Abstract
Background and purpose
Active smokers with myocardial infarction were shown to have enhanced benefit with clopidogrel compared with aspirin. Whether this “paradox” exists in ischemic stroke patients is unknown. We aimed to investigate whether smoking status has a differential impact on the efficacy of clopidogrel vs. aspirin in patients with non-cardioembolic strokes.
Methods
This single-center study retrospectively assessed 1792 non-cardioembolic ischemic stroke patients discharged from January 2013 to October 2014, and followed for 12 months. Patients were categorized as current-smokers and never-smokers. Primary outcome was a composite of secondary ischemic stroke, myocardial infarction and all-cause death. Secondary outcome was secondary ischemic stroke.
Results
1066 patients were current-smokers and 726 were never-smokers. Compared with never-smokers, current-smokers had significantly higher rates of ischemic stroke (4.3% vs. 1.2%; adjusted OR: 3.60, 95%CI: 1.50–8.64, p = 0.004). Regarding the primary outcome, among smokers, rates showed a lower trend in clopidogrel vs. aspirin groups (3.7% vs. 6.4%; adjusted OR 0.57, 95%CI: 0.31–1.07, p = 0.08), but no difference among never-smokers (2.1% vs. 1.0%; adjusted OR: 1.67, 95%CI: 0.47–5.89, p = 0.42). Similarly, among smokers, trending lower rates for recurrent ischemic stroke were observed in clopidogrel vs. aspirin group (3.1% vs. 5.0%; adjusted OR: 0.60, 95%CI: 0.31–1.18, p = 0.14); but no difference between the two groups among never-smokers (1.7% vs. 1.0%; adjusted OR 1.36, 95%CI: 0.36–5.52, p = 0.65).
Conclusions
Smoking is a major risk factor for recurrent stroke in our retrospective non-cardioembolic ischemic stroke cohort. Active-smokers trend toward better cardiovascular outcomes when on clopidogrel. This finding needs to be confirmed in a prospective cohort.
Keywords: Smoking, Clopidogrel, Aspirin, Outcome, Ischemic stroke
1. Introduction
The interaction between cigarette smoking and cardiovascular outcomes is complex [1]. On one hand, cigarette smoking influences the inception and progression of atherosclerosis [2] and poses hazards to cardiovascular and cerebrovascular systems which can trigger thrombotic complications including myocardial infarction (MI), ischemic stroke (IS), and cardiovascular death [3]. However, several recent studies observed reduced recurrence of cardiovascular events and an improved survival in smokers with antithrombotic therapy after an index cardiovascular event, a phenomenon called “smoker’s paradox” [4,5]. This observation has been postulated to be due to cytochrome P450 (CYP) 1A2 and B6 induction by cigarette smoking leading to increased clopidogrel active metabolite and enhanced platelet inhibition [6].
While a smoker-clopidogrel paradox has been observed among cardiovascular patients, little is known about whether this paradox exists in ischemic stroke patients. The objective of this study was to assess whether smoking status has a differential clinical impact on the efficacy of clopidogrel vs. aspirin among recent ischemic stroke patients.
2. Methods
2.1. Subjects
We retrospectively reviewed the prospectively maintained stroke registry of a single medical center (Xuanwu Hospital) comprising 1910 non-cardiogenic ischemic stroke patients consecutively discharged from between January 2013 to October 2014, who were prescribed clopidogrel (75 mg/day) or aspirin (100 mg/day) after their index events. In the local protocol, subjects were not prescribed either of these agents if they met any of the following criteria: known allergy or intolerance to aspirin or clopidogrel; active bleeding or bleeding tendency; any bleeding within last 6 months; dyscrasia and malignancy, simultaneous use of other antithrombotic drugs (oral anticoagulants, dipyridamole, ticlopidine, or cilostazol), platelet count <100 × 106/L during admission, liver disease with baseline hepatic enzymes >2.5 times the upper limit of normal during admission. The study was approved by the local institutional review board.
Patients were categorized as current smokers, former smokers and never-smokers according to their smoking status which was ascertained and recorded on the medical records at hospital admission for the indexed event. Current smokers were defined as persons smoking at least 1 cigarette per day during the month before hospital admission. Never-smokers were defined as those who had never smoked [7]. As the former smoker is not easy to defined and its impact on cardiovascular events is not well defined, the study excluded 118 patients who had smoked previously and stopped >1 month before the stroke hospitalization. As a result, there were two groups for the purpose of this analysis: current smokers vs. never-smokers.
2.2. Clinical outcomes assessment
All participants had standard assessments of demographic characteristics, medical history and clinical outcomes per local clinical stroke protocol. Per protocol, stroke patients were evaluated at the time of admission, and were continuously assessed every month until 12 months post-stroke. Primary outcome was a composite of secondary IS, MI and all-cause death. The secondary outcome was secondary IS alone. In addition, we compared safety profiles of clopidogrel vs. aspirin on the cumulative bleeding events (major or minor, including mucocutaneous hemorrhage, gastrointestinal bleeding, and intracranial hemorrhage, et al.) during the 12-month period according to smoking status.
2.3. Statistical analysis
We performed two-tailed t-tests for continuous variables and chi-squared tests for categorical variables. A Mann-Whitney U test was performed for the variables that were not normally distributed. Odds ratios (OR) and 95% confidence intervals (95% CI) were calculated and stratified by the smoking status. Adjusted OR and 95% CI were calculated using a logistic regression model. We adjusted age, sex, hypertension, diabetes, hyperlipidemia and prior coronary heart disease. p value <0.05 was considered as statistical significance. Statistical analyses were conducted with SPSS statistical software, version 22.0 (Chicago, IL, USA).
3. Results
3.1. Study population
A total of 1792 patients were included in this study, of which 1066 (59.5%) were classified as “current smokers” and 726 (40.5%) as “never smokers”. The baseline characteristics and clinical outcomes of the patients were reported by smoking status in Table 1. Compared with never smokers, current smokers were relatively younger, more frequently male, more likely to have a history of hyperlipidemia. Current smokers had significantly higher rates of secondary IS [46 (4.3%) vs. 9 (1.2%), p = 0.000], MI [10 (0.9%) vs. 1 (0.1%), p = 0.034] and bleeding events [21 (2.0%) vs. 3 (0.4%), p = 0.005] than never-smokers. In both unadjusted and adjusted model, current smokers had an increased risk of secondary IS compared with never smokers at statistically significant level [3.59 (1.75–7.39) vs. 3.60 (1.50–8.64)]. Table 2 shows both unadjusted and adjusted ORs for other clinical outcomes according to the smoking status.
Table 1.
Baseline demographics and clinical outcomes by smoking status.
| Current smokers (n = 1066) |
Never-smokers (n = 726) |
p-Value | |
|---|---|---|---|
| Demographics | |||
| Age (yr, mean ± SD) | 58.68 ± 11.60 | 62.78 ± 13.56 | 0.000 |
| Male (%) | 95.4 | 43.8 | 0.000 |
| Clinical History (n, %) | |||
| Hypertension | 682 (64.0) | 494 (68.0) | 0.075 |
| Diabetes | 304 (28.5) | 227 (31.3) | 0.211 |
| Hyperlipidemia | 469 (44.0) | 264 (36.4) | 0.001 |
| Prior coronary heart disease | 132 (12.4) | 104 (14.3) | 0.233 |
| Medication (n, %) | 0.210 | ||
| Aspirin | 683 (64.1) | 486 (66.9) | |
| Clopidogrel | 383 (35.9) | 240 (33.1) | |
| Primary outcome (n, %) | |||
| Secondary ischemic stroke | 46 (4.3) | 9 (1.2) | 0.000 |
| Myocardial infarction | 10 (0.9) | 1 (0.1) | 0.034 |
| All-cause death | 2 (0.2) | 0 | 0.518 |
| All primary events | 58 (5.4) | 10 (1.4) | 0.000 |
| Safety endpoint (n, %) | |||
| Bleeding events | 21 (2.0) | 3 (0.4) | 0.005 |
Table 2.
Association of smoking status with end points.
| Current smokers (n = 1066) | Never-smokers (n = 726) | Unadjusted OR (95% CI) | p-Value | Adjusted ORa(95% CI) | p-Value | |
|---|---|---|---|---|---|---|
| Secondary ischemic stroke (n, %) | 46 (4.3) | 9 (1.2) | 3.59 (1.75–7.39) | 0.001 | 3.60 (1.50–8.64) | 0.004 |
| Myocardial infarction (n, %) | 10 (0.9) | 1 (0.1) | 6.87 (0.88–53.75) | 0.067 | 6.15 (0.56–67.53) | 0.137 |
| All-cause death (n, %) | 2 (0.2) | 0 | 1,102,288,300 (0.000–) | 0.999 | 369,399,332 (0.000–) | 0.999 |
| All primary events (n, %) | 58 (5.4) | 10 (1.4) | 3.90 (1.97–7.69) | 0.000 | 3.84 (1.68–8.78) | 0.001 |
| Bleeding events (n, %) | 21 (2.0) | 3 (0.4) | 4.84 (1.44–16.30) | 0.011 | 3.78 (0.90–15.97) | 0.070 |
Adjusted factors: age, sex, hypertension, diabetes, hyperlipidemia and prior coronary heart disease.
3.2. Impact of smoking status on outcomes: clopidogrel vs. aspirin
Of the current smokers, 683 patients were treated with aspirin and 383 patients were treated with clopidogrel. In never-smokers, 486 subjects were prescribed with aspirin and 240 subjects with clopidogrel. In the never-smokers, aspirin-treated patients were younger, less frequently to have a history of hypertension compared with clopidogrel-treated patients. Table 3 shows the baseline characteristics and clinical outcomes of patients according to clopidogrel or aspirin treatment stratified by the smoking status. Regarding the primary outcome, for smokers, rates were numerically lower in clopidogrel vs. aspirin groups [14 (3.7%) vs. 44 (6.4%); adjusted OR 0.57, 95% CI: 0.31–1.07, p = 0.080], but more congruent among never-smokers [5 (2.1%) vs. 5 (1.0%); adjusted OR 1.67, 95% CI: 0.47–5.89, p = 0.424]. Similarly, for the outcome of secondary IS alone, among smokers, relatively lower rates were observed in the clopidogrel vs. aspirin group [12 (3.1%) vs. 34 (5.0%); adjusted OR 0.60, 95% CI: 0.31–1.18, p = 0.138]; but a less pronounced difference between clopidogrel vs. aspirin was observed among never-smokers [4 (1.7%) vs. 5 (1.0%); adjusted OR 1.36, 95% CI: 0.36–5.52, p = 0.651]. The rates of bleeding events were similar in the clopidogrel vs. aspirin group among both current smokers [9 (2.3%) vs. 12 (1.8%); adjusted OR 0.94, 95% CI: 0.08–10.48, p = 0.959] and never-smokers [1 (0.4%) vs. 2 (0.4%); adjusted OR 1.73 95% CI: 0.55–3.19, p = 0.526] (Fig. 1).
Table 3.
Baseline demographics and clinical outcomes by smoking status and antiplatelet group.
| Currentsmokers (n = 1066)
|
p-Value | Never-smokers (n = 726)
|
p-Value | |||
|---|---|---|---|---|---|---|
| Clopidogrel (n = 383) | Aspirin (n = 683) | Clopidogrel (n = 240) | Aspirin (n = 486) | |||
| Demographics | ||||||
| Age (yr, mean ± SD) | 58.27 ± 11.65 | 59.40 ± 11.49 | 0.128 | 64.96 ± 12.73 | 61.71 ± 13.84 | 0.002 |
| Male (%) | 367 (95.8) | 650 (95.2) | 0.625 | 98 (40.8) | 220 (45.3) | 0.257 |
| Clinical History (n, %) | ||||||
| Hypertension | 248 (64.8) | 434 (63.5) | 0.693 | 181 (75.4) | 313 (64.4) | 0.003 |
| Diabetes | 123 (32.1) | 181 (26.5) | 0.051 | 83 (35.0) | 143(29.4) | 0.127 |
| Hyperlipidemia | 176 (46.0) | 293 (42.9) | 0.335 | 92(38.3) | 172 (35.4) | 0.438 |
| Prior coronary heart disease | 49 (12.8) | 83 (12.2) | 0.760 | 40 (16.7) | 64 (13.2) | 0.206 |
| Primary outcome (n, %) | ||||||
| Secondary ischemic stroke | 12 (3.1) | 34 (5.0) | 0.155 | 4 (1.7) | 5 (1.0) | 0.488 |
| Myocardial infarction | 2 (0.5) | 8 (1.2) | 0.292 | 1 (0.4) | 0 | 0.331 |
| All-cause death | 0 | 2 (0.3) | 0.289 | 0 | 0 | n/a |
| All primary events | 14 (3.7) | 44 (6.4) | 0.096 | 5 (2.1) | 5 (1.0) | 0.312 |
| Safety endpoint (n, %) | ||||||
| Bleeding events | 9 (2.3) | 12 (1.8) | 0.504 | 1 (0.4) | 2 (0.4) | 1.000 |
Fig. 1.
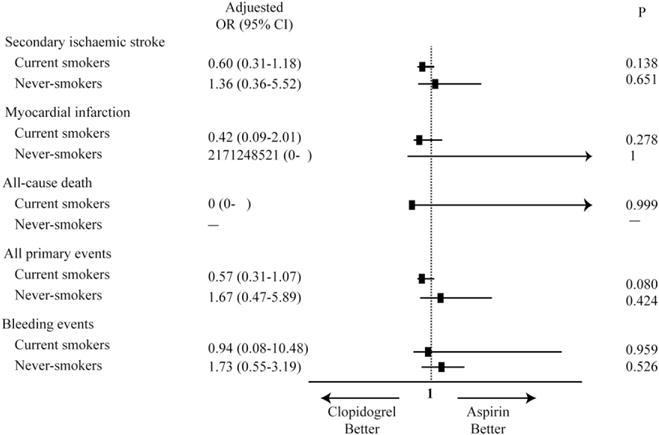
Forest plot of efficacy and bleeding outcomes. Adjusted primary and secondary efficacy and bleeding outcomes in relation to smoking status and treatment allocation.
4. Discussion
The primary findings in this study are as follows: 1) Of patients with non-cardioembolic ischemic strokes, current smokers experienced an increase in the primary composite clinical outcome of secondary IS, MI, and all-cause death in 12 months after indexed event, compared with never-smokers; 2) Of smokers, There is a trend of lower composite vascular events in clopidogrel-treated patients as compared with the aspirin-treated patients, whereas no such trend was observed in never-smokers; 3) No significant difference was observed between antiplatelet agents and smoking status for bleeding events.
Cigarette smoking is a strong independent risk factor for all-cause mortality and recurrent ischemic events [2], therefore, smoking cessation is a recommended treatment with strong evidence for secondary prevention of atherosclerotic vascular disease [8].
Clopidogrel may pose better protective effect and may be better substitute for aspirin in smokers for secondary stroke prevention. The Clopidogrel vs. Aspirin in Patients at Risk of Ischemic Events (CAPRIE) trial showed that clopidogrel is superior to aspirin in lowering ischemic events with a favorable safety profile in patients with atherosclerotic disease [9]. In a post-hoc analysis of CAPRIE, it was shown that clopidogrel was more effective than aspirin with a decreased incidence of ischemic outcomes in current smokers (8.3% vs. 10.8%; HR 0.76, 95% CI 0.64–0.90), whereas no superiority of clopidogrel over aspirin was observed in nonsmokers (10.4% vs. 10.6%; HR 0.99, 95% CI 0.89–1.10) [10]. Our study is different, of which we specifically assessed our hypothesis in IS patients with etiology of non-cardioembolism in a retrospective hospital discharge cohort with Chinese stroke survivors (vs. multi-national population in CAPRIE). With large sample size, they were able to classified patient into 3 groups (current-smoker, never-smoker, ex-smoker) while we were only able to included current-smoker and never-smoker. Regardless, both study showed similar data, however, the results should be considered as hypothesis generating, not as definitive conclusions on this topic. In a meta-analysis, Zhao et al. showed that clopidogrel was linked with a 10% reduction in ischemic events among non-current smokers (HR 0.90; 95% CI 0.85 to 0.96), while this clinical benefit was boosted by 2.9-fold in current smokers (HR 0.71; 95% CI 0.62 to 0.80) [11], suggesting that this add-on benefit of clopidogrel occurred mainly in smokers, and a differential risk-benefit evaluation should be considered according to the smoking status [12]. Previous data mainly focused on patients with a myocardial infarction and showed that active smokers have enhanced benefit with clopidogrel therapy compared with aspirin. However, little is known whether this ‘paradox’ exists in non-cardioembolic IS patients. In the present study, we recruited non-cardioembolic IS patients to assess the relationship between use of antiplatelet drugs and prognosis (IS, MI, and all-cause death), and we found a lower trend for secondary IS and overall ischemic events in clopidogrel vs. aspirin groups among current smokers.
The key mechanism underlying the smoker’s paradox has been postulated to be a greater pharmacodynamic (PD) effect of clopidogrel in smokers [13]. Clopidogrel is an inactive prodrug that requires to be metabolized into a bioactive form via the cytochrome P450 enzyme system in the liver. Cigarette smoking is an inducer of CYP1A2, which can upregulate the CYP1A2 activity, thereby may increase the conversion of clopidogrel into its active metabolite [14] leading to more potent efficacy. Compared with nonsmokers, clopidogrel therapy in current smokers is correlated with strengthened platelet inhibition, decreased aggregation and less occurrence of clopidogrel resistance [15,16]. Moreover, the increased inhibition of platelet aggregation by clopidogrel in smokers diminished after smoking cessation [17], indicating the clopidogrel responsiveness may be enhanced by smoking.
This is a study to evaluate the impact of smoking status on clopidogrel therapy in Chinese population with non-cardioembolic ischemic stroke. A trend toward a lower risk of ischemic events among clopidogrel-treated subjects was found in our study, indicating smokers with non-cardioembolic ischemic stroke may have additional benefit from clopidogrel therapy. Smoking is a major healthcare threat in China, and only 32.5% of patients after heart attack [18] and 21.0% of patients after stroke [19] quitted smoking. Our study result may have an important healthcare implication.
Our study has several limitations. First, this study is a retrospective cohort study in nature which may introduce bias as we only extracted data from the patients who returned for follow-up visits. Secondly, we were only able to extract and control the traditional cardiovascular risk factors, which may not be adequate. Steady-state clopidogrel pharmacokinetic (PK) and PD differ widely due to various factors including polymorphisms, compliance, concomitant medications, life-style factors, demographic factors, and pre-treatment platelet hyper-reactivity [20]. Platelet reactivity was not a routine test and was not available in our cohort. Thirdly, sample size may not be adequate and the follow-up period is only 12 months. Expanding the sample size and extending the time of follow-up to allow more events would increase the power to detect difference in outcomes. Lastly, the smoking status was determined only at hospital admission which may change during the study period as smoking cessation is part of stroke prevention regimen. Misclassification of the smoking status would likely have reduced the strength of the association between smoking status and clinical outcomes [10].
5. Conclusions
In this hospital discharge cohort, smoking, not surprisingly, is a major risk factor for recurrent stroke. We also observed a trend of “smoker’s paradox” in ischemic stroke patients with etiology of non-cardioembolism - cardiovascular events were lower, but not at statistical significance level, in current-smokers who were taking clopidogrel. This finding needs to be confirmed in a dedicated prospective cohort study as it may have an important clinical implication for secondary stroke prevention.
Acknowledgments
Dr. Wuwei Feng acknowledges grant support from American Heart Association (14SDG1829003) and National Institute of Health (P20 GM109040 and UL1RR029882). Dr. Bruce Ovbiagele acknowledges grant support from National Institute of Health (NS079179 and NS094033). Dr. Xunming Ji acknowledges grant support from Chinese 12th Five Science and Technology Support Program (2013BAI07B01).
Footnotes
Disclosure of conflicts of interest
None of the authors has any conflict of interest to disclose.
References
- 1.Gurbel PA, Baker BA, Bailey WL, Bliden KP, Tantry US. Unravelling the smokers’ paradox: cigarette smoking, high-risk coronary artery disease and enhanced clinical efficacy of oral P2Y(1)(2) inhibitors. Thromb Haemost. 2014;111:1187–1190. doi: 10.1160/TH13-08-0642. [DOI] [PubMed] [Google Scholar]
- 2.Rollini F, Franchi F, Cho JR, et al. Cigarette smoking and antiplatelet effects of aspirin monotherapy versus clopidogrel monotherapy in patients with atherosclerotic disease: results of a prospective pharmacodynamic study. J Cardiovasc Transl Res. 2014;7:53–63. doi: 10.1007/s12265-013-9535-3. [DOI] [PubMed] [Google Scholar]
- 3.How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-attributable Disease: A Report of the Surgeon General. Atlanta GA: 2010. [PubMed] [Google Scholar]
- 4.Berger JS, Bhatt DL, Steinhubl SR, et al. Smoking, clopidogrel, and mortality in patients with established cardiovascular disease. Circulation. 2009;120:2337–2344. doi: 10.1161/CIRCULATIONAHA.109.866533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desai NR, Mega JL, Jiang S, Cannon CP, Sabatine MS. Interaction between cigarette smoking and clinical benefit of clopidogrel. J Am Coll Cardiol. 2009;53:1273–1278. doi: 10.1016/j.jacc.2008.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yousef AM, Arafat T, Bulatova NR, Al-Zumyli R. Smoking behaviour modulates pharmacokinetics of orally administered clopidogrel. J Clin Pharm Ther. 2008;33:439–449. doi: 10.1111/j.1365-2710.2008.00936.x. [DOI] [PubMed] [Google Scholar]
- 7.Ryan H, Trosclair A, Gfroerer J. Adult current smoking: differences in definitions and prevalence estimates—NHIS and NSDUH, 2008. J Environ Public Health. 2012;2012:918368. doi: 10.1155/2012/918368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith SC, Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58:2432–2446. doi: 10.1016/j.jacc.2011.10.824. [DOI] [PubMed] [Google Scholar]
- 9.A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischemic events (CAPRIE). CAPRIE Steering Committee. Lancet. 1996;348:1329–1339. doi: 10.1016/s0140-6736(96)09457-3. [DOI] [PubMed] [Google Scholar]
- 10.Ferreiro JL, Bhatt DL, Ueno M, Bauer D, Angiolillo DJ. Impact of smoking on long-term outcomes in patients with atherosclerotic vascular disease treated with aspirin or clopidogrel: insights from the CAPRIE trial (clopidogrel versus aspirin in patients at risk of ischemic events) J Am Coll Cardiol. 2014;63:769–777. doi: 10.1016/j.jacc.2013.10.043. [DOI] [PubMed] [Google Scholar]
- 11.Zhao ZG, Chen M, Peng Y, et al. The impact of smoking on clinical efficacy and pharmacodynamic effects of clopidogrel: a systematic review and meta-analysis. Heart. 2014;100:192–199. doi: 10.1136/heartjnl-2013-304138. [DOI] [PubMed] [Google Scholar]
- 12.Gagne JJ, Bykov K, Choudhry NK, Toomey TJ, Connolly JG, Avorn J. Effect of smoking on comparative efficacy of antiplatelet agents: systematic review, meta-analysis, and indirect comparison. BMJ. 2013;347:f5307. doi: 10.1136/bmj.f5307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gurbel PA, Bliden KP, Logan DK, et al. The influence of smoking status on the pharmacokinetics and pharmacodynamics of clopidogrel and prasugrel: the PARADOX study. J Am Coll Cardiol. 2013;62:505–512. doi: 10.1016/j.jacc.2013.03.037. [DOI] [PubMed] [Google Scholar]
- 14.Zevin S, Benowitz NL. Drug interactions with tobacco smoking. An update. Clin Pharmacokinet. 1999;36:425–438. doi: 10.2165/00003088-199936060-00004. [DOI] [PubMed] [Google Scholar]
- 15.Bliden KP, Dichiara J, Lawal L, et al. The association of cigarette smoking with enhanced platelet inhibition by clopidogrel. J Am Coll Cardiol. 2008;52:531–533. doi: 10.1016/j.jacc.2008.04.045. [DOI] [PubMed] [Google Scholar]
- 16.Maruyama H, Fukuoka T, Deguchi I, et al. Relationship between smoking and responsiveness to clopidogrel in non-cardiogenic ischemic stroke patients, Intern. Med. 2014;53:2575–2579. doi: 10.2169/internalmedicine.53.2918. [DOI] [PubMed] [Google Scholar]
- 17.Park KW, Kang SH, Kang J, et al. Enhanced clopidogrel response in smokers is reversed after discontinuation as assessed by VerifyNow assay: additional evidence for the concept of ‘smokers’ paradox. Heart. 2012;98:1000–1006. doi: 10.1136/heartjnl-2011-301565. [DOI] [PubMed] [Google Scholar]
- 18.Jing W, Mingzi L. Questionnaires on the willing and behavior of smoking cessation of the patients with coronary disease. Chin J Med Nure. 2010;16:262–264. Chinese. [Google Scholar]
- 19.Yueqing L, Yuehao H, Xiaoling W, Yinan L. Stop smoking health education supplemented with behavior therapy for stroke patients quit smoking behavior. Guide of China Medicine. 2008;6:20–21. Chinese. [Google Scholar]
- 20.Frelinger AL, 3rd, Bhatt DL, Lee RD, et al. Clopidogrel pharmacokinetics and pharmacodynamics vary widely despite exclusion or control of polymorphisms (CYP2C19, ABCB1, PON1), noncompliance, diet, smoking, co-medications (including proton pump inhibitors), and pre-existent variability in platelet function. J Am Coll Cardiol. 2013;61:872–879. doi: 10.1016/j.jacc.2012.11.040. [DOI] [PubMed] [Google Scholar]


