Abstract
We aimed to explore the predictive value of screening for distress alone, hope alone, or a combination of both. In a multi-center prospective study, 37 English-speaking Adolescents and Young Adults (AYAs) with cancer and 40 parents completed validated instruments at diagnosis (“baseline”) and 3–6 months later (“follow-up”). Correlated regression models described associations. Within each instrument, baseline and follow-up scores were associated. However, only a composite hope/distress score predicted all three patient-centered outcomes. Multi-dimensional screens incorporating positive and negative psychosocial constructs may predict patient-centered outcomes better than isolated, single-construct instruments.
Keywords: Patient-Centered Outcomes, Psychological Distress, Positive Psychology, Pediatric Cancer, Adolescent and Young Adult Oncology, Palliative Care
INTRODUCTION
Dedicated psychosocial care is important for Adolescents and Young Adults (AYAs) with cancer.1 These patients are at risk for poor mental health and quality of life (QOL), in part because cancer may disrupt normal developmental processes such as the establishment of self-identity, independence, and sexual and social relationships.2,3
While comprehensive psychosocial care is a standard of patient-centered oncology,4,5 evidence-based recommendations are still in development.6 Many guidelines focus on screening for psychological distress;7 however, individual tools may miss significant proportions of AYAs who would benefit from psychosocial services.8 Likewise, evaluations may be less successful if they fail to identify positive psychological resources (e.g., hope) which buffer the impact of illness.9–11 Finally, research regarding the predictive value of screening is limited; its association with longer term patient-centered outcomes such as QOL is unclear.
We conducted post-hoc analyses of data from the “Resilience in Adolescents and Young Adults with Cancer” (RAYA) study12–15 to explore whether distress alone, hope alone, or a composite hope/distress score was more predictive of later patient-reported QOL.
METHODS
Study Design and Participants
RAYA was a multi-center, prospective, longitudinal, mixed-methods study of English-speaking AYAs (ages 14–25) with newly diagnosed, non-Central Nervous System cancer requiring chemotherapy, and their parents.12–15 Consecutive, eligible AYA patients were recruited from two centers (Seattle Children’s Hospital and Dana-Farber/Boston Children’s Hospital). The study was approved by Institutional Review Boards at both sites. All participants provided written informed consent (≥18 years-old) or assent with corresponding parental consent (<18 years-old).
Assessments
AYAs and their parents completed a patient-reported outcome (PRO) survey at the time of enrollment (“baseline,” 14–60 days following diagnosis) and 3–6 months later (“follow-up”). Parents participated at the AYA’s discretion; >1 parent per family could participate. Parents answered questions related to their own self-perceptions.
The survey included age-validated screening tools for: (a) Psychological Distress (Kessler-6 psychological distress scale)16; (b) Dispositional Hope, including sub-scores for “agency” (ability to generate a route to one’s goals) and “pathway” (ability to initiate and maintain actions to reach those goals)17; and, (c) for AYAs only, Cancer-Related QOL (PedsQL 3.0 Cancer Module).18 In each instrument, higher scores represent higher patient-report of the given construct.
Statistical Analyses
We categorized baseline distress as low (Kessler-6 score 0–3), moderate (4–6), high (7–12), or serious (>12), and created a composite hope/distress measure by summing baseline Hope-Pathway and reversed Kessler-6 scores and converting to a 0–100 scale. Where both parents and AYAs completed the same PRO (e.g., Kessler-6 and Hope), data were pooled to augment power. We explored associations between baseline and follow-up assessments using bivariate regression modeling with robust cluster variance estimators to account for within-family or within-patient correlations. Predictors included baseline distress, hope, hope/distress composite, and cancer-related QOL total scores. Outcomes included follow-up high-to-serious distress for logistic regression modeling and total hope and cancer-related QOL total score for linear regression modeling. Each was modeled separately. All testing was two-sided and conducted at alpha <0.05 without correction for multiple comparisons.
RESULTS
Thirty-seven AYAs and 40 parents completed baseline surveys. The AYA median age was 18 years (range 14–24). Fifteen (42%) were female, and 29 (78%) were non-Hispanic White. Acute leukemia and sarcoma were their most common diagnoses. Parent median age was 48 years (range 33–66) and 36 (90%) were non-Hispanic White. Twenty-five AYAs (69%) and 33 parents (83%) remained eligible and completed the second survey. Reasons for attrition were predominantly progressive disease and/or death, although patients who participated in concurrent qualitative interviews appeared more engaged.14
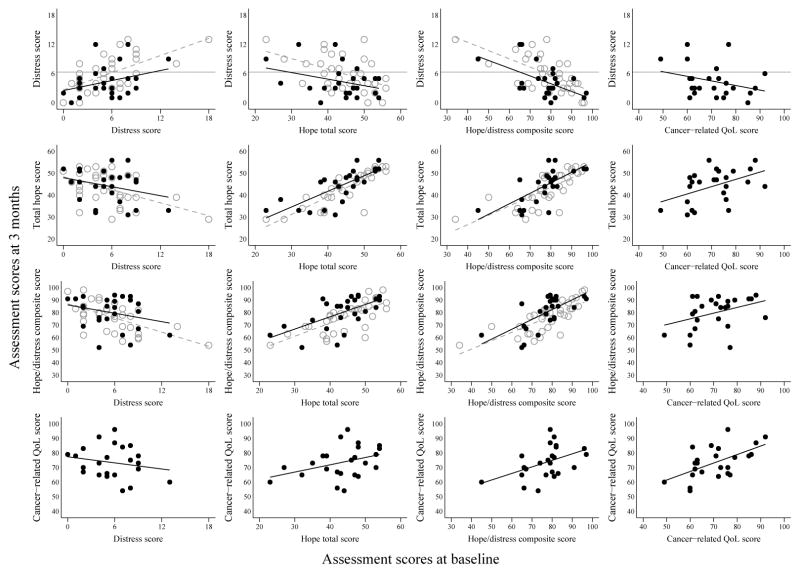
At each time-point, at least one-third of respondents reported high-serious distress (Table 1). Hope and QOL scores were similar to population norms at each time-point.18,19 There was a linear relationship between baseline and follow-up scores for each individual instrument (Figure 1).
Table 1.
Adolescent and Young Adult (AYA) and Parent assessment scores at baseline and 3 month follow-up
| AYA | Parent | |||
|---|---|---|---|---|
|
| ||||
| Baseline (n=37) | 3 months (n=25) | Baseline (n=40) | 3 months (n=33) | |
| Kessler-6 score, mean (SD) | 6 (3) | 4 (3) | 6 (4) | 6 (4) |
| Range | 0–14 | 0–12 | 0–18 | 0–13 |
|
| ||||
| Kessler-6 score categories, n (%) | ||||
|
| ||||
| 0–3 | 8 (22) | 13 (52) | 10 (26) | 8 (24) |
|
| ||||
| 4–6 | 15 (41) | 7 (28) | 13 (33) | 11 (33) |
|
| ||||
| 7–12 | 12 (32) | 5 (20) | 14 (36) | 12 (36) |
|
| ||||
| >12 | 2 (5) | 0 (0) | 2 (5) | 2 (6) |
|
| ||||
| Moderate or serious distress (Kessler-6 >6), n (%) | 14 (38) | 5 (20) | 16 (41) | 14 (42) |
|
| ||||
| Hope total score, mean (SD) | 44 (7) | 44 (8) | 45 (7) | 43 (8) |
|
| ||||
| Hope-Agency* score, mean (SD) | 22 (4) | 22 (4) | 22 (4) | 21 (4) |
|
| ||||
| Hope-Pathway* score, mean (SD) | 22 (4) | 22 (4) | 23 (4) | 22 (4) |
|
| ||||
| Hope/distress composite score**, mean (SD) | 77 (11) | 80 (13) | 78 (12) | 76 (12) |
| Range | 45–97 | 52–94 | 34–96 | 54–98 |
|
| ||||
| PedsQL Cancer Module total score, mean (SD) | 70 (12) | 74 (11) | n/a | n/a |
| Range | 49–93 | 54–96 | n/a | n/a |
Agency sub-score=goal-directed energy, Pathway sub-score=planning to accomplish goals
Higher scores suggest greater hopeful patterns of thought and lower psychological distress
Figure 1.
AYA and parent assessments at follow-up vs. baseline assessments. Cancer-related quality of life plots include AYA only, all others include AYA and parents. Black dots = AYA, gray circles = parents.
Models predicting PROs at follow-up
Distress
Baseline distress, hope, and composite hope/distress, but not QOL, were associated with later high-to-serious psychological distress (Table 2). For example, every higher point of baseline distress increased the odds of later high distress (Odds Ratio [OR]=1.38, 95% CI 1.15–1.67, p<0.01) while every higher point of baseline hope lowered the odds of later high distress (OR=0.89, 95% CI 0.82–0.97, p=0.01). In contrast, associations between baseline QOL and later distress did not reach our threshold of statistical significance (OR=0.9, 95% CI 0.79–1.02, p=0.1).
Table 2.
Associations between individual screening instruments at baseline and patient-centered outcomes at 3 months.
| Outcomes (measured at 3-month follow-up) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Odds Ratio (OR) for high/serious distress (Kessler-6>6) | Hope total score | Cancer-related QOL total score | ||||||||||
|
| ||||||||||||
| Predictors (measured at baseline) | n* | OR | 95% CI | P | n* | Beta | 95% CI | P | n** | Beta | 95% CI | P |
| Kessler-6 score | 57 | 1.38 | 1.15, 1.67 | <0.01 | 57 | −0.9* | −1.4, −0.4 | <0.01 | 24 | −0.7 | −2.2, 0.8 | 0.34 |
| Hope total score | 57 | 0.89 | 0.82, 0.97 | 0.01 | 57 | 0.8* | 0.6, 0.9 | <0.01 | 24 | 0.5 | 0, 1 | 0.07 |
| Hope/distress composite score | 57 | 0.88 | 0.82, 0.95 | <0.01 | 57 | 0.4* | 0.3, 0.6 | <0.01 | 24 | 0.4 | 0.1, 0.8 | 0.02 |
| Cancer-related QOL total score | 25 | 0.90 | 0.79. 1.02 | 0.10 | 25 | 0.3 | 0.1, 0.6 | 0.02 | 24 | 0.6 | 0.2, 0.9 | <0.01 |
Legend: AYA: Adolescent and Young Adult; QOL: Quality of Life
AYAs and parents for all predictors except QOL.
AYAs only
Hope
All baseline PROs, including composite hope/distress, were linearly associated with hope scores at follow-up (Table 2). Baseline higher distress was associated with later lower distress (β −0.9, 95% CI −1.4, −0.4, p<0.01), higher hope (β 0.8, 95% CI 0.6–0.9, p<0.01), and higher QOL (β 0.3, 95% CI 0.1–0.6, p=0.02).
QOL
While baseline QOL was associated with later QOL (β 0.6, 95% CI 0.2–0.9, p<0.01) neither baseline distress nor hope alone was associated with later QOL (Table 2). The only PRO associated later QOL was composite hope/distress (β 0.4, 95% CI 0.1–0.8, p=0.02).
DISCUSSION
We sought to explore the role of early distress and hope as predictors of later patient-centered outcomes, and posited that combined assessment of both might be more informative than either in isolation. Unsurprisingly, early distress predicted later distress and early hope predicted later hope. But, only composite hope/distress scores predicted later QOL. Taken together, our findings suggest solely focusing on alleviating negative symptoms may be insufficient. Although psychosocial intervention research for AYAs with cancer is increasing, optimal targets for intervention design are unclear.20 Concurrent focus on promoting positive psychological resources may hold more promise.
These findings have several important limitations. First, we conducted this post-hoc, exploratory analysis to develop hypotheses for future studies. Second, our sample was relatively small, necessitating pooled parent-child data. We lacked power to adjust for covariates, including sex and potentially collinear PROs. Although we adjusted for intra-family correlation and repeated measures, these results may be different were we to conduct analyses only among AYAs or parents. Third, participants were predominantly white, English-speaking families. Findings may not be generalizable. Fourth, in prior analyses, we found that AYA participation in qualitative interviews minimized attrition.14 Our results may be biased; interviewed participants may have been less distressed and/or more hopeful. Finally, although a strength of this study is its prospective longitudinal design, the utility of distress/hope or other composite screening methods must be validated in future studies.
Until then, these data suggest new opportunities to promote the overall wellbeing of patients with cancer. Screening for both psychopathology and protective resources may provide targeted opportunities for interventions, thereby improving patient experiences with cancer.
Acknowledgments
Funding: St. Baldrick’s Foundation, CureSearch for Children’s Cancer, Seattle Children’s Hospital’s Center for Clinical and Translational Research, and the National Center for Advancing Translational Sciences of the National Institutes of Health (KL2TR000421).
Footnotes
Conflict of Interest: None of the authors has a financial or other conflict of interest to disclose.
References
- 1.Zebrack B, Isaacson S. Psychosocial care of adolescent and young adult patients with cancer and survivors. J Clin Oncol. 2012;30(11):1221–1226. doi: 10.1200/JCO.2011.39.5467. [DOI] [PubMed] [Google Scholar]
- 2.Kwak M, Zebrack BJ, Meeske KA, et al. Prevalence and predictors of post-traumatic stress symptoms in adolescent and young adult cancer survivors: a 1-year follow-up study. Psychooncology. 2013;22(8):1798–1806. doi: 10.1002/pon.3217. [DOI] [PubMed] [Google Scholar]
- 3.Smith AW, Bellizzi KM, Keegan TH, et al. Health-related quality of life of adolescent and young adult patients with cancer in the United States: the Adolescent and Young Adult Health Outcomes and Patient Experience study. J Clin Oncol. 2013;31(17):2136–2145. doi: 10.1200/JCO.2012.47.3173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jacobsen PB, Wagner LI. A new quality standard: the integration of psychosocial care into routine cancer care. J Clin Oncol. 2012;30(11):1154–1159. doi: 10.1200/JCO.2011.39.5046. [DOI] [PubMed] [Google Scholar]
- 5.Kazak AE, Abrams AN, Banks J, et al. Psychosocial Assessment as a Standard of Care in Pediatric Cancer. Pediatr Blood Cancer. 2015;62(Suppl 5):S426–459. doi: 10.1002/pbc.25730. [DOI] [PubMed] [Google Scholar]
- 6.Fann JR, Ell K, Sharpe M. Integrating psychosocial care into cancer services. J Clin Oncol. 2012;30(11):1178–1186. doi: 10.1200/JCO.2011.39.7398. [DOI] [PubMed] [Google Scholar]
- 7.Carlson LE, Waller A, Mitchell AJ. Screening for distress and unmet needs in patients with cancer: review and recommendations. J Clin Oncol. 2012;30(11):1160–1177. doi: 10.1200/JCO.2011.39.5509. [DOI] [PubMed] [Google Scholar]
- 8.Recklitis CJ, Blackmon JE, Chang G. Screening young adult cancer survivors for distress with the Distress Thermometer: Comparisons with a structured clinical diagnostic interview. Cancer. 2016;122(2):296–303. doi: 10.1002/cncr.29736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Folkman S, Greer S. Promoting psychological well-being in the face of serious illness: when theory, research and practice inform each other. Psychooncology. 2000;9(1):11–19. doi: 10.1002/(sici)1099-1611(200001/02)9:1<11::aid-pon424>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 10.Barakat LP, Alderfer MA, Kazak AE. Posttraumatic growth in adolescent survivors of cancer and their mothers and fathers. J Pediatr Psychol. 2006;31(4):413–419. doi: 10.1093/jpepsy/jsj058. [DOI] [PubMed] [Google Scholar]
- 11.Zebrack BJ, Stuber ML, Meeske KA, et al. Perceived positive impact of cancer among long-term survivors of childhood cancer: a report from the childhood cancer survivor study. Psychooncology. 2012;21(6):630–639. doi: 10.1002/pon.1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenberg AR, Yi-Frazier JP, Wharton C, Gordon K, Jones B. Contributors and Inhibitors of Resilience Among Adolescents and Young Adults with Cancer. J Adolesc Young Adult Oncol. 2014;3(4):185–193. doi: 10.1089/jayao.2014.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenberg AR, Bona K, Ketterl T, Wharton CM, Wolfe J, Baker KS. Intimacy, Substance Use, and Communication Needs During Cancer Therapy: A Report From the “Resilience in Adolescents and Young Adults” Study. J Adolesc Health. 2016 doi: 10.1016/j.jadohealth.2016.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosenberg AR, Bona K, Wharton CM, et al. Adolescent and Young Adult Patient Engagement and Participation in Survey-Based Research: A Report From the “Resilience in Adolescents and Young Adults With Cancer” Study. Pediatr Blood Cancer. 2016;63(4):734–736. doi: 10.1002/pbc.25843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Straehla JP, Barton KS, Yi-Frazier JP, et al. The Benefits and Burdens of Cancer: A Prospective Longitudinal Cohort Study of Adolescents and Young Adults. J Palliat Med. 2017;20(5):494–501. doi: 10.1089/jpm.2016.0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 17.Snyder CR, Harris C, Anderson JR, et al. The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol. 1991;60(4):570–585. doi: 10.1037//0022-3514.60.4.570. [DOI] [PubMed] [Google Scholar]
- 18.Varni JW, Burwinkle TM, Katz ER, Meeske K, Dickinson P. The PedsQL in pediatric cancer: reliability and validity of the Pediatric Quality of Life Inventory Generic Core Scales, Multidimensional Fatigue Scale, and Cancer Module. Cancer. 2002;94(7):2090–2106. doi: 10.1002/cncr.10428. [DOI] [PubMed] [Google Scholar]
- 19.Feudtner C, Carroll KW, Hexem KR, Silberman J, Kang TI, Kazak AE. Parental hopeful patterns of thinking, emotions, and pediatric palliative care decision making: a prospective cohort study. Arch Pediatr Adolesc Med. 2010;164(9):831–839. doi: 10.1001/archpediatrics.2010.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walker E, Martins A, Aldiss S, Gibson F, Taylor RM. Psychosocial Interventions for Adolescents and Young Adults Diagnosed with Cancer During Adolescence: A Critical Review. J Adolesc Young Adult Oncol. 2016;5(4):310–321. doi: 10.1089/jayao.2016.0025. [DOI] [PubMed] [Google Scholar]