Abstract
Poor self-regulation (i.e., inability to harness cognitive, emotional, motivational resources to achieve goals) is hypothesized to contribute to unhealthy behaviors across the lifespan. Enhancing early self-regulation may increase positive health outcomes. Obesity is a major public health concern with early-emerging precursors related to self-regulation; it is therefore a good model for understanding self-regulation and health behavior. Preadolescence is a transition when children increase autonomy in health behaviors (e.g., eating, exercise habits), many of which involve self-regulation. This paper presents the scientific rationale for examining self-regulation mechanisms that are hypothesized to relate to health behaviors, specifically obesogenic eating, that have not been examined in children. We describe novel intervention protocols designed to enhance self-regulation skills, specifically executive functioning, emotion regulation, future-oriented thinking, and approach bias. Interventions are delivered via home visits. Assays of self-regulation and obesogenic eating behaviors using behavioral tasks and self-reports are implemented and evaluated to determine feasibility and psychometrics and to test intervention effects. Participants are low-income 9–12 year-old children who have been phenotyped for self-regulation, stress, eating behavior and adiposity through early childhood. Study goals are to examine intervention effects on self-regulation and whether change in self-regulation improves obesogenic eating.
Keywords: Obesity, Eating Behavior, Child, Self-Regulation, Health Behavior, Intervention
Childhood obesity is an ongoing public health problem, with almost 25% of children overweight by age 4 years and 35% by adolescence in the United States (Ogden, Carroll, Kit, & Flegal, 2014). Once established, childhood obesity is difficult to treat and tracks into adulthood (Freedman et al., 2005; Nader et al., 2006). The more years one is obese, the greater risk for obesity-associated comorbidities such as coronary heart disease, type 2 diabetes, or hypertension (Berenson et al., 1989; Everhart, Pettitt, Bennett, & Knowler, 1992; Nader et al., 2006). Current prevention and treatment programs focused on diet and physical activity in children and youth have limited efficacy (Czajkowski, 2016; Summerbell et al., 2009). One reason for the modest efficacy of these programs may be the limited attention to basic mechanisms of health behavior change (Onken, 2015; Onken, Carroll, Shoham, Cuthbert, & Riddle, 2014), specifically self-regulation processes that may shape whether the promoted health behaviors are adopted.
Self-regulation occurs at cognitive, emotional, motivational, biological, and behavioral levels. It influences capacity to control thoughts, emotions, and actions to achieve a desired outcome (Blair & Diamond, 2008; Mischel, Shoda, & Rodriguez, 1989). Self-regulation develops during childhood and can set the stage for adult self-regulation (Blair & Diamond, 2008; Kochanska, Coy, & Murray, 2001; Posner & Rothbart, 2000). Adults’ self-regulation deficits are linked to poorer health outcomes for conditions which require long-term behavior management and lifestyle changes (Bickel & Mueller, 2009; Bickel, Quisenberry, Moody, & Wilson, 2015; Heatherton & Wagner, 2011).
Here, we use the Science of Behavior Change (SOBC) experimental medicine approach (Riddle & Science of Behavior Change Working, 2015) to understand processes or mechanisms that influence change in eating behavior. The SOBC approach includes identifying and validating intervention targets, testing whether the target can be engaged through an intervention or experimental manipulation, and systematically testing whether engagement of the targets achieves the hypothesized behavior change. In this study, we focus on testing the engagement of four self-regulation targets and evaluating whether change in these self-regulations causes changes in obesogenic eating.
Improving self-regulation early in life may be a novel approach to obesity prevention; eating behavior provides an excellent context in which to test a self-regulation behavior change model (Czajkowski, 2016; Onken, 2015; Onken et al., 2014). We examine “obesogenic” eating behaviors that are hypothesized to promote risk for obesity, such as eating in the absence of hunger (Birch, Fisher, & Davison, 2003), (in)ability to delay gratification (Francis & Susman, 2009; Seeyave, Coleman, Appugliese, Corwyn, et al., 2009), emotional eating, and unhealthy diet. Pediatric weight management guidelines recommend adherence to diet and physical activity goals (Barlow, 2007). Adhering to such goals requires 1) cognitive capacity to understand how to achieve them (e.g., monitoring diet); 2) emotion regulation to engage despite obstacles (e.g., not overeating when stressed); 3) focus on long-term outcomes (e.g., maintaining healthy weight); and 4) motivation to approach items consistent with goals (e.g., healthy foods) and avoid items inconsistent with goals (e.g., unhealthy foods). Of note, improving self-regulation in one domain may not apply to behavior change in another domain, or across different populations. It is also likely that motivation and effective approaches to behavior change vary as a function of age, social setting, and cultural norms. We focus here on children growing up in poverty, a group at high risk for obesity (Pan, May, Wethington, Dalenius, & Grummer-Strawn, 2013).
Origins of self-regulation can be detected in childhood (Cole, Michel, & Teti, 1994; Ryan & Deci, 2000; Wentzel, 1999; Zelazo et al., 2003) and may shape eating behaviors and obesity risk. Early-life self-regulation associates with lowered obesity risk in adolescence (Seeyave, Coleman, Appugliese, & et al., 2009) and adulthood (Schlam, Wilson, Shoda, Mischel, & Ayduk, 2013), suggesting that early-life self-regulatory capacity may be important for obesity prevention. Associations between self-regulation and obesity during childhood are inconsistent, however perhaps because most studies use a delay-of-gratification task (Mischel et al., 1989) that combines multiple self-regulation components like executive functioning and appetitive drive. Thus, we do not know the specific pathways through which (poor) self-regulation increases childhood obesity risk. Furthermore, although few studies have examined stability of obesogenic eating behaviors from childhood into adulthood, these eating behaviors in adults have been associated with poorer self-regulation (Forman & Butryn, 2015; Martin, Davidson, & McCrory, 2017) and obesity (Teixeira et al., 2015). Further understanding of how improvements in specific self-regulation components, or targets, reduce obesogenic eating during childhood could aid in developing novel strategies to prevent obesogenic eating and obesity risk for adults, as well as children.
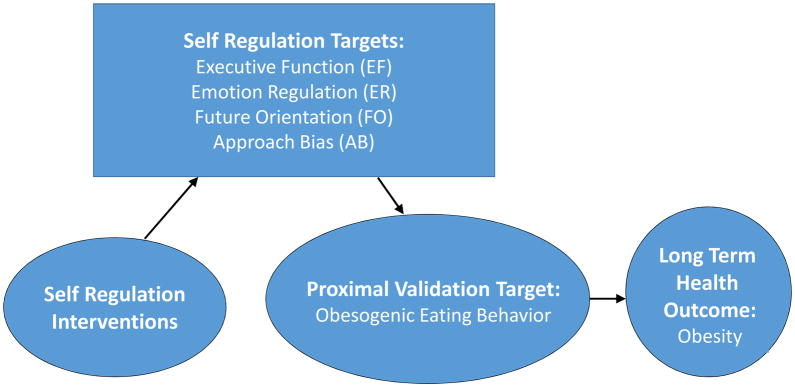
The goal of the current study is to identify, engage, and measure self-regulation targets and map change in these targets to change in obesogenic eating behaviors in school-aged children. Figure 1 presents our conceptual model of self-regulation as a mechanism of health behavior change with regard to eating and obesity risk. Self-regulation targets are Executive Function (EF); Emotion Regulation (ER); Future Orientation (FO); and Approach Bias (AB). The health behavior of interest is obesogenic eating. We view this study as a model that may be applied to a broader spectrum of health behaviors that require self-regulation to achieve improved health outcomes.
Figure 1.
Conceptual Model: Self-Regulation as Mechanism of Behavior Change
Self-Regulation Targets as Mechanisms of Change
Our self-regulation targets (EF, ER, FO, AB) have been shown to associate with eating behavior or obesity. These targets can be assessed in children, with adaptation, and can be changed through intervention, as evidence suggests. Each target is discussed below with regard to the evidence linking it to obesity risk; behavioral interventions to change it; and assessment in children. Goals of this study, aligned with the SOBC framework, are to develop novel methods to assess four domains of self-regulation, evaluate their psychometrics, and test intervention techniques to enhance self-regulation and reduce obesogenic eating behavior. We also address the developmental issues that arise when conducting this work with children.
Target 1: Executive Function (EF)
EF is essential for self-regulation. EF broadly includes working memory, cognitive flexibility, and inhibitory control (Diamond, 2013; Miyake et al., 2000). Deficits in processing speed, working memory (Li, Dai, Jackson, & Zhang, 2008; Maayan, Hoogendoorn, Sweat, & Convit, 2011; Schwartz et al., 2013), cognitive flexibility (Cserjési, Molnár, Luminet, & Lénárd, 2007; Lokken, Boeka, Austin, Gunstad, & Harmon, 2009; Maayan et al., 2011), inhibition and decision-making (Bartholdy, Dalton, O’Daly, Campbell, & Schmidt, 2016; Maayan et al., 2011; Verdejo-Garcia, 2014) have been increasingly identified in association with obesity correlates (Jansen, Houben, & Roefs, 2015; Liang, Matheson, Kaye, & Boutelle, 2013; Smith, Hay, Campbell, & Trollor, 2011). EF deficits may make it difficult to remember guidelines and plan ahead. In school-age children, poorer attention shifting, working memory, and response inhibition were associated with obesogenic eating (Groppe & Elsner, 2014, 2015) and unhealthy diet (Riggs, Spruijt-Metz, Chou, & Pentz, 2011). Further, EF training in obese children enhanced working memory and increased healthy weight maintenance (Verbeken, Braet, Goossens, & van der Oord, 2013). EF training programs that promote working memory (Chacko et al., 2014; Cortese et al., 2015; Jaeggi, Buschkuehl, Jonides, & Shah, 2011; Katz, Jaeggi, Buschkuehl, Stegman, & Shah, 2014; Rapport, Orban, Kofler, & Friedman, 2013; Shinaver, Entwistle, & Soderqvist, 2014) have been found to be effective with school-aged children (Jaeggi et al., 2011; Khalili Kermani, Mohammadi, Yadegari, Haresabadi, & Sadeghi, 2016; Wass, 2014). We use this approach to enhance EF (see “Self-Regulation Interventions” for intervention descriptions).
Target 2: Emotion Regulation (ER)
ER is another self-regulation process affecting health. Stressed and depressed individuals experience poorer health through biological and behavioral pathways (Chen, Langer, Raphaelson, & Matthews, 2004; Chrousos, 1997; Rozanski, Blumenthal, & Kaplan, 1999), which can be established early in life (Chen et al., 2004; G. E. Miller, Chen, & Parker, 2011; Repetti, Taylor, & Seeman, 2002). Emotions may affect health and obesity through multiple pathways. One potential behavioral pathway is through emotional overeating in response to distress (Levitan & Davis, 2010; Turton, Chami, & Treasure, 2017) and feelings of depression (Isasi, Ostrovsky, & Wills, 2013). Consumption of palatable food has been shown to be biologically calming (Dallman M., 2003) and stress-reduction strategies have been proposed as a mechanism to reduce emotional overeating among adults (O’Reilly, Cook, Spruijt-Metz, & Black, 2014). Yet, few child obesity prevention/treatment programs specifically address ER as a mechanism of behavior change. We use biofeedback activities (McKenna, Gallagher, Forbes, & Ibeziako, 2014; Moss, 2014) to enhance child ER capacity.
Target 3: Future Orientation (FO)
Motivation is important in achieving short-term goals (e.g., healthy diet) and longer-term health outcomes (e.g., weight control). (J. O. Prochaska & Velicer, 1997; Strecher, DeVellis, Becker, & Rosenstock, 1986)Motivational interviewing is a health behavior change technique that involves setting personal change goals and building self-efficacy to achieve them (Rollnick, Miller, & Butler, 2008; Strecher et al., 1986). School-age children are developing planning and organizational skills that enable conception of longer-term goals (Anderson, 1996; Krikorian, 1998). Engaging children in future-oriented (FO) thinking, or the process of visualizing and valuing future events, could enhance their capacity for motivation and self-efficacy with regard to health behaviors. It could build their capacity to “mentally project” and invest in their own future (R. B. Miller & Brickman, 2004; Nurmi, 2005). A recent brief intervention using episodic future thinking to promote FO reduced food consumption in adult women (Daniel, Stanton, & Epstein, 2013) and was associated with reduced delay discounting and reduced energy intake among 9 to 14-year-olds (Daniel, Said, Stanton, & Epstein, 2015; Lin & Epstein, 2014). Optimistic thoughts about the future were also found to associate with lower BMI among 9 to 15-year-olds (Kallem et al., 2013). Some have examined FO in relation to health behavior in adults (Hall & Fong, 2003; Joireman, Shaffer, Balliet, & Strathman, 2012), but FO has rarely been considered with regard to health behaviors in children. We developed an intervention to promote FO using episodic future thinking approaches.
Target 4: Approach Bias (AB)
Cues that are repeatedly paired with a given substance (e.g., smell of cigarettes) or food (e.g., image of cookie) can become powerful conditioned stimuli (Berridge, Ho, Richard, & DiFeliceantonio, 2010). Exposure to such cues can trigger a motivational drive for the item (Robinson & Berridge, 1993). Action tendencies in response to the cue can reflect tendencies to approach or avoid the stimulus (Strack & Deutsch, 2004). An approach bias is associated with greater drive for desired substances like alcohol (R. W. Wiers et al., 2007) and food (Dickson, Kavanagh, & MacLeod, 2016). Emerging research suggests that ABs can be modified through approach-avoidance training tasks, wherein individuals are trained to push a joystick away to avoid certain stimuli and to pull it closer to approach other stimuli (Becker, Jostmann, Wiers, & Holland, 2015; Brockmeyer, Hahn, Reetz, Schmidt, & Friederich, 2015; Dickson et al., 2016). Changing AB’s in this manner can reduce substance use (Beard, Sawyer, & Hofmann, 2012; Eberl et al., 2013; Fadardi & Cox, 2009; C. E. Wiers et al., 2014) and may also apply to food-specific AB’s (Becker et al., 2015; Brockmeyer et al., 2015; Houben & Jansen, 2015; Kakoschke, Kemps, & Tiggemann, 2017a; Köpetz, Lejuez, Wiers, & Kruglanski, 2013). Training to reduce AB’s in adults was shown to reduce cravings for and consumption of palatable foods (Fishbach & Shah, 2006; Guerrieri, Nederkoorn, Schrooten, Martijn, & Jansen, 2009; Hardman, Rogers, Etchells, Houstoun, & Munafò, 2013; Houben, 2011; Houben & Jansen, 2015; Kakoschke, Kemps, & Tiggemann, 2014, 2015, 2017b; Kemps, Tiggemann, Martin, & Elliott, 2013; Lawrence, Verbruggen, Morrison, Adams, & Chambers, 2015; Schumacher, Kemps, & Tiggemann, 2016). Scant research has been conducted with children. Altering AB’s early in development could be a powerful tool in shaping later health behavior (Lau, 2013). We created a child-friendly approach-avoidance training task in order to reduce AB for unhealthy food and increase AB for healthy food.
The current study examines EF, ER, FO and AB as self-regulation targets that are hypothesized to relate to obesogenic eating behaviors in children. We seek to manipulate these targets through the interventions described below and additionally assess whether changing self-regulation targets reduces obesogenic eating behavior.
Participants and Intervention Setting
Participants are drawn from an extant cohort of low-income US children (n=250; 56% white/non-Hispanic; 49% male) followed longitudinally since children were 4 years old (Gearhardt et al., in preparation, under review; Lumeng et al., 2014; A. L. Miller et al., 2013; A. L. Miller et al., 2015). Low-income children have higher obesity prevalence (Singh, Siahpush, & Kogan, 2010) and more chronic health problems (Montgomery, Kiely, & Pappas, 1996) than their middle-income peers. Participants were phenotyped for biological and behavioral aspects of self-regulation, including parent-reported and objective measures of eating behavior, emotion regulation and stress reactivity (Leung et al., 2014; Lumeng et al., 2014; A. L. Miller et al., 2013) across early childhood (ages 4–7 years). Here, we focus on middle-to-late childhood (9–12 years), a developmental period in which children assume increased responsibility for their own health behaviors.
Study Design
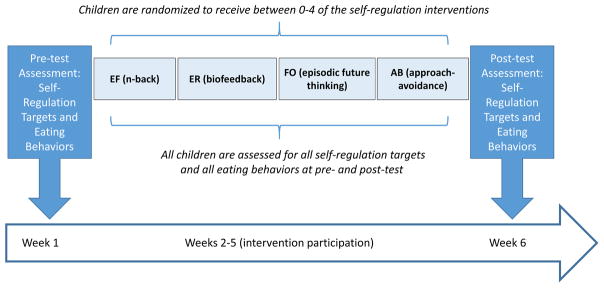
We employ a Multiphase Optimization Strategy Trial (MOST) design (Collins, Dziak, Kugler, & Trail, 2014) to assess which self-regulation targets are changed through intervention. MOST uses a factorial design to identify effectiveness of individual intervention components. MOST is well-suited to the SOBC goal to assess mechanisms of change, as it allows us to map each intervention approach to a specific self-regulation target and to test the impact of each intervention on each target. Children are randomized to receive between 0–4 of the self-regulation interventions, resulting in 16 possible conditions. With 10–11 children per condition, the study is powered to detect small-to-medium effect sizes. The order of intervention delivery is randomized across participants. Self-regulation targets (proximal outcome) and eating behaviors (distal outcome) are assessed for all children at pre- and post-assessment (see Figure 2). We will use MOST to assess which intervention combinations engage self-regulation targets (see Analysis Plan) and whether other factors (e.g., maternal education; child weight) predict response to intervention. The current study will test effectiveness of each intervention to engage each self-regulation target, whether change in self-regulation targets predicts change in health behavior (obesogenic eating), and provide information to enhance tailoring in future interventions.
Figure 2.
Timeline for Intervention Participation and Pre-Post Outcome Evaluation
Self-Regulation Interventions: Development and Implementation
Interventions were selected based on prior experimental or clinical work that showed change in the identified self-regulation target and were feasible to conduct with children in the field. While some interventions had been used with children, others had only been used with adults (e.g., approach-avoidance training). In such cases, we adapted interventions to be developmentally appropriate as described below. Each intervention is delivered during three home visits over a 6-week period where activities are introduced, reviewed and practiced with a trained bachelor’s level interventionist. Home visits were selected for ease of family participation. Some interventions also include home practice and most include a technological component. The child’s parent/guardian is present, but interventions are individually delivered. Protocols are scripted and manualized to ensure implementation fidelity. All sessions are videotaped and 20% coded for fidelity.
Executive Function
The EF training program was selected based on prior work with children that have shown improvements in EF (Jaeggi et al., 2011; Katz et al., 2014; Loosli, Buschkuehl, Perrig, & Jaeggi, 2012). Children are shown pictorial stimuli like fruit or animals on a tablet. They are asked to indicate whether they have seen that image before and how many stimuli ‘back’ they have seen it (e.g., 1 image prior “1-back”, 2 images prior “2-back”). Children learn how to play the “n-back” game during the first home visit and play up to 10 rounds and receive their score at each visit. The game automatically increases or decreases in difficulty depending on the child’s performance. Since school-aged children benefitted most from such training when sessions were administered across a few weeks’ time with daily practice (Wang, Zhou, & Shah, 2014), we leave the tablet with the family after the first home visit. The child is encouraged to practice in between visits by playing through 10 rounds of the game each day and trying to beat prior times. The child completes a home practice log and can earn bigger prizes with more practice.
Emotion Regulation
Our ER intervention uses a combination of biofeedback and assisted relaxation training techniques that are used clinically to promote capacity for self-calming (Bell, 2003; Divine, 2006; McKenna et al., 2014; Moss, 2014). It incorporates computer-mediated biofeedback and home-practice. The child is shown how to monitor and control heart rate and skin conductance using breathing techniques in a computer-game context, Journey to Wild Divine (Bell, 2003; Divine, 2006). A finger sensor displays the child’s heart rate variability data. The child uses this variability to control the game. While the child wears the sensor, the interventionist prompts the child to complete activities. The interventionist demonstrates how the child can alter the color of the heart rate variability status bar with physical movements and breathing (e.g., wiggling fingers, slowing down, taking calm breaths), saying “this colored bar is showing us how calm your body is.” The interventionist helps the child to relax and engage in diaphragmatic breathing using an image of butterfly wings that move in a rhythm on the screen, and narrates how the colors change in response to the child’s breathing. Next, the interventionist teaches the child to use this “power of your body” in a game using breathing techniques to move balloons across the screen. The interventionist also teaches the child relaxation exercises to do at home and leaves laminated instruction cards for home practice.
Future Orientation
Little work has sought to enhance FO in children, but studies in adolescents (Oyserman, Brickman, & Rhodes, 2007; Oyserman & Fryberg, 2006) have shown that visualizing and writing descriptions of future events may enhance future-oriented thinking. Research with adults (Daniel et al., 2013) and pre-adolescents (Daniel et al., 2015) in weight management programs found that enhancing episodic future thinking by encouraging concrete visualization of future events may reduce obesogenic eating. We drew on developmental literature on episodic future thinking (Atance & O’Neill, 2005; Nigro, Brandimonte, Cicogna, & Cosenza, 2014; Nurmi, 2005; Trommsdorff, 1983) and studies of FO in older children (Gott & Lah, 2014; McCabe & Barnett, 2000; Willoughby, Desrocher, Levine, & Rovet, 2012) to develop an intervention to promote FO by engaging children in episodic future thinking. The interventionist asks the child to describe three upcoming events that are positive in nature, using as many details as possible to describe the events. The interventionist works with the child to generate examples, prompting to “use lots of detail to describe it to me; make me really understand what it would be like to be there.” Standard prompts (e.g., “describe what’s happening”; “who will you be with?”, “how will you be feeling?”, “what do you see?”) are used to elicit concrete, descriptive language from the child. There are no between-visit home-practice activities for this protocol.
Approach Bias
Based on experimental work with adults (Becker et al., 2015; Brockmeyer et al., 2015; Dickson et al., 2016), we developed a novel approach-avoidance bias training task, feasible with children as young as 9-years old, that uses images of healthy and unhealthy foods. The task is presented as a timed game for the child. First, the child categorizes images of eight common foods into those that are healthy (e.g., carrots) and unhealthy (e.g., potato chips). This ensures they understand how to sort foods and almost all sort the foods correctly. If not, the incorrectly sorted food is described as “this food is good for our body because it has vitamins that make us grow strong” if healthy, or “this food is not so good for our body” if unhealthy. Next, the child is instructed to use a joystick to pull healthy foods forward and push unhealthy foods away as fast as he/she can. When the food images are pulled toward the child, the image grows larger to fill the screen; when pushed away, the image disappears into the horizon. At each visit, the child plays the game twice through with the examiner and tries to beat the prior round(s); 40 foods are sorted each time. There are no between-visit home-practice activities for this protocol.
Outcome Assessments
We use a multi-method approach to assess self-regulation targets and eating behaviors. We code all interview and observational data, training coders to reliability (Cohen’s Kappa>.70 or ICC>.80) and conducting periodic checks to protect against “coder drift”. We administer parent and child questionnaires orally to reduce literacy concerns. Visits are conducted at community sites. For each child, self-regulation and eating behaviors are assessed in a standard order at pre- and post-intervention (6 weeks later) by trained bachelors-level examiners who are different from the interventionists and blinded to child intervention condition.
Self-Regulation Targets
We hypothesize that children in the self-regulation intervention focused on a given target will show better self-regulation outcomes in that domain (e.g., higher EF scores among children who complete n-back training; better observed ER and more ER strategy use among children who complete biofeedback training; more FO-thinking among children who complete the episodic future thinking task; reduced AB for unhealthy foods among children who complete the approach-avoidance training task) than children who did not receive that intervention. Per the SOBC approach, if evidence emerges that these interventions affect the self-regulation target, they may be used as novel intervention strategies to enhance that domain of self-regulation.
Executive Functioning
As there is some evidence for transfer effects of working memory training (Cortese et al., 2015; Jaeggi et al., 2011; Loosli et al., 2012), we assess multiple EF outcomes (working memory; inhibitory control). Working memory is assessed using a standardized digit span task (Wechsler, 2003). Children recite digits they have just heard in progressively longer sequences; the longest span repeated correctly indexes working memory. Inhibitory control is measured using a go/no-go “Zoo” task (Grammer, Carrasco, Gehring, & Morrison, 2014). The child is taught to play a computer-based game wherein the goal is to help a zookeeper find animals that are loose in the zoo. The child is instructed to press a key to respond as fast as possible when he/she sees the “go” stimulus (orangutan who is “helping” the zookeeper retrieve the escaped animals, presented for 300 ms) but not when he/she sees the no-go stimulus (any other animal). The task requires children to inhibit the response to “go” when they see the “helper” animal, indexing inhibitory control. Scores are based on accuracy and reaction time. Faster, more accurate responses indicate better EF (Akshoomoff et al., 2013; Grammer et al., 2014).
Parents report on child EF using the Metacognition subscale of the Behavior Rating Inventory of Executive Function (Gioia, Isquith, Retzlaff, & Espy, 2002), which is normed for ages 5–18 years. Higher scores indicate better EF (e.g., planning and organizing, attention shifting, working memory).
Emotion Regulation
Children complete a standard task designed to be frustrating: removing a toy from a lockbox using the wrong key (Berger, Miller, Seifer, Cares, & LeBourgeois, 2012; Goldsmith, Reilly, Lemery, Longley, & Prescott, 2001; Lengua, 2008; A. L. Miller, Seifer, Crossin, & LeBourgeois, 2014). The task is videotaped for observational coding of frustration indicators such as negative affect (e.g., frown, cry) or behaviors (e.g., loud sigh, set keys down roughly) based on prior work (Berger et al., 2012; A. L. Miller, Gouley, Seifer, Dickstein, & Shields, 2004; A. L. Miller et al., 2014). More negative displays indicate poorer ER.
Children complete individual interviews to assess ER strategy use and emotion dysregulation. The SIDES Affect dysregulation scale (Brown et al., 2012) assesses how much emotions are disruptive (e.g., “small problems got me very upset”); higher scores indicate poorer ER. Children report on ER strategies using the Children’s Emotion Management Scales (Zeman, Shipman, & Penza-Clyve, 2001) (e.g., “when I am feeling mad, I can stop myself from losing my temper”). Higher scores indicate more effective ER strategies.
Parents report on children’s coping with stress using the NIH Toolbox Perceived Stress scale normed for ages 8–12 years (Kupst et al., 2015; Salsman et al., 2013). They also report on child positive and negative mood using the Positive and Negative Affect Schedule for children (Ebesutani, Okamura, Higa-McMillan, & Chorpita, 2011) which presents positively- and negatively-valenced words and has respondents indicate which best describe how the child generally feels (e.g., upset, scared vs. interested, excited). Responses are summed to generate positive and negative affect scores, with more positive scores indicating better ER.
Future Orientation
As there are few extant measures of FO, we developed our assessment of FO based on a semi-structured interview and two adapted questionnaires. The interview draws on FO research with low-income children (McCabe & Barnett, 2000) and autobiographical memory studies of adolescents (Addis, Wong, & Schacter, 2008; Bohn & Berntsen, 2013; Bromberg, Wiehler, & Peters, 2015) and children (Gott & Lah, 2014; Willoughby et al., 2012). The interviewer asks the child to think of three different events that could happen over the next few days, next week, and next few months, and to describe each event. The interview is audiotaped and later coded using an adaptation of prior coding systems assessing episodic future thinking (Addis et al., 2008; Bromberg et al., 2015). Indicators of FO include use of rich, descriptive detail, vivid imagery, mental state and future-oriented language (e.g., “we will…”) (Bohn & Berntsen, 2013; Bromberg et al., 2015).
The NIH Toolbox Self-Efficacy questionnaire, validated for 8–12 year-old children (Kupst et al., 2015), assesses belief in one’s capacity to manage and have control over meaningful events (e.g., “I can manage to solve difficult problems if I try hard enough”). The Future Time Perspective subscale from the Zimbardo Time Perspective Questionnaire (Zimbardo & Boyd, 2015) assesses how much individuals value future compared to present events and engage in behaviors that prioritize long-term gains (e.g., starting work ahead of time). We adapted certain questions from the adult version based on prior work with youth (e.g., changing “it upsets me to be late for appointments” to “it upsets me to be late for school”) to reflect more child-appropriate language and contexts (Barnett et al., 2013; Wills, Sandy, & Yaeger, 2001). Children indicate how much items reflect their views (e.g., “I can manage to solve difficult problems if I try hard enough”). Higher scores indicate greater FO.
Approach Bias
Because AB’s are related to greater motivation to seek out the substance, we use a relative reinforcing value (RRV) task from prior research (Gearhardt et al., under review) to assess how hard the child is willing to work to gain access to a desired food (Epstein, Leddy, Temple, & Faith, 2007; Raynor & Epstein, 2003). The child is shown how to play a computer game and told that he/she may play the game to win candy. The screen displays boxes containing different shapes; each time a key is pressed the shapes rotate. When all shapes match, the child receives a point. For every five points, the child is given a ticket to redeem for candy. The reinforcement schedule begins at 10 presses to earn one point and doubles each time a ticket is earned (Progressive Ratio (PR) 20, PR 40, PR 80, PR 160, PR 320, PR 640, PR 1280, PR 2560, PR 5120, PR 10240). The highest reinforcement schedule the child completes to earn candy indicates his/her motivation to work for palatable food.
As AB’s are thought to be implicit, we assess children’s implicit bias for food with a single-category implicit association task that we developed based on prior methods to assess attitudes about chocolate and candy in adults (Hofmann, Rauch, & Gawronski, 2007; Houben & Jansen, 2015; Kemps et al., 2013). The task assesses implicit associations between images of chocolate (all images are chocolate per prior work) and “stopping” versus “going”. Children are first shown how to press different buttons when they see a “stop” (e.g., hand signaling stop) versus a “go” signal (e.g., walk sign; 16 trials). In block 2 (48 trials) children sort the “stop” or “go” signals by pressing one of the buttons when one of the signals is paired with an image of chocolate (e.g., “go+chocolate”), and the other button for the other (unpaired) signal (“stop”). In block 3 (48 trials), the pattern is reversed; children sort the “stop” or “go” signals based on the alternate signal-chocolate pairing (e.g., “stop+chocolate” vs. “go”). Following others (Houben & Jansen, 2015), order is counterbalanced such that half of the children first sort chocolate with “stop”, and then with “go” signals; and the other half respond to “go” signals with their left hand and “stop” with their right hand. Scores are calculated using the D600 scoring protocol (Greenwald, Nosek, & Banaji, 2003); higher values indicate a stronger implicit association between chocolate and “go” (AB for chocolate), compared to chocolate and “stop”.
Children also complete the Power of Food Scale (Cappelleri et al., 2009; Lowe et al., 2009) to assess sensitivity to food cues in the environment (e.g. “I think about food even when I’m not truly hungry”) and the ability of these cues to increase desire for food (e.g., “If I see or smell a food I like, I get a very strong desire to have some”). Higher scores reflect greater AB for tempting foods.
Obesogenic Eating Behaviors
Keeping with the SOBC approach, we hypothesize that better self-regulation (the proximal intervention target) will reduce obesogenic eating (the distal outcome). We index obesogenic eating through direct assessment, parent- and child-report.
Eating in the Absence of Hunger (EAH) (eating in response to external cues, vs. hunger) has been found to predict excessive weight gain and obesity (Birch et al., 2003). We use methods from prior work (Gearhardt et al., under review). Children and their families are served a standardized meal: 12-inch deli meat sandwich, baked potato chips, apple sauce, fruit cups, condiments, water. When the child indicates he/she is finished, the researcher invites the child, without the parent, to a separate room. The researcher presents generous, pre-weighed portions of sweet foods, instructs the child that he/she can have as much dessert as he/she would like for five minutes, but cannot take the food home, and goes into the other room (5 minutes). Foods are weighed before and after the protocol and total energy intake (kcal) is calculated to generate an EAH score, representing propensity to eat in the absence of hunger.
Delay of gratification requires balancing the desire to have something now with having more of it later; poorer ability to delay gratification (ATDG) is associated with obesity risk (Appelhans et al., 2011; Epstein, Salvy, Carr, Dearing, & Bickel, 2010; Francis & Susman, 2009). Our ATDG task (Gearhardt et al., under review) involves waiting for food and money (in counterbalanced order), comparable to adult delay discounting tasks (Bickel & Mueller, 2009; Epstein et al., 2010). The child chooses a preferred candy (15-gram packet of M&M’s® or 15-gram packet of Skittles®) and is then shown two piles of candy or money: one with a large quantity (two packets/$1.00) and the other with a small quantity (one packet/$0.50). The child is told that he/she will be allowed to eat the large quantity (or have $1.00) if he/she waits until the examiner returns (up to five trials for both candy and money). The amount of candy or money added is the same absolute value, but the difference between the smaller and larger amounts becomes progressively smaller as the time the child waits increases (up to 15 minutes). The number of trials (zero to five) the child passes is used to indicate ATDG for food (versus money).
Children complete the Dutch Eating Behavior Questionnaire for Children (Carper, Orlet Fisher, & Birch, 2000) which generates three subscales associated with obesity/overweight: dietary restraint/cognitive control of eating; emotional disinhibition of eating; and external disinhibition (eating in response to external cues). Children also complete a questionnaire (Koffarnus & Bickel, 2014) on which they are asked whether they would like to have a smaller amount of a desired food sooner versus a larger amount later. Children respond to nine questions and their discounting rate (point at which their preference for immediate vs. future reward switches) is calculated. Finally, healthy diet attitudes and preferences are measured using a questionnaire that assesses how much the child wants to consume fruits and vegetables (De Bourdeaudhuij et al., 2005).
Parents complete the Children’s Eating Behavior Questionnaire (Wardle, Guthrie, Sanderson, & Rapoport, 2001) a validated, reliable, and frequently used questionnaire that generates eating behavior subscales associated with obesity/overweight (Food Responsiveness, Enjoyment of Food, Emotional Overeating) (Carnell, Haworth, Plomin, & Wardle, 2008; Domoff, Miller, Kaciroti, & Lumeng, 2015). Parents report on their child’s diet (servings/day of sugar-sweetened beverages, high-fat foods, desserts, fruit, vegetables), physical activity and media use in the past seven days and “typical week” (Carlson, Crespo, Patterson, & Elder, 2012; Joe, Carlson, & Sallis, 2012). They also report on the number of restaurant or fast food meals, meals in front of the TV, breakfasts, and family dinners.
Covariates
The study cohort is well characterized regarding perinatal history, demographics (sex, race/ethnicity, maternal education), food insecurity (Kendall, Olson, & Frongillo, 1995) and household chaos (Matheny, Wachs, Ludwig, & Phillips, 1995). Mothers report on their own eating behaviors (Strien, Frijters, Bergers, & Defares, 1986)) impulsivity (Patton & Stanford, 1995) depression symptoms (Radloff), perceived stress (Cohen, Kamarck, & Mermelstein, 1994), and adverse childhood experiences (Dube et al., 2001). Mothers complete the Child Behavior Questionnaire short form (Rothbart, Ahadi, Hershey, & Fisher, 2001) to assess child temperament and report on child pubertal status (NICHD, 2010), child sleep (Owens, Spirito, & McGuinn, 2000), and whether there are electronics/TV in the child’s bedroom. Children self-report on their sleep (Meltzer et al., 2013), media use, physical activity (J. J. Prochaska, Sallis, & Long, 2001) and pubertal status (NICHD, 2010). Children and mothers are weighed using a Detecto Portable Scale Model #DR550C and measured using a Seca 214 portable stadiometer. Mother and child BMIs are calculated and child BMI z-score derived using age- and sex-specific CDC norms (Kuczmarski et al., 2000).
Analysis Plan
Our analysis plan includes three steps. First, we will examine psychometrics (i.e., adequate range; Cronbach’s alpha >.70) and examine factor structure of the self-regulation and eating behavior variables using exploratory factor analysis (EFA). We will examine whether meaningful factors emerge and whether they differ across child groups, e.g., by race/ethnicity. We will also generate a weighted index based on factor loadings.
Second, we will test for change in self-regulation targets. The factorial design used in the MOST approach allows testing of the effect of each specific intervention as well as interactions between interventions using effect coding (Kugler, 2012). Effects of the four individual interventions will be examined as a factorial experiment by crossing of the four interventions (EF; ER; FO; AB) by two levels (present vs. not). A self-regulation target will be considered “engaged” if participation is associated with change in that target (small-to-moderate effect size or statistically significant change in the hypothesized direction). We will test on an intent-to-treat basis using linear mixed models whether each factor has a significant effect on each self-regulation target from pre- to post-intervention. Statistically these effects will be modeled as component by time interactions, with the post-intervention outcome as the primary endpoint. MOST designs also allow for testing whether participant characteristics modify intervention effects so that interventions can be tailored for maximum effectiveness (Collins et al., 2014). We will use a modified version of this decision making approach (Pellegrini, Hoffman, Collins, & Spring, 2014) to examine interactions with child characteristics (e.g., age, weight status, race/ethnicity) to determine whether interventions are equally effective across groups.
Third, we will assess whether change in self-regulation is in turn associated with change in eating behavior. We will examine bivariate associations of self-regulation and eating behavior variables, and employ multivariate analysis using a general linear modeling approach to assess associations among key variables using the appropriate models based on the distribution of the data (i.e., normal, categorical data, count data, reaction time data). We will include covariates as warranted. We will also conduct an intent-to-treat analysis to examine impact of the self-regulation interventions on eating behavior outcomes.
Limitations and Conclusion
In the current study we seek to assess whether the self-regulation assays that were adapted for use based on prior work and that were newly developed for the current study are psychometrically valid with this population of low-income children, to determine whether the self-regulation interventions prompt change in these constructs, and test whether change in these constructs alters obesogenic eating behavior. Following the SOBC approach, we hypothesize that if an intervention does not alter proximal behaviors (e.g., self-regulation), it is unlikely that distal outcomes (e.g., obesogenic eating) will be affected via these mechanisms. Yet, it is also possible that distal outcomes may be affected due to unmeasured mechanisms that change in response to intervention, or that our measures do not adequately capture self-regulation change. Interventions may also have differential effectiveness due to dosage (e.g., home practice vs. not). These hypotheses could be tested in future work, and self-regulation assays that are found to be psychometrically valid and associated with change may be tested in other settings with children (e.g., pediatric clinics; school settings). Ultimately, interventions that integrate multiple elements of self-regulation enhancement may be most effective in reducing health risk behaviors and promoting positive health behaviors. Overall, findings may not only inform obesity prevention efforts, but have broader implications for the science of behavior change by articulating how early self-regulation may function as a broad mechanism of health behavior change.
Highlights.
Self-regulation in children is proposed as mechanism of health behavior change
Executive function, emotion regulation, future orientation, approach bias are assessed
Behavioral interventions to improve child self-regulation are described
Change in self-regulation and obesogenic eating behavior will be tested
Acknowledgments
Role of the Funding Source:
This study was supported by the National Institutes of Health (NIH) Science of Behavior Change Common Fund Program through an award administered by the NICHD UH2HD087979. Open Science Framework (OSF) page: https://osf.io/4vs6z/
Abbreviations
- EF
Executive Function
- ER
Emotion Regulation
- FO
Future Orientation
- AB
Approach Bias
- EAH
Eating in the Absence of Hunger
- ATDG
Ability to Delay Gratification
- CEBQ
Child Eating Behavior Questionnaire
- BMI
Body Mass Index
Footnotes
Conflicts of Interest:
The authors have no conflicts of interests to disclose
ClinicalTrials.gov identifier: NCT03060863
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Addis DR, Wong AT, Schacter DL. Age-related changes in the episodic simulation of future events. Psychol Sci. 2008;19(1):33–41. doi: 10.1111/j.1467-9280.2008.02043.x. [DOI] [PubMed] [Google Scholar]
- Akshoomoff N, Beaumont JL, Bauer PJ, Dikmen SS, Gershon RC, Mungas D, … Heaton RK. Viii. Nih toolbox cognition battery (cb): Composite scores of crystallized, fluid, and overall cognition. Monographs of the Society for Research in Child Development. 2013;78(4):119–132. doi: 10.1111/mono.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson P, Anderson V, Lajoie G. The tower of london test: Validation and standardisation for pediatric populations. The Clinical Neuropsychologist. 1996;10:54–65. [Google Scholar]
- Appelhans BM, Woolf K, Pagoto SL, Schneider KL, Whited MC, Liebman R. Inhibiting food reward: Delay discounting, food reward sensitivity, and palatable food intake in overweight and obese women. Obesity. 2011;19(11):2175–2182. doi: 10.1038/oby.2011.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atance CM, O’Neill DK. The emergence of episodic future thinking in humans. Learning and Motivation. 2005;36(2):126–144. [Google Scholar]
- Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120(Suppl 4):S164–192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- Barnett E, Spruijt-Metz D, Unger JB, Rohrbach LA, Sun P, Sussman S. Bidirectional associations between future time perspective and substance use among continuation high-school students. Substance Use & Misuse. 2013;48(8):574–580. doi: 10.3109/10826084.2013.787092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartholdy S, Dalton B, O’Daly OG, Campbell IC, Schmidt U. A systematic review of the relationship between eating, weight and inhibitory control using the stop signal task. Neuroscience & Biobehavioral Reviews. 2016;64:35–62. doi: 10.1016/j.neubiorev.2016.02.010. doi: http://dx.doi.org/10.1016/j.neubiorev.2016.02.010. [DOI] [PubMed] [Google Scholar]
- Beard C, Sawyer AT, Hofmann SG. Efficacy of attention bias modification using threat and appetitive stimuli: A meta-analytic review. Behavior Therapy. 2012;43(4):724–740. doi: 10.1016/j.beth.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker D, Jostmann NB, Wiers RW, Holland RW. Approach avoidance training in the eating domain: Testing the effectiveness across three single session studies. Appetite. 2015;85:58–65. doi: 10.1016/j.appet.2014.11.017. [DOI] [PubMed] [Google Scholar]
- Bell C. The journey to the wild divine: Users manual. The Wild Divine Project; Boulder, CO: 2003. [Google Scholar]
- Berenson G, Hunter S, Nicklas T, Freedman D, Shear C, Webber L. Risk factors in early life as predictors of adult heart disease: The bogalusa heart study. American Journal of Medical Sciences. 1989;298:141–151. doi: 10.1097/00000441-198909000-00001. [DOI] [PubMed] [Google Scholar]
- Berger RH, Miller AL, Seifer R, Cares SR, LeBourgeois MK. Acute sleep restriction effects on emotion responses in 30- to 36-month-old children. J Sleep Res. 2012;21(3):235–246. doi: 10.1111/j.1365-2869.2011.00962.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge KC, Ho CY, Richard JM, DiFeliceantonio AG. The tempted brain eats: Pleasure and desire circuits in obesity and eating disorders. Brain Res. 2010;1350:43–64. doi: 10.1016/j.brainres.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Mueller ET. Toward the study of trans-disease processes: A novel approach with special reference to the study of co-morbidity. J Dual Diagn. 2009;5(2):131–138. doi: 10.1080/15504260902869147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Quisenberry AJ, Moody L, Wilson AG. Therapeutic opportunities for self-control repair in addiction and related disorders: Change and the limits of change in trans-disease processes. Clinical Psychological Science. 2015;3(1):140–153. doi: 10.1177/2167702614541260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch L, Fisher J, Davison K. Learning to overeat: Maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. Am J Clin Nutr. 2003;78(2):215–220. doi: 10.1093/ajcn/78.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair C, Diamond A. Biological processes in prevention and intervention: The promotion of self-regulation as a means of preventing school failure. Development and psychopathology. 2008;20(03):899–911. doi: 10.1017/S0954579408000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohn A, Berntsen D. The future is bright and predictable: The development of prospective life stories across childhood and adolescence. Dev Psychol. 2013;49(7):1232–1241. doi: 10.1037/a0030212. [DOI] [PubMed] [Google Scholar]
- Brockmeyer T, Hahn C, Reetz C, Schmidt U, Friederich HC. Approach bias modification in food craving - a proof-of-concept study. European Eating Disorders Review. 2015;23(5):352–360. doi: 10.1002/erv.2382. [DOI] [PubMed] [Google Scholar]
- Bromberg U, Wiehler A, Peters J. Episodic future thinking is related to impulsive decision making in healthy adolescents. Child development. 2015;86(5):1458–1468. doi: 10.1111/cdev.12390. [DOI] [PubMed] [Google Scholar]
- Brown LK, Houck C, Lescano C, Donenberg G, Tolou-Shams M, Mello J. Affect regulation and hiv risk among youth in therapeutic schools. AIDS Behav. 2012;16(8):2272–2278. doi: 10.1007/s10461-012-0220-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappelleri JC, Bushmakin AG, Gerber RA, Leidy NK, Sexton CC, Karlsson J, Lowe MR. Evaluating the power of food scale in obese subjects and a general sample of individuals: Development and measurement properties. Int J Obes (Lond) 2009;33(8):913–922. doi: 10.1038/ijo.2009.107. [DOI] [PubMed] [Google Scholar]
- Carlson J, Crespo N, Sallis JF, Patterson R, Elder J. Dietary-related and physical activity-related predictors of obesity in children: A 2-year prospective study. Childhood Obesity. 2012;8(2):110–115. doi: 10.1089/chi.2011.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnell S, Haworth CMA, Plomin R, Wardle J. Genetic influence on appetite in children. International Journal of Obesity. 2008;32(10):1468–1473. doi: 10.1038/ijo.2008.127. [DOI] [PubMed] [Google Scholar]
- Carper JL, Orlet Fisher J, Birch LL. Young girls’ emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite. 2000;35(2):121–129. doi: 10.1006/appe.2000.0343. [DOI] [PubMed] [Google Scholar]
- Chacko A, Bedard AC, Marks DJ, Feirsen N, Uderman JZ, Chimiklis A, … Ramon M. A randomized clinical trial of cogmed working memory training in school-age children with adhd: A replication in a diverse sample using a control condition. J Child Psychol Psychiatry. 2014;55(3):247–255. doi: 10.1111/jcpp.12146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Langer DA, Raphaelson YE, Matthews KA. Socioeconomic status and health in adolescents: The role of stress interpretations. Child development. 2004;75(4):1039–1052. doi: 10.1111/j.1467-8624.2004.00724.x. [DOI] [PubMed] [Google Scholar]
- Chrousos G. Stressors, stress, and neuroendocrine integration of the adaptive response. Hans Selye Memorial Lecture. 1997 doi: 10.1111/j.1749-6632.1998.tb09006.x. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. Perceived stress scale. Measuring stress: A guide for health and social scientists 1994 [Google Scholar]
- Cole PM, Michel MK, Teti LOD. The development of emotion regulation and dysregulation: A clinical perspective. Monographs of the Society for Research in Child Development. 1994;59(2–3):73–102. [PubMed] [Google Scholar]
- Collins LM, Dziak JJ, Kugler KC, Trail JB. Factorial experiments: Efficient tools for evaluation of intervention components. Am J Prev Med. 2014;47(4):498–504. doi: 10.1016/j.amepre.2014.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortese S, Ferrin M, Brandeis D, Buitelaar J, Daley D, Dittmann RW, … Sonuga-Barke EJ. Cognitive training for attention-deficit/hyperactivity disorder: Meta-analysis of clinical and neuropsychological outcomes from randomized controlled trials. J Am Acad Child Adolesc Psychiatry. 2015;54(3):164–174. doi: 10.1016/j.jaac.2014.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cserjési R, Molnár D, Luminet O, Lénárd L. Is there any relationship between obesity and mental flexibility in children? Appetite. 2007;49(3):675–678. doi: 10.1016/j.appet.2007.04.001. doi: http://dx.doi.org/10.1016/j.appet.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Czajkowski SM. National institutes of health update: Translating basic behavioral science into new pediatric obesity interventions. Pediatric Clinics of North America. 2016;63(3):389–399. doi: 10.1016/j.pcl.2016.02.009. doi: http://dx.doi.org/10.1016/j.pcl.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallman M, PN, Akana S, et al. Chronic stress and obesity: A new view of “comfort food”. Proceedings of the National Academy of Sciences. 2003;100(20):11696–11701. doi: 10.1073/pnas.1934666100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel TO, Said M, Stanton CM, Epstein LH. Episodic future thinking reduces delay discounting and energy intake in children. Eat Behav. 2015;18:20–24. doi: 10.1016/j.eatbeh.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel TO, Stanton CM, Epstein LH. The future is now: Reducing impulsivity and energy intake using episodic future thinking. Psychol Sci. 2013;24(11):2339–2342. doi: 10.1177/0956797613488780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bourdeaudhuij I, Klepp K, Due P, Rodrigo CP, De Almeida M, Wind M, … Brug J. Reliability and validity of a questionnaire to measure personal, social and environmental correlates of fruit and vegetable intake in 10–11-year-old children in five european countries. Public Health Nutr. 2005;8(02):189–200. doi: 10.1079/phn2004673. [DOI] [PubMed] [Google Scholar]
- Diamond A. Executive functions. Annual Review of Psychology. 2013;64(1):135–168. doi: 10.1146/annurev-psych-113011-143750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickson H, Kavanagh DJ, MacLeod C. The pulling power of chocolate: Effects of approach-avoidance training on approach bias and consumption. Appetite. 2016;99:46–51. doi: 10.1016/j.appet.2015.12.026. [DOI] [PubMed] [Google Scholar]
- Divine W. Relaxing rhythms 15-step guided training program, version 11.5 [computer program] Las Vegas, NV: Wild Divine, Inc; 2006. [Google Scholar]
- Domoff S, Miller AL, Kaciroti N, Lumeng JC. Validation of the children’s eating behaviour questionnaire in a low-income preschool-aged sample in the united states. Appetite. 2015;95:415–420. doi: 10.1016/j.appet.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the adverse childhood experiences study. Jama. 2001;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- Eberl C, Wiers RW, Pawelczack S, Rinck M, Becker ES, Lindenmeyer J. Approach bias modification in alcohol dependence: Do clinical effects replicate and for whom does it work best? Developmental Cognitive Neuroscience. 2013;4:38–51. doi: 10.1016/j.dcn.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebesutani C, Okamura K, Higa-McMillan C, Chorpita BF. A psychometric analysis of the positive and negative affect schedule for children–parent version in a school sample. Psychological Assessment. 2011;23(2):406. doi: 10.1037/a0022057. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Leddy JL, Temple JL, Faith MS. Food reinforcement and eating: A multilevel analysis. Psychological bulletin. 2007;133(5):884. doi: 10.1037/0033-2909.133.5.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein LH, Salvy SJ, Carr KA, Dearing KK, Bickel WK. Food reinforcement, delay discounting and obesity. Physiol Behav. 2010;100(5):438–445. doi: 10.1016/j.physbeh.2010.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everhart JE, Pettitt DJ, Bennett PH, Knowler WC. Duration of obesity increases the incidence of niddm. Diabetes. 1992;41(2):235–240. doi: 10.2337/diabetes.41.2.235. [DOI] [PubMed] [Google Scholar]
- Fadardi JS, Cox WM. Reversing the sequence: Reducing alcohol consumption by overcoming alcohol attentional bias. Drug Alcohol Depend. 2009;101(3):137–145. doi: 10.1016/j.drugalcdep.2008.11.015. [DOI] [PubMed] [Google Scholar]
- Fishbach A, Shah JY. Self-control in action: Implicit dispositions toward goals and away from temptations. Journal of Personality and Social Psychology. 2006;90(5):820–832. doi: 10.1037/0022-3514.90.5.820. [DOI] [PubMed] [Google Scholar]
- Forman EM, Butryn ML. A new look at the science of weight control: How acceptance and commitment strategies can address the challenge of self-regulation. Appetite. 2015;84:171–180. doi: 10.1016/j.appet.2014.10.004. doi: http://dx.doi.org/10.1016/j.appet.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis LA, Susman EJ. Self-regulation and rapid weight gain in children from age 3 to 12 years. Arch Pediatr Adolesc Med. 2009;163(4):297–302. doi: 10.1001/archpediatrics.2008.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman D, Khan LK, Serdula M, Dietz W, Srinivasan S, Berenson G. The relation of childhood bmi to adult adiposity: The bogalusa heart study. Pediatrics. 2005;115:22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- Gearhardt AN, Miller AL, Sturza J, Epstein LH, Kaciroti N, Lumeng JC. Food motivation, the ability to delay gratification, and eating in the absence of hunger are differentially related to overweight in low-income children (in preparation) [Google Scholar]
- Gearhardt AN, Miller AL, Sturza J, Epstein LH, Kaciroti N, Lumeng JC. Behavioral associations with overweight in low-income children. doi: 10.1002/oby.22033. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Retzlaff PD, Espy KA. Confirmatory factor analysis of the behavior rating inventory of executive function (brief) in a clinical sample. Child Neuropsychology. 2002;8(4):249–257. doi: 10.1076/chin.8.4.249.13513. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Reilly J, Lemery K, Longley S, Prescott A. The laboratory temperament assessment battery: Middle childhood version description of procedures. University of Wisconsin; 2001. [Google Scholar]
- Gott C, Lah S. Episodic future thinking in children compared to adolescents. Child Neuropsychology. 2014;20(5):625–640. doi: 10.1080/09297049.2013.840362. [DOI] [PubMed] [Google Scholar]
- Grammer JK, Carrasco M, Gehring WJ, Morrison FJ. Age-related changes in error processing in young children: A school-based investigation. Developmental Cognitive Neuroscience. 2014;9:93–105. doi: 10.1016/j.dcn.2014.02.001. doi: http://dx.doi.org/10.1016/j.dcn.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, Banaji MR. Understanding and using the implicit association test: I. An improved scoring algorithm. Journal of Personality and Social Psychology. 2003;85(2):197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- Groppe K, Elsner B. Executive function and food approach behavior in middle childhood. Front Psychol. 2014;5:447. doi: 10.3389/fpsyg.2014.00447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groppe K, Elsner B. The influence of hot and cool executive function on the development of eating styles related to overweight in children. Appetite. 2015;87(0):127–136. doi: 10.1016/j.appet.2014.12.203. doi: http://dx.doi.org/10.1016/j.appet.2014.12.203. [DOI] [PubMed] [Google Scholar]
- Guerrieri R, Nederkoorn C, Schrooten M, Martijn C, Jansen A. Inducing impulsivity leads high and low restrained eaters into overeating, whereas current dieters stick to their diet. Appetite. 2009;53(1):93–100. doi: 10.1016/j.appet.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Hall PA, Fong GT. The effects of a brief time perspective intervention for increasing physical activity among young adults. Psychology and Health. 2003;18(6):685–706. [Google Scholar]
- Hardman CA, Rogers PJ, Etchells KA, Houstoun KVE, Munafò MR. The effects of food-related attentional bias training on appetite and food intake. Appetite. 2013;71(0):295–300. doi: 10.1016/j.appet.2013.08.021. doi: http://dx.doi.org/10.1016/j.appet.2013.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Wagner DD. Cognitive neuroscience of self-regulation failure. Trends in cognitive sciences. 2011;15(3):132–139. doi: 10.1016/j.tics.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann W, Rauch W, Gawronski B. And deplete us not into temptation: Automatic attitudes, dietary restraint, and self-regulatory resources as determinants of eating behavior. Journal of Experimental Social Psychology. 2007;43(3):497–504. doi: http://dx.doi.org/10.1016/j.jesp.2006.05.004. [Google Scholar]
- Houben K. Overcoming the urge to splurge: Influencing eating behavior by manipulating inhibitory control. Journal of Behavior Therapy and Experimental Psychiatry. 2011;42(3):384–388. doi: 10.1016/j.jbtep.2011.02.008. doi: http://dx.doi.org/10.1016/j.jbtep.2011.02.008. [DOI] [PubMed] [Google Scholar]
- Houben K, Jansen A. Chocolate equals stop. Chocolate-specific inhibition training reduces chocolate intake and go associations with chocolate. Appetite. 2015;87:318–323. doi: 10.1016/j.appet.2015.01.005. [DOI] [PubMed] [Google Scholar]
- Isasi CR, Ostrovsky NW, Wills TA. The association of emotion regulation with lifestyle behaviors in inner-city adolescents. Eating Behaviors. 2013;14(4):518–521. doi: 10.1016/j.eatbeh.2013.07.009. doi: http://dx.doi.org/10.1016/j.eatbeh.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaeggi SM, Buschkuehl M, Jonides J, Shah P. Short- and long-term benefits of cognitive training. Proc Natl Acad Sci U S A. 2011;108(25):10081–10086. doi: 10.1073/pnas.1103228108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen A, Houben K, Roefs A. A cognitive profile of obesity and its translation into new interventions. Frontiers in Psychology. 2015;6(1807) doi: 10.3389/fpsyg.2015.01807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joe L, Carlson J, Sallis JF. Active where? Individual item reliability statistics parent/child survey 2012 [Google Scholar]
- Joireman J, Shaffer MJ, Balliet D, Strathman A. Promotion orientation explains why future-oriented people exercise and eat healthy evidence from the two-factor consideration of future consequences-14 scale. Personality and Social Psychology Bulletin. 2012;38(10):1272–1287. doi: 10.1177/0146167212449362. [DOI] [PubMed] [Google Scholar]
- Kakoschke N, Kemps E, Tiggemann M. Attentional bias modification encourages healthy eating. Eating Behaviors. 2014;15(1):120–124. doi: 10.1016/j.eatbeh.2013.11.001. doi: http://dx.doi.org/10.1016/j.eatbeh.2013.11.001. [DOI] [PubMed] [Google Scholar]
- Kakoschke N, Kemps E, Tiggemann M. Combined effects of cognitive bias for food cues and poor inhibitory control on unhealthy food intake. Appetite. 2015;87:358–364. doi: 10.1016/j.appet.2015.01.004. [DOI] [PubMed] [Google Scholar]
- Kakoschke N, Kemps E, Tiggemann M. Approach bias modification training and consumption: A review of the literature. Addictive Behaviors. 2017a;64:21–28. doi: 10.1016/j.addbeh.2016.08.007. [DOI] [PubMed] [Google Scholar]
- Kakoschke N, Kemps E, Tiggemann M. The effect of combined avoidance and control training on implicit food evaluation and choice. Journal of Behavior Therapy and Experimental Psychiatry. 2017b;55:99–105. doi: 10.1016/j.jbtep.2017.01.002. [DOI] [PubMed] [Google Scholar]
- Kallem S, Carroll-Scott A, Rosenthal L, Chen E, Peters SM, McCaslin C, Ickovics JR. Shift-and-persist: A protective factor for elevated bmi among low-socioeconomic-status children. Obesity (Silver Spring) 2013;21(9):1759–1763. doi: 10.1002/oby.20195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz B, Jaeggi S, Buschkuehl M, Stegman A, Shah P. Differential effect of motivational features on training improvements in school-based cognitive training. Frontiers in Human Neuroscience. 2014;8:242. doi: 10.3389/fnhum.2014.00242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemps E, Tiggemann M, Martin R, Elliott M. Implicit approach-avoidance associations for craved food cues. Journal of Experimental Psychology: Applied. 2013;19(1):30–38. doi: 10.1037/a0031626. [DOI] [PubMed] [Google Scholar]
- Kendall A, Olson C, Frongillo E. Validation of the radimer/cornell measures of hunger and food insecurity. J Nutr. 1995;125(11):2793. doi: 10.1093/jn/125.11.2793. [DOI] [PubMed] [Google Scholar]
- Khalili Kermani F, Mohammadi MR, Yadegari F, Haresabadi F, Sadeghi SM. Working memory training in the form of structured games in children with attention deficit hyperactivity disorder. Iran J Psychiatry. 2016;11(4):224–233. [PMC free article] [PubMed] [Google Scholar]
- Kochanska G, Coy KC, Murray KT. The development of self-regulation in the first four years of life. Child development. 2001;72(4):1091–1111. doi: 10.1111/1467-8624.00336. [DOI] [PubMed] [Google Scholar]
- Koffarnus MN, Bickel WK. A 5-trial adjusting delay discounting task: Accurate discount rates in less than one minute. Experimental and clinical psychopharmacology. 2014;22(3):222. doi: 10.1037/a0035973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Köpetz CE, Lejuez CW, Wiers RW, Kruglanski AW. Motivation and self-regulation in addiction: A call for convergence. Perspectives on Psychological Science. 2013;8(1):3–24. doi: 10.1177/1745691612457575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krikorian R, Bartok J. Developmental data for the porteus maze test. The Clinical Neuropsychologist. 1998;12:305–310. [Google Scholar]
- Kuczmarski R, Ogden C, Grummer-Strawn L, Flegal K, Guo S, Wei R. Cdc growth charts. Adv Data. 2000;314:1–28. [PubMed] [Google Scholar]
- Kugler KC, Trail JB, Dziak JJ, Collins LM. Effect coding versus dummy coding in analysis of data from factorial experiments. University Park, PA: The Methodology Center, Penn State; 2012. (Technical Report No. 12–120) [Google Scholar]
- Kupst MJ, Butt Z, Stoney CM, Griffith JW, Salsman JM, Folkman S, Cella D. Assessing stress and self-efficacy for the nih toolbox for neurological and behavioral function. Anxiety, stress, and coping. 2015;28(5):531–544. doi: 10.1080/10615806.2014.994204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau JY. Cognitive bias modification of interpretations: A viable treatment for child and adolescent anxiety? Behav Res Ther. 2013;51(10):614–622. doi: 10.1016/j.brat.2013.07.001. [DOI] [PubMed] [Google Scholar]
- Lawrence NS, Verbruggen F, Morrison S, Adams RC, Chambers CD. Stopping to food can reduce intake. Effects of stimulus-specificity and individual differences in dietary restraint. Appetite. 2015;85:91–103. doi: 10.1016/j.appet.2014.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengua LJ. Anxiousness, frustration, and effortful control as moderators of the relation between parenting and adjustment in middle-childhood. Social Development. 2008;17(3):554–577. doi: 10.1111/j.1467-9507.2007.00438.x. [DOI] [Google Scholar]
- Leung CYY, Lumeng JC, Kaciroti NA, Chen YP, Rosenblum K, Miller AL. Surgency and negative affectivity, but not effortful control, are uniquely associated with obesogenic eating behaviors among low-income preschoolers. Appetite. 2014;78:139–146. doi: 10.1016/j.appet.2014.03.025. doi: http://dx.doi.org/10.1016/j.appet.2014.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitan RD, Davis C. Emotions and eating behaviour: Implications for the current obesity epidemic. University of Toronto Quarterly. 2010;79(2):783–799. doi: 10.3138/utq.79.2.783. [DOI] [Google Scholar]
- Li Y, Dai Q, Jackson JC, Zhang J. Overweight is associated with decreased cognitive functioning among school-age children and adolescents. Obesity. 2008;16(8):1809–1815. doi: 10.1038/oby.2008.296. [DOI] [PubMed] [Google Scholar]
- Liang J, Matheson BE, Kaye WH, Boutelle KN. Neurocognitive correlates of obesity and obesity-related behaviors in children and adolescents. Int J Obes. 2013;5(10):142. doi: 10.1038/ijo.2013.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H, Epstein LH. Living in the moment: Effects of time perspective and emotional valence of episodic thinking on delay discounting. Behavioral Neuroscience. 2014;128(1):12–19. doi: 10.1037/a0035705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lokken KL, Boeka AG, Austin HM, Gunstad J, Harmon CM. Evidence of executive dysfunction in extremely obese adolescents: A pilot study. Surgery for obesity and related diseases: Official journal of the American Society for Bariatric Surgery. 2009;5(5):547–552. doi: 10.1016/j.soard.2009.05.008. [DOI] [PubMed] [Google Scholar]
- Loosli SV, Buschkuehl M, Perrig WJ, Jaeggi SM. Working memory training improves reading processes in typically developing children. Child Neuropsychol. 2012;18(1):62–78. doi: 10.1080/09297049.2011.575772. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Butryn ML, Didie ER, Annunziato RA, Thomas JG, Crerand CE, … Halford J. The power of food scale. A new measure of the psychological influence of the food environment. Appetite. 2009;53(1):114–118. doi: 10.1016/j.appet.2009.05.016. [DOI] [PubMed] [Google Scholar]
- Lumeng JC, Miller AL, Peterson KE, Kaciroti N, Sturza J, Rosenblum K, Vazquez DM. Diurnal cortisol pattern, eating behaviors and overweight in low-income preschool-aged children. Appetite. 2014;73:65–72. doi: 10.1016/j.appet.2013.10.016. doi: http://dx.doi.org/10.1016/j.appet.2013.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maayan L, Hoogendoorn C, Sweat V, Convit A. Disinhibited eating in obese adolescents is associated with orbitofrontal volume reductions and executive dysfunction. Obesity (Silver Spring) 2011;19(7):1382–1387. doi: 10.1038/oby.2011.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin AA, Davidson TL, McCrory MA. Deficits in episodic memory are related to uncontrolled eating in a sample of healthy adults. Appetite. 2017 doi: 10.1016/j.appet.2017.05.011. doi: http://dx.doi.org/10.1016/j.appet.2017.05.011. [DOI] [PMC free article] [PubMed]
- Matheny AP, Wachs TD, Ludwig JL, Phillips K. Bringing order out of chaos: Psychometric characteristics of the confusion, hubbub, and order scale. Journal of Applied Developmental Psychology. 1995;16(3):429–444. [Google Scholar]
- McCabe K, Barnett D. The relation between familial factors and the future orientation of urban, african american sixth graders. Journal of Child and Family Studies. 2000;9(4):491–508. doi: 10.1023/A:1009474926880. [DOI] [Google Scholar]
- McKenna K, Gallagher KA, Forbes PW, Ibeziako P. Ready, set, relax: Biofeedback-assisted relaxation training (bart) in a pediatric psychiatry consultation service. Psychosomatics. 2014 doi: 10.1016/j.psym.2014.06.003. [DOI] [PubMed] [Google Scholar]
- Meltzer LJ, Avis KT, Biggs S, Reynolds AC, Crabtree VM, Bevans KB. The children’s report of sleep patterns (crsp): A self-report measure of sleep for school-aged children. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine. 2013;9(3):235–245. doi: 10.5664/jcsm.2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AL, Clifford C, Sturza J, Rosenblum K, Vazquez DM, Kaciroti N, Lumeng JC. Blunted cortisol response to stress is associated with higher body mass index in low-income preschool-aged children. Psychoneuroendocrinology. 2013;38(11):2611–2617. doi: 10.1016/j.psyneuen.2013.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AL, Gouley KK, Seifer R, Dickstein S, Shields A. Emotions and behaviors in the head start classroom: Associations among observed dysregulation, social competence, and preschool adjustment. Early Education and Development. 2004;15(2):147–166. doi: 10.1207/s15566935eed1502_2. [DOI] [Google Scholar]
- Miller AL, Seifer R, Crossin R, LeBourgeois MK. Toddler’s self-regulation strategies in a challenge context are nap-dependent. J Sleep Res. 2014 doi: 10.1111/jsr.12260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AL, Sturza J, Rosenblum K, Vazquez DM, Kaciroti N, Lumeng JC. Salivary alpha amylase diurnal pattern and stress response are associated with body mass index in low-income preschool-aged children. Psychoneuroendocrinology. 2015;53:40–48. doi: 10.1016/j.psyneuen.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological bulletin. 2011;137(6):959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller RB, Brickman SJ. A model of future-oriented motivation and self-regulation. Educational Psychology Review. 2004;16(1):9–33. [Google Scholar]
- Mischel W, Shoda Y, Rodriguez MI. Delay of gratification in children. Science. 1989;244(4907):933–938. doi: 10.1126/science.2658056. [DOI] [PubMed] [Google Scholar]
- Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: A latent variable analysis. Cogn Psychol. 2000;41(1):49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- Montgomery LE, Kiely JL, Pappas G. The effects of poverty, race, and family structure on us children’s health: Data from the nhis, 1978 through 1980 and 1989 through 1991. American Journal of Public Health. 1996;86(10):1401–1405. doi: 10.2105/ajph.86.10.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss DP. Functional symptoms in pediatric disease. Springer; 2014. The use of biofeedback and neurofeedback in pediatric care; pp. 285–303. [Google Scholar]
- Nader P, O’Brien M, Houts R, Bradley R, Belksy J, Crosnoe R … Development, N. I. o. C. H. a. H. D. S. o. E. C. C. a. Y. Identifying risk for obesity in early childhood. Pediatrics. 2006;118:e594–e601. doi: 10.1542/peds.2005-2801. [DOI] [PubMed] [Google Scholar]
- NICHD. Phase iv data collection and timeline: 14 and 15 years of age. Study of Early Child Care and Youth Development (SECCYD) 2010 [Google Scholar]
- Nigro G, Brandimonte MA, Cicogna P, Cosenza M. Episodic future thinking as a predictor of children’s prospective memory. Journal of Experimental Child Psychology. 2014;127:82–94. doi: 10.1016/j.jecp.2013.10.013. [DOI] [PubMed] [Google Scholar]
- Nurmi J-E. Thinking about and acting upon the future: Development of future orientation across the life span. In: Joireman ASJ, editor. Understanding behavior in the context of time: Theory, research, and application. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers; 2005. pp. 31–57. [Google Scholar]
- O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: A literature review. Obes Rev. 2014;15(6):453–461. doi: 10.1111/obr.12156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the united states, 2011–2012. Jama. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onken LS. Cognitive training: Targeting cognitive processes in the development of behavioral interventions. Clinical Psychological Science. 2015;3(1):39–44. doi: 10.1177/2167702614561512. [DOI] [Google Scholar]
- Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M. Reenvisioning clinical science: Unifying the discipline to improve the public health. Clinical Psychological Science. 2014;2(1):22–34. doi: 10.1177/2167702613497932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens JA, Spirito A, McGuinn M. The children’s sleep habits questionnaire (cshq): Psychometric properties of a survey instrument for school-aged children. SLEEP-NEW YORK- 2000;23(8):1043–1052. [PubMed] [Google Scholar]
- Oyserman D, Brickman D, Rhodes M. School success, possible selves, and parent school involvement*. Family Relations. 2007;56(5):479–489. doi: 10.1111/j.1741-3729.2007.00475.x. [DOI] [Google Scholar]
- Oyserman D, Fryberg S. The possible selves of diverse adolescents: Content and function across gender, race and national origin. Possible selves: Theory, research, and applications. 2006;2(4):17–39. [Google Scholar]
- Pan L, May AL, Wethington H, Dalenius K, Grummer-Strawn LM. Incidence of obesity among young us children living in low-income families, 2008–2011. Pediatrics. 2013;132(6):1006–1013. doi: 10.1542/peds.2013-2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton JH, Stanford MS. Factor structure of the barratt impulsiveness scale. Journal of clinical psychology. 1995;51(6):768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pellegrini CA, Hoffman SA, Collins LM, Spring B. Optimization of remotely delivered intensive lifestyle treatment for obesity using the multiphase optimization strategy: Opt-in study protocol. Contemporary Clinical Trials. 2014;38(2):251–259. doi: 10.1016/j.cct.2014.05.007. doi: http://dx.doi.org/10.1016/j.cct.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner MI, Rothbart MK. Developing mechanisms of self-regulation. Development and psychopathology. 2000;12(03):427–441. doi: 10.1017/s0954579400003096. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Sallis JF, Long B. A physical activity screening measure for use with adolescents in primary care. Arch Pediatr Adolesc Med. 2001;155(5):554–559. doi: 10.1001/archpedi.155.5.554. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. American journal of health promotion. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- Radloff L. The ces-d scale: A self report depression scale for research in the general population. J Applied Psychol Measurement. 1977;1:385–401. [Google Scholar]
- Rapport MD, Orban SA, Kofler MJ, Friedman LM. Do programs designed to train working memory, other executive functions, and attention benefit children with adhd? A meta-analytic review of cognitive, academic, and behavioral outcomes. Clin Psychol Rev. 2013;33(8):1237–1252. doi: 10.1016/j.cpr.2013.08.005. [DOI] [PubMed] [Google Scholar]
- Raynor HA, Epstein LH. The relative-reinforcing value of food under differing levels of food deprivation and restriction. Appetite. 2003;40(1):15–24. doi: 10.1016/s0195-6663(02)00161-7. [DOI] [PubMed] [Google Scholar]
- Repetti R, Taylor S, Seeman T. Risky families:Family social environments and the mental and physical health ofoffspring. Psychol Bull. 2002;128:330–366. [PubMed] [Google Scholar]
- Riddle M Science of Behavior Change Working G. News from the nih: Using an experimental medicine approach to facilitate translational research. Transl Behav Med. 2015;5(4):486–488. doi: 10.1007/s13142-015-0333-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggs NR, Spruijt-Metz D, Chou CP, Pentz MA. Relationships between executive cognitive function and lifetime substance use and obesity-related behaviors in fourth grade youth. Child Neuropsychology. 2011;18(1):1–11. doi: 10.1080/09297049.2011.555759. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. The neural basis of drug craving: An incentive-sensitization theory of addiction. Brain research reviews. 1993;18(3):247–291. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Miller W, Butler . Motivational interviewing in health care. Sage Publications; 2008. [Google Scholar]
- Rothbart MK, Ahadi SA, Hershey KL, Fisher P. Investigations of temperament at three to seven years: The children’s behavior questionnaire. Child Dev. 2001;72(5):1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- Rozanski A, Blumenthal J, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55(1):68. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- Salsman JM, Butt Z, Pilkonis PA, Cyranowski JM, Zill N, Hendrie HC, … Cella D. Emotion assessment using the nih toolbox. Neurology. 2013;80(11 Suppl 3):S76–S86. doi: 10.1212/WNL.0b013e3182872e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlam TR, Wilson NL, Shoda Y, Mischel W, Ayduk O. Preschoolers’ delay of gratification predicts their body mass 30 years later. The Journal of Pediatrics. 2013;162(1):90–93. doi: 10.1016/j.jpeds.2012.06.049. doi: http://dx.doi.org/10.1016/j.jpeds.2012.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher SE, Kemps E, Tiggemann M. Bias modification training can alter approach bias and chocolate consumption. Appetite. 2016;96:219–224. doi: 10.1016/j.appet.2015.09.014. [DOI] [PubMed] [Google Scholar]
- Schwartz DH, Leonard G, Perron M, Richer L, Syme C, Veillette S, … Paus T. Visceral fat is associated with lower executive functioning in adolescents. Int J Obes. 2013;37(10):1336–1343. doi: 10.1038/ijo.2013.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeyave DM, Coleman S, Appugliese D, Corwyn RF, Bradley RH, Davidson NS, … Lumeng JC. Ability to delay gratification at age 4 years and risk of overweight at age 11 years. Arch Pediatr Adolesc Med. 2009;163(4):303–308. doi: 10.1001/archpediatrics.2009.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeyave DM, Coleman S, Appugliese D, et al. Ability to delay gratification at age 4 years and risk of overweight at age 11 years. Arch Pediatr Adolesc Med. 2009;163(4):303–308. doi: 10.1001/archpediatrics.2009.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinaver CS, 3rd, Entwistle PC, Soderqvist S. Cogmed wm training: Reviewing the reviews. Appl Neuropsychol Child. 2014;3(3):163–172. doi: 10.1080/21622965.2013.875314. [DOI] [PubMed] [Google Scholar]
- Singh GK, Siahpush M, Kogan MD. Rising social inequalities in us childhood obesity, 2003–2007. Annals of Epidemiology. 2010;20(1):40–52. doi: 10.1016/j.annepidem.2009.09.008. doi: http://dx.doi.org/10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Smith E, Hay P, Campbell L, Trollor JN. A review of the association between obesity and cognitive function across the lifespan: Implications for novel approaches to prevention and treatment. Obesity Reviews. 2011;12(9):740–755. doi: 10.1111/j.1467-789X.2011.00920.x. [DOI] [PubMed] [Google Scholar]
- Strack F, Deutsch R. Reflective and impulsive determinants of social behavior. Personality and social psychology review. 2004;8(3):220–247. doi: 10.1207/s15327957pspr0803_1. [DOI] [PubMed] [Google Scholar]
- Strecher VJ, DeVellis BM, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health Education & Behavior. 1986;13(1):73–92. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- Strien TV, Frijters J, Bergers G, Defares P. The dutch eating behavior questionnaire (debq) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord. 1986;5:295–315. [Google Scholar]
- Summerbell C, Waters E, Edmunds L, Kelly S, Brown T, Campbell K. Interventions for preventing obesity in children. Cochrane Library; 2009. [DOI] [PubMed] [Google Scholar]
- Teixeira PJ, Carraca EV, Marques MM, Rutter H, Oppert JM, De Bourdeaudhuij I, … Brug J. Successful behavior change in obesity interventions in adults: A systematic review of self-regulation mediators. BMC Med. 2015;13:84. doi: 10.1186/s12916-015-0323-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trommsdorff G. Future orientation and socialization*. International Journal of Psychology. 1983;18(1–4):381–406. doi: 10.1080/00207598308247489. [DOI] [Google Scholar]
- Turton R, Chami R, Treasure J. Emotional eating, binge eating and animal models of binge-type eating disorders. Curr Obes Rep. 2017;6(2):217–228. doi: 10.1007/s13679-017-0265-8. [DOI] [PubMed] [Google Scholar]
- Verbeken S, Braet C, Goossens L, van der Oord S. Executive function training with game elements for obese children: A novel treatment to enhance self-regulatory abilities for weight-control. Behav Res Ther. 2013;51(6):290–299. doi: 10.1016/j.brat.2013.02.006. doi: http://dx.doi.org/10.1016/j.brat.2013.02.006. [DOI] [PubMed] [Google Scholar]
- Verdejo-Garcia A. Treatment of the obese patient. Springer; 2014. Reward, reinforcement, and impulsivity in obesity; pp. 23–35. [Google Scholar]
- Wang Z, Zhou R, Shah P. Spaced cognitive training promotes training transfer. Frontiers in Human Neuroscience. 2014;8(217) doi: 10.3389/fnhum.2014.00217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardle J, Guthrie C, Sanderson S, Rapoport L. Development of the children’s eating behavior questionnaire. J Child Psychol Psychiatr. 2001;42(7):963–970. doi: 10.1111/1469-7610.00792. [DOI] [PubMed] [Google Scholar]
- Wass SV. Applying cognitive training to target executive functions during early development. Child Neuropsychology. 2014;21(2):150–166. doi: 10.1080/09297049.2014.882888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler intelligence scale for children-wisc-iv. Psychological Corporation; 2003. [Google Scholar]
- Wentzel KR. Social-motivational processes and interpersonal relationships: Implications for understanding motivation at school. Journal of educational psychology. 1999;91(1):76. [Google Scholar]
- Wiers CE, Stelzel C, Gladwin TE, Park SQ, Pawelczack S, Gawron CK, … Bermpohl F. Effects of cognitive bias modification training on neural alcohol cue reactivity in alcohol dependence. Am J Psychiatry. 2014 doi: 10.1176/appi.ajp.2014.13111495. appiajp201413111495. [DOI] [PubMed] [Google Scholar]
- Wiers RW, Bartholow BD, van den Wildenberg E, Thush C, Engels RC, Sher KJ, … Stacy AW. Automatic and controlled processes and the development of addictive behaviors in adolescents: A review and a model. Pharmacol Biochem Behav. 2007;86(2):263–283. doi: 10.1016/j.pbb.2006.09.021. [DOI] [PubMed] [Google Scholar]
- Willoughby K, Desrocher M, Levine B, Rovet J. Episodic and semantic autobiographical memory and everyday memory during late childhood and early adolescence. Frontiers in Psychology. 2012;3(53) doi: 10.3389/fpsyg.2012.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills TA, Sandy JM, Yaeger AM. Time perspective and early-onset substance use: A model based on stress–coping theory. Psychology of Addictive Behaviors. 2001;15(2):118. doi: 10.1037//0893-164x.15.2.118. [DOI] [PubMed] [Google Scholar]
- Zelazo PD, Müller U, Frye D, Marcovitch S, Argitis G, Boseovski J, … Sutherland A. The development of executive function in early childhood. Monographs of the Society for Research in Child Development. 2003:i–151. doi: 10.1111/j.0037-976x.2003.00260.x. [DOI] [PubMed] [Google Scholar]
- Zeman J, Shipman K, Penza-Clyve S. Development and initial validation of the children’s sadness management scale. Journal of Nonverbal Behavior. 2001;25(3):187–205. doi: 10.1023/A:1010623226626. [DOI] [Google Scholar]
- Zimbardo PG, Boyd JN. Time perspective theory; review, research and application. Springer; 2015. Putting time in perspective: A valid, reliable individual-differences metric; pp. 17–55. [Google Scholar]