Abstract
Background
While mindfulness-based interventions (MBIs) employ two distinct practices, focused attention (FA) and open monitoring (OM), the integrated delivery of these practices in MBIs precludes understanding of their practice-specific effects or mechanisms of action. The purpose of this study is to isolate hypothesized active ingredients and practice-specific mechanistic target engagement by creating structurally equivalent interventions that differ only by the active ingredient (meditation practice) offered and to test whether the hypothesized components differentially engage the mechanistic targets that they are purported to engage.
Methods
Participants were intended to be representative of American meditators and had mild to severe affective disturbances. Measures of structural equivalence included participant-level (sample characteristics), treatment-level (program structure and duration, program materials, class size, attendance, homework compliance, etc.), and instructor-level variables (training, ratings and adherence/fidelity). Measures of differential validity included analysis of program materials and verification of differential mechanistic target engagement (cognitive and affective skills and beliefs about meditation acquired by participants after the 8-week training).
Results
The results indicate successful creation of structurally equivalent FA and OM programs that were matched on participant-level, treatment-level, and instructor-level variables. The interventions also differed as expected with respect to program materials as well as mechanistic targets engaged (skills and beliefs acquired).
Conclusions
These validated 8-week FA and OM training programs can be applied in future research to assess practice-specific effects of meditation.
Keywords: meditation, mindfulness, focused attention, open monitoring, dismantling
Introduction: Mindfulness and the Science of Behavior Change
The Science of Behavior Change uses an experimental medicine approach in order to maximize effectiveness of behavioral interventions (Riddle & Ferrer, 2015). This approach requires a paradigm shift toward focusing on (1) identifying and targeting mechanisms, and (2) evaluating the degree to which changes in the hypothesized mechanisms result in altered clinically meaningful outcomes, such as health behavior change and disease occurrence. When target mechanisms are known, interventions can then be modified to maximally engage them. Despite the critical importance of a mechanism-focused approach, few intervention studies test whether their intervention engages the target mechanism, but instead focus on efficacy or clinical outcomes. Like most behavioral interventions, mindfulness-based interventions (MBIs), have an abundance of efficacy trials that lack concurrent verification of target mechanisms. As a result, not enough is known about how MBIs work or how they could be modified to be maximally effective for different populations or endpoints (Dimidjian & Segal, 2015; Gu, Strauss, Bond, & Cavanagh, 2015).
The Mindfulness Research Collaborative (MRC) consists of 11 mindfulness researchers across five universities, and is one of the eight teams in the SOBC Research Network who are working to advance a mechanism-focused approach to behavioral interventions. Our SOBC project “Mindfulness Influences on Self-Regulation: Mental and Physical Health Implications” (Open Science Identifiers: DOI 10.17605/OSF.IO/7752D | ARK c7605/osf.io/7752d) seeks to identify self-regulation intervention targets that are engaged by MBIs, as well as factors that influence target engagement. The collaborative project consists of several meta-analyses and five concurrent clinical trials. The current paper describes the “Dismantling Mindfulness” concurrent clinical trial which aims to verify differential target engagement by different components of MBIs.
Mindfulness-based interventions (MBIs) are one of the fastest growing behavioral interventions. MBIs are being applied to a wide range of disorders, including mental health conditions, especially stress, anxiety and depression (Hofmann, Sawyer, Witt, & Oh, 2010; Khoury, Sharma, Rush, & Fournier, 2015; Wyatt, Harper, & Weatherhead, 2014), as well as physical conditions that are known to interact with mental health and self-regulation, such as obesity, diabetes, cardiovascular disease (Loucks, et al., 2015; Ruffault, et al., 2016), smoking (Maglione, et al., 2017; Oikonomou, Arvanitis, & Sokolove, 2016), and substance abuse (Li, Howard, Garland, McGovern, & Lazar, 2017).
The two most common and prototypical MBIs are Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT). MBSR, originally introduced to improve the management of chronic pain and other medical conditions (J Kabat-Zinn, 1982), has since been applied to a wide variety of clinical and non-clinical populations. MBCT combines the foundational principles of MBSR with elements of cognitive-behavioral therapy (Segal, Williams, & Teasdale, 2002b). While originally designed to prevent depressive relapse, MBCT is now also applied to a wide range of other conditions that are known to be linked to poor emotion regulation, such as overeating/obesity, smoking, substance abuse, and medical treatment non-compliance (Elfhag & Rössner, 2005; Li, et al., 2017; Magai, Consedine, Neugut, & Hershman, 2007; Oikonomou, et al., 2016; Ruffault, et al., 2016; Wallis & Hetherington, 2009; Wing, et al., 2008).
While MBI efficacy studies of multiple clinical and health behavior outcomes are abundant, less is known about their active ingredients or mechanisms of action (Gu, et al., 2015). This gap in knowledge is largely due to the fact that MBIs incorporate a variety of distinct practices and train a variety of different cognitive and affective skills that are presented together under the umbrella term “mindfulness”. Common modern definitions of mindfulness are comprised of two different types of self-regulation: cognitive self-regulation, especially the regulation of attention, and affect regulation, especially secondary emotional reactivity toward both internal and external events (Bishop, et al., 2004; Rapgay & Bystrisky, 2009). While both attention and emotion regulation are thought to be key mechanisms of mindfulness, there are multiple, opposing methods of attention and emotion regulation trained within MBIs. In one, attention is directed away from negative thoughts and emotions—disengaging from them—while in the other, attention is directed toward difficult experiences—intentionally engaging with them. These two attention regulation strategies correspond to two types of affect regulation strategies, as well as two distinct meditation practices, focused attention (FA) and open monitoring (OM), respectively (Lutz, Slagter, Dunne, & Davidson, 2008).
FA practice purportedly engages mechanistic targets related to attentional control, especially orienting and executive function (Fan, McCandliss, Sommer, Raz, & Posner, 2002; Fan, Raz, & Posner, 2003). Orienting directs and limits attention to a selected stimulus. Executive attention—also called conflict monitoring, selective attention, or focused attention—involves prioritizing among competing tasks or responses, and suppressing the goal-incongruent responses (i.e. inhibitory control) (Dillon & Pizzagalli, 2007; Ridderinkhof, van den Wildenberg, Segalowitz, & Carter, 2004; Rueda, Posner, & Rothbart, 2005; van Gaal, Lamme, Fahrenfort, & Ridderinkhof, 2011). FA meditation is a systematic training in directing and sustaining attention on a chosen neutral object (e.g. the breath), noticing when the mind wanders from the object, and disengaging from distractions, negative emotions, rumination or worry by redirecting or shifting one’s attention back to the chosen neutral object (Lutz, et al., 2008; Segal, Williams, et al., 2002b). FA is thought to cultivate both calmness and stability of mind and reduce the arising of afflictive thoughts and emotions (Lutz, et al., 2008).
In a contrast to FA, OM meditation does not involve any specific object of focus, nor does it disengage from negative thoughts or emotions or expect them to diminish; rather, OM entails cultivating “nonreactive awareness of automatic cognitive and emotional interpretations of sensory, perceptual, and endogenous stimuli,” regardless of valence (Lutz, et al., 2008). Rather than reduce the occurrence of afflictive emotions, OM is thought to change one’s relationship to them so that secondary reactivity does not fuel or sustain them. This non-reactive awareness is purported to be a central mechanism by which MBIs exert their effects. “A theoretical premise of MBCT and MBSR is that the development of mindfulness skills leads to non-judgmental and non-reactive acceptance of all experience, which in turn results in positive psychological outcomes”(Gu, et al., 2015). By deliberately turning toward rather than away from difficult thoughts and emotions, OM is thought to promote distress tolerance, non-reactivity and habituation, similar to exposure (Brake, et al., 2016; Uusberg, Uusberg, Talpsep, & Paaver, 2016).
MBSR and MBCT dedicate approximately half of treatment time to attention training through methods of focused attention and the other half to cultivating non-reactivity through methods of open-monitoring (Santorelli, Meleo-Meyer, & Koerbel, 2017; Segal, Williams, et al., 2002b). Because these two practices are delivered in combination, it is difficult to assess their individual contributions to treatment outcomes. More broadly, one of the largest limitations in the field of contemplative science at present is that MBIs have yet to be dismantled into their most basic components and practices (Davidson, 2010; Davidson & Dahl, 2017; Ospina, et al., 2007). As Ospina, et al. (2007) prescribe, “further research needs to be directed toward distinguishing the effects and characteristics of the many different techniques falling under the rubric ‘meditation’” (p. 209). Rapgay and Bystrisky (2009) echo, “since MBSR is an adapted version [of mindfulness practice] with multi-interventional components, advancing its empirical study is problematic since it would require time-consuming efforts and costs to dismantle its various mechanisms” (pp. 160–61). Similarly, Davidson and Dahl (2017), referring to a study conducted by Kok and Singer (2017), point out that the empirical combination of different meditation practices “prevents us from learning which specific component may have been the active ingredient in producing change on the outcome measures…In the absence of dismantling designs that dissect the different constituents of the intervention, we cannot answer this question” (p. 122).
FA and OM exemplify two distinct meditation techniques that are combined together in MBSR/CT but are thought to have different cognitive, affective, behavioral and neurophysiological outcomes (Brefczynski-Lewis, Lutz, Schaefer, Levinson, & Davidson, 2007; Dickenson, Berkman, Arch, & Lieberman, 2013; Hasenkamp & Barsalou, 2012; Hasenkamp, Wilson-Mendenhall, Duncan, & Barsalou, 2012; Lutz, et al., 2008; Manna, et al., 2010; Marzetti, et al., 2014; Rapgay & Bystrisky, 2009). However, like most behavioral research, investigation of mechanism has occurred separately from intervention research (Riddle & Ferrer, 2015). Clear conclusions about practice-specific intervention mechanisms cannot be drawn from current studies on mindfulness because they either used brief (5 min–3 hours) inductions of FA or OM in novices (Ainsworth, Eddershaw, Meron, Baldwin, & Garner, 2013; Arch & Craske, 2006; Dickenson, et al., 2013) or employed cross-sectional analyses of expert meditators who already had training in multiple practices (Brefczynski-Lewis, et al., 2007; Colzato, Szapora, & Hommel, 2012; Hasenkamp & Barsalou, 2012; Hasenkamp, et al., 2012; Manna, et al., 2010; Marzetti, et al., 2014). While practice-specific effects can theoretically be isolated in novices with no prior meditation experience, it is unclear whether novices are able to correctly learn and perform different practices with only a small amount of training or if brief mindfulness inductions are sufficient to produce observable changes in brain activity or behavior. On the other hand, while expert meditators have the advantage of being able to correctly perform each practice on command and can likely demonstrate measureable neuroplastic and behavioral changes as a result of long-term practice, experts inevitably have extensive experience with both FA and OM, which prevents the isolation of practice-specific effects. Thus, the practice-specific effects of longer-term (8-week) FA and OM training programs have yet to be experimentally compared in individuals with no prior meditation experience.
The current study employed the mechanism-focused SOBC experimental medicine approach to isolate hypothesized active ingredients and practice-specific mechanistic target engagement. Following the classic dismantling design of Jacobson, et al. (1996), who compared the relative importance of cognitive restructuring and behavioral activation components of cognitive behavioral therapy (CBT), the current study dismantled MBCT into the separate core practices of FA and OM in order to assess the mechanisms of each practice independently and in comparison to the combination (i.e., MBCT) in a randomized controlled trial.
The primary aims of the current paper are to provide the theoretical rationale for the creation of two separate 8-week programs for FA and OM that are structurally equivalent to MBSR/CT and differentially “valid” in that they reliably engage different hypothesized mechanisms. Differential validity refers to testing that the FA and OM programs address and engage the targets they are purported to engage, as formulated both in Buddhist meditation literature as well as modern, western clinical applications. Measures of structural equivalence include participant-level variables (demographics, clinical diagnoses), treatment-level variables (program structure and duration, program materials, class size, attendance/attrition, homework compliance, etc.) and instructor-level variables (training, treatment ratings, and adherence/fidelity). Measures of differential validity include analysis of program materials (handouts, audiotapes, and readers) and mechanistic target engagement in terms of differential skills and beliefs acquired. Specifically, we will test whether FA engages targets related to attention control, and OM engages targets related to affective non-reactivity.
Methods
Participants
Inclusion criteria
Americans commonly engage in meditation as an alternative means to alleviate symptoms associated with affective disturbance and to improve overall health and well-being (Barnes, Bloom, & Nahin, 2008; Grossman, Niemann, Schmidt, & Walach, 2004). The present sample was intended to be representative of this population and therefore included both clinical and non-clinical expressions of affective disturbances, including stress, anxiety and depression. Participants were English-speaking individuals, age 18–65 with mild-severe levels of depression (Inventory of Depressive Symptomatology [IDS] score of 10–48) and persistently high levels of negative affect (Positive and Negative Affect Schedule [PANAS] negative affect scale score >18 in last month). Specific diagnostic criteria, although measured, were not required for inclusion, as such a categorical approach overlooks the significant contribution of subclinical symptoms to the persistent course of illness (Cuijpers, Beekman, Smit, & Deeg, 2006; Cuijpers & Smit, 2004; Jacob, in press; Krueger, Caspi, Moffitt, & Silva, 1998; Krueger, Chentsova-Dutton, Markon, Goldberg, & Ormel, 2003; Lovibond, 1998); functional impairment and quality of life (Cuijpers, de Graaf, & van Dorsselaer, 2004; Gotlib, Lewinsohn, & Seeley, 1995; K. B. Wells, et al., 1989); economic burden (P Cuijpers, et al., 2006; Das-Munshi, et al., 2008) and increased risk for developing health problems, including heart disease, stroke and cardiovascular mortality (Frasure-Smith, Lesperance, & Talajic, 1995; Nabi, Kivimaki, De Vogli, Marmot, & Singh-Manoux, 2008; Nabi, Kivimaki, Zins, et al., 2008; Nabi, et al., 2009). In addition, mild to severe affective disturbances, including anxiety and depression that are primary or secondary to another health condition, are the unifying sample characteristic and exhibit the most reliable improvements across MBSR/CT treatment studies of various conditions and diagnoses (Barnhofer, et al., 2009; Eisendrath, et al., 2008; Finucane & Mercer, 2006; Kenny & Williams, 2007; Kingston, Dooley, Bates, Lawlor, & Malone, 2007; Lengacher, et al., 2009; Schroevers & Brandsma, 2009; Williams, et al., 2008; Yook, et al., 2008).
Exclusion criteria
Participants were excluded if they met any of the following criteria: a) extremely severe levels of depression (IDS>48) or active suicidal ideation; b) history of bipolar disorder, psychotic disorder, persistent antisocial behavior, repeated self-harm, borderline or antisocial personality disorder, or organic brain damage; c) current panic, PTSD, obsessive-compulsive disorder, eating disorder or substance abuse/dependence; d) inability to read and write in English; e) current psychotherapy (>1 session/month); f) regular meditation practice or e) change in antidepressant medication type or dosage in the last 8 weeks. Although MBSR/CT has been used in individuals with extremely severe levels of depression (Barnhofer, et al., 2009; Eisendrath, et al., 2008; Finucane & Mercer, 2006; J Kabat-Zinn, et al., 1992; Kenny & Williams, 2007; Kingston, et al., 2007), these individuals were excluded from the present study because the clinical efficacy of individual MBSR/CT subcomponents (i.e., FA and OM) has not been evaluated.
Trial Design and Procedure
Setting
The study took place at the Clinical and Affective Neuroscience Laboratory in the Department of Psychiatry and Human Behavior at Brown University Medical School in Providence, RI between November 2012 and March 2016. Participants were recruited through community flyers for a mindfulness or meditation-based program intended for people with anxiety, stress or depression. Efforts were made to recruit racial and ethnic minorities by advertising in areas with high representation of those demographics.
Sample size and power
While effect sizes in mood and sleep following MBCT compared to a waitlist in a previous study were large (Britton, Haynes, Fridel, & Bootzin, 2010) the differences between active treatments tend to be small (Wampold, et al., 1997). Using G*Power, a sample size of 90 (30 per intervention) would be able to detect a small effect size (d = 0.34, power > .80, alpha= 0.05) of within-between interactions in a repeated-measures ANOVA. Based on pilot studies, we estimated a 15% attrition rate (Shahar, Britton, Sbarra, Figueredo, & Bootzin, 2010) and thus needed to enroll a total of 105 subjects (35 per group) in order to have 90 completers.
Randomization
The trial was a 3-armed cluster-randomized trial with a 1:1:1 allocation ratio, without baseline variable stratification. The random allocation sequence was generated by an independent statistician using R (www.r-project.org) with a pre-specified seed. The sequence was a Latin square design, where each treatment appeared only once in each year and in each season such that for each treatment, the year and seasonality effects are balanced out. In order to ensure adequate group size and minimize wait time to enter treatment, randomization required a quorum of at least four eligible participants who had completed baseline assessments. Treatment start dates were preset, and randomization of eligible participants occurred no later than three days before the treatment start date. The results of each allocation were recorded by the statistician and communicated to the PI, who was one of the co-therapists for each treatment. Following the methods of other multi-arm MBCT and MBSR trials (Ong, Hedeker, Wyatt, & Manber, 2016; Segal, et al., 2010) treatment allocation was performed at the group level. For example, each group of 10–12 participants was randomized into one of three treatments (i.e., group allocation) nine different times. Because all three active treatments were presented as “mindfulness training,” participants were unaware that they received a certain treatment rather than another. Only the therapists, one of whom was the PI, knew the identifications of each treatment. Baseline assessment occurred before randomization, and staff involved in post-treatment assessments were blind to treatment allocation. The PI maintained the treatment information in a password-protected electronic file and provided de-identified codes to signify different treatments during analysis.
Interventions
FA and OM manual creation
The FA and OM programs were created collectively by Drs. Britton, Davis, and Lindahl, who hold Ph.D.’s in clinical psychology, philosophy, and religious studies, respectively. Dr. Britton is a clinical psychologist and certified MBSR/CT instructor who has more than two decades of personal practice experience and has taught and/or researched meditation-based interventions in clinical and school-based populations for more than 15 years. Dr. Davis holds a Ph.D. in Philosophy with a specialty in Buddhist philosophy. He received textual, meditative and monastic training in the Theravāda Buddhist tradition of Burma in the lineage of Mahasi Sayadaw and has served as an interpreter and meditation teacher for that tradition. Dr. Lindahl holds a Ph.D. in religious studies with a specialty in the theory and practice of Indian and Tibetan Buddhist meditation. His research employs a cognitive science of religion approach to provide explanatory frameworks that account for the relationship between contemplative practices and resultant experiences.
Treatment content and format
FA and OM-based treatments are based on the Mindfulness-Based Cognitive Therapy format. While extremely similar in approach and content, MBCT was chosen over MBSR because MBCT has a published session-by-session manual with standardized handouts (Segal, Williams, et al., 2002b) and precise, published treatment fidelity guidelines for therapists (Segal, Teasdale, Williams, & Gemar, 2002). In contrast, MBSR's (unpublished) treatment guidelines (Santorelli, 2014; Santorelli & Kabat-Zinn, 2003) allow for a large variation in content and practices, including the possibility of up to 67% of total practice time allocated to yoga. Furthermore, MBCT allocates 100% of its psychoeducation content to addressing affective disturbances (the main outcome of the proposed study), while MBSR includes potentially confounding training in areas such as communication skills, diet and nutrition. In addition, MBCT contains explicit, in-class exercises and audio files for using mindfulness practices to cope with acute negative affect, while MBSR does not.
All three interventions were matched for duration, format and content, including class size, minutes of meditation, and number of handouts. Classes met for three hours once a week for eight weeks with a daylong (10am–4pm) silent retreat during either the sixth or seventh week. Homework consisted of 45 min/day of formal meditation practice, six days/week. Weeks 1–4 included basic practice instruction; weeks 5–8 focused on applying the practices to manage acute negative affect (e.g., “working with difficulty”). Like MBSR/CT, FA and OM modules engaged all 4 postures, including sitting, lying down, standing/walking, and moving/stretching (yoga), both during formal practice as well as during interpersonal exchanges and daily activities. All meditations were followed by discussion first in dyads and then with the larger group with inquiry from the instructors.
Psychoeducation
Didactic portions including the neuroscience and physiology of stress/depression and meditation and psychoeducation about depression were kept constant in all three treatments. The Healing from Within video (Grubin, 1993) was shown in all three treatments during sessions four and five. The MBCT version was unedited, but the FA and OM versions were edited to match practice-specific content (e.g., the OM version did not show focusing on the breath).
Location
To control for the effect of environment and surroundings (Chaikin, Derlega, & Miller, 1976; Miwa & Hanyu, 2006; Shibata & Suzuki, 2002; Ulrich, 1991), all treatment sessions took place in the same room in the Biomed complex at Brown University. The room was decorated with two plants and two silk wall hangings for each session. Each participant was provided with a chair and two meditation cushions (zafu/zabuton). The content and format of the proposed FA and OM modules can be compared to standard MBCT in the Session by Session Comparison Table in Supplementary Appendix 1.
Focused Attention Meditation Program
The FA module included training in focused attention techniques, which by definition require sustained attention on a selected object (or “anchor”) with concomitant de-selection of surrounding objects and events. According to Lutz, et al. (2008), FA includes four interrelated skills: 1) sustaining attention on a chosen object; 2) identifying distractions without destabilizing the intended focus; 3) disengaging from a distracting object without further involvement and 4) redirecting focus promptly to the chosen object (Lutz, et al., 2008). As skills develop, FA involves “attending continuously to a familiar object, without forgetfulness or distraction” (Wallace, 2006, p. 13). The main practice in FA used six meditation objects or anchors that are commonly used in mindfulness training and MBSR/CT: the feet, the hands, breath at belly, breath at chest, breath at nostrils, and sound (see Supplementary Appendix 2). Participants were encouraged to pick at least two anchors, a primary and secondary, as their main meditation objects. In week six, when “series two” audiotapes are introduced in MBSR/CT, additional objects that were derived from traditional meditation objects (Buddhaghosa, 1976) were introduced, including repeated phrase-based brahmavihāras (metta/karuna) (Salzberg, 2002). Additionally, subtle objects such as stillness, silence, and space were adapted from Wangyal and Vaughn (2012). While compassion and loving-kindness meditation have been categorized as different styles of meditation from FA or OM (Lee, et al., 2012), traditionally the brahmavihāras are often used as a means to cultivate concentration in the style of FA (Buddhaghosa, 1976).
Open Monitoring meditation program
The OM module included training in bringing a balanced and unbiased attention to ongoing experience without directing attention or selecting or de-selecting objects. In OM meditation, “one aims to remain only in the monitoring state, attentive moment by moment to anything that occurs in experience without focusing on any explicit object” (Lutz, et al., 2008, p. 2). Thus, unlike FA, OM is considered “objectless” and “choiceless,” as it involves no strong distinction between selection and de-selection of stimuli. Whereas extraneous stimuli are considered distractors in FA, in OM no stimuli are extraneous because attention is open to the entire field of experience (Lutz, et al., 2008).
Noting or verbal labeling of phenomena, such as “sadness” or “wanting to move” or “itching” is a common practice in many forms of mindfulness in both Buddhist (Goldstein, 2002) and clinical settings, including DBT, MBSR and MBCT (Jon Kabat-Zinn, 1990; Linehan, 1993; Segal, Williams, & Teasdale, 2002a). Meditations in the OM module employed the Mahasi tradition’s style of noting (Sayadaw, 1991; Young, 2011), where a verbal label is given to categories of experience as these experiences arise and pass in each moment. Labeling began with six categories of experience: seeing, hearing, feeling (body sensations), tasting, smelling and thinking (see Supplementary Appendix 3). Participants were encouraged to break down feeling and thinking into more fine-grained categories of their choosing, such as body sensations into warmth/coolness, pressure, vibration, moisture, etc., and thinking into image-thought, memory thought, planning thought, evaluative thought, etc. Participants were taught to practice OM at different levels of subtlety, progressing from saying the labels out loud, to mentally noting, to noticing wordlessly (i.e., without labeling). In week two, where “feeling tone” or valence is introduced in MBSR/CT, participants learned to notice (and label) the valence of each passing experience as pleasant, unpleasant, or neutral.
Noticing whatever is most salient in one’s experience can reinforce automatic and unconscious attention or affective biases if one is not aware of them. As a result, some people may attend to their experience and only notice unpleasant thoughts or pain. Thus, as an extension to the automatic thoughts worksheet, participants completed exercises to become familiar with their tendencies to attend to certain categories of experience over others (e.g., thinking vs. body sensation) as well as certain valences (e.g., negative vs. positive). Their week six “series two” OM practice was to “balance awareness” evenly across all six categories and valences in an even-handed or balanced way. While negative thinking bias is the example here, positive biases that neglect or avoid negative stimuli are also addressed with this exercise.
Measures
Structural equivalence outcome measures
Participant-level variables
Sample characteristics included demographics (age, gender, race, education, etc.), anti-depressant medication use, baseline mental health diagnoses and severity of those diagnoses.
Treatment-level variables
Program structure
Structural components included number and duration of each session, total number of contact hours, number of groups (treatment cycles), number of participants in each group, attendance, attrition and homework compliance.
Course materials
In order to maintain structural equivalence across programs, course materials were comparable across treatment conditions. Course materials included class handouts, worksheets, homework instructions and audio files of meditation exercises provided for home practice. In addition, each group received a “reader” that was specifically tailored to match their treatment condition. Per standard practice for MBIs, the MBCT group received Full Catastrophe Living (FCL) (Jon Kabat-Zinn, 1990), distributed in session four, which includes practice instructions and testimonials. The FA and OM treatment conditions each received a reader comprised of practice-specific excerpts and testimonials from FCL and additional practice-specific resources excerpted from meditation manuals (see Supplementary Appendices 2 and 3, respectively). Structural equivalence was considered in terms of both the count of individual items provided for each course (i.e., number of handouts, worksheets, homework assignments, audio files, etc.) as well as the length of these class materials (i.e., length of audio files in minutes, number of words and/or pages of the worksheets, and handouts).
Course materials provided to participants in the MBCT group were based on those laid out in the Segal, Williams, et al. (2002b) and Crane (2013) manuals. In order to standardize the class materials across conditions, the MBCT handouts were modified to create a version that included only information relevant to FA and OM practices for the FA and OM groups, respectively. Where information or instructions were removed from the MBCT class materials to create the FA and OM versions, supplemental information relevant to the target practice was added, such that the FA and OM handouts were comparable in number and in length to the MBCT versions.
Meditation homework compliance
Participants were instructed to practice meditation approximately 45 minutes per day, six days per week, for a total of 2160 minutes of home practice across all eight weeks (not counting class or retreat time). Homework compliance was monitored with a daily online survey, which queried about types of both formal and informal practice, time(s) of day, duration(s), use of recordings, whether or not they fell asleep, and any other comments, questions or challenges. Treatments were compared for the total number of minutes of formal home practice and percent compliance (i.e., minutes practiced divided by 2160).
Instructor-level variables
Instructors
The instructors of each intervention were balanced for gender, expertise and consistent treatment-matching. Each treatment had one male and one female instructor. The female instructor was constant throughout all treatments to balance therapist effects, and the male instructor had a special expertise in the specific practice being offered. Because provider enthusiasm and confidence in the efficacy of the intervention is related to its degree benefits (Davidson & Kaszniak, 2015; MacCoon, et al., 2012), it was important to find instructors who were not only capable of delivering the intervention but also particularly enthusiastic about their intervention (i.e., believed their intervention was superior to the others).
All instructors had more than 20 years of meditation experience in the Theravāda or Zen traditions. Three had received MBSR instructor training at the UMASS Center for Mindfulness and two were mental health professionals trained in MBCT. The female instructor was trained in both MBSR and MBCT and had taught more than 25 8-week MBSR/CT courses, many in the context of federally funded clinical research trials. The male OM instructor was a former ordained monk in the Mahasi tradition of Theravāda Buddhism, which focuses on noting-style of vipassana. The male FA instructor was a MBSR- and DBT-trained LCMHC with more than 20 years of experience as a mental health counselor and a background of concentration practices of Theravāda Buddhism. The male MBCT instructor was a qualified MBSR instructor with 17 years of experience in the Thich Nhat Hanh style of Zen Buddhism.
Treatment ratings
At the end of treatment (week eight), participants were asked to rate the treatment on a number of factors known to impact treatment outcomes (MacNair-Semands, Ogrodniczuk, & Joyce, 2010). The Therapeutic Factors Inventory (TFI) (Lese & MacNair-Semands, 2000) is a 99-item scale designed to measure 11 therapeutic factors, put forth by Yalom and Leszcz (1995), that facilitate group therapy outcomes, including group cohesion, feelings of hope, trust, belonging, social learning and shared goals. Items on the TFI are rated using a seven-point Likert scale ranging from “strongly agree” to “strongly disagree.” The TFI total score (alpha = .98) was used to compare treatments on participant ratings of overall therapeutic experience.
The Working Alliance Inventory (WAI) (Horvath & Greenberg, 1989) is a 36 item self-report scale designed to measure aspects of the working alliance between a client, instructor and/or other group members. The scale has three subscales: tasks, goals, and bonds, which are based on Bordin’s (1979) pan-theoretical conceptualization of the therapeutic alliance. The tasks subscale assesses the extent to which the activities during sessions were perceived as relevant and efficacious, the goals subscale measures the extent to which a participant’s therapeutic goals are shared by the instructors and group members, and the bonds subscale assesses mutual trust and appreciation. Each item was rated on a seven-point Likert scale ranging from “not at all true” to “very true.” The WAI total score (alpha = .96) was used to compare treatments on participant ratings of the overall working alliance with the instructors and other group members.
The Empathy Scale (ES) (Burns & Auerbach, 1996; Persons & Burns, 1985) is a 10-item self-report questionnaire that assesses clients’ perceptions of the therapist’s warmth, genuineness, and empathy. Each item is scored on a seven-point Likert scale, with responses ranging from “strongly disagree” to “strongly agree.” The first five items are worded so that agreement indicates a positive therapeutic relationship, whereas the second five items are worded so that agreement indicates a poor therapeutic relationship. Total scores are calculated by subtracting the negatively worded items from the positively worded items. The ES total score (alpha = .89) was used to compare treatments on participant ratings of perceived instructor empathy.
Treatment adherence and fidelity
A list of 7–12 agenda items were created for each session, based on the MBCT manual and MBCT adherence scale (Segal, Teasdale, et al., 2002) and adapted for FA and OM treatments. Items were rated as “present” or “not present” (0 or 1) by 2–3 study staff who either attended the treatment as interns, and/or reviewed the session audio tapes. Percent adherence to the agenda refers to the number of items completed divided by the total. Inter-rater reliability (Cohen’s kappa) refers to the degree of agreement between the raters of adherence.
Differential Validity
Course materials
A comparative analysis of course materials (handouts, audiotapes, readers) for each arm of the trial was performed in order to evaluate differential validity across treatment conditions. Treatment materials for each condition were compiled for comparative analysis of the frequency of key terms. The treatment materials used for word count analysis were comprised of the reader (a collection of readings, class handouts and worksheets, including homework instructions) and transcriptions of the audio recordings of the meditation exercises provided for home use.
The course instructors for all treatment conditions came to consensus on key terms that should differ in frequency across the treatments. Instructors agreed that the terms “anchor” and “object,” which refer to a single point of focus during meditation, should occur more frequently in FA. For OM, the terms “note/noting,” “label,” “track,” “monitor,” “transient,” “momentary” and “fleeting” were thought to reflect the unique attributes of the meta-cognitive OM method, as well as demonstrate the greater emphasis on awareness of the impermanence of cognitive phenomena, physical sensations, and emotional reactivity.
The emphasis on acceptance was hypothesized to be greater in MBCT, though not unique to it. Lutz, et al. (2008) do not include acceptance as a characteristic of OM, but do note a non-reactive quality of OM styles of practice. In MBSR and MBCT, however, acceptance is explicitly taught and encouraged. This emphasis could be understood, by teachers as well as participants, as encouraging a deliberate change of one’s mental attitudes so as to be accepting and not reactive, specifically “by cultivating a deliberate, intentional ‘turning towards’ and ‘inviting in’ of difficulties” (Crane, 2013, p. 53). For example, in response to difficult emotions, MBCT participants are instructed to say to themselves “It’s OK. Whatever it is, it’s OK. Let me feel it” (Segal, Williams, et al., 2002a). Other researchers have described this deliberate change in the relationship to thoughts or emotions as a form of re-appraisal (Garland, Gaylord, & Park, 2009; Garland, Hanley, Farb, & Froeliger, 2015; Hanley & Garland, 2014; Hanley, Garland, & Black, 2014). In contrast, in the Mahasi tradition of OM practice, what is encouraged instead is simply an observing of physical and mental experience, including awareness of any emotional reactivity that arises from such observing. It is thought that the progressive development of intensive, precise, continuous awareness will ultimately leave no room for emotional reactivity and, moreover, will naturally result in the growth of equanimity without explicitly or intentionally cultivating it. Thus, in order to differentiate, on the one hand, the effects of participants’ non-interfering, non-manipulative, awareness from, on the other hand, the effects of participants’ direct attempts to reduce judgmental reactivity through explicitly cultivating acceptance, we were careful not to include explicit encouragement of acceptance in our presentation of OM.
Instructors also hypothesized which treatment condition should come first, second and third in terms of the frequency of use of each key term. Because MBCT is hypothetically half FA and half OM, every key term designated as occurring most often in either the FA or OM condition was anticipated to occur second-most frequently in the MBCT condition. A word search was performed to determine the frequency of each term in the class materials for each treatment condition. Every instance of each key term was counted regardless of context, as nearly all uses of the key terms for communication not relevant to the target meditative practice(s) would be identical across treatment conditions, and therefore would not impact the frequency rankings.
Mechanistic differences or skills learned
The Five Factors of Mindfulness Questionnaire (FFMQ) (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006) is a 39-item self-report instrument that measures five dimensions of mindfulness: observing, describing, acting with awareness, nonjudging and nonreactivity to inner experience. While we expected that all five facets of mindfulness would increase with all forms of training, based on Lutz et al.’s (2008) description of OM as “nonreactive meta-cognitive monitoring” or a “nonreactive awareness,” we hypothesized that nonreactivity would be maximally increased by OM training. The 7-item nonreactivity subscale (pre, post alpha = 0.76, 0.86, respectively) contains items describing psychological distance from thoughts and emotions (i.e., decentering), such as “When I have distressing thoughts or images, I ‘step back;’” “I am aware of the thought or image without getting taken over by it” and “I watch my feelings without getting lost in them,” as well as items more directly related to affective nonreactivity or nonperseveration, such as “I perceive my feelings and emotions without having to react to them.” Four items describe affective nonreactivity to thoughts or images, while two items refer to nonreactivity to emotions or feelings.
The Attention Control Questionnaire (ACQ) (Derryberry & Reed, 2002) is a 20-item scale that measures the ability to sustain attention (concentrate) and direct attention at will. In addition to the total score (pre, post, 3 month alpha = 0.84, 0.88, 0.88, respectively), this survey has two subscales. Higher total and subscale scores reflect better attentional abilities. The “focus” subscale (pre, post, 3 month alpha = 0.73, 0.78, 0.79, respectively) assesses attentional focus, or the ability to intentionally focus on desired channels (objects or tasks at hand) in a sustained way, thereby resisting unintentional shifting to distractions. A sample item is: “My concentration is good even if there is music in the room around me.” The “shift” subscale (pre, post, 3 month alpha = 0.76, 0.81, 0.81, respectively) assesses the ability to intentionally shift attention to desired channels. A sample item is: “I can quickly switch from one task to another.” ACQ scores have been found to correlate with objective measures of attentional control, which further demonstrates the scale’s reliability (Derryberry & Reed, 2002). The ACQ was used to assess differential validity, with both the “focus” and “shift” subscales hypothesized to show greater increases with FA compared to OM training.
The Mindfulness Skill Acquisition Scale (MSAS) (Britton & Shahar, Unpublished results) is a 38-item scale that was created to assess MBSR/CT skill acquisition. Reponses range from 1 (almost never) to 6 (almost always) and assess the frequency with which strategies learned in class were employed in response transient negative affect in the last week, e.g., “This week, when I encountered an unpleasant thought or feeling…” Types of strategies include avoidance, resistance, rumination (all reverse scored), cognitive reappraisal, exploration, allowing, noting/labeling and compassion. Items were drawn from other scales (Carver, Scheier, & Weintraub, 1989; Mayer & Stevens, 1994; Nolen-Hoeksema & Morrow, 1991; Salovey, Mayer, Goldman, Turvey, & Palfai, 1995; A. Wells & Davies, 1994), the MBCT manual and MBSR/CT instructor training materials. Pre- and post-treatment alpha scores of the MSAS were .71 and .90, respectively, in the current study and .83 and .93, respectively, in past (unpublished) studies of MBCT. While the validity of the MSAS has not been formally assessed, in a RCT of MBCT vs. waitlist controls (Shahar, et al., 2010), changes in MSAS scores correlated positively with changes in other mindfulness scales (e.g., Mindful Attention Awareness Scale [MAAS]: r = .59, p = .0005; ACQ: r = .48, p = .001), and the MBCT group showed a greater increase in MSAS scores than controls (F(1,43) = 26.0, p < .001, d = 1.60). MSAS scores for controls did not change significantly across the eight weeks.
In the current study, the frequency with which participants engaged in breath focus or labeling their emotions in response to transient negative affect served as confirmation of differential validity, i.e., that participants were learning and using the specific skills they had been taught in response to everyday stressors. Thus, by the end of the program, we predicted that OM participants would report a greater frequency of naming emotions (e.g., “I named the emotion over and over as long as it lasted” or “I labeled my thoughts ‘images’ or verbal ‘talk’”) and that FA participants would differentially endorse “I focused on my breathing” in response to transient negative affect.
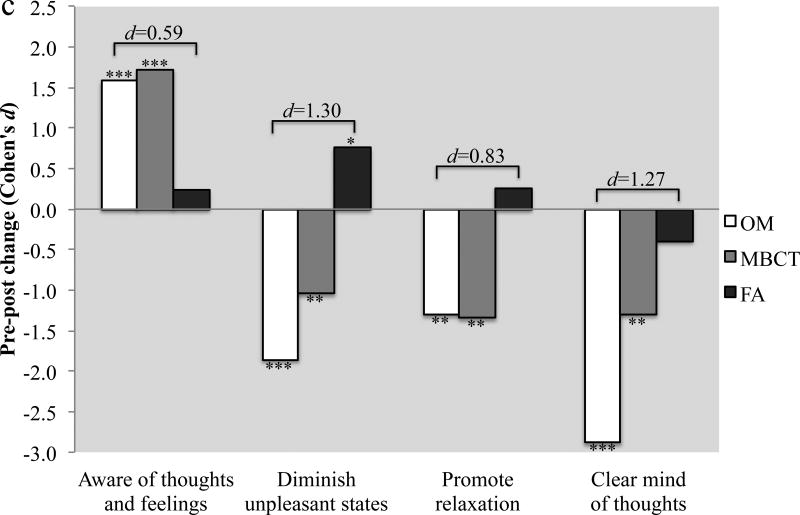
The Beliefs About Meditation Scale (BAM) (Britton & Roth, Unpublished results) is a 36-item scale that measures beliefs about the effects of meditation practices. Responses range from 1 (strongly disagree) to 7 (strongly agree). Items include questions that gauge expectations of the beneficial effects of meditation on attention and concentration, memory, depression, anxiety and physical health as well as questions about the perceived purpose(s) of meditation. We hypothesized that FA and OM training would engender different beliefs about the purpose of meditation. In line with traditional and contemporary descriptions (Lutz, et al., 2008), we predicted that FA training would engender beliefs about meditation as a method of calming the mind, promoting focus and tranquility and reducing afflictive mental states. In contrast, we predicted that OM training would reduce change-based or improvement-based orientations toward meditation, and instead emphasize an understanding of meditation as detached observation. To test these hypotheses, we used the following four BAM items: “The purpose of meditation is…” (1) “to become more aware of one's thoughts and feelings” (OM>FA); (2) “to promote relaxation” (FA>OM); (3) “to clear one's mind of thoughts” (FA>OM) and, (4) the belief that “unpleasant mental states diminish as one advances in meditation” (FA>OM).
Statistical methods
For measures of structural equivalence, where all treatments were hypothesized to be equal, a one-way ANOVA was used for continuous variables (e.g., minutes of meditation) and a chi-squared test was used for categorical variables (e.g., number of individuals who met criteria for Major Depressive Disorder). For measures of divergent validity, where specific differences between FA and OM were hypothesized, a one-way ANOVA was used with planned contrasts between FA and OM groups.
Data were analyzed using SPSS 24.0 software. Statistical significance was set at alpha levels < .05 using a two-tailed test. Effect sizes are reported as Cohen’s d and interpreted in the following manner: small = 0.20, medium = 0.50, and large = 0.80 (Cohen, 2013). Since current statistical reporting guidelines (Cumming, Fidler, Kalinowski, & Lai, 2012; Kline, 2013; Moher, et al., 2010; Wilkinson, 1999) recommend interpreting results according to effect size and not just significance testing or dichotomous p-value cut-offs, non-significant (p ≥ .05) differences with an effect size of d > 0.20 are interpreted and discussed as meaningful.
Results
Participant flow
A total of 104 participants were cluster randomized in nine groups to one of three treatments. Each group had an average of 11.5 participants with a range of 10–13. A total of eight participants dropped from the study after randomization: one from FA, two from MBCT and five from OM. Two participants, both in OM, dropped before attending the first class, two after class two (both MBCT), three after class three (all OM) and one after class seven (FA). Reasons given for attrition included scheduling conflicts with work (n=2, MBCT); time commitment (n=2, OM); lack of desire to be in a research study (n=1, OM); lack of commitment to practice (n=1, FA); increased stress due to the study (n=1, OM) and moving away (n=1, OM). See Fig. 1 for the flow diagram.
Fig. 1.
CONSORT flow diagram. FA = Focused Attention; MBCT = Mindfulness-Based Cognitive Therapy; OM = Open Monitoring.
Participant-level outcomes
Sample characteristics, including age, gender, race and baseline levels of psychopathology were matched across treatments (see Table 1). The sample exhibited mild to severe depression symptoms with IDS scores (mean 23.2 ± 7.3) ranging from 11 to 39. Approximately 40% met criteria for Major Depressive Disorder (MDD), and 50% met criteria for Generalized Anxiety Disorder (GAD). The vast majority of the sample had either clinical or subclinical levels of GAD or MDD at the time of enrollment (85.6%), or in the past (93.3%). Approximately one-third were taking antidepressant medication.
Table 1.
Sample characteristics
| FA | MBCT | OM | Total | p value | |
|---|---|---|---|---|---|
| Female, n (%) | 27 (75.0%) | 23 (71.9%) | 26 (72.2%) | 76 (73.1%) | .949 |
| Race, n (%) | .315 | ||||
| Asian | 0 (0.0%) | 1 (3.2%) | 0 (0.0%) | 1 (1.0%) | |
| White | 36 (100.0%) | 30 (96.8%) | 35 (100.0%) | 101 (99.0%) | |
| Ethnicity, n (%) | .371 | ||||
| Hispanic/Latino | 1 (2.8%) | 2 (6.5%) | 4 (11.1%) | 7 (6.8%) | |
| Not Hispanic/Latino | 35 (97.2%) | 29 (93.5%) | 32 (88.9%) | 96 (93.2%) | |
| Age, mean (SD) | 42.1 (12.8) | 38.6 (12.4) | 40.0 (13.2) | 40.3 (12.8) | .534 |
| Highest level of education, n (%) | .204 | ||||
| High school | 0 (0.0%) | 2 (6.3%) | 1 (2.8%) | 3 (2.9%) | |
| College | 22 (61.1%) | 18 (56.3%) | 16 (44.4%) | 56 (53.8%) | |
| Master’s | 12 (33.3%) | 7 (21.9%) | 10 (27.8%) | 29 (27.9%) | |
| MD or PhD | 2 (5.6%) | 5 (15.6%) | 9 (25.0%) | 16 (15.4%) | |
| AD meds, n (%) | 11 (30.6%) | 12 (37.5%) | 12 (33.3%) | 35 (33.7%) | .832 |
| Baseline IDS, mean (SD) | 22.8 (7.6) | 23.4 (7.3) | 23.4 (7.2) | 23.2 (7.3) | .917 |
| Axis I Diagnoses, n (%) | |||||
| Current clinical MDD | 14 (38.9%) | 12 (37.5%) | 15 (41.7%) | 41 (39.4%) | .937 |
| Current (sub)clinical MDD | 23 (63.9%) | 20 (62.5%) | 22 (61.1%) | 65 (62.5%) | .971 |
| Current/past (sub)clinical MDD | 31 (86.1%) | 28 (87.5%) | 32 (88.9%) | 91 (87.5%) | .938 |
| Current clinical GAD | 20 (55.6%) | 14 (43.8%) | 18 (50.0%) | 52 (50.0%) | .624 |
| Current (sub)clinical GAD | 22 (61.1%) | 18 (56.3%) | 24 (66.7%) | 64 (61.5%) | .677 |
| Current/past (sub)clinical GAD | 25 (69.4%) | 21 (65.6%) | 25 (69.4%) | 71 (68.3%) | .928 |
| Current subclinical PTSD | 6 (16.7%) | 5 (15.6%) | 4 (11.1%) | 15 (14.4%) | .777 |
| Current/past (sub)clinical PTSD | 10 (27.8%) | 8 (25.0%) | 14 (38.9%) | 32 (30.8%) | .414 |
Note. AD meds = Antidepressant medication; IDS = Inventory of Depressive Symptomatology; MDD = Major Depressive Disorder; GAD = Generalized Anxiety Disorder; PTSD = Post-traumatic Stress Disorder
Treatment-level outcomes
All three interventions were matched for duration, format and content (see Table 2). Analysis of the course materials (including minutes of meditation audio recordings provided, number of meditations assigned and number of pages/words for handouts) verified structural equivalence across the three treatment conditions with respect to all course materials with the exception of the reader (see Table 3).
Table 2.
Course structure
| FA | MBCT | OM | Total | p value | |
|---|---|---|---|---|---|
| Course Structure | |||||
| Number of sessions | 9 | 9 | 9 | 9 | n/a |
| Total contact hours | 30 | 30 | 30 | 30 | n/a |
| # Groups | 3 | 3 | 3 | 9 | n/a |
| # Per group (range) | 12 (12) | 10.7 (10–11) | 12 (10–13) | 11.6 (10–13) | n/a |
| Attendance and Attrition | |||||
| Total randomized, n | 36 | 32 | 36 | 104 | n/a |
| Dropped out, n (%)a | 1 (2.8%) | 2 (6.3%) | 3 (8.8%) | 6 (5.9%) | .558 |
| Completed intervention, n (%)b | 35 (97.2%) | 30 (93.8%) | 31 (91.2%) | 96 (94.1%) | .558 |
| Classes attended, mean (SD)b | 8.1 (1.3) | 7.7 (1.8) | 7.7 (1.8) | 7.8 (1.6) | .368 |
| Attended retreat, n (%)b | 33 (91.7%) | 26 (81.3%) | 28 (82.4%) | 87 (85.3%) | .403 |
| % Attendance, mean (SD)b | 90.3% (14.0) | 85.1% (19.8) | 84.6% (19.4) | 86.8% (17.8) | .341 |
| Meditation Homework Compliance | |||||
| 8wk % Compliance, mean (SD)b | 76.1% (24.4) | 68.6% (30.6) | 80.0% (26.7) | 75.0% (27.3) | .256 |
| 8wk formal min/wk, mean (SD)b | 205.6 (65.9) | 185.2 (82.6) | 215.9 (72.2) | 202.6 (73.7) | .256 |
| 3mo formal min/wk, mean (SD)b | 100.0 (96.6) | 97.8 (97.2) | 104.2 (106.9) | 100.7 (99.2) | .969 |
Note. % Compliance = number of formal minutes of practice reported divided by total number of minutes assigned as homework; 8wk = during 8-week intervention; 3mo = between 8-week intervention and 3-month follow-up
Drop-outs only include participants who began treatment (i.e., attended the first class). Two additional participants dropped from OM before the beginning of treatment.
These variables only include participants who completed all 8 weeks of treatment (FA, MBCT, OM n’s = 35, 30, 31, respectively).
Table 3.
Course materials
| FA | MBCT | OM | |
|---|---|---|---|
| Reader total number of words | 28,000 | 182,078 | 33,251 |
| Reader total number of pages | 61 | 304 | 78 |
| Total number of handouts | 53 | 58 | 56 |
| Handout total number of pages | 145 | 159 | 157 |
| Handouts total number of words | 29,668 | 32,586 | 29,030 |
| Total number of meditations | 14 | 17 | 13 |
| Combined audio minutes | 313 | 418 | 249 |
Instructor-level outcomes
Instructor-level outcomes, including instructor qualities (gender ratio, credentials and prior years of meditation experience), treatment adherence and participants’ ratings of the overall therapeutic experience (TFI) were matched among the three treatments (see Table 4). However, FA demonstrated higher scores of both perceived instructor empathy (ES) and overall working alliance with the instructors and other group members (WAI; see Table 4).
Table 4.
Instructor-level outcomes
| FA | MBCT | OM | p value | |
|---|---|---|---|---|
| Instructor qualities | ||||
| Instructor gender ratio (male: female) | 1:1 | 1:1 | 1:1 | n/a |
| Combined years of meditation experience | 40 | 40 | 40 | n/a |
| # Clinical degrees | 2 | 1 | 1 | n/a |
| # Ph.D.’s | 1 | 2 | 2 | n/a |
| Treatment adherence and fidelity | ||||
| Agenda items per session, mean (range) | 10.3 (8–12) | 8.4 (7–11) | 9.5 (7–11) | n/a |
| Total agenda items (all sessions) | 83 | 67 | 76 | n/a |
| Treatment adherence | 97.1% | 93.9% | 88.9% | n/a |
| Cohen’s kappa | 0.66 | 0.73 | 0.73 | n/a |
| Treatment/Instructor ratings | ||||
| TFI total, mean (SD) | 502.0 (78.0) | 470.2 (79.4) | 463.5 (90.4) | .131 |
| ES total, mean (SD) | 65.9 (5.6) | 61.3 (9.2) | 59.9 (10.2) | .012* |
| WAI total, mean (SD) | 233.2 (32.6) | 210.1 (34.0) | 207.6 (37.0) | .005** |
Note. TFI = Therapeutic Factors Inventory; ES = Therapist Empathy Scale; WAI = Working Alliance Inventory
p < .05.
p < .01.
Differential Validity
Treatment materials
Differential validity was assessed by the comparative frequency of key terms across the three treatment conditions. The actual frequency of key terms in each condition was evaluated in terms of the key term frequency rankings agreed upon by the instructors in order to ascertain how closely the treatment materials adhered to the study design. As Table 5 indicates, the key terms differentiated the course materials across conditions, with frequency of key terms predominantly ranking in the expected order.
Table 5.
Frequency of key terms by treatment
| Key Term | Hypothesized order | Handouts | Reader | Audio files | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| FA | MBCT | OM | FA | MBCT | OM | FA | MBCT | OM | ||
| anchor | FA>MBCT>OM | 109a | 5 | 0 | 22 | 13 | 2 | 134 | 22 | 0 |
| object | FA>MBCT>OM | 5 | 2 | 3 | 51 | 25 | 8 | 6 | 4 | 0 |
| note/noting | OM>MBCT>FA | 14 | 15 | 37 | 16 | 26 | 71 | 1 | 22 | 31 |
| label | OM>MBCT>FA | 3 | 4 | 39 | 0 | 13 | 16 | 0 | 3 | 41 |
| transient, fleeting momentary | OM>MBCT>FA | 2 | 6 | 8 | 2 | 5 | 7 | 1 | 4 | 2 |
| track, monitor | OM>MBCT>FA | 6 | 10 | 13 | 3 | 15 | 6 | 0 | 0 | 3 |
| accept/acceptance | MBCT>FA, OM | 16 | 45 | 22 | 6 | 124 | 22 | 1 | 7 | 2 |
Bold text indicates that frequency of key terms ranks in expected order.
Participant skills acquisition
Participants acquired the specific skills they were taught as predicted. Specifically, participants who received OM reported increased frequencies of naming emotions (OM pre-post: F(1,28) = 12.02, p = .002, d = 1.31) and labeling thoughts as “images” or verbal “talk” (OM pre-post: F(1,28) = 58.00, p < .001, d = 2.88) in response to transient negative affect compared to participants randomized to FA (naming emotions: FA pre-post: F(1,33) = 0.051, p = 0.822, d = 0.09; FA-OM contrast: t(90) = 2.29, p = .024, d = 0.60; labeling thoughts: FA pre-post: F(1,33) = 16.78, p < .001, d = 1.43; FA-OM contrast: t(90) = 2.11, p = .038, d = 0.59; see Fig. 2a). All three treatments showed large increases on the FFMQ nonreactivity scale. As predicted, OM showed the greatest magnitude of change (F(1,29) = 38.35, p < .001, d = 2.30) and FA the smallest (F(1,33) = 11.54, p = .002, d = 1.18), although the FA-OM contrast did not reach significance (t(91) = 1.43, p = 0.157, d = 0.33).
Fig. 2.
The acquisition of cognitive and affective skills and beliefs about meditation following the 8-weeks intervention for all three treatments. The Y axes (bar height) represent the degree of skill/belief acquisition from pre- to post-treatment in Cohen’s d effect size units. The magnitude of difference in skill/belief acquisition between FA and OM treatments is represented by a separate set of Cohen’s d effect sizes on top of each set of bars. (a) Skills for which OM participants demonstrated greater increases than FA participants (b) Skills for which FA participants demonstrated greater increases than OM participants (c) Changes in beliefs about meditation that reflected divergence between FA and OM groups.
* p < .05, ** p < .01, *** p < .001
As predicted, participants who received FA were more likely than OM participants to focus on their breath in response to transient negative affect, although OM participants also showed a significant and large increase in negative emotion-induced breath awareness after OM training (FA pre-post: F(1,33) = 89.04, p < .001, d = 3.29; OM pre-post: F(1,28) = 27.78, p < .001, d = 1.99; FA-OM contrast: t(90) = 2.98, p = .004, d = 0.75; see Fig. 2b). The FA group also showed larger increases than OM in both attentional focus (FA pre-post: F(1,33) = 31.92, p < .001, d = 1.97; OM pre-post: F(1,29) = 9.78, p = .004, d = 1.16) and attentional shifting (FA pre-post: F(1,33) = 30.94, p < .001, d = 1.94; OM pre-post: F(1,29) = 4.28, p = .048, d = 0.77), although neither FA-OM contrast reached statistical significance (Focus: t(91) = 1.63, p = .107, d = 0.40; Shift: t(91) = 1.34, p = .185, d = 0.36; see Fig. 2b).
In terms of beliefs about the purpose or goal of meditation, OM participants were more likely to orient towards meditation as a method of becoming “more aware of one’s thoughts and feelings,” (OM pre-post: F(1,29) = 18.08, p < .001, d = 1.58; FA pre-post: F(1,33) = 0.46, p = .502, d = 0.24; FA-OM contrast: t(91) = 2.50, p = .014, d = 0.59) while FA participants were more likely to retain the belief that meditation is a method for “clearing one’s mind” of thoughts (FA pre-post: F(1,33) = −1.27, p = .267, d = −0.39; OM pre-post: F(1,29) =−60.26, p < .001, d = −2.88; FA-OM contrast: t(91) = −5.16, p < 0.001, d = 1.27) and “promoting relaxation” (FA pre-post: F(1,33) = 0.57, p = .454, d = 0.26; OM pre-post: F(1,29) = −12.25, p = .002, d = −1.30; FA-OM contrast: t(91) = −3.23, p = .002, d = 0.83; see Fig. 2c). In addition, participants in FA were more likely to believe after training that “unpleasant mental states diminish as one advances in meditation" whereas OM participants were less likely to endorse this statement after training (FA pre-post: F(1,33) = 4.71, p = .037, d = 0.76; OM pre-post: F(1,29) = −25.05, p < .001, d = −1.86; FA-OM contrast: t(91) = −5.16, p < 0.001, d = 1.30; see Fig. 2c).
Discussion
The overarching purpose of this dismantling study was to test the purported mechanistic target engagement of two separate MBI components by isolating and comparing focused attention and open monitoring practices. The current paper describes the creation and validation of 8-week FA and OM programs that are both structurally equivalent to MBCT and also differentially valid single-ingredient programs. The results indicate that we successfully created FA and OM programs that were structurally equivalent to each other as well as to standard MBCT in terms of participant-level variables (demographics and clinical diagnoses), treatment-level variables (program structure and duration, program materials, class size, attendance/attrition, homework compliance, etc.) and instructor-level variables (training, ratings and adherence/fidelity).
The study also succeeded in creating treatments that were differentially valid. That is, the treatments differed in terms of program materials (handouts, audiotapes and readers) and differential target engagement (skills acquired) as predicted by a priori hypotheses. FA program materials had more references to targets, objects or anchors of directed attention, while OM materials emphasized tracking, noting or labeling transient stimuli. In terms of skills acquired, OM participants were more likely to use affect and thought labeling to cope with transient negative affect, while FA participants were more likely to use breath focus when distressed. Similarly, OM training resulted in the greatest increase in nonreactivity, while FA training resulted in the largest increases in attentional control. In addition to mindfulness-related skills, FA and OM training also led to differential beliefs about the purpose and consequences of meditation. OM participants were more likely to believe that meditation is a method of becoming more aware of one’s thoughts and emotions without any expectation of reducing unpleasant mental states. In contrast, FA participants were more likely to believe that meditation reduces negative mental states and increases positive ones. It is interesting to note that with the exception of beliefs about the effects of meditation on improving distress, FA training did not alter participants’ beliefs about meditation from their pre-existing levels. In contrast, OM training produced significant decreases in a number of pre-existing beliefs, suggesting that OM training is disabusing participants of their beliefs about meditation. Together, these results suggest that FA largely conforms to pre-existing expectations, while OM is somewhat counterintuitive. This has implications for dissemination, as according to the NIH stage model, the best interventions are ones that can be the most easily implemented in real-world settings (Onken, Carroll, Shoham, Cuthbert, & Riddle, 2014), that is, when all else is equal, interventions that are simple, intuitive and easy to learn and teach.
While the study revealed that FA and OM differed from each other, they also displayed substantial overlap and parallel mechanisms. For example, both programs showed significant pre-post increases in affective non-reactivity and attentional control, two mechanisms that were hypothesized to be uniquely engaged by OM and FA respectively. Similarly, both FA and OM participants increased in their frequency of labeling their thoughts (a hypothesized OM-specific skill) or focusing on their breath (a hypothesized FA-specific skill) in response to negative affect. Thus, it will be important to test whether the efficacy of each program is mediated through similar or different mechanisms.
Study Limitations and Recommendations for Future Research
All three programs were structurally equivalent on nearly all measures, including class content and format. One exception was the supplementary reading materials. The MBCT group received a copy of Full Catastrophe of Living (FCL) (Jon Kabat-Zinn, 1990), which is over 300 pages. The FA and OM readers contained excerpts from FCL, including many of the testimonials, and were equal in length to each other but were significantly shorter than FCL. Because supplemental reading compliance was not assessed, it is unknown whether the difference in reader lengths actually manifested. Since FCL is a standard part of most MBIs, and could potentially represent a significant time commitment and a kind of “bibliotherapy” treatment of its own, future studies may want to assess both participant compliance and its impact on outcomes.
Instructor ratings were another exception to structural equivalence in that the FA instructors received more favorable ratings with respect to perceived instructor empathy and working alliance. These more positive instructor ratings for FA could be related to the fact that the FA-specific instructor was the only full-time clinician and thus had more clinical experience than the OM- and MBCT-specific instructors, though it is unclear what impact this could have had on treatment outcomes. For example, while there is some evidence that instructor qualities such as empathy and therapeutic relationship are related to more favorable outcomes (Norcross & Wampold, 2011), there is a less conclusive relationship between outcomes and instructors’ clinical experience or competence in teaching mindfulness (Huijbers, et al., 2017; Mason, Grey, & Veale, 2016). Future analyses of the current study will assess the contribution of specific instructor qualities to changes in depression, anxiety, stress and well-being. Future intervention studies should similarly assess participants’ ratings of the instructors in order to further differentiate the clinical impact of intervention practices themselves from participant-instructor relationships.
Other limitations of the current study include the choice of control group and the limited sample size. The choice of control group is both a strength and limitation. We chose MBCT rather than a passive control because we were following Jacobson et al.’s (1996) dismantling design, and it will be important in future analyses to be able to assess how FA and OM compare to MBCT in terms of clinical outcomes. However, the lack of a no-treatment or even a non-meditation control group leaves open the possibility that all pre-post changes could be due to non-specific effects, such as the passage of time and social support, rather than meditation. However, because the general efficacy of MBIs has already been established in studies with appropriate designs, the focus of the current study was to create programs that could assess the differences between different practices. Future studies that employ these new FA and OM programs are encouraged to employ appropriate control groups.
Another limitation is limited power and small sample size. Effect sizes of FA vs. OM contrasts ranged from medium to large (d =.33 – 1.30), but not all reached statistical significance due to lack of power. Since differences between active treatments tend to be small (Wampold, et al., 1997), a larger sample would have been able to detect smaller differences.
The study design has implications related to generalizability. With more than 20 years of personal meditation experience and advanced, graduate level clinical, research and/or monastic training, it is likely that the instructors in the current trial were more qualified than many MBI instructors. Since it is unclear whether MBI instructor training has an impact on participant outcomes (Brefczynski-Lewis, et al., 2007), this difference is of unknown significance.
The sample is representative for estimating effects in people who choose to engage in meditation, but not for people who are not seeking meditation (i.e., are randomly assigned to a treatment condition without prior knowledge). Thus, the results likely do generalize to meditators in the U.S., but not to subjects in randomized controlled trials. Similarly, although the sample was aimed at representing the average American meditator and included individuals with mild to severe anxiety and depression, people with other serious mental illnesses were excluded according to standard MBSR/CT exclusion criteria (Kuyken, Crane, & Williams, 2012; Santorelli, 2014). Thus, although the results most likely generalize to standard MBSR/CT samples, results would not extend to other clinical samples.
From an experimental medicine perspective, this study addresses one dimension of a mechanism-focused approach, namely verifying that different components of MBIs engage (some assays of) the targets they are purported to. As such, the study provides a useful research tool for mindfulness researchers to investigate the next component of the SOBC framework: whether engagement of one or both targets actually leads to meaningful behavior change or clinical endpoints. Verification of target engagement with different assays of attention control and emotional non-reactivity, including behavioral, neuroimaging and peripheral biological assays, will promote cross-validation of reliable target engagement.
Mindfulness research in general could benefit from employing the SOBC experimental medicine approach. While many mechanism of mindfulness have been hypothesized (Holzel, et al., 2011; Shapiro, Carlson, Astin, & Freedman, 2006; Vago & Silbersweig, 2012; van der Velden & Roepstorff, 2015), very few of these mechanisms have been tested or verified (Gu, et al., 2015). As a result, little is known about how MBIs work or how they should be modified to maximize effectiveness (Dimidjian & Segal, 2015; Gu, et al., 2015). The SOBC experimental medicine approach will not only help MBIs become maximally effective, but also provide essential mechanistic information that will help tailor the intervention and instructor training to specific populations and conditions.
Conclusion
This study employed the mechanism-focused SOBC experimental medicine approach to identify active ingredients of MBIs by testing the purported mechanistic target engagement of two separate MBI components. The current 3-armed dismantling study created two separate 8-week focused attention meditation and open monitoring meditation training programs that are structurally equivalent to MBCT but differentially engage mechanistic targets as predicted by both Buddhist and scientific frameworks. Specifically, FA practice engaged mechanistic targets related to attention control, while OM practice engaged mechanistic targets related to emotional non-reactivity. By delineating MBIs into their separate practices and creating separate, validated, single-ingredient training programs for each practice, the current project provides researchers with a tool to test the individual contributions of each component and mechanism to clinical endpoints. Using evidence-based information about practice-specific mechanisms, clinicians, educators and meditation teachers could begin to tailor meditation practice regimens to meet specific and unique needs and goals of different individuals, groups or conditions (i.e., a personalized medicine approach).
Supplementary Material
Supplementary Appendix 1 Session × Session Comparison Table.
Supplementary Appendix 2 Example FA program materials.
Supplementary Appendix 3 Example OM program materials.
Highlights.
3-armed RCT that isolates focused attention (FA) and open monitoring (OM) practices
Separate 8-week FA and OM programs were created and validated
FA and OM are structurally equivalent to Mindfulness-Based Cognitive Therapy (MBCT)
As expected, FA engages mechanistic targets related to attention control while OM engages mechanistic target related to emotional non-reactivity
Post-training, FA and OM exhibit divergent beliefs about the goals of meditation
Acknowledgments
Funding
This work was supported by the National Institutes of Health (grant K23-AT006328-01A1); the National Institutes of Health (NIH) Science of Behavior Change Common Fund Program through an award administered by the National Center for Complementary and Integrative Health (grant UH2AT009145); the Mind and Life Institute; and the Brown University Contemplative Studies Initiative. The views presented here are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
We would like to thank the Clinical and Affective Neuroscience Laboratory at Brown University.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Ethical standards
The study was approved by the appropriate ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants gave informed consent prior to their inclusion in the study.
Conflict of Interest
The authors declare no conflict of interest.
Registration number and name of trial registry: clinicaltrials.gov NCT#: 01831362
References
- Ainsworth B, Eddershaw R, Meron D, Baldwin DS, Garner M. The effect of focused attention and open monitoring meditation on attention network function in healthy volunteers. Psychiatry research. 2013;210:1226–1231. doi: 10.1016/j.psychres.2013.09.002. [DOI] [PubMed] [Google Scholar]
- Arch JJ, Craske MG. Mechanisms of mindfulness: Emotion regulation following a focused breathing induction. Behaviour research and therapy. 2006;44:1849–1858. doi: 10.1016/j.brat.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Barnes P, Bloom B, Nahin R. Complementary and Alternative Medicine Use Among Children and Adults: United States, 2007. CDC National Health Statisitics Report #12. 2008:1–24. [PubMed] [Google Scholar]
- Barnhofer T, Crane C, Hargus E, Amarasinghe M, Winder R, Williams JM. Mindfulness-based cognitive therapy as a treatment for chronic depression: A preliminary study. Behav Res Ther. 2009;47:366–373. doi: 10.1016/j.brat.2009.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Segal Z, Abbey S, Speca M, Velting D, Devins G. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice. 2004;11:230–241. [Google Scholar]
- Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, research & practice. 1979;16:252. [Google Scholar]
- Brake CA, Sauer-Zavala S, Boswell JF, Gallagher MW, Farchione TJ, Barlow DH. Mindfulness-Based Exposure Strategies as a Transdiagnostic Mechanism of Change: An Exploratory Alternating Treatment Design. Behav Ther. 2016;47:225–238. doi: 10.1016/j.beth.2015.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brefczynski-Lewis JA, Lutz A, Schaefer HS, Levinson DB, Davidson RJ. Neural correlates of attentional expertise in long-term meditation practitioners. Proceedings of the national Academy of Sciences. 2007;104 doi: 10.1073/pnas.0606552104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton WB, Haynes PL, Fridel KW, Bootzin RR. Polysomnographic and subjective profiles of sleep continuity before and after mindfulness-based cognitive therapy in partially remitted depression. Psychosomatic Medicine. 2010;72:539–554. doi: 10.1097/PSY.0b013e3181dc1bad. [DOI] [PubMed] [Google Scholar]
- Britton WB, Roth HD. Beliefs About Meditation Scale (Unpublished results) [Google Scholar]
- Britton WB, Shahar B. Mindfulness Skills Acquisition Scale (Unpublished results) [Google Scholar]
- Buddhaghosa . The path of purification: Visuddhimagga. Berkeley, Calif.: Shambhala Publications : Distributed in the United States by Random House; 1976. [Google Scholar]
- Burns DD, Auerbach A. Frontiers of cognitive therapy. New York, NY, US: Guilford Press; 1996. Therapeutic empathy in cognitive-behavioral therapy: Does it really make a difference? pp. 135–164. [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Chaikin AL, Derlega VJ, Miller SJ. Effects of room environment on self-disclosure in a counseling analogue. Journal of Counseling Psychology. 1976;23:479. [Google Scholar]
- Cohen BH. Explaining psychological statistics. Fourth. Hoboken, NJ: John Wiley & Sons; 2013. [Google Scholar]
- Colzato LS, Szapora A, Hommel B. Meditate to create: the impact of focused-attention and open-monitoring training on convergent and divergent thinking. Frontiers in psychology. 2012;3 doi: 10.3389/fpsyg.2012.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane R. Mindfulness-based cognitive therapy: Distinctive features 2013 [Google Scholar]
- Cuijpers P, Beekman A, Smit F, Deeg D. Predicting the onset of major depressive disorder and dysthymia in older adults with subthreshold depression: a community based study. Int J Geriatr Psychiatry. 2006;21:811–818. doi: 10.1002/gps.1565. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, de Graaf R, van Dorsselaer S. Minor depression: risk profiles, functional disability, health care use and risk of developing major depression. J Affect Disord. 2004;79:71–79. doi: 10.1016/S0165-0327(02)00348-8. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Smit F. Subthreshold depression as a risk indicator for major depressive disorder: a systematic review of prospective studies. Acta Psychiatr Scand. 2004;109:325–331. doi: 10.1111/j.1600-0447.2004.00301.x. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Smit F, Oostenbrink J, de Graaf R, ten Have M, Beekman A. Economic costs of minor depression: a population-based study. Acta Psychiatrica Scandinavica. 2006;115:229–236. doi: 10.1111/j.1600-0447.2006.00851.x. [DOI] [PubMed] [Google Scholar]
- Cumming G, Fidler F, Kalinowski P, Lai J. The statistical recommendations of the American psychological association publication manual: Effect sizes, confidence intervals, and meta-analysis. Australian Journal of Psychology. 2012;64 [Google Scholar]
- Das-Munshi J, Goldberg D, Bebbington PE, Bhugra DK, Brugha TS, Dewey ME, Jenkins R, Stewart R, Prince M. Public health significance of mixed anxiety and depression: beyond current classification. Br J Psychiatry. 2008;192:171–177. doi: 10.1192/bjp.bp.107.036707. [DOI] [PubMed] [Google Scholar]
- Davidson RJ. Empirical explorations of mindfulness: Conceptual and methodological conundrums. Emotion. 2010 doi: 10.1037/a0018480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ, Dahl CJ. Varieties of Contemplative Practice. JAMA Psychiatry. 2017;74:121–123. doi: 10.1001/jamapsychiatry.2016.3469. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Kaszniak AW. Conceptual and methodological issues in research on mindfulness and meditation. American Psychologist. 2015;70 doi: 10.1037/a0039512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derryberry D, Reed MA. Anxiety-related attentional biases and their regulation by attentional control. Journal of abnormal psychology. 2002;111 doi: 10.1037//0021-843x.111.2.225. [DOI] [PubMed] [Google Scholar]
- Dickenson J, Berkman ET, Arch J, Lieberman MD. Neural correlates of focused attention during a brief mindfulness induction. Social cognitive and affective neuroscience. 2013;8:40–47. doi: 10.1093/scan/nss030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon DG, Pizzagalli DA. Inhibition of Action, Thought, and Emotion: A Selective Neurobiological Review. Appl Prev Psychol. 2007;12:99–114. doi: 10.1016/j.appsy.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, Segal Z. Prospects for a clinical science of mindfulness-based intervention. Am Psychol. 2015;70:593–620. doi: 10.1037/a0039589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisendrath SJ, Delucchi K, Bitner R, Fenimore P, Smit M, McLane M. Mindfulness-based cognitive therapy for treatment-resistant depression: a pilot study. Psychotherapy and Psychosomatics. 2008;77:319–320. doi: 10.1159/000142525. [DOI] [PubMed] [Google Scholar]
- Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2005;6:67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- Fan J, McCandliss BD, Sommer T, Raz A, Posner MI. Testing the efficiency and independence of attentional networks. Journal of Cognitive Neuroscience. 2002;14:340–347. doi: 10.1162/089892902317361886. [DOI] [PubMed] [Google Scholar]
- Fan J, Raz A, Posner M. Attentional Mechanisms. In: Aminoff M, Daroff R, editors. Encyclopedia of Neurological Sciences. New York: Elsevier; 2003. pp. 292–299. [Google Scholar]
- Finucane A, Mercer SW. An exploratory mixed methods study of the acceptability and effectiveness of Mindfulness-Based Cognitive Therapy for patients with active depression and anxiety in primary care. BMC Psychiatry. 2006;6:14. doi: 10.1186/1471-244X-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F, Talajic M. The impact of negative emotions on prognosis following myocardial infarction: is it more than depression? Health Psychol. 1995;14:388–398. doi: 10.1037//0278-6133.14.5.388. [DOI] [PubMed] [Google Scholar]
- Garland EL, Gaylord S, Park J. The role of mindfulness in positive reappraisal. Explore (NY) 2009;5:37–44. doi: 10.1016/j.explore.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Hanley A, Farb NA, Froeliger BE. State Mindfulness During Meditation Predicts Enhanced Cognitive Reappraisal. Mindfulness (N Y) 2015;6:234–242. doi: 10.1007/s12671-013-0250-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein J. One Dharma: The emerging Western Buddhism. San Francisco: 2002. [Google Scholar]
- Gotlib IH, Lewinsohn PM, Seeley JR. Symptoms versus a diagnosis of depression: differences in psychosocial functioning. J Consult Clin Psychol. 1995;63:90–100. doi: 10.1037//0022-006x.63.1.90. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. Journal of Psychosomatic Research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Grubin D. Healing and the Mind with Bill Moyers. New York: Ambrose Video Publishing; 1993. Healing from Within. [Google Scholar]
- Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev. 2015;37:1–12. doi: 10.1016/j.cpr.2015.01.006. [DOI] [PubMed] [Google Scholar]
- Hanley AW, Garland EL. Dispositional Mindfulness Co-varies with Self-Reported Positive Reappraisal. Pers Individ Dif. 2014;66:146–152. doi: 10.1016/j.paid.2014.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanley AW, Garland EL, Black DS. Use of mindful reappraisal coping among meditation practitioners. J Clin Psychol. 2014;70:294–301. doi: 10.1002/jclp.22023. [DOI] [PubMed] [Google Scholar]
- Hasenkamp W, Barsalou LW. Effects of meditation experience on functional connectivity of distributed brain networks. Frontiers in human neuroscience. 2012;6 doi: 10.3389/fnhum.2012.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasenkamp W, Wilson-Mendenhall CD, Duncan E, Barsalou LW. Mind wandering and attention during focused meditation: a fine-grained temporal analysis of fluctuating cognitive states. Neuroimage. 2012;59:750–760. doi: 10.1016/j.neuroimage.2011.07.008. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzel BK, Lazar S, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspectives on Psychological Science. 2011;8:537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36:223–233. [Google Scholar]
- Huijbers M, Crane R, Kuyken, Heijke L, van den Hout I, Donders A, Speckens A. Teacher Competence in Mindfulness-Based Cognitive Therapy for Depression and Its Relation to Treatment Outcome. Mindfulness (N Y): 2017. Jan 12 online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob K. Confirmatory factor analysis of common mental disorders. In: Goldberg D, Kendler P, Sirovatka P, Regier D, editors. Diagnostic Issues in Depression and Generalized Anxiety Disorder: Refining the Research Agenda for DSM-V. Arlington, VA: American Psychiatric Association; (in press) [Google Scholar]
- Jacobson NS, Dobson KS, Traux PA, Addis ME, Koerner K, Gollan JK, Gortner E, Prince SE. A component analysis of cognitive-behavioral treatment for depression. Journal of consulting and clinical psychology. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General hospital psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delta: 1990. [Google Scholar]
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, Pbert L, Lenderking WR, Santorelli SF. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149:936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- Kenny MA, Williams JM. Treatment-resistant depressed patients show a good response to Mindfulness-based Cognitive Therapy. Behav Res Ther. 2007;45:617–625. doi: 10.1016/j.brat.2006.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury B, Sharma M, Rush SE, Fournier C. Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J Psychosom Res. 2015;78:519–528. doi: 10.1016/j.jpsychores.2015.03.009. [DOI] [PubMed] [Google Scholar]
- Kingston T, Dooley B, Bates A, Lawlor E, Malone K. Mindfulness-based cognitive therapy for residual depressive symptoms. Psychol Psychother. 2007;80:193–203. doi: 10.1348/147608306X116016. [DOI] [PubMed] [Google Scholar]
- Kline RB. Beyond significance testing: Statistics reform in the behavioral sciences 2013 [Google Scholar]
- Kok BE, Singer T. Effects of Contemplative Dyads on Engagement and Perceived Social Connectedness Over 9 Months of Mental Training: A Randomized Clinical Trial. JAMA Psychiatry. 2017;74:126–134. doi: 10.1001/jamapsychiatry.2016.3360. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. J Abnorm Psychol. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. J Abnorm Psychol. 2003;112:437–447. doi: 10.1037/0021-843x.112.3.437. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Crane W, Williams JM. In: Mindfulness-Based Cognitive Therapy (MBCT) Implementation Resources. U. o. E. Oxford University, Bangor University, editor. 2012. [Google Scholar]
- Lee TM, Leung MK, Hou WK, Tang JC, Yin J, So KF, Lee CF, Chan CC. Distinct neural activity associated with focused-attention meditation and loving-kindness meditation. PLoS One. 2012;7:e40054. doi: 10.1371/journal.pone.0040054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengacher CA, Johnson-Mallard V, Post-White J, Moscoso MS, Jacobsen PB, Klein TW, Widen RH, Fitzgerald SG, Shelton MM, Barta M, Goodman M, Cox CE, Kip KE. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology. 2009;18:1261–1272. doi: 10.1002/pon.1529. [DOI] [PubMed] [Google Scholar]
- Lese KP, MacNair-Semands RR. The therapeutic factors inventory: development of a scale. Group. 2000;24:303–317. [Google Scholar]
- Li W, Howard MO, Garland EL, McGovern P, Lazar M. Mindfulness treatment for substance misuse: A systematic review and meta-analysis. J Subst Abuse Treat. 2017;75:62–96. doi: 10.1016/j.jsat.2017.01.008. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Skills training manual for treating borderline personality disorder 1993 [Google Scholar]
- Loucks EB, Schuman-Olivier Z, Britton WB, Fresco DM, Desbordes G, Brewer JA, Fulwiler C. Mindfulness and Cardiovascular Disease Risk: State of the Evidence, Plausible Mechanisms, and Theoretical Framework. Curr Cardiol Rep. 2015;17:112. doi: 10.1007/s11886-015-0668-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF. Long-term stability of depression, anxiety, and stress syndromes. J Abnorm Psychol. 1998;107:520–526. doi: 10.1037//0021-843x.107.3.520. [DOI] [PubMed] [Google Scholar]
- Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends in cognitive sciences. 2008;12:163–169. doi: 10.1016/j.tics.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Weng HY, Sullivan JC, Lutz A. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behaviour research and therapy. 2012;50:3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacNair-Semands RR, Ogrodniczuk JS, Joyce AS. Structure and initial validation of a short form of the Therapeutic Factors Inventory. International journal of group psychotherapy. 2010;60 doi: 10.1521/ijgp.2010.60.2.245. [DOI] [PubMed] [Google Scholar]
- Magai C, Consedine N, Neugut AI, Hershman DL. Common Psychosocial Factors Underlying Breast Cancer Screening And Breast Cancer Treatment Adherence: A Conceptual Review And Synthesis. Journal of Women's Health. 2007;16:11–23. doi: 10.1089/jwh.2006.0024. [DOI] [PubMed] [Google Scholar]
- Maglione MA, Maher AR, Ewing B, Colaiaco B, Newberry S, Kandrack R, Shanman RM, Sorbero ME, Hempel S. Efficacy of mindfulness meditation for smoking cessation: A systematic review and meta-analysis. Addict Behav. 2017;69:27–34. doi: 10.1016/j.addbeh.2017.01.022. [DOI] [PubMed] [Google Scholar]
- Manna A, Raffone A, Perrucci MG, Nardo D, Ferretti A, Tartaro A, Romani GL. Neural correlates of focused attention and cognitive monitoring in meditation. Brain research bulletin. 2010;82:46–56. doi: 10.1016/j.brainresbull.2010.03.001. [DOI] [PubMed] [Google Scholar]
- Marzetti L, Di Lanzo C, Zappasodi F, Chella F, Raffone A, Pizzella V. Magnetoencephalographic alpha band connectivity reveals differential default mode network interactions during focused attention and open monitoring meditation. Frontiers in human neuroscience. 2014;8 doi: 10.3389/fnhum.2014.00832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason L, Grey N, Veale D. My Therapist is a Student? The Impact of Therapist Experience and Client Severity on Cognitive Behavioural Therapy Outcomes for People with Anxiety Disorders. Behav Cogn Psychother. 2016;44:193–202. doi: 10.1017/S1352465815000065. [DOI] [PubMed] [Google Scholar]
- Mayer JD, Stevens A. An emerging understanding of the reflective (meta-) experience of mood. Journal of Research in Personality. 1994;28:351–373. [Google Scholar]
- Miwa Y, Hanyu K. The effects of interior design on communication and impressions of a counselor in a counseling room. Environment and Behavior. 2006;38:484–502. [Google Scholar]
- Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche P, Devereaux PJ. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. Journal of clinical epidemiology. 2010;63 doi: 10.1136/bmj.c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabi H, Kivimaki M, De Vogli R, Marmot MG, Singh-Manoux A. Positive and negative affect and risk of coronary heart disease: Whitehall II prospective cohort study. British Medical Journal. 2008;337:a118. doi: 10.1136/bmj.a118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabi H, Kivimaki M, Zins M, Elovainio M, Consoli SM, Cordier S, Ducimetiere P, Goldberg M, Singh-Manoux A. Does personality predict mortality? Results from the GAZEL French prospective cohort study. Int J Epidemiol. 2008;37:386–396. doi: 10.1093/ije/dyn013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabi H, Koskenvuo M, Singh-Manoux A, Korkeila J, Suominen S, Korkeila K, Vahtera J, Kivimaki M. Low Pessimism Protects Against Stroke. The Health and Social Support (HeSSup) Prospective Cohort Study. Stroke. 2009 doi: 10.1161/STROKEAHA.109.565440. Epub-ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow JA. A Prospective Study of Depression and Posttraumatic Stress Symptoms After a Natural Disaster: The 1989 Loma Prieta Earthquake. Journal of Personality and Social Psychology. 1991;61:115–121. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- Norcross JC, Wampold BE. Evidence-based therapy relationships: research conclusions and clinical practices. Psychotherapy (Chic) 2011;48:98–102. doi: 10.1037/a0022161. [DOI] [PubMed] [Google Scholar]
- Oikonomou MT, Arvanitis M, Sokolove RL. Mindfulness training for smoking cessation: A meta-analysis of randomized-controlled trials. J Health Psychol. 2016 doi: 10.1177/1359105316637667. [DOI] [PubMed] [Google Scholar]
- Ong JC, Hedeker D, Wyatt JK, Manber R. Examining the Variability of Sleep Patterns during Treatment for Chronic Insomnia: Application of a Location-Scale Mixed Model. Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine. 2016;12 doi: 10.5664/jcsm.5872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M. Reenvisioning Clinical Science: Unifying the Discipline to Improve the Public Health. Clin Psychol Sci. 2014;2:22–34. doi: 10.1177/2167702613497932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ospina MB, Bond K, Karkhaneh M, Tjosvold L, Vandermeer B, Liang Y, Bialy L, Hooton N, Buscemi N, Dryden DM, Klassen TP. Evidence Report/Technology Assessment No. 155 (Prepared by the University of Alberta Evidence-Based Practice Center under Contract No. 290-02-0023.) Rockville MD: Agency for Healthcare Research and Quality; 2007. Meditation practices for health: state of the research; pp. 1–263. AHQR Publication No. 07-E010. [PMC free article] [PubMed] [Google Scholar]
- Persons JB, Burns DD. Mechanisms of action of cognitive therapy: The relative contributions of technical and interpersonal interventions. Cognitive therapy and Research. 1985;9:539–551. [Google Scholar]
- Rapgay L, Bystrisky A. Classical mindfulness: an introduction to its theory and practice for clinical application. Ann N Y Acad Sci. 2009;1172:148–162. doi: 10.1111/j.1749-6632.2009.04405.x. [DOI] [PubMed] [Google Scholar]
- Ridderinkhof KR, van den Wildenberg WP, Segalowitz SJ, Carter CS. Neurocognitive mechanisms of cognitive control: the role of prefrontal cortex in action selection, response inhibition, performance monitoring, and reward-based learning. Brain Cogn. 2004;56:129–140. doi: 10.1016/j.bandc.2004.09.016. [DOI] [PubMed] [Google Scholar]
- Riddle MW, Ferrer R. The Science of Behavior Change. Association for Psychological Science Observer. 2015 https://www.psychologicalscience.org/observer/the-science-of-behavior-change#.WSLyyZLyt6k.
- Rueda MR, Posner MI, Rothbart MK. The development of executive attention: contributions to the emergence of self-regulation. Dev Neuropsychol. 2005;28:573–594. doi: 10.1207/s15326942dn2802_2. [DOI] [PubMed] [Google Scholar]
- Ruffault A, Czernichow S, Hagger MS, Ferrand M, Erichot N, Carette C, Boujut E, Flahault C. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: A systematic review and meta-analysis. Obes Res Clin Pract. 2016 doi: 10.1016/j.orcp.2016.09.002. [DOI] [PubMed] [Google Scholar]
- Salovey P, Mayer JD, Goldman SL, Turvey C, Palfai TP. Emotional Attention, Clarity and Repair: Exploring Emotional Intelligence Using the Trait Meta-Mood Scale. Washinton D.C.: American Psychological Association; 1995. [Google Scholar]
- Salzberg S. Lovingkindness: The revolutionary art of happiness. Shambhala Publications; 2002. [Google Scholar]
- Santorelli S. Center for Mindfulness in Medicine, Health Care, and Society. University of Massachusetts Medical School; 2014. Mindfulness-Based Stress Reduction Standards of Practice. [Google Scholar]
- Santorelli S, Kabat-Zinn J. Mindfulness Based Stress Reduction Professional Training. Worcester, MA: Center for Mindfulness; 2003. MBSR Curriculum Guide and Supporting Materials. [Google Scholar]
- Santorelli S, Meleo-Meyer F, Koerbel L. Mindfulness-Based Stress Reduction (MBSR) Authorized Curriculum Guide. Worcester, MA: Center for Mindfulness in Medicine, Health Care, and Society; 2017. [Google Scholar]
- Sayadaw M. Practical insight meditation: basic and progressive stages 1991 [Google Scholar]
- Schroevers MJ, Brandsma R. Is learning mindfulness associated with improved affect after mindfulness-based cognitive therapy? Br J Psychol. 2009 doi: 10.1348/000712609X424195. Epub-ahead of print. [DOI] [PubMed] [Google Scholar]
- Segal Z, Bieling P, Young T, MacQueen G, Cooke R, Martin L, Levitan RD. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Archives of General Psychiatry. 2010;67:1256–1264. doi: 10.1001/archgenpsychiatry.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal Z, Teasdale J, Williams J, Gemar M. The Mindfulness-Based Cognitive Therapy Adherence Scale: Inter-rater realiability, adherence to and treatment distintiveness. Clinical Psychology and Psychotherapy. 2002;9:131–138. [Google Scholar]
- Segal Z, Williams J, Teasdale J. Minfulness-Based Cognitive Therapy for Depression: A New Approach for Preventing Relapse. New York: Guilford; 2002a. Handout 10.1 Summary of Session 5: Allowing/Letting Be. [Google Scholar]
- Segal Z, Williams J, Teasdale J. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. London: Guilford; 2002b. [Google Scholar]
- Shahar B, Britton WB, Sbarra DA, Figueredo AJ, Bootzin RR. Mechanisms of change in mindfulness-based cognitive therapy for depression: Preliminary evidence from a randomized controlled trial. International Journal of Cognitive Therapy. 2010;3:402–418. [Google Scholar]
- Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. J Clin Psychol. 2006;62:373–386. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- Shibata S, Suzuki N. Effects of the foliage plant on task performance and mood. Journal of Environmental Psychology. 2002;22:265–272. [Google Scholar]
- Ulrich RS. Effects of interior design on wellness: theory and recent scientific research. J Health Care Inter Des. 1991;3:97–109. [PubMed] [Google Scholar]
- Uusberg H, Uusberg A, Talpsep T, Paaver M. Mechanisms of mindfulness: The dynamics of affective adaptation during open monitoring. Biol Psychol. 2016;118:94–106. doi: 10.1016/j.biopsycho.2016.05.004. [DOI] [PubMed] [Google Scholar]
- Vago DR, Silbersweig DA. Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Front Hum Neurosci. 2012;6:296. doi: 10.3389/fnhum.2012.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Velden AM, Roepstorff A. Neural mechanisms of mindfulness meditation: bridging clinical and neuroscience investigations. Nat Rev Neurosci. 2015;16:439. doi: 10.1038/nrn3916-c1. [DOI] [PubMed] [Google Scholar]
- van Gaal S, Lamme VA, Fahrenfort JJ, Ridderinkhof KR. Dissociable brain mechanisms underlying the conscious and unconscious control of behavior. J Cogn Neurosci. 2011;23:91–105. doi: 10.1162/jocn.2010.21431. [DOI] [PubMed] [Google Scholar]
- Wallace BA. The attention revolution: Unlocking the power of the focused mind 2006 [Google Scholar]
- Wallis DJ, Hetherington MM. Emotions and eating. Self-reported and experimentally induced changes in food intake under stress. Appetite. 2009;52:355–362. doi: 10.1016/j.appet.2008.11.007. [DOI] [PubMed] [Google Scholar]
- Wampold BE, Mondin GW, Moody M, Stich F, Benson K, Ahn H. A meta-analysis of outcome studies comparing bona fide psychotherapies: Empiricially, "all must have prizes". Psychological Bulletin. 1997;122:203–215. [Google Scholar]
- Wangyal T, Vaughn M. Awakening the luminous mind : Tibetan meditation for inner peace and joy. 1. Carlsbad, CA: Hay House, Inc; 2012. [Google Scholar]
- Wells A, Davies MI. The Thought Control Questionnaire: A measure of individual differences in the control of unwanted thoughts. Behaviour research and therapy. 1994;32:871–878. doi: 10.1016/0005-7967(94)90168-6. [DOI] [PubMed] [Google Scholar]
- Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, Berry S, Greenfield S, Ware J. The functioning and well-being of depressed patients. Results from the Medical Outcomes Study. Jama. 1989;262:914–919. [PubMed] [Google Scholar]
- Wilkinson L. APA Task Force for Statistical Inference Statistical inference: Statistical Methods in psychology journals: Guidelines and explanations. American Psychologist. 1999;54:594–604. [Google Scholar]
- Williams JM, Alatiq Y, Crane C, Barnhofer T, Fennell MJ, Duggan DS, Hepburn S, Goodwin GM. Mindfulness-based Cognitive Therapy (MBCT) in bipolar disorder: preliminary evaluation of immediate effects on between-episode functioning. J Affect Disord. 2008;107:275–279. doi: 10.1016/j.jad.2007.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Papandonatos G, Fava JL, Gorin AA, Phelan S, McCaffery J, Tate DF. Maintaining large weight losses: the role of behavioral and psychological factors. Journal of consulting and clinical psychology. 2008;76:1015–1021. doi: 10.1037/a0014159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt C, Harper B, Weatherhead S. The experience of group mindfulness-based interventions for individuals with mental health difficulties: a meta-synthesis. Psychother Res. 2014;24:214–228. doi: 10.1080/10503307.2013.864788. [DOI] [PubMed] [Google Scholar]
- Yalom ID, Leszcz M. The therapeutic factors. The theory and practice of group psychotherapy 1995 [Google Scholar]
- Yook K, Lee SH, Ryu M, Kim KH, Choi TK, Suh SY, Kim YW, Kim B, Kim MY, Kim MJ. Usefulness of mindfulness-based cognitive therapy for treating insomnia in patients with anxiety disorders: a pilot study. Journal of Nervous and Mental Disease. 2008;196:501–503. doi: 10.1097/NMD.0b013e31817762ac. [DOI] [PubMed] [Google Scholar]
- Young S. Ways to Know Yourself: An Introduction to Basic Mindfulness 2011 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Appendix 1 Session × Session Comparison Table.
Supplementary Appendix 2 Example FA program materials.
Supplementary Appendix 3 Example OM program materials.