Abstract
This study investigated whether intact young Black MSM differed from their circumcised counterparts regarding condom use behaviors and perceptions and HIV/Chlamydia/gonorrhea. Young Black MSM completed a self-interview, including a pictorial item assessing circumcision status and measures of condom use. Twenty-seven percent of 388 participants reported not being circumcised. With one exception, no associations tested approached significance. The mean frequency of unprotected insertive anal sex for circumcised men was about twice as high compared to those intact (P = .04). Intact young Black MSM did not differ from circumcised men relative to prevalence of STIs (including HIV) or condom use behaviors as reported only by insertive partners.
Keywords: Circumcision, Condoms, STIs
Introduction
Representing only an estimated 2 % of the U.S. population, men who have sex with men (MSM) are disproportionately affected by the HIV/AIDS epidemic [1]. In 2011, among adult and adolescent males, 78 % of all new HIV infections were attributed to male-to-male sexual contact [2].
Evidence suggests that approximately 79 % of U.S. males are circumcised [3]. Although the protective value of circumcision against HIV acquisition for men having sex with women is well established [4], whether protection is conferred for men having sex with men is not known. Biological evidence suggests that the penile foreskin is rich in CD4? target cells thereby creating a convenient “target” for the attachment of free virus during sex as an insertive partner [5]. A recent review examining the sexual risk behavior of Black MSM concluded that evidence was insufficient to support the effectiveness of circumcision to prevent HIV acquisition among Black MSM [4]. Similar reviews of study participants identifying as MSM and homosexual have not found evidence supporting a protective role of circumcision [6, 7]. One study, however, did find a significant protective effect of circumcision for the insertive partner having anal sex with males [8].
There have been no investigations examining whether intact MSM, as compared to circumcised MSM, experience different types or frequencies of condom use errors and problems. A previous study described the prevalence of condom use issues, errors, and problems among MSM [9], but studies have not investigated whether these issues differ by circumcision status. The presence of foreskin may indeed interfere with the application of condoms. Thus, it is conceivable that intact MSM may report relatively more errors and problems (e.g., late application, breakage, slippage) with condom use compared to their circumcised counterparts. As a consequence it is also possible that intact MSM may use condoms less frequently than their circumcised counterparts. Further, it is possible that intact MSM may experience more interference with arousal and pleasure in comparison to circumcised men [10]. Finally, based on the premise of smegma collection under the foreskin, it is also possible that intact MSM may be more likely to have urethral infections and because the foreskin is rich in CD4? cells, it is possible that intact MSM may be more likely to be HIV-positive. Accordingly, the purpose of this study was twofold: (1) to examine associations between circumcision status and men’s condom use/sexual behaviors and perceptions, and (2) to examine associations between circumcision status and the prevalence of urethral Chlamydia, urethral gonorrhea, and HIV infection.
The population for this study was selected based on epidemiological priority. Young Black MSM were sampled for this study because they are the single most at-risk population for HIV acquisition in the U.S. Between 2008 and 2011, young Black MSM experienced the largest increase in HIV infections, representing 58 % of all new HIV cases among young MSM [11].
Methods
Study Sample
A convenience sample of 400 young, Black men who have sex with men (YBMSM) was recruited for participation from a larger NIH-funded randomized controlled trial of a safer sex intervention program. Only baseline data (collected before randomization and intervention) was used for the present study. Recruitment occurred in a federally supported clinic designated specifically for the diagnosis and treatment of HIV and other sexually transmitted infections. The clinic was located in a mid-size southern city experiencing extremely high incidence rates of HIV. Inclusion criteria were: (1) self-identification as Black/African American; (2) aged 15–29 years; (3) attending the clinic to be tested for HIV or other STIs, (4) engaging in penile-anal sex, as an insertive partner with a male, at least once in the past 6 months, and (5) the ability to speak and comprehend English.
Age-eligible Black males were approached in clinic waiting areas and asked about their interest in volunteering for an HIV prevention study. Those expressing interest were screened for eligibility. After being offered the opportunity to enroll, 85 YBMSM declined, yielding a participation rate of 82.5 %. All study procedures were approved by the Institutional Review Board at the University of Mississippi Medical Center and the Office of Research Integrity at the University of Kentucky.
Study Procedures
After providing written informed consent (or parental consent for those under 18 years of age) men completed an online questionnaire, using Qualtrics software, in a private office not physically connected to the clinic. A key item in this Qualtrics interview presented two photographs (an intact and a circumcised penis, see Fig. 1) to men and asked them to indicate if they were circumcised. The questionnaire also collected information related to men’s sexual risk behaviors and their condom use behaviors. Subsequently, they were evaluated for Chlamydia and gonorrhea in three anatomic locations; urethral and rectal infections were detected through nucleic acid amplification testing (NAAT) performed on a rectal swab; oral infections were detected through NAAT testing of a bucosal swab. For those not already HIV-positive according to clinic records, a blood sample was collected to test for HIV using OraSure.
Fig. 1.
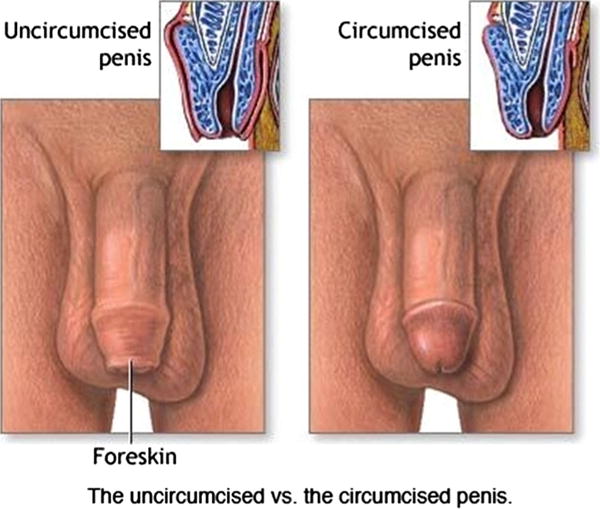
The uncircumcised versus the circumcised penis
Assessment
Twenty outcome measures were assessed. The majority were items adapted from the Condom Use Errors Survey [11]. Other measures included items assessing men’s perceptions of condoms distracting from sexual pleasure, whether condoms did not fit right (length and width were assessed separately), and a scale measuring men’s sexual pleasure when using condoms. The scale was comprised of five items: (1) Condoms help me intensify orgasm, (2) Condoms help me feel better about having sex after it ends, (3) Condoms help me have better sex, (4) Condoms help me let go of my fears, and (5) Condoms help me enjoy sex. Response options were provided on a 5-point scale, with higher scores representing greater agreement. The scale produced a Cronbach’s alpha of .84. Also, an item assessed whether any condomless sex as an insertive partner had occurred in the past 90 days.
In addition, the laboratory results for urethral Chlamydia and urethral gonorrhea were used as outcome measures, as was men’s HIV serostatus.
Data Analysis
Due to marked skewness, the scale measure of pleasure from condom use was dichotomized by performing a median split. Bivariate associations between circumcision status and the selected outcomes assessed dichotomously were tested using χ2 analyses. Two potentially confounding measures (confidence in using condoms and education level) were tested for possible association with circumcision status.
Results
Average age was 22.58 (SD = 3.13). Men’s average monthly income ranged from less than $500 per month (19.6 %), to $500–$1000 per month (28.0 %), to $1001–$1500 (20.6 %), to $1501–$2000 (15.0 %), to greater than $2000 (16.8 %). More than one-half (58.8 %) reported having education beyond high school graduation and 47.0 % reported current enrollment in a school or college. The mean number of sex partners when enrolled men were the insertive partner in the past 90 days was 2.68 (SD = 7.1). More than one-third (37.0 %) tested positive for Chlamydia or gonorrhea and one-quarter (25.6 %) were HIV-positive at study enrollment.
Table 1 displays the findings from the χ2 tests of associations. As shown, none of the associations approached significance. Noteworthy among these null findings is that HIV serostatus was not associated with circumcision status.
Table 1.
Attitudes, experiences and problems related to condom use among circumcised and intact young black men
| Correlates | n/ % Circumcised (n = 279) | n/ % Intact (n = 105) | P |
|---|---|---|---|
| Attitudes | |||
| Condoms don’t feel good | 145/52.0 | 53/50.5 | .79 |
| Condoms rub and make you feel sore | 88/35.1 | 28/26.7 | .35 |
| Condoms feel unnatural | 136/48.7 | 50/47.6 | .84 |
| Experiences and problems | |||
| Started having anal sex then put condom on later | 40/14.3 | 11/10.5 | .32 |
| Took condom off before ejaculation | 58/20.8 | 28/26.7 | .22 |
| Condom slipped off penis during withdraw | 26/9.3 | 10/9.5 | .95 |
| Gave up condom use because it got too frustrating | 27/9.7 | 6/5.7 | .22 |
| Condom did not enhance the pleasure of sex | 137/49.1 | 58/52.5 | .28 |
| Condom was damaged during sex | 17/6.1 | 8/7.6 | .59 |
| Condom broke during sex | 5/183 | 22/21 | .55 |
| Condom slipped off during sex | 33/11.8 | 11/10.5 | .71 |
| Condom leaked during sex | 12/4.3 | 5/4.8 | .84 |
| Condom length was not right | 33/20.41 | 14/22.22 | .76 |
| Condom width was not right | 50/30.91 | 15/23.82 | .29 |
| Condom distracted attention from the pleasure of sex | 47/16.8 | 20/105 | .11 |
| Pleasure from condom use | 124/44.4 | 51/48.6 | .47 |
| Diagnosed with HIV | 76/28.13 | 30/304 | .73 |
| Diagnosed with Chlamydia | 19/7.55 | 5/5.46 | .49 |
| Diagnosed with gonorrhea | 15/5.95 | 4/4.36 | .56 |
n = 162;
n = 163;
270;
100;
n = 253;
n = 93
To determine whether men’s confidence in using condoms may have been a confounding variable, the association between a single-item of confidence using condoms and circumcision was assessed. Most men (70.6 %) were highly confident. This measure did not differ at all by circumcision status. Among those who were cut, 29.7 % were not highly confident and among those who were intact 28.6 % were not highly confident (P = .82). Whether men’s level of education was a confounding factor was also tested and ruled out as a possibility based on lack of association with circumcision status. Among those who were cut 40.4 % had not pursued education beyond high school and among those who were intact 44.8 % had not pursued education beyond high school (P = .43).
Discussion
In this clinic-based sample of young Black MSM residing in a high HIV seroprevalence city of the southern U.S., intact men were no more likely than their circumcised counterparts to experience problems with condom use or to perceive that condoms detracted from sexual pleasure. Further, they were no more likely to test positive for urethral Chlamydia, urethral gonorrhea, or HIV. In this risky sexual environment (overall prevalence of STIs was 37.0 % and more than one of every four men was HIV-positive), the condom related attitudes, experiences, and problems (listed in Table 1) of intact men were apparently not affected by having a foreskin and circumcised men were not protected from infection relative to their intact counterparts. Thus, circumcision may not be an important intervention for this population of MSM.
Of interest, a recent study of heterosexual men found that those who were intact were generally more likely than their circumcised counterparts to use condoms [12]. How intact men have managed to overcome any issues in condom application or use that may be posed by having a foreskin is an important research question for future studies. Relatedly, whether the intact men had learned to wash smegma away from under their foreskins is a possible research question. Apparently, however, in this sample of high-risk YBMSM intact MSM avoided any potential risk associated with having foreskins, rendering adult circumcision an unnecessary medical intervention for STI risk reduction in this group.
Limitations
The use of a convenience sample, recruited for participation in a RCT, limits the generalizability of the study findings. Participation bias may have occurred and this may have over-represented men requiring relatively less time-consuming clinical care. Also noteworthy is that some men may not have known their circumcision status and they may not have made an accurate determination based on the pictures provided to them as part of the assessment—for these unknown number of men a misclassification bias was possible. Additionally, a number of variables that were not assessed in the current study may have differed between intact and circumcised men and may have confounded the study findings. For instance, penis size or shape may have varied between the two groups and that difference may have influenced several of the assessed outcomes. Finally, statistical power issues may have limited the ability to find true differences between cut and intact men.
Conclusion
Study findings add another dimension to the evidence suggesting that adult circumcision may not be an effective strategy for the prevention of HIV acquisition among MSM [6, 7, 14, 15]. Evidence from this study suggests that behavioral differences regarding condom use may not differ between YBMSM who are intact versus circumcised. Further, differences in the prevalence of urethral Chlamydia and urethral gonorrhea may not occur among YBMSM groups.
Acknowledgments
This study was funded by a Grant from the National Institute of Mental Health to the first author, R01MH092226.
References
- 1.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2012. HIV Surveillance Supplemental Report. 2014;19(3) Published November 2014. [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV/AIDS Surveillance, (year end edition) US Department of Health and Human Services; Atlanta, GA: 2012. http://www.cdc.gov/hiv/surveillance/resources/reports/2010report/pdf/2010_HIV_Surveillance_Report_vol_22.pdf#Page=66. [Google Scholar]
- 3.Xu F, Markowitz L, Sternberg M, Aral S. Prevalence of circumcision in men in the United States: data from the National Health and Nutrition Examination Survey (NHANES), 1999–2002. Sex Transm Dis. 2007;34(7):479–84. doi: 10.1097/01.olq.0000253335.41841.04. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan PS, Kilmarx PH, Peterman TA, Taylor AW, Nakashima AK, Kamb ML, et al. Male circumcision for prevention of HIV transmission: what the new data mean for HIV prevention in the United States. PLoS Med. 2007;4(7):e223. doi: 10.1371/journal.pmed.0040223.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lemos MP, Lama JR, Karuma ST, et al. The inner foreskin of healthy males at risk of HIV infection harbors epithelial CD4? CCR5? cells and has features of inflamed epidermal barrier. PLoS One. 2014;30:e108954. doi: 10.1371/journal.pone.0108954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kreiss JK, Hopkins SG. The association between circumcision status and human immunodeficiency virus infection among homosexual men. J Infect Dis. 1993;168(6):1404–8. doi: 10.1093/infdis/168.6.1404. [DOI] [PubMed] [Google Scholar]
- 7.Millett GA, Flores SA, Marks G, Reed JB, Herbst JH. Circumcision status and risk of HIV and sexually transmitted infections among men who have sex with men: a meta-analysis. J Am Med Assoc. 2008;300(14):1674–84. doi: 10.1001/jama.300.14.1674. [DOI] [PubMed] [Google Scholar]
- 8.Wiysonge CS, Kongnyuy EJ, Shey M, et al. Male circumcision for prevention of homosexual acquisition of HIV in men. Cochrane Database Syst Rev. 2011;15(6):CD007496. doi: 10.1002/14651858.CD007496.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Hernández-Romieu AC, Siegler AJ, Sullivan PS, Crosby RA, Rosenberg ES. How often do condoms fail? A cross-sectional study exploring incomplete use of condoms, condom failures and other condom problems among black and white MSM in southern USA. Sex Transm Infect. 2014;90:602–7. doi: 10.1136/sextrans-2014-051581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frisch M, Lindholm M, Grønbæk M. Male circumcision and sexual function in men and women: a survey-based, cross-sectional study in Denmark. Int J Epidemiol. 2011;104:10–29. doi: 10.1093/ije/dyr104. [DOI] [PubMed] [Google Scholar]
- 11.Center for Disease Control and Prevention. Estimated HIV incidence in the United States, 2007-2010. HIV Surveillance Supplemental Report. 2012;17(4) Published December 2012. [Google Scholar]
- 12.Crosby RA, Graham CA, Milhausen RR, Sanders SA, Yarber WL. Condom use errors/problems survey. In: Fisher T, Davis C, Yarber W, Davis S, editors. Handbook of sexuality-related measures. 3rd. New York: Routledge; 2010. [Google Scholar]
- 13.Crosby RA, Charnigo R. A comparison of condom use perceptions and behaviors between circumcised and intact men attending STD clinics in the United States. Int J STD and AIDS. 2013;24:175–8. doi: 10.1177/0956462412472444. [DOI] [PubMed] [Google Scholar]
- 14.Doerner R, McKeown E, Nelson S, Anderson J, Low N, Elford J. Circumcision and HIV infection among men who have sex with men in Britain: the insertive sexual role. Arch Sex Behav. 2013;42(7):1319–26. doi: 10.1007/s10508-012-0061-1. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Fact Sheet: Male Circumcision. http://www.cdc.gov/hiv/pdf/prevention_research_malecircumcision.pdf.


