Abstract
Background
The role of wound drainage after total knee arthroplasty is still considered controversial as although closed drainage systems have been believed to be effective in decreasing the post-operative complications, they could also facilitate the bleeding and increase the rate of transfusion and infection. We have conducted the current study to compare the outcomes superficial subcutaneous, one deep, and two deep drain techniques after total knee arthroplasty.
Methods
Between 2014 and 2015 sixty consecutive patients were prospectively selected and underwent primary total knee arthroplasty. Patients randomized to receive one superficial, one deep and two deep drains at the end of operation. Tourniquet was used and opened at the end of the surgery after dressing. Patients were studied for volume of blood loss, hemoglobin drop, number of transfusion, and any complications. Knee range of motion and diameter were measured and compared with contralateral side in all cases at the end of the third day.
Results
There was no statistical difference regarding red blood cell volume loss, Hb drop, and transfusion rate between groups. Patients in one superficial group had the most sever post-operative ecchymosis. Knee flexion and swelling were the same in all groups. Patients in one superficial drain group had the worst VAS for the pain. Need for early blood transfusion was significantly higher in two deep drain group. In one deep drain group returned back to operating room for sever hemarthrosis and wound dehiscence was occurred in a patient. One patient in one deep group had also developed mild thrombo-emboli.
Conclusion
Regarding the blood volume loss after total knee arthroplasty there is no difference between superficial drainage and even more effective intra-articular techniques. Outcome and complication rates are the same.
Level of evidence: II
Keywords: Hemorrhage, Knee arthroplasty, Transfusion
Introduction
There are different schools of thought regarding the use of vacuum drainage after TKA; each concept having its own pros and cons (1, 2). Using a variable indwelling vacuum drainage in the intra-articular space will evacuate blood from the joint space and may impact the rate of complications. These complications mostly include wound complications such as bruising, hematoma formation, blistering, serous ooze and wound dehiscence as well as general complications such as blood loss and DVT. Infections including the deep and superficial forms are also a very important category of complications that should be considered when choosing a drainage method.
Many studies have compared the blood loss and infection rates between the drained and non-drained groups in order to elucidate the effect of the drainage method on the prognosis of TKA surgery; However, the results have been contradictory, necessitating more studies to untangle the problem (3, 4). We have conducted this comparative prospective study to explore the impact of different drainage techniques on patient’s blood loss and related complications. Our main focus is to evaluate the impact of the number and position of the drains on early complications and clinical outcomes.
Materials and Methods
A total of 60 patients (16 males and 44 females) undergoing TKA for the first time were included in this prospective randomized study from Sep 2014 to Oct 2015. The average age of the patients was 66±12.8 years old (range: 5 to 78 years). The study was approved by the Ethics Committee of Urmia University of Medical Sciences (95-345). An informed consent was obtained from all patients. All patients undergoing primary TKA for osteoarthritis or rheumatoid arthritis were included in the study. Patients with severe varus or valgus deformity (>200); patients with concomitant medical diseases or history of thromboembolic issues who need additional treatments; any use of antithrombotic devices (pneumatic device or vena cava filters); and patients with uncontrolled hypertension were excluded from the study. Patients were randomly divided by means of concealed envelopes into 3 groups: placement of one superficial drainage tube under the skin (group A), one 14Fr intra-articular drainage tube (group B), or two 12Fr and 14Fr intra-articular drainage tubes (group C). All drains were used from the same commercial brand (SUPA, Iran), loaded with similar negative pressure, and used with the same size reservoirs (600ml bottles). Spinal anesthesia was applied for all patients. All operations were done by the same senior attending surgeon and the same technique. After performing the classic TKA incision, the quadriceps splitting approach was carried out. Tourniquet was used prior to the incision and opened at the end of the surgery after dressing. Zimmer® prostheses (gender type) were used for all patients. The skin was closed by means of interrupted mattress sutures. Three-layered sterile gauzes were applied for dressing and the knees were wrapped by elastic bandages. Femoral nerve block along with intravenous Apotel® (Paracetamol) transfusion and narcotic agents were used for postoperative pain control. Elastic stockinette as well as Enoxiheparin, 60 mg (Clexane, Sanofi, France) was prescribed as antithrombotic agents. Enoxiheparin was continued for 20 days post-surgery. Blood transfusion was considered when Hb dropped to <8.5 g/dl or patients developed any signs of hypovolemia including tachycardia and hypotension. Blood transfusion was performed to stabilize the patient’s condition and increasing the Hb level up to 10 g/dl. Hb, Hct, and blood loss volume were measured daily until day 3 post-operation. The drain tubes were removed 48 hours post-surgery. The volume of red blood cell loss was calculated using Gross method:

The preoperative circulating blood volume was calculated by Nadler’s formula:
For Males:
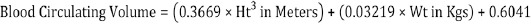
For Females:

The intra-operative blood loss was not measured due to tourniquet use and difficulty in measurement of small amounts of bleeding. The blood volume absorbed by each gauze (4”×4”) was estimated to be 30 cc. By the 3rd day after surgery patients were clinically evaluated for degree of flexion as well as swelling and ecchymosis. The degree of flexion was measured using a goniometry when the patients were asked to actively flex their knees as could as possible. The swelling was assessed by measuring the equator of thigh 3 cm above the patella and compared to the other side. The area of each ecchymosis was also calculated by from the geometric shape. Pain assessment was performed using a visual analog scale (VAS). Patients were allowed for tolerated weight bearing on the 3rd day. The rehabilitation protocol was similar in all patients. All patients were followed up to 6 months for any signs and symptoms of infection. Evaluation of early complication including bleedings that need blood transfusion as well as infection was performed 4 days after operation; however, patients’ functions including knee flexion were monitored within the 6-month follow up duration.
Statistical Analysis
SPSS software version 17 (Illinois, USA) was used for data analysis. Number, percentage, and mean ± standard deviation were used as descriptive statistics. The normal distribution was assessed using Kolmogorov-Smirnov test in all three groups and then repeated measure ANOVA (Tukey’s post hoc test) was used to compare the quantitative data. A P<0.05 was considered as statistically significant.
Results
No significant difference was found in red blood cell loss volume between the 3 groups: A (1.01±0.27 L), B (1.08±0.48 L), and C (1.1±0.24 L) (P=0.73). Also, no significant difference was found in the hemoglobin drop among the 3 groups in three days follow up: A (3.5±1.11), B (3.5±1.43), and C (3.48±1.36) (P=0.9) [Figure 1]. There was no significant difference in the transfusion rate between the 3 groups (P=0.1).
Figure 1.

Measured repeat test shows pattern of Hb drop in three groups.
Table 1 shows the bleeding data of patients. Early blood transfusion was done for 4 patients in group C and 2 in group B due to symptomatic drop in blood pressure in early hours after surgery. The ecchymosis area in group A was 78.57±34.5 cm2; no ecchymosis in group B; and only one patient with a 60 cm2 ecchymosis in group C (P=0.8). Dressing reinforcement or change due to blood soaking was needed in 9 patients, from which, 7 were in group B. Except for 2 patients whose hospitalization was prolonged due to thromboembolic events and bleeding, all other patients discharged by the 4th day. The difference in thigh diameter between two limbs were 1.07±0.04 in group A; 1.05±0.02 in group B; and 1.05±0.03 in group C (P=0.2). Table 2 shows the range of motion in patients in all 3 groups on the day of discharge. It was nearly the same in all groups (P=0.2). The VAS for groups A, B, and C was 5.5±1.19, 4.3±2.1, and 3.2±1.76, respectively (P=0.03). Patients with superficial drains had more sever post operative pain.
Table 1.
Volume of bleeding and transfusion in three groups
| Variable | Group A (superficial drainage) | Group B (one deep drain) | Group C (two deep drain) |
|---|---|---|---|
| Total hemovac blood | 167.3±134.7 | 868.4±377 | 1256.3±386.3 |
| Hb drop day 1 | 2.8±1.14 | 3.1±1.22 | 3.11±1.18 |
| Hb drop day 2 | 0.6±0.94 | 1.03±0.96 | 0.84±0.96 |
| Hb drop day 3 | 0.1±1.22 | 0.5±1.6 | 0.4±1.36 |
| No of patients transfused | 8 | 12 | 15 |
| No of units of blood transfused | 0.5 ±0.07 | 0.7±0.85 | 1.15±0.83 |
Table 2.
Mean of active flexion of knee at the end of third day
| Group | Mean flexion±SD |
|---|---|
| Group A (superficial drainage) | 71.9±17.6 |
| Group B (one deep drain) | 82.4±11.8 |
| Group C (two deep drain) | 84.5±9.6 |
Complications
Only 1 female patient in group B was affected by a non-severe thromboembolic issue who was recovered within 2 days and hence, her hospitalization course was prolonged for additional 3 days. There was only one bleeding and wound dehiscence case in group B. He developed a sever hemarthrosis two hours after surgery with sever bleeding through incisional wound. He was returned back to the operating room and the hamarthrosis was evacuated. Although he had no further bleeding, his hospitalization prolonged for 2 more day. There was no deep or superficial infection in any of the study groups.
Discussion
The supra-patellar pouch together with the posterior capsular space of the knee provide a potential space for accumulation of post-operative bleeding with any arthroplasty technique; So, the drainage system after total knee arthroplasty has a great importance in prevention of post operation complications (5, 6).
In this study, 3 cohorts with different methods of drainage were compared for post-operative blood loss, number of transfusions, and early postoperative complications after primary TKA. According to the results, the number and position of the drains had no significant effect on blood loss volume, Hb drop, and transfusion rate. However, the need for transfusion was much earlier in 2-deep-drains group. There was also no significant difference in early post-operative complications. The superficial drain system does not drain the intra-articular blood and, theoretically, it should be more effective in tamponing the knee joint; however, this was not the scenario in the current study. In fact, releasing the posterior capsule results in the perforation of the balloon. This explains why Hb drop in superficial and deep groups does not differ.
In this study, we tried to achieve an exact matching between the two groups. However, there is a difference in the patients’ hemoglobin levels and blood capacity that can affect the results. Also, blood transfusion was required in the elderly patients undergoing joint replacement regardless of the bleeding volume due to their low cardiovascular and pulmonary capacity. Ultimately, the removal of these specimens has led to a reduction in the sample size.
Intermittent clamping of the suction drain tube is a moderated technique described in the literature. Yamada showed that a 24-h clamping period is more effective than 1-h clamping time in terms of blood loss; however, they reported a high complication rate in the 24-h group (22.7%), and the study did not continue (6). This can be attributed to the fact that releasing the drain tube after 24 hours induces a negative pressure capable of detaching the clots from the arterial ends and aggravates bleeding. Larsson had previously shown that the reactive blood flow increased with the peak flow appearing within 5 minutes when the tourniquet was released (7). It has also been shown that most of the blood loss in TKA occurs during the first few post-operative hours (8). The knee joint is no longer a closed system after total knee arthroplasty. The body’s coagulation system is the most effective procurator for stopping blood loss in these situations. Several studies have reported the efficacy of tranexamic acid in decreasing blood loss after TKA (9-11). These studies have emphasized the role of blood coagulation system in controlling total knee arthroplasty post-bleeding.
Expectedly, the most severe ecchymosis was occurred in group A. Ecchymosis is a sign of subcutaneous spreading of blood and depends on the bleeding volume and pressure (12). Subcutaneous drains were less effective in preventing ecchymosis than the deep drains. One may expect that the most dressing reinforcement was also occurred in group A, but it didn’t happen. Seven out of 9 dressing changes in group B were due to the leakage from the drain tube rather than the surgical wound itself.
The highest pain scores seen in group A may be due to the more severe joint distention in this group. Pain after TKA is multifactorial (13, 14). Ligament tightness also plays an important role in post-TKA pain. In acute conditions, however, it may be claimed that patients with superficial drains might have more severe pain (15, 16). There was also no difference between the 3 groups considering the thigh diameter and range of motion. Knee flexion at day 3 after operation was a non-significantly less in group A. The presence of the drain tube on its own could create a mechanical block in deep drain groups, explaining why the similarity of the range of motion in all groups despite a less sever distended joint.
The previous trials have demonstrated no difference between non-drain and drain methods (17, 18). The present study also suggests that the superficial drain method does not significantly increase the risk of thromboembolic syndrome.
Infection is the most dreadful complication regarding application of drain. According to this study, no significant difference in infection was found between the three groups. Due to low incidence of infection after TKA, however, the sample size of this study is not statistically powerful to prove this point. Further studies with larger sample sizes and proper design are needed to draw a conclusion.
There are several reports throughout the literature comparing the drainage and non-drainage methods (19). The present study has looked at problem from a different perspective, speculating the subcutaneous indwelling closed-suction drainage.
More officious drainage through deployment of more than one suction drain offers no beneficial alternative to traditional drainage methods. On the other hand, more drainage does not mean less complication rate. Furthermore, the main shortcoming of superficial drainage method, i.e. bleeding, does not differ with deep drain methods. Using intra-articular tamponade was not successful in decreasing the blood loss. In fact, the coagulation system of body plays an important role in hemostasis.
There is no conflict of interest to be reported.
Acknowledgments
This study was financially supported by Urmia University of Medical sciences.
References
- 1.Zhang XN, Wu G, Xu RZ, Bai XZ. [Closed suction drainage or non-drainage for total knee arthroplasty: a meta-analysis] Zhonghua Wai Ke Za Zhi. 2012;50(12):e1119–25. [PubMed] [Google Scholar]
- 2.Sun JG, Zhai S, Yuan H. [Systematic review of the earlier safety of closed suction drainage for knee arthroplasty] Zhonghua Wai Ke Za Zhi. 2009;47(20):e1544–9. [PubMed] [Google Scholar]
- 3.Chandratreya A, Giannikas K, Livesley P. To drain or not drain: literature versus practice. J R Coll Surg Edinb. 1998;43(6):e404–6. [PubMed] [Google Scholar]
- 4.Demirkale I, Tecimel O, Sesen H, Kilicarslan K, Altay M, Dogan M. Nondrainage decreases blood transfusion need and infection rate in bilateral total knee arthroplasty. J Arthroplasty. 2014;29(5):e993–7. doi: 10.1016/j.arth.2013.10.022. [DOI] [PubMed] [Google Scholar]
- 5.Matziolis G, Roehner E, Windis C, Wagner A. The volume of the human knee joint. Arch Orthop Trauma Surg. 2015;135(10):1401–3. doi: 10.1007/s00402-015-2272-0. [DOI] [PubMed] [Google Scholar]
- 6.Yamada K, Imaizumi T, Uemura M, Takada N, Kim Y. Comparison between 1-hour and 24-hour drain clamping using diluted epinephrine solution after total knee arthroplasty. J Arthroplasty. 2001;16(4):458–62. doi: 10.1054/arth.2001.23620. [DOI] [PubMed] [Google Scholar]
- 7.Larsson J, Lewis DH, Liljedahl SO, Löfström JB. Early biochemical and hemodynamic changes after operation in a bloodless field. Eur Surg Res. 1977;9(5):311–20. doi: 10.1159/000127950. [DOI] [PubMed] [Google Scholar]
- 8.Yang JH, Yoon JR, Dahuja A, Song S. Subcutaneous versus intraarticular closed suction indwelling drainage after total knee arthroplasty: a randomised control trial. Indian J Orthop. 2016;50(1):59–64. doi: 10.4103/0019-5413.173515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drosos GI, Ververidis A, Valkanis C, Tripsianis G, Stavroulakis E, Vogiatzaki T, et al. A randomized comparative study of topical versus intravenous tranexamic acid administration in enhanced recovery after surgery (ERAS) total knee replacement. J Orthop. 2016;13(3):127–31. doi: 10.1016/j.jor.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keyhani S, Esmailiejah AA, Abbasian MR, Safdari F. Which route of tranexamic acid administration is more effective to reduce blood loss following total knee arthroplasty? Arch Bone Jt Surg. 2016;4(1):65–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Goyal N, Kaul R, Harris IA, Chen DB, MacDessi SJ. Is there a need for routine post-operative hemoglobin level estimation in total knee arthroplasty with tranexamic acid use? Knee. 2016;23(2):310–3. doi: 10.1016/j.knee.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 12.Ho D, Jagdeo J, Waldorf HA. is there a role for arnica and bromelain in prevention of post-procedure ecchymosis or edema? A systematic review of the literature. Dermatol Surg. 2016;42(4):445–63. doi: 10.1097/DSS.0000000000000701. [DOI] [PubMed] [Google Scholar]
- 13.Kluger MT, Lewis G, Rice D, McNair P. Psychological rather than pharmacological interventions for effective prevetion of pain after knee joint replacement? Br J Anaesth. 2016;116(1):e150. doi: 10.1093/bja/aev431. [DOI] [PubMed] [Google Scholar]
- 14.Short Form-McGill Pain Questionnaire-2 (SF-MPQ-2) A Cross-Cultural Adaptation and Validation Study of the Persian Version in Patients with Knee Osteoarthritis. Arch Bone Jt Surg. 2015;3(1):45–50. [PMC free article] [PubMed] [Google Scholar]
- 15.Si HB, Yang TM, Zeng Y, Shen B. No clear benefit or drawback to the use of closed drainage after primary total knee arthroplasty: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2016;17(1):183–91. doi: 10.1186/s12891-016-1039-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abolghasemian M, Huether TW, Soever LJ, Drexler M, MacDonald MP, Backstein DJ. The use of a closed-suction drain in revision knee arthroplasty may not be necessary: a prospective randomized study. J Arthroplasty. 2016;31(7):1544–8. doi: 10.1016/j.arth.2015.08.041. [DOI] [PubMed] [Google Scholar]
- 17.Yang JH, Yoon JR, Dahuja A, Song S. Subcutaneous versus intraarticular closed suction indwelling drainage after total knee arthroplasty: a randomised control trial. Indian J Orthop. 2016;50(1):59–64. doi: 10.4103/0019-5413.173515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee QJ, Mak WP, Hau WS, Yeung ST, Wong YC, Wai YL. Short duration and low suction pressure drain versus no drain following total knee replacement. J Orthop Surg (Hong Kong) 2015;23(3):278–81. doi: 10.1177/230949901502300302. [DOI] [PubMed] [Google Scholar]
- 19.Watanabe T, Muneta T, Yagishita K, Hara K, Koga H, Sekiya I. Closed Suction drainage is not necessary for total knee arthroplasty: a prospective study on simultaneous bilateral surgeries of a mean follow-up of 5.5 years. J Arthroplasty. 2016;31(3):641–5. doi: 10.1016/j.arth.2015.10.005. [DOI] [PubMed] [Google Scholar]


