Abstract
Neurologists should consider the possibility of an inherited metabolic disorder in adults with neurologic symptoms that may or may not mimic those seen in affected children, such as in the case of biotinidase deficiency. Because many of these disorders are treatable, they must be included in the differential diagnosis. Technologies, such as specific biochemical analysis and whole exomic sequencing, can assist the clinician by leading to the appropriate diagnosis and treatment. Whole exomic sequencing can identify known and putative mutations in a patient's genome. The neurologist must “think metabolic” in sorting out complex and difficult cases.
Many physicians consider inherited metabolic diseases to be pediatric disorders, because they usually present with symptoms in childhood. Because pediatricians, pediatric neurologists, or pediatricians who specialize in genetics and metabolism usually see these disorders, adult neurologists often do not include inherited metabolic diseases in their differential diagnoses, except for those disorders that are well-known to occur during adolescence or adulthood. When adults exhibit neurologic features that are indicative of more common disorders, these individuals are usually diagnosed with these disorders and subsequently treated as such. Not until these therapies have failed to improve or resolve the symptoms, often leaving the clinician perplexed, does the clinician turn to considering other rare inherited metabolic or genetic disorders. However, over the last several decades, an increasing number of adults are being diagnosed with inherited metabolic diseases. This increase is due in part because of the technological advances in metabolic diseases and genetics.
The clinician may perform some of the more common metabolic disorder testing procedures, such as organic acids or acylcarnitine analysis, resulting in the correct diagnosis. More recently, even newer technologies, such as whole exomic sequencing (WES), have revealed the true diagnosis and led the neurologist to the definitive diagnosis and appropriate treatment. WES analysis is useful in identifying the underlying molecular basis of a genetic disorder in an affected individual. Alterations in an individual's nucleotide sequences are then compared to reference sequences of normal, control individuals, thereby identifying mutations or variants that could possibly explain the clinical findings in an affected individual. The increasing recognition of inherited metabolic diseases in adults has been the subject of new textbooks.1
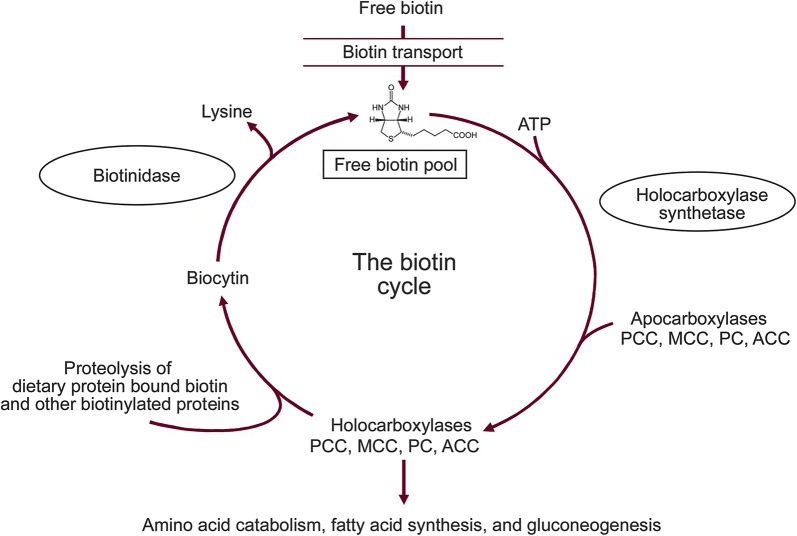
These principles specifically hit home with me in my studies of the autosomal recessively inherited metabolic disorder biotinidase deficiency, which I have been researching for the last 35 years. Biotinidase is the enzyme that is required for recycling the vitamin biotin (figure). Dietary free biotin enters the cellular biotin pool via biotin transport. Once biotin is in the cell, holocarboxylase synthetase attaches biotin to inactive apocarboxylases (propionyl-CoA carboxylase, β-methylcrotonyl-CoA carboxylase, pyruvate carboxylase, and acetyl-CoA carboxylase), forming active holocarboxylases. The holocarboxylases subsequently participate in amino acid catabolism, fatty acid synthesis, and gluconeogenesis. Biotinidase releases biotin from biocytin or proteolytically degraded holocarboxylases and biotin-bound dietary peptides. The released biotin is recycled and enters the free biotin pool.
Figure. Biotin–biotinidase cycle.
ACC = acetyl-CoA carboxylase; ATP = adenosine 5′-triphosphate; MCC = β-methylcrotonyl-CoA carboxylase; PC = pyruvate carboxylase; PCC = propionyl-CoA carboxylase.
Biotinidase deficiency is the primary enzyme defect in most individuals with late-onset multiple carboxylase deficiency.2,3 An individual with biotinidase deficiency cannot recycle his or her endogenous biotin. The resultant secondary biotin deficiency results in an inability to biotinylate the various apocarboxylases, causing deficiencies of the various holocarboxylases. The multiple carboxylase deficiencies result in the accumulation of toxic metabolites resulting in the clinical symptoms. Supplementation with pharmacologic doses of exogenous biotin circumvents the biotinidase deficiency and supplies the necessary free biotin for the biotinylation of the carboxylases, thereby restoring normal holoenzyme activities. Biotin supplementation is a lifelong therapy for these individuals.
Most clinicians have recognized biotinidase deficiency as a childhood disease characterized by various neurologic symptoms, such as lethargy, hypotonia, seizures, ataxia, and developmental delay, and cutaneous features, such as eczematoid skin rashes, alopecia, and fungal infections.4,5 Symptoms markedly improve or resolve with pharmacologic doses of the vitamin biotin.6 Because biotinidase deficiency meets the major criteria for inclusion of a disorder in newborn screening, all the states in the United States and many countries screen their newborns for the disorder.7,8 We have recently shown that continuous biotin treatment prevents the development of symptoms in adolescents and adults with the disorder.9
We initially found several older children and young adolescents with biotinidase deficiency, which we called delayed-onset biotinidase deficiency, who presented with a spectrum of symptoms, including paresis/paraplegia and scotomata, which is not usually seen in younger children with the disorder.10 Over the last several years, a group of older adolescents and adults has been identified with profound biotinidase deficiency who exhibited symptoms of myelitis and spastic paresis/paraplegia with and without retinal/visual abnormalities.11-15 In many of these cases, because an inherited metabolic disorder, let alone biotinidase deficiency, was not included in the differential diagnosis, many of these individuals were thought to have multiple sclerosis, transverse myelitis, myasthenia gravis, neuromyelitis optica, brainstem encephalitis, or Wernicke encephalopathy. These individuals were treated with various regimens based on these putative disorders, but failed to improve. Eventually these individuals were diagnosed with biotinidase deficiency and treated with pharmacologic doses of biotin. In most, symptoms improved or resolved with therapy. However, we have recently shown that if the diagnosis and treatment are markedly delayed in an adult, the symptoms can be irreversible.16 This exemplifies the importance of early diagnosis and treatment to prevent irreversible damage.
Some metabolic disorders are screened for in newborns, but not in all countries. However, even if a country currently screens its newborns for various inherited metabolic disorders, there is a gap of time between when the state or country began screening and the ages of the adult population that may present with symptoms. In addition, even if an individual was found to be unaffected by newborn screening, we must remember that newborn screening is, in fact, screening, and is not always definitive at making or excluding a diagnosis, especially when the screening is based on a cutoff value of a specific metabolite. If a symptom or a constellation of symptoms suggests that an individual may have a metabolic disorder, more specific testing is usually warranted.
As we learn more about the natural history of adults with metabolic diseases, we will gain more knowledge about the symptoms to be included in a variety of differential diagnoses. Because the clinical spectrum of symptoms may be misleading based on those disorders that usually present in children or the symptoms are usually seen in other more common disorders, neurologists will become more dependent on the newer technologies, but they must be aware that the methodologies described above are available.
As stated above, many of the adults diagnosed with inherited metabolic disorders were diagnosed because an astute clinician considered the possibility of inherited metabolic disorder and performed the appropriate metabolic testing. This is likely to change with an increasing awareness about genetic testing methods, such as exomic sequencing. In fact, several of the adults with biotinidase deficiency were not identified because the clinician considered a metabolic disorder or specifically biotinidase deficiency, but rather the clinician performed exomic sequencing, which subsequently identified two nonallelic mutations in the biotinidase gene, indicating that the individual had biotinidase deficiency.10,14 The definitive diagnosis was confirmed by finding profoundly deficient serum biotinidase activity.
The take-home lessons for neurologists that I learned from biotinidase deficiency that apply to many inherited metabolic disorders are as follows:
The possibility of an inherited metabolic disorder should be considered in adults with neurologic symptoms that may or may not mimic those seen in affected children.
These inherited disorders must be included in the differential diagnosis of adults who exhibit neurologic symptoms of a more common disorder, but fail to improve with routine therapies.
Awareness of appropriate testing, such as organic acid and amino acid analysis and exomic sequencing, can help to sort out these disorders, thereby leading to appropriate diagnosis and treatment. Moreover, exomic sequencing can identify specific alterations or mutations in an individual's genome that identify a definitive diagnosis.
Neurologists should “think metabolic” in sorting out their complex and difficult cases. If the neurologist is not comfortable with these metabolic disorders, he or she should consider consulting or referring such individuals to a geneticist or metabolic specialist.
AUTHOR CONTRIBUTIONS
B. Wolf conceived the content of the manuscript and wrote the manuscript.
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
B. Wolf serves as an Associate Editor for Molecular Genetics and Metabolism and MedLink Neurology and receives research support from Safra Research Foundation. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Hollak CEM, Lachmann RH, editors. Inherited Metabolic Disease in Adults, 1st ed New York City: Oxford University Press; 2016. [Google Scholar]
- 2.Wolf B, Heard GS, Weissbecker KA, Secor McVoy JR, Grier RE, Leshner RT. Biotinidase deficiency: initial clinical features and rapid diagnosis. Ann Neurol 1985;18:614–617. [DOI] [PubMed] [Google Scholar]
- 3.Wolf B, Grier RE, Allen RJ, Goodman SI, Kien CL. Biotinidase deficiency: the enzymatic defect in late-onset multiple carboxylase deficiency. Clin Chim Acta 1983;131:273–281. [DOI] [PubMed] [Google Scholar]
- 4.Wolf B. The neurology of biotinidase deficiency. Mol Genet Metab 2011;104:27–34. [DOI] [PubMed] [Google Scholar]
- 5.Salbert BA, Astruc J, Wolf B. Ophthalmological findings in biotinidase deficiency. Ophthalmologica 1993;206:177–181. [DOI] [PubMed] [Google Scholar]
- 6.Wolf B. Biotinidase deficiency: if you have to have an inherited metabolic disease, this is the one to have. Genet Med 2012;14:565–575. [DOI] [PubMed] [Google Scholar]
- 7.Wolf B, Heard GS. Survey of results of neonatal screening programs for biotinidase deficiency. In: Therrell B, ed. Proceedings of the International Symposium for Neonatal Screening. Amsterdam: Elsevier Publishing; 1992. [Google Scholar]
- 8.Wolf B. Worldwide survey of neonatal screening for biotinidase deficiency. J Inherit Metab Dis 1991;14:923–927. [DOI] [PubMed] [Google Scholar]
- 9.Wolf B. Successful outcomes of older adolescents and adults with profound biotinidase deficiency identified by newborn screening. Genet Med 2016;19:396–402. [DOI] [PubMed] [Google Scholar]
- 10.Wolf B, Pomponio RJ, Norrgard KJ, et al. . Delayed-onset profound biotinidase deficiency. J Pediatr 1998;132:362–365. [DOI] [PubMed] [Google Scholar]
- 11.Bottin L, Prud'hon S, Guey S, et al. . Biotinidase deficiency mimicking neuromyelitis optica: initially exhibiting symptoms in adulthood. Mult Scler J 2015;21:1604–1607. [DOI] [PubMed] [Google Scholar]
- 12.Rahman S, Standing S, Dalton RN, Pike MG. Late presentation of biotinidase deficiency with acute visual loss and gait disturbance. Dev Med Child Neurol 1997;39:830–831. [DOI] [PubMed] [Google Scholar]
- 13.Wolf B. Biotinidase deficiency should be considered in individuals exhibiting myelopathy with or without vision loss. Mol Genet Metabol 2015;116:113–118. [DOI] [PubMed] [Google Scholar]
- 14.Girard B, Bonnemains C, Schmitt E, Raffo E, Bilbault C. Biotinidase deficiency mimicking neuromyelitis optica beginning at the age of 4: a treatable disease. Mult Scler 2017;23:119–122. [DOI] [PubMed] [Google Scholar]
- 15.Ferreira P, Chan A, Wolf B. Irreversibility of symptoms with biotin therapy in an adult with profound biotinidase deficiency. J Inherit Metab Dis Rep (in press 2017). [DOI] [PMC free article] [PubMed]
- 16.Demirturk Z, Senturk E, Kose A, Ozcan PE, Telci L. A case of biotinidase deficiency in an adult with respiratory failure in the intensive care unit. Balkan Med J 2016;33:563–565. [DOI] [PMC free article] [PubMed] [Google Scholar]