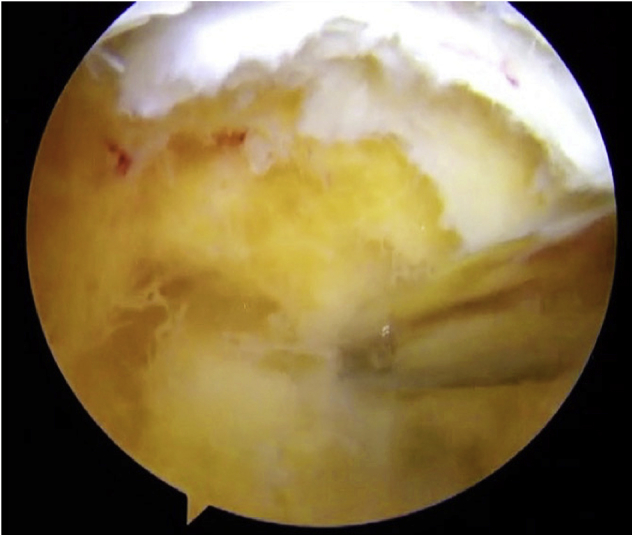
The cyst after evacuating its content using a 4.5-mm shaver. Note the size difference between the cyst and the shaver.
Fig 8.
The lateral portal view of the rotator cuff tissue (black arrowhead) debridement to expose a healthy tendon, with the shaver being introduced through the posterior portal.
Fig 9.
The grasper is introduced from the posterior portal to assess the mobility of the tissue after the release of adhesions.
Fig 10.
The anchor placement lateral to the articular margin (single arrowhead). Note the location of the cyst (double arrowhead).
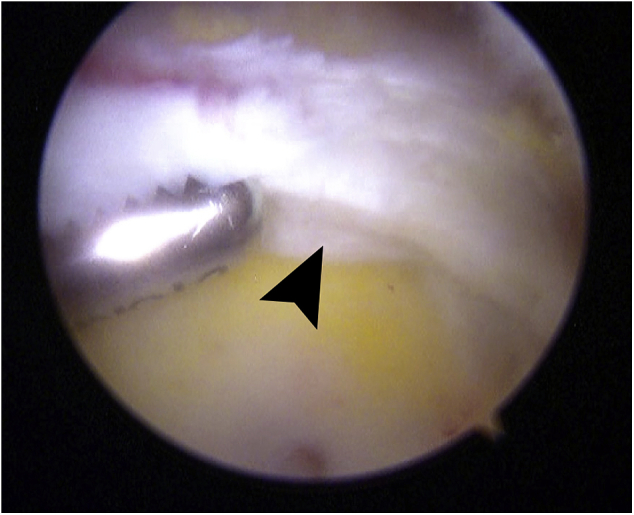
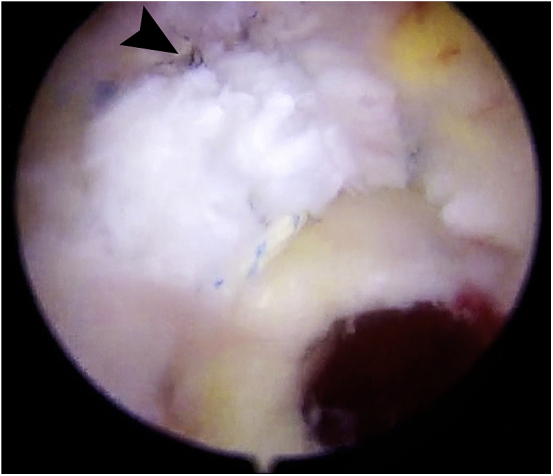
Fig 11.
Looking inside the cyst to ensure that anchors are not penetrating. Note the single arrowhead pointing at the posterior anchor, and the double arrowhead indicating the cuff tear.
Step 4: Tendon Repair and GraftJacket Implantation
The tendon is repaired back to the footprint using 9 simple sutures from the 3 previously described anchors. Looking laterally and using a 45° angle suture passer from the posterior portal, sutures from the anchors are shuttled from posterior to anterior to repair the tendon in a simple suture fashion (Figs 12 and 13). A GraftJacket allograft, 3 cm in width by 3 cm in length, is then prepared with 6 short tailed interference knots13 (Fig 14). A 45° left and right Spectrum suture passer (Conmed/Linvatec) is used to shuttle the 4 medial sutures through the repaired tendon. Using a full thickness bite, each of the 4 sutures is sequentially passed posterior to anterior through the tendon. The super shuttle is grasped through the lateral PassPort cannula in a sequential fashion so each pass is anterior to the previous, to not tangle the short tailed interference knots in the GraftJacket. Two sutures are transported through the posterior portal and 2 through the anterior portal. The graft is then rolled and passed through the lateral PassPort cannula with a grasper on the leading edge (Fig 15). Once inside the shoulder, the sutures through the anterior and posterior cannulas are tensioned to unroll the graft. Each suture is then individually retrieved through the lateral portal and tied using SMC knots onto the tendon side.
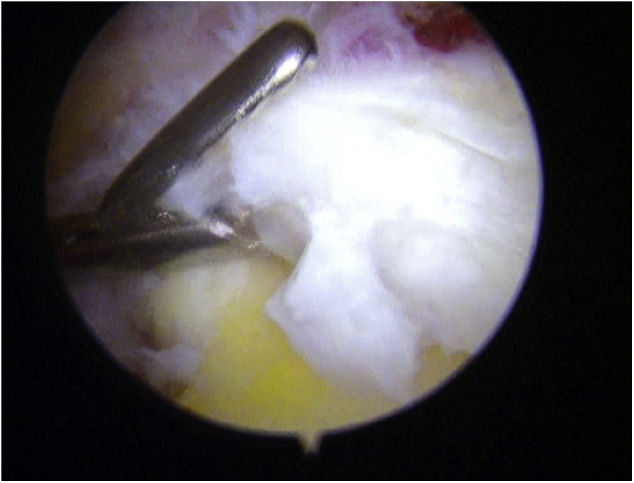
Fig 12.
Coming in from the posterior portal and viewing from the lateral portal, a 45° angled Spectrum Suture Passer is used to pass the sutures through the edge of the cuff to perform the primary repair of the tendon.
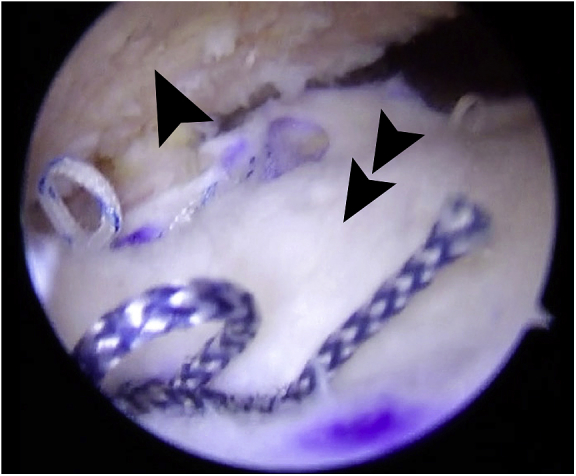
Fig 13.
The repair of the rotator cuff before GraftJacket augmentation. Note the black arrowhead pointing to the completed knots.
Fig 14.
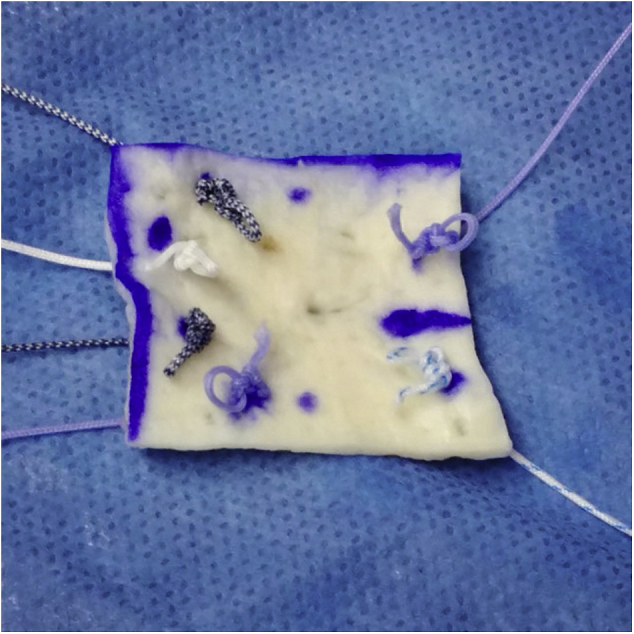
The position of the short tailed interference knots on the prepared GraftJacket, with 4 medial and 2 lateral sutures. Note the use of alternating colored sutures to assist with identification and planning suture placement.
Fig 15.
The allograft (double arrowhead) after being passed into the glenohumeral joint and unfolded, through the Passport cannula placed laterally and viewing from the posteriolateral portal. Note the location of the acromion (single arrowhead).
Step 5: Final Anchors and Demineralized Bone Matrix Injection
Through the lateral portal, the remainder of the graft is secured with 2 ReelX anchors (Stryker, Denver, CO) over the lateral edge of the GT. These 2 knotless anchors are placed lateral to the GT, away from the cyst, achieving optimal mechanical fixation and covering the opening of the cyst. Before final tensioning of the lateral row anchors, demineralized bone matrix (DBM) is injected through a 10-cc syringe to fill the cyst (Fig 16). The GraftJacket augmentation is then tightened to completely cover the large cyst (Fig 17).
Fig 16.
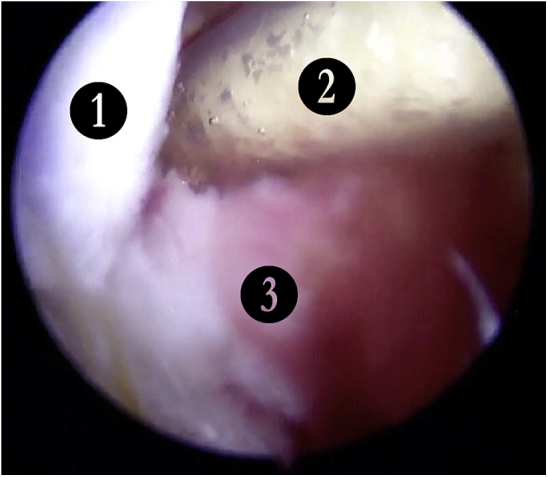
The DBM during injection into the cyst. Note the numbers denoting the (1) GraftJacket, (2) DMB bone graft, and (3) greater tuberosity. (DBM, demineralized bone matrix.)
Fig 17.
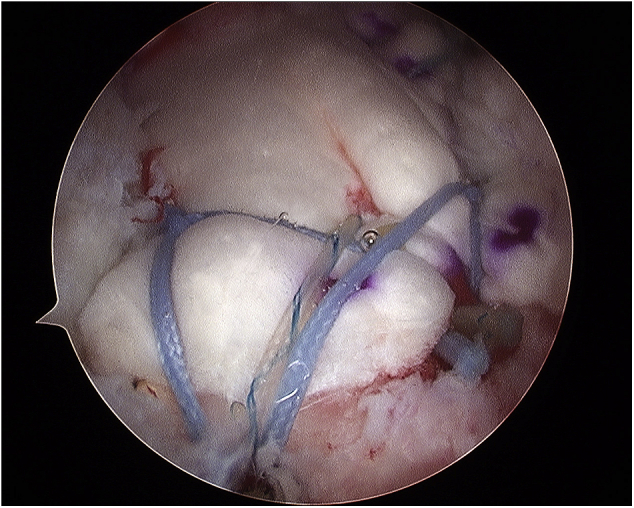
Final lateral view of the repair after tightening the lateral row sutures.
Step 6: Postoperative Rehabilitation
Postoperatively, the patients are managed similar to those with large rotator cuff repairs. Patients are supported in an abduction sling for 6 weeks, removing it daily to perform Codman pendulum, elbow, wrist, and hand exercises. Formal therapy begins at 6 weeks. Pool therapy is very helpful at 6 to 8 weeks to allow passive motion without stress on the healing graft. Active and active-assisted elevation exercises allowed at 8 weeks and gentle strengthening at 12 weeks.
Discussion
Bone cysts in the humeral head can pose technical challenges when trying to repair or reconstruct the rotator cuff tendon back to its footprint. We present our technique to maximize the repair strength and healing potential of a large humeral bone cyst using a single surgical approach. The suture anchors are strategically placed medial to the cyst, and using a graft, this repair is augmented. Using a second row of anchors over the lateral edge of the GT, the bone graft is contained inside the humeral cyst to maximize healing potential.
DBM is used for grafting the cyst due to the size of the cyst, as well as the ease of injecting DBM arthroscopically. This also has the added benefit of avoiding autograft harvest morbidity. DBM is a commercial bone substitute, prepared from allograft. It has been shown to have both osteoinductive and osteoconductive properties close to that of an autogenous iliac crest bone graft.14
Human dermal allograft (GraftJacket) is used as a bridging or augmentation material for massive retracted primary or revision rotator cuff tears, reported with good short- to medium-term outcomes in the literature.13, 15, 16, 17, 18, 19 It has been shown that healing rates with augmented repairs increase radiographic success from 40% to 85%.17
Our technique has the advantage of being a single-stage arthroscopic technique that enables the surgeon to reconstruct the cuff and re-establish the bone stock in one operation (Table 1). Also, it has the advantage of avoiding the use of autograft with its associated donor site morbidity. Some of the disadvantages of the procedure include the technique complexity, which makes it relatively longer than the routine shoulder arthroscopic procedures. The surgeon performing the procedure requires advanced arthroscopic skills and familiarity with the arthroscopic GraftJacket reconstruction technique to make the procedure more efficient.
Table 1.
Advantages and Disadvantages of the Described Technique to Treat a Large Humeral Cyst Found in the Revision of a Failed GraftJacket Reconstruction
| Advantages | Disadvantages |
|---|---|
|
|
DBM, demineralized bone matrix.
We recommend using low pump pressure during the procedure and the use of inflow-outflow pumps with an outflow portal. We find that these pumps are better in controlling the inflow of arthroscopy fluid to the shoulder than other types of pumps. One of the other limitations to this technique is the availability and expense of the GraftJacket and DBM bone graft, which could be an issue in some community hospital settings.
There have been few techniques published to address humeral head cysts. Our technique is similar to what was described by Kim et al.7 They described their technique of using medial and lateral rows of anchors after filling the cyst with allograft or autograft and tamping it down with an impactor. Agrawal and Stinson8 described their technique dealing with the humeral head cysts by using synthetic TruFit plugs (Smith & Nephew, San Antonio, TX) composed of calcium sulfate bone graft substitute that is designed to be used for osteochondral lesions with good success. Burkhart and Klein2 described a technique to address these large cysts by impacting the bone chips using the osteochondral autograft transfer system (Arthrex) impactors, and then using suture anchors within the impacted bone area. The technique described in this Technical Note could lower the risk of failure, by attempting to avoid using any fixation points in the cyst/bone graft cavity, which is believed to put greater tension on the anchor-bone interface leading to failure. Table 2 describes the pearls of the technical procedure.
Table 2.
The Pearls and Pitfalls of the Described Technique to Treat a Large Humeral Cyst Found in the Revision of a Failed GraftJacket Reconstruction
| Pearls | Pitfalls |
|---|---|
|
|
DBM, demineralized bone matrix; GT, greater tuberosity.
Conclusions
This surgical technique addresses the challenge of dealing with revision rotator cuff tears, with a large humeral cyst in the GT footprint. We describe a single-stage technique that is designed to optimize the biological and biomechanical environment for healing rotator cuff tears and grafting a humeral bone cyst while avoiding the donor site morbidity of autogenous bone grafting. We also recommend the use of nonabsorbable anchors for rotator cuff surgery to avoid cyst formation.
Acknowledgment
The authors thank Nicole Paquet, Nova Scotia Health Authority, Halifax, Nova Scotia, Canada, for writing assistance, formatting, and submission to journal.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: C.C. receives payment for lectures including service on speakers bureaus from Smith & Nephew (Complex Knee Course Lab, October 2016, London, ON). I.W. receives payment for lectures including service on speakers bureaus from Smith & Nephew and Depuy. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The description of a technique used to revise a failed GraftJacket rotator cuff reconstruction, for an individual with a large humeral head cyst. The single-stage technique is performed in the lateral decubitus position, after failed physiotherapy and other conservative measures, using another GraftJacket, as well as demineralized bone matrix.
References
- 1.Williams M., Lambert R.G.W., Jhangri G.S. Humeral head cysts and rotator cuff tears: An MR arthrographic study. Skeletal Radiol. 2006;35:909–914. doi: 10.1007/s00256-006-0157-6. [DOI] [PubMed] [Google Scholar]
- 2.Burkhart S.S., Klein J.R. Arthroscopic repair of rotator cuff tears associated with large bone cysts of the proximal humerus: Compaction bone grafting technique. Arthroscopy. 2005;21:1149.e1–1149.e5. doi: 10.1016/j.arthro.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 3.Levy D.M., Moen T.C., Ahmad C.S. Bone grafting of humeral head cystic defects during rotator cuff repair. Am J Orthop (Belle Mead NJ) 2012;41:92–94. [PubMed] [Google Scholar]
- 4.Fritz L.B., Ouellette H., O'Hanley T., Kassarjian A., Palmer W.E. Cystic changes at supraspinatus and infraspinatus tendon insertion sites: Association with age and rotator cuff disorders in 238 patients. Radiology. 2007;244:239–248. doi: 10.1148/radiol.2441050029. [DOI] [PubMed] [Google Scholar]
- 5.Galatz L.M., Rothermich S.Y., Zaegel M., Silva M.J., Havlioglu N., Thomopoulos S. Delayed repair of tendon to bone injuries leads to decreased biomechanical properties and bone loss. J Orthop Res. 2005;23:1441–1447. doi: 10.1016/j.orthres.2005.05.005.1100230629. [DOI] [PubMed] [Google Scholar]
- 6.Glueck D., Wilson T.C., Johnson D.L. Extensive osteolysis after rotator cuff repair with a bioabsorbable suture anchor: A case report. Am J Sports Med. 2005;33:742–744. doi: 10.1177/0363546504269254. [DOI] [PubMed] [Google Scholar]
- 7.Kim K.C., Rhee K.J., Shin H.D., Kim Y.M. Arthroscopic footprint reconstruction of a bone cyst-associated rotator cuff tear. Knee Surg Sports Traumatol Arthrosc. 2007;15:1486–1488. doi: 10.1007/s00167-007-0326-8. [DOI] [PubMed] [Google Scholar]
- 8.Agrawal V., Stinson M. Arthroscopic grafting of greater tuberosity cyst and rotator cuff repair. Arthroscopy. 2007;23:904.e1–904.e3. doi: 10.1016/j.arthro.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 9.Nho S.J., Provencher M.T., Seroyer S.T., Romeo A.A. Bioabsorbable anchors in glenohumeral shoulder surgery. Arthroscopy. 2009;25:788–793. doi: 10.1016/j.arthro.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 10.Pearsall A.W., Bonsell S., Heitman R.J., Helms C.A., Osbahr D., Speer K.P. Radiographic findings associated with symptomatic rotator cuff tears. J Shoulder Elbow Surg. 2003;12:122–127. doi: 10.1067/mse.2003.19. [DOI] [PubMed] [Google Scholar]
- 11.Müller M., Kääb M.I., Villiger C., Holzach P. Osteolysis after open shoulder stabilization using a new bio-resorbable bone anchor: A prospective, non-randomized clinical trial. Injury. 2002;33:30–36. doi: 10.1016/s0020-1383(02)00130-4. [DOI] [PubMed] [Google Scholar]
- 12.Pilge H., Spang J., Rose T., Wolter H., Woertler K., Imhoff A.B. Osteolysis after rotator cuff repair with bioabsorbable anchors. Arch Orthop Trauma Surg. 2012;132:305–310. doi: 10.1007/s00402-011-1369-3. [DOI] [PubMed] [Google Scholar]
- 13.Wong I., Burns J., Snyder S. Arthroscopic GraftJacket repair of rotator cuff tears. J Shoulder Elbow Surg. 2010;19:104–109. doi: 10.1016/j.jse.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 14.Kang J., An H., Hilibrand A., Yoon S.T., Kavanagh E., Boden S. Grafton and local bone have comparable outcomes to iliac crest bone in instrumented single-level lumbar fusions. Spine (Phila Pa 1976) 2012;37:1083–1091. doi: 10.1097/BRS.0b013e31823ed817. [DOI] [PubMed] [Google Scholar]
- 15.Bond J.L., Dopirak R.M., Higgins J., Burns J., Snyder S.J. Arthroscopic replacement of massive, irreparable rotator cuff tears using a GraftJacket allograft: Technique and preliminary results. Arthroscopy. 2008;24:403–409. doi: 10.1016/j.arthro.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 16.Kokkalis Z.T., Mavrogenis A.F., Scarlat M. Human dermal allograft for massive rotator cuff tears. Orthopedics. 2014;37:e1108–e1116. doi: 10.3928/01477447-20141124-59. [DOI] [PubMed] [Google Scholar]
- 17.Barber F.A., Burns J.P., Deutsch A., Labbé M.R., Litchfield R.B. A prospective, randomized evaluation of acellular human dermal matrix augmentation for arthroscopic rotator cuff repair. Arthroscopy. 2012;28:8–15. doi: 10.1016/j.arthro.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 18.Wong I.H., Burns J., Snyder S. Arthroscopic GraftJacket repair of rotator cuff tears. J Shoulder Elbow Surg. 2010;19:104–109. doi: 10.1016/j.jse.2009.12.017. (2 suppl) [DOI] [PubMed] [Google Scholar]
- 19.Ferguson D.P., Lewington M.R., Smith T.D., Wong I.H. Graft utilization in the augmentation of large-to-massive rotator cuff repairs: A systematic review. Am J Sports Med. 2016;44:2984–2992. doi: 10.1177/0363546515624463. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The description of a technique used to revise a failed GraftJacket rotator cuff reconstruction, for an individual with a large humeral head cyst. The single-stage technique is performed in the lateral decubitus position, after failed physiotherapy and other conservative measures, using another GraftJacket, as well as demineralized bone matrix.


