Practical Implications
Consider small fiber neuropathy as a neurologic complication of undifferentiated arthritis even prior to development of rheumatoid arthritis.
In contrast to Sjögren syndrome (SS),1 small fiber neuropathies (SFN) associated with rheumatoid arthritis (RA) have been sparsely reported.2 Furthermore, many patients with RA pass through an antecedent period termed undifferentiated arthritis (UA),3 in which they may experience an inflammatory arthritis not satisfying criteria for RA or another inflammatory syndrome. SFN may be a rare complication occurring during this presaging period of UA. Yet this possibility is relevant, given that SFN may antedate systemic manifestations of other rheumatic diseases (i.e., SS).1 We report an unusual case of SFN initially developing in a patient with UA, who ultimately develops RA.
Case report
A 55-year-old, right-handed man developed oligoarthritis affecting his ankles. Two months later, a rheumatologist's evaluation did not identify features of RA or another inflammatory disorder, and the patient was subsequently diagnosed with an undifferentiated arthritis3 (table 1). Four months later, he developed overnight (within 6 hours) explosive onset of burning feet pain. Nerve conduction studies were normal (table 2). As described in the figure, punch skin biopsy findings were diagnostic of a length-dependent SFN.4 Further studies did not reveal an identifiable cause, as previously described.4 Over the ensuing year, intensity of burning pain worsened, became refractory to polysymptomatic therapy, and spread to the shins and hands. Oral pulses of corticosteroids (maximal dose 40 mg of prednisone), used for no longer than 2 weeks at a time, were ineffective. Six months later, he developed an unintentional 20-pound weight loss, splinter hemorrhages, and a livedo reticularis rash. He also developed worsening inflammatory arthritis affecting the wrists, knees, and hands, and was referred to our center. In addition to skin lesions, we noted synovitis in symptomatic joints (>10 joints) and radiographic findings of erosions in his wrist. As demonstrated in table 1, the patient now satisfied the revised 2010 classification criteria for RA.5
Table 1.
Distinction between the patient's initial presentation of undifferentiated arthritis vs rheumatoid arthritis (RA) 2 years after disease onset3,5
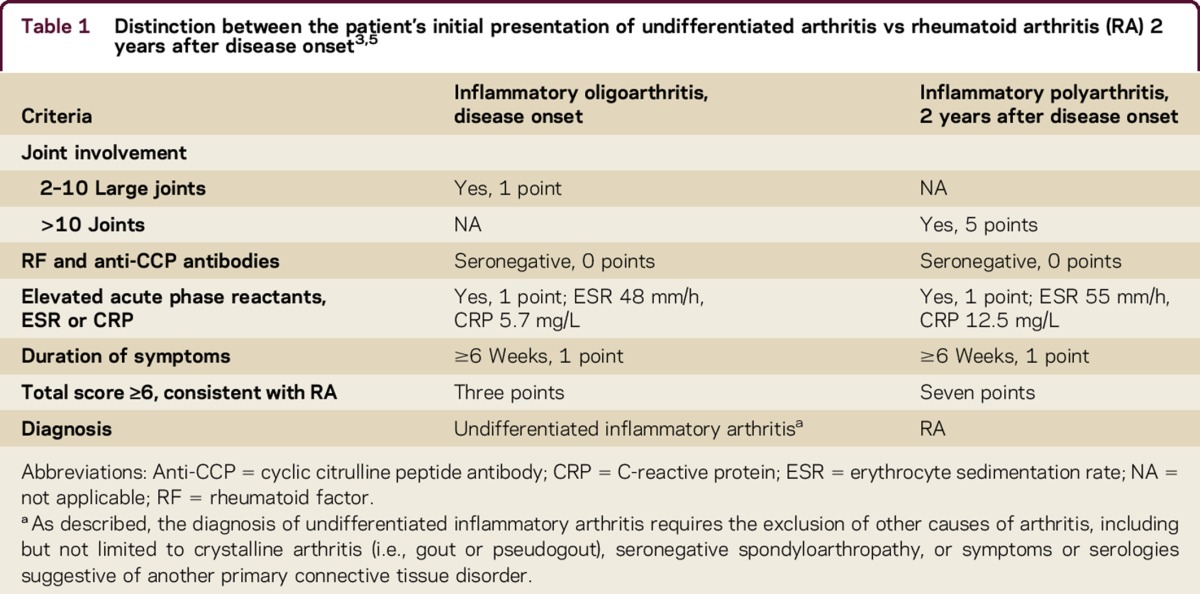
Table 2.
Nerve conduction studies
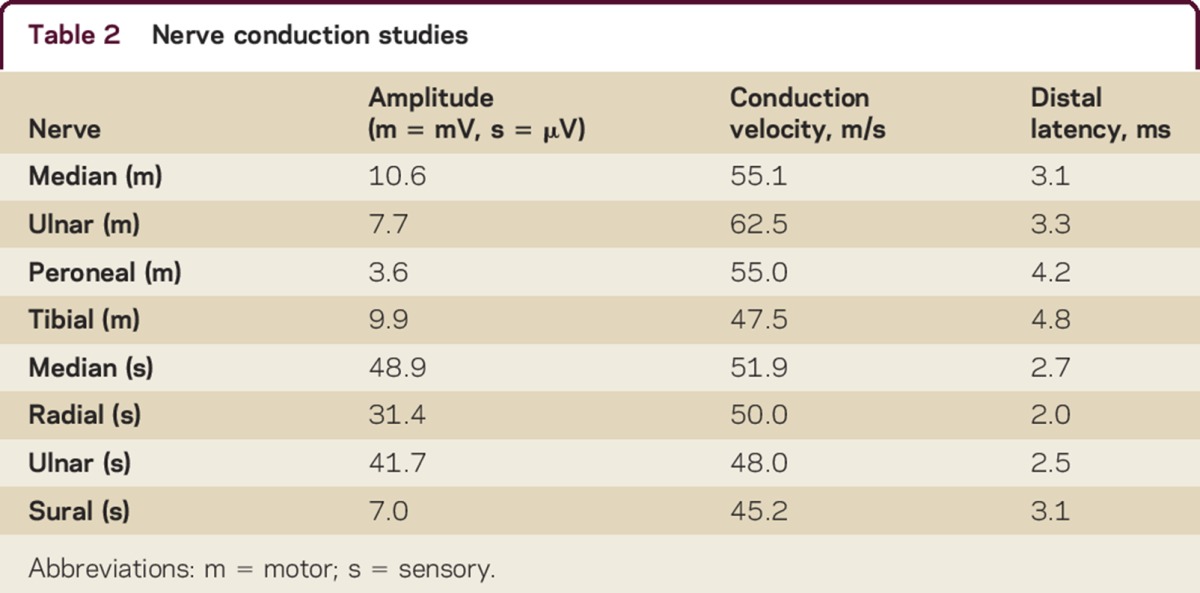
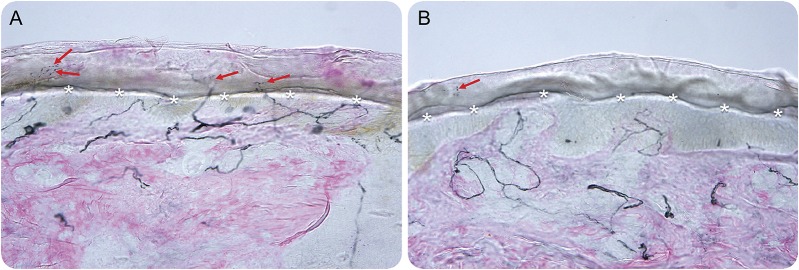
Figure. Skin biopsy findings diagnostic of a small-fiber neuropathy (SFN) in a patient with rheumatoid arthritis.
The patient had symptoms and clinical findings suggestive of SFN, including burning and allodynic pain in his feet, normal Achilles reflexes, preserved vibratory and joint position sensation, normal nerve conduction studies, and length-dependent diminution to pinprick up to the distal shins. Therefore, punch skin biopsy findings were taken from standardized sites at the right calf (A) and the right foot (B). The respective biopsy sites were 10 cm above the lateral malleolus in the calf and in the dorsum of the foot above the extensor digitorum brevis muscle. Panaxonal protein PGP 9.5 immunostaining was performed on the skin biopsy specimens. The intraepidermal nerve fiber density (IENFD) of unmyelinated nerves was quantified. The diagnosis of a SFN was ascertained when the IENFD was below the fifth percentile from normal controls. The asterisks correspond to the boundary between the epidermis and dermis. The arrows correspond to the nerve fibers. As shown in the figure, there is normal IENFD of unmyelinated nerves in a punch biopsy taken from the right calf. In contrast, the figure demonstrates that there is decreased IENFD of unmyelinated nerves in a punch biopsy taken from the right foot. This pattern in which there is a gradient of abnormally reduced IENFD at the distal site (figure) vs the proximal site (figure) is termed a length-dependent SFN, and is consistent with a pattern of primarily axonal degeneration.
The patient appeared barefoot, as even wearing socks on his feet caused intolerable allodynic pain. Examination findings consistent with a SFN included preserved reflexes, normal vibratory and joint position sensation, and length-dependent diminution to pinprick spreading up to the knees and forearms.4 At that point, his SFN was considered as an extra-articular manifestation of his inflammatory arthritis (see rationale, Discussion). There are no guidelines regarding managing RA SFN. We elected to treat with cyclophosphamide, given its role in management of severe RA-associated neuropathies, given that our patient's hyperacute onset of SFN was suggestive of a vasculitic mechanism, and given collective findings suggestive of high disease activity (neuropathy, 20-pound weight loss, rashes, erosive changes).6 The patient did not want further biopsies. Prednisone 60 mg (∼1 mg/kg) given orally once daily (PO qd) was initiated with cyclophosphamide titrated up to 150 mg (∼2 mg/kg) PO qd.
After only 1 month of cyclophosphamide therapy, there was complete and striking resolution of neuropathic pain, inflammatory arthritis, and skin lesions. After 3 months, methotrexate was substituted (titrated up to 25 mg PO weekly) and prednisone was tapered. Despite no recurrence of SFN symptoms, the patient had recurrent arthritis. Consequently, infliximab (tumor necrosis factor inhibitor) was started IV at 5 mg/kg on weeks 0, 2, 6, and then continued every 8 weeks as a maintenance dose, with no recurrence of SFN symptoms or articular disease.
DISCUSSION
We describe an uncommon case in which SFN was identified during antecedent UA. There were several important findings. First, we noted that SFN symptoms initially occurred during presentation of UA, and before the full expression of RA. This finding is similar to other rheumatic diseases, whereby SFN can antedate emergence of rheumatic disease.1 Second, findings that suggested attribution of SFN to an inflammatory arthritis include onset of SFN developing within months of UA, severe and treatment-refractory SFN symptoms persisting until graduation to RA, the association of SFN with high RA disease activity (presence of erosions, diffuse polyarthritis, rashes, and 20-pound weight loss), and the brisk response of SFN symptoms and RA disease activity to immunosuppressive therapy. Finally, the hyperacute onset (<6 hours) of SFN is highly unusual for other noninflammatory causes of SFN, and further suggests attribution to RA.
Clinicians who care for patients with UA should be vigilant for manifestations of SFN, which may persist during graduation to RA. Our suspicion is that SFN is underrecognized in UA as well as other inflammatory arthropathies. Increased recognition can further inform therapeutic strategies.
AUTHOR CONTRIBUTIONS
Drafting/revising the manuscript; study concept or design; analysis or interpretation of data.
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
J. Birnbaum has received speaker honoraria from American College of Rheumatology and receives research support from NIH. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Sene D, Cacoub P, Authier FJ, et al. Sjögren syndrome-associated small fiber neuropathy: characterization from a prospective series of 40 cases. Medicine Epub 2013 Aug 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan S, Zhou L. Characterization of non-length-dependent small-fiber sensory neuropathy. Muscle Nerve 2012;45:86–91. [DOI] [PubMed] [Google Scholar]
- 3.Brinkmann GH, Norli ES, Kvien TK, et al. Disease characteristics and rheumatoid arthritis development in patients with early undifferentiated arthritis: a 2-year followup study. J Rheumatol 2017;44:154–161. [DOI] [PubMed] [Google Scholar]
- 4.Chan AC, Wilder-Smith EP. Small fiber neuropathy: getting bigger! Muscle Nerve 2016;53:671–682. [DOI] [PubMed] [Google Scholar]
- 5.Aletaha D, Neogi T, Silman AJ, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 2010;62:2569–2581. [DOI] [PubMed] [Google Scholar]
- 6.Watts RA, Scott DG. Vasculitis and inflammatory arthritis. Best Pract Res Clin Rheumatol 2016;30:916–931. [DOI] [PubMed] [Google Scholar]