Abstract
Community-acquired pneumonia (CAP) is one of the most common serious infections in childhood. This review focuses on pediatric CAP in the United States and other industrialized nations, specifically highlighting the changing epidemiology of CAP, diagnostic and therapeutic challenges, and areas for further research.
Keywords: Community-acquired pneumonia, Pediatric, Epidemiology
Key points
-
•
Pediatric community-acquired pneumonia (CAP) continues to cause significant morbidity and remains one of the most common serious infections of childhood.
-
•
Routine childhood vaccination against Streptococcus pneumoniae has greatly reduced invasive disease rates caused by this pathogen.
-
•
Although molecular diagnostics have helped highlight the important role that respiratory viruses play in pediatric CAP, bacterial diagnostics remain suboptimal.
-
•
Biomarkers and molecular host responses to infection are current areas of intense study that may facilitate a deeper understanding of pneumonia etiology and disease outcomes.
Introduction
Pneumonia is an infection of the lower airways (distal bronchi and alveoli) caused by both viruses and bacteria. Community-acquired pneumonia (CAP) specifically refers to clinical signs and symptoms of pneumonia acquired outside a hospital setting.1 It is one of the most common serious infections in childhood, accounting for more than 900,000 deaths among children younger than 5 years of age in 2015.2 Although the rate of mortality due to CAP is much lower in the developed world compared with the developing world, CAP continues to account for a significant proportion of health care visits and hospitalizations in high-income countries. This review focuses on pediatric CAP in the United States and other industrialized nations, specifically highlighting the changing epidemiology of CAP, diagnostic and therapeutic challenges, and areas for further research.
Epidemiology
In the United States, CAP accounts for approximately 2 million outpatient visits annually3 and is among the most common causes for hospitalization, with approximately 124,000 pediatric hospitalizations annually (annual incidence of 15.7–22.5 hospitalizations per 100,000 children).4, 5, 6 The highest rate of health care utilization occurs in children younger than 2 years of age and decreases with increasing age in the pediatric population.4
Diagnosis
Children with pneumonia most often present with fever, tachypnea, and other signs of respiratory distress (Table 1 ). Signs and symptoms may include tachypnea, cough, dyspnea, retractions, grunting, hypoxemia, abdominal pain, or lethargy, and physical examination findings of decreased breath sounds, crackles, rales, or wheezing on auscultation of lung fields. Many of these findings overlap with other acute lower respiratory tract diseases (eg, asthma and viral bronchiolitis), and identifying children with pneumonia based only on clinical signs and symptoms is sometimes difficult. As a result, chest radiographs are commonly used to confirm the diagnosis. Even when a chest radiograph reveals an infiltrate, however, it is sometimes difficult to differentiate between consolidation representing pneumonia and atelectasis commonly seen in children with asthma or bronchiolitis. As a result, variation in chest radiograph interpretation is common and may contribute to antibiotic overuse.7, 8 For this reason, the guideline developed by the Pediatric Infectious Diseases Society (PIDS) and Infectious Diseases Society of America (IDSA) discourages use of chest radiographs in children with suspected uncomplicated pneumonia in an outpatient setting.7 Chest radiographs are recommended in children who are hospitalized with hypoxemia or respiratory distress and in those with suspected complications, such as parapneumonic effusions, necrotizing pneumonia, or pneumothorax (Fig. 1 ).
Table 1.
Manifestations of community-acquired pneumonia requiring hospitalization among those enrolled in the Centers for Disease Control Etiology of Pneumonia in the Community study
| Characteristic | Frequency in Children with Radiographic Evidence of Pneumonia (N = 2358) no. (%) |
|---|---|
| Symptom | |
| Cough | 2230 (95) |
| Abnormal temperature | 2155 (91) |
| Anorexia | 1766 (75) |
| Dyspnea | 1657 (70) |
| Chest indrawing | 1278 (55) |
| Radiographic finding | |
| Consolidation | 1376 (58) |
| Alveolar or interstitial infiltrate | 1195 (51) |
| Pleural effusion | 314 (13) |
Adapted from Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. NEJM 2015;372(9):839. Table 1; with permission.
Fig. 1.
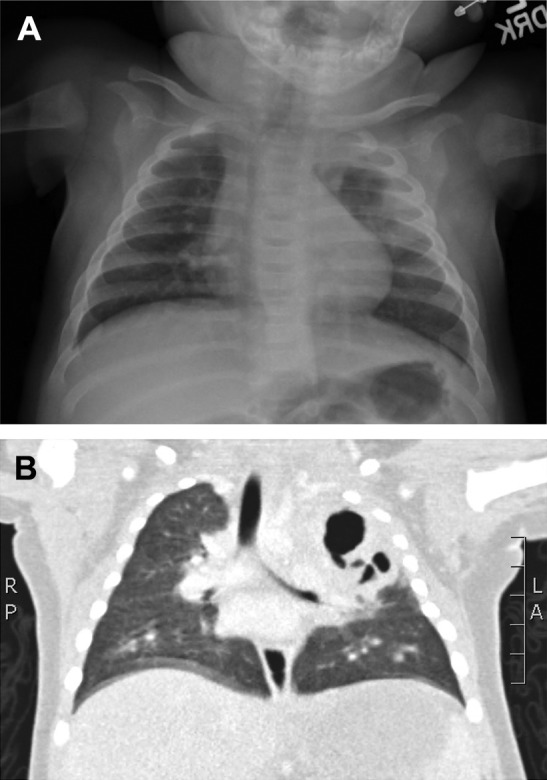
Radiographic imaging in cavitating pneumonia. (A) Chest radiograph demonstrating a complex air space opacity in the left upper lobe with central lucency consistent with cavitating pneumonia. (B) CT of the same lesion demonstrates a large cavity with central necrosis and multiple air fluid levels occupying most of the left upper lobe.
Chest ultrasound is most often used for evaluating local complications, such as parapneumonic effusion and empyema, but recent studies have demonstrated high sensitivity (92%–98%) and specificity (92%–100%) for detecting lung consolidation compared with chest radiography.9, 10, 11, 12, 13 Additional benefits of chest ultrasound include a lack of ionizing radiation and availability in most emergency department settings. An important limitation of ultrasound is that evaluation and interpretation are highly operator dependent. Thus, despite these promising early studies, large-scale, pragmatic studies are needed to better evaluate the effectiveness of this imaging technique versus standard chest radiography.
Etiology
Pneumonia is a heterogeneous disease caused by a variety of pathogens, including viruses and bacteria. Historically, CAP was largely considered a bacterial process, most often due to Streptococcus pneumoniae, Haemophilus influenzae, Streptococcus pyogenes, and Staphylococcus aureus.14, 15, 16, 17, 18 The introduction of routine childhood vaccination against both Streptococcus pneumoniae and H influenzae, however, has dramatically reduced disease caused by these pathogens. At the same time, highly sensitive molecular diagnostics for viral respiratory pathogens have heightened awareness of the impact of viruses as a cause of CAP.
Pneumonia Etiology Prior to Introduction of Pneumococcal Conjugate Vaccine
A 2004 study by Michelow and colleagues15 exemplifies pre–pneumococcal conjugate vaccine (PCV) era etiology studies. That study used traditional culture methods, pneumolysin-based polymerase chain reaction (PCR) assays, viral direct fluorescent antibody tests, and serologic tests for viruses, Mycoplasma spp, and Chlamydia spp to identify pathogens in 154 hospitalized children with radiographically confirmed lower respiratory infections at a single institution. A majority of patients (60%) were noted to have infection with typical respiratory bacteria (most commonly, Streptococcus pneumoniae, detected in 73% of children with documented bacterial disease), with viruses identified in 45% of children.
Impact of Pneumococcal Conjugate Vaccines
A 7-valent PCV (PCV7) targeting the most common clinically important pneumococcal serotypes was introduced into the United States childhood immunization schedule in 2000. Rates of invasive pneumococcal disease caused by PCV7 serotypes in children less than 5 years of age plummeted from an average of 95.2 cases to 22.6 cases per 100,000 population within 4 years after the introduction of PCV7.19 By 2006, hospitalization rates for CAP and pneumonia-associated complications among young children decreased by 39% and 36%, respectively.5, 20 Despite these declines, disease caused by nonvaccine serotypes soon emerged, and rates of complicated pneumonia increased, prompting introduction of an expanded, 13-valent PCT (PCV13) into the US childhood immunization program in 2010.21 Since that time, hospitalization rates decreased from 53.6 per 100,000 admissions in the pre-PCV13 era to 23.3 per 100,000 admissions in the post-PCV13 era, and rates of complicated pneumococcal pneumonia decreased significantly.22
Pneumonia Etiology in the Post–Pneumococcal Conjugate Vaccine Era
The multicenter Centers for Disease Control and Prevention (CDC) Etiology of Pneumonia in the Community (EPIC) Study was a prospective, population-based surveillance study of greater than 2300 pediatric CAP hospitalizations in the United States conducted from 2010 to 2012.4 This study used serology and nasopharyngeal PCR to identify 8 different viruses, culture-based methods and whole-blood PCR (pneumococcal lyt-A) to identify typical bacteria, and nasopharyngeal PCR to identify atypical bacterial pathogens.
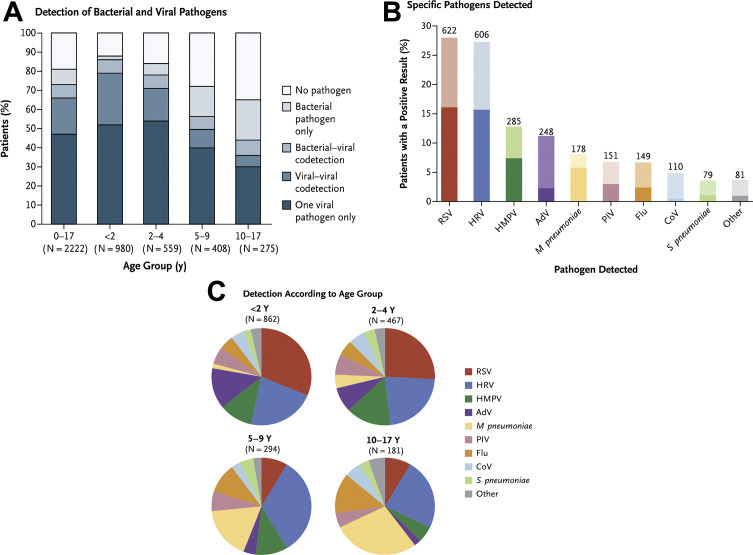
Viruses were identified in greater than 70% of children, whereas bacteria were identified in only 15% of children (Fig. 2 ).4 The most common viral pathogens included respiratory syncytial virus (RSV), human rhinovirus, human metapneumovirus, and adenovirus, all detected in greater than 10% of children. RSV, adenovirus, and human metapneumovirus were more commonly identified in children younger than 5 years of age compared with older children.
Fig. 2.
Pathogens detected in US children with CAP requiring hospitalization, detection according to age group. Darker shading in the bar graph in panel B indicates that only the single pathogen was detected, and lighter shading indicates the pathogen was detected in combination with at least one other pathogen. Panel A shows the proportion of pathogen types among 2222 hospitalized children in the CDC EPIC study. A total of 4 patients had more than one bacterial pathogen without a virus detected. Panel C shows the proportions of pathogens detected, according to age group. AdV, denotes adenovirus; CoV, coronavirus; Flu, influenza A or B virus; HMPV, human metapneumovirus; HRV, human rhinovirus; PIV, parainfluenza virus.
(Data from Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. NEJM 2015;372(9):840. Fig. 2; with permission.)
Bacteria were identified in approximately 15% of children in the CDC EPIC study, although Streptococcus pneumoniae was only identified in 4% of children, further underscoring the impact that PCV has had on the epidemiology of pediatric CAP.4 Mycoplasma pneumoniae was the most frequently identified bacterial pathogen, detected in 8% of children, including 19% of school-aged children, but only 3% of children younger than 5 years of age. Other bacteria were identified in 1% or less of children. Importantly, 19% of children in the CDC EPIC study had no pathogen identified, highlighting the continued need for enhanced diagnostics and novel pathogen discovery techniques.
Uncommon Causes of Community-acquired Pneumonia
Other pathogens that are less commonly seen among US children include Mycobacterium tuberculosis, fungi, Burkholderia cepacia, Aspergillus fumigatus, and Pseudomonas aeruginosa and usually occur in patients with underlying risk factors, such as immunocompromising conditions; chronic conditions, such as cystic fibrosis and spinal muscular atrophy; or history of international travel (Table 2 ). These pathogens should also be suspected in patients who experience treatment failure for more common etiologic agents.
Table 2.
Rare microorganisms causing pediatric community-acquired pneumonia or occurring in specialized populations
| Microorganism | Comment |
|---|---|
| Viruses | |
| Varicella zoster virus | Potential complication after primary varicella infection. Often severe and associated with secondary bacterial infection. |
| Measles virus | Rubeola. Pneumonia is a frequent complication. |
| Hantavirus | Hantavirus pulmonary syndrome. Rodent exposure. |
| Bacteria | |
| Bordatella pertussis | Pneumonia uncommon manifestation. Bacterial coinfection may be severe, especially in infants. |
| Group B streptococci | Neonatal pneumonia and sepsis. |
| Listeria monocytogenes | Neonatal pneumonia and sepsis. |
| Gram-negative enterics | Neonatal pneumonia and sepsis. Potential pathogens in aspiration pneumonia. |
| Chlamydia trachomatis | Cause of afebrile pneumonia in young infants <3 mo of age. |
| Anaerobes (oral flora) | Potential pathogens in aspiration pneumonia. |
| Legionella pneumophila | Legionnaires’ disease. Rare in children but associated with community outbreaks. Exposure to contaminated artificial freshwater systems. |
| Coxiella burnetti | Q fever. Exposure to wild and domesticated herbivores or unpasteurized dairy (eg, cattle, sheep, and goats). Also potential bioterrorism agent. |
| Chlamydia psittaci | Psittacosis. Bird (eg, pet birds and pigeons) exposure. |
| Francisella tularensis | Tularemia. Rabbit exposure. |
| Yersinia pestis | Pneummonic plague. Rodent flea exposure. |
| Bacillus anthracis | Anthrax. Woolsorter’s disease. Wild and domesticated herbivore (eg, cattle, sheep, goats) exposure. Also potential bioterrorism agent. |
| Leptospira interrogans | Leptospirosis. Exposure to urine of wild and domestic animals carrying the bacterium. |
| Mycobacterium tuberculosis | Rare in US children. Usually associated with high-risk exposures. |
| Brucella abortus | Brucellosis. Exposure to wild and domesticated animals or unpasteurized dairy (eg, cattle, sheep, pigs, goats, deer, and dogs). |
| Fungi | |
| Histoplasma capsulatum | Histoplasmosis. Exposure to bird or bat droppings (eg, poultry/bird roosts and caves). Endemic to eastern and central United States. |
| Blastomyces dermaitidis | Blastomycosis. Environmental exposure to fungal spores (wooded areas). Endemic to Southeastern and Midwestern United States. |
| Cryptococcus neoformans | Cryptococcosis. Exposure to soil contaminated with bird droppings. Significant pathogen nearly exclusively among immunocompromised. |
| Coccidioides immitis | Coccidiomycosis. Valley fever. Environmental exposure to fungal spores (dry, dusty environments). Endemic to Southwestern United States. |
Adapted from Williams DJ, Shah SS. Community-acquired pneumonia in the conjugate vaccine era. J Pediatric Infect Dis Soc 2012;1(4):320. Table 2; with permission.
Challenges and areas for future research
Bacterial Diagnostics
Blood cultures
The 2011 PIDS/IDSA CAP guideline recommends obtaining blood cultures in children hospitalized with CAP.7, 23, 24 In this setting, however, blood cultures identify a pathogen in only 2% to 7% of children with CAP.24, 25, 26, 27 Blood cultures are more often positive in children with parapneumonic effusion, ranging from 10% to 35%.25, 26, 28 In the outpatient setting, blood cultures are not routinely recommended, because positivity rates are low and results are unlikely to change management. Regardless, despite their low yield, blood cultures currently provide the best opportunity to identify typical bacterial pathogens in most children with CAP.
Diagnostic yield of blood cultures can be optimized by restricting their use to those patients with increased pretest probability of having a positive culture, such as those who are severely ill or have parapneumonic effusion.29, 30, 31 Isolation of pathologic organisms occurs significantly less frequently in patients exposed to antibiotics before specimen collection.32, 33 Studies have also demonstrated increased yield of blood cultures with each additional milliliter of blood drawn.34, 35, 36 Obtaining adequate weight-based blood volumes is also associated with lower rates of blood culture contamination, for reasons yet unknown.35, 37 Contamination rates can also be minimized by adhering to proper sterile collection methods.32, 35, 37
Cultures of the lower respiratory tract
Pleural fluid cultures are positive in up to 35% of cases and should be performed whenever pleural fluid is obtained.7, 25, 26, 38, 39, 40 The invasive methods associated with sampling the pleural space, however, make it impractical to obtain pleural fluid specimens except when dictated for clinical care. Bronchoalveolar lavage is rarely indicated in CAP, except in instances of lack of response to therapy, very severe pneumonia, or immunocompromised hosts in whom opportunistic pathogens are suspected.41 Sputum cultures are of low diagnostic yield in children, due to the inability of most young children with pneumonia to produce an adequate sputum sample. Pretreatment with antibiotics further hinders diagnostic yield. Induced sputum has been explored as an opportunity to collect sputum samples in young children, although utility is limited by frequent detection of upper respiratory tract bacteria and similar rates of recovery of pathogens in pneumonia cases compared with children without pneumonia.42, 43
Molecular Diagnostics
Bacterial diagnostics
Pneumococcal urinary antigen testing is often used in the evaluation of pneumonia in adults. In children, however, detection of Streptococcus pneumoniae urinary antigen is associated with false-positive results due to high rates of nasopharyngeal colonization.44, 45 More recently, a serotype-specific urinary antigen detection method has been developed and validated in adults with pneumonia46; whether or not this test could prove useful in children remains to be determined.
Although not widely used in clinical settings, whole-blood pneumococcal PCR (lyt-A) has been used in epidemiologic studies, including EPIC and Pneumonia Etiology Research for Child Health (PERCH). Potential benefits include improved sensitivity, rapid turnaround time, and less influence of antibiotic pretreatment compared with culture-based methods.47, 48 In the EPIC study, 2.5% of children tested were PCR-positive for Streptococcus pneumoniae, whereas blood cultures were positive for pneumococcus in only 1% of children (P<.001).4 In the PERCH study, 291 children with pneumonia (7.3%) were pneumococcal PCR-positive, whereas only 44 children (denominator not provided) had a positive blood culture for Streptococcus pneumoniae.49 Moreover, although prior studies demonstrated 100% specificity of lyt-A pneumococcal PCR from the blood,50 the PERCH study also identified pneumococcal DNA in the blood of 273 control children (5.5%).49 Thus, although pneumococcal PCR may increase rate of detection over blood culture, suboptimal test specificity hampers interpretation.
PCR also increases yield for pleural fluid specimens. In a study evaluating archived pleural fluid specimens from 63 pediatric patients with CAP, a pathogen was detected in 84% of samples using PCR compared with only 35% of samples when using conventional culture methods (P<.001).28 The most frequent pathogen detected using both methods was Streptococcus pneumoniae, 71% using PCR and 24% using conventional culture. The next most frequent pathogens identified were Streptococcus pyogenes (11% using PCR and 5% using conventional culture) and S aureus (8% using PCR and 6% using conventional culture). This study also highlighted the potential for bias with respect to pathogen identification introduced when relying on culture alone for epidemiologic studies, because penicillin-resistant pneumococcal isolates and S aureus were more likely to be positive in culture, whereas other serotypes of Streptococcus pneumoniae and bacterial pathogens commonly susceptible to penicillins were more commonly identified by PCR.
Up to two-thirds of children younger than 5 years are colonized in the upper respiratory tract with common bacterial pathogens known to cause pneumonia,51 and PCR from the upper respiratory tract is not a reliable method for ascertaining bacterial etiologies of pneumonia. A possible exception is M pneumoniae, which has not previously been considered a frequent colonizer of the upper respiratory tract. Consistent with this theory, the CDC EPIC study demonstrated that although M pneumoniae was detected in 8% of children with pneumonia, fewer than 1% of controls had evidence of M pneumoniae.4 In contrast, a cross-sectional, observational study in the Netherlands of asymptomatic children and children with symptoms of upper and lower respiratory tract infection detected M pneumoniae DNA not only in 16% of symptomatic children but also in 21% of asymptomatic children.52 Given the conflicting results of these 2 studies and the increasing commercial availability of M pneumoniae PCR tests, caution is warranted when interpreting test results in the clinical setting.
Viral diagnostics
In contrast to bacteria, PCR testing for viruses from upper respiratory samples has largely replaced culture and serology-based methods to investigate pneumonia etiology, owing to superior sensitivity, rapid turnaround time, and ability to identify viruses that are difficult to grow in culture. A major concern, however, is whether lower respiratory tract disease can be attributed to a viral pathogen detected in the upper airway. The scope of the problem is well illustrated in a study conducted by Self and colleagues53 that compared PCR detections of 13 viruses from the upper respiratory tract among 1024 children with CAP and 759 healthy, asymptomatic children enrolled in the CDC EPIC study. Overall, approximately 25% of asymptomatic children had 1 or more viruses detected compared with approximately 65% of children with CAP. Detection of most viruses was higher among children with CAP compared with asymptomatic controls, including influenza (3% vs 0%), RSV (27% vs 2%), and human metapneumovirus (15% vs 2%), with attributable fractions greater than 90% for all. Conversely, rhinovirus was detected at a similar frequency in both children with CAP and asymptomatic children (22% vs 17%; attributable fraction 12%; 95% CI, 18% to 34%). Attributable fractions for other viruses studied ranged from 44% to 68%. Thus, although some viruses detected in the upper airway likely reflect lower airway disease (eg, RSV, influenza, and human metapneumovirus), detection of other viruses must be interpreted with caution. As proposed for adults, investigating viral loads may further help to differentiate disease versus asymptomatic colonization.54
Because sensitive methods of diagnosing viral infections have become more widely available, the recognition of viral and bacterial coinfection has also increased. It is well known that upper tract disease with respiratory viruses often precedes the development of bacterial pneumonia.55, 56, 57 Although it is not always clear if a virus detected in the upper airway represents prior or concurrent infection in a subject with bacterial pneumonia, studies suggest that viral-bacterial codetections are associated with a more severe clinical course compared with single viral or bacterial detections.58, 59, 60 The association between influenza and coinfection with pneumococcal or staphylococcal pneumonia is perhaps the best described of these viral and bacterial coinfections.61, 62
Acute-Phase Reactants and Biomarkers
Elevated leukocyte count was traditionally considered to be associated with serious bacterial infection, but the specificity of leukocyte count in making the diagnosis of bacterial pneumonia in children is poor, and the degree of elevation does not reliably distinguish between viral and bacterial pneumonia.7, 63, 64, 65 As such, routine measurement of leukocyte count is likely not beneficial.
More recent biomarkers used in the detection of pneumonia include C-reactive protein (CRP) and procalcitonin (PCT). These biomarkers may perform better than leukocyte count for identifying bacterial infections,64, 66, 67 although identifying relevant clinical cutpoints remains a challenge. To evaluate the impact of CRP in the etiologic diagnosis of pneumonia, a meta-analysis of 8 studies with more than 1200 children with viral or bacterial causes of CAP demonstrated that CRP levels greater than or equal to 40 mg/L to 60 mg/L were associated with only a 64% positive predictive value for identifying children with bacterial pneumonia.68
PCT is a peptide precursor of calcitonin and is produced by C cells in the thyroid gland and by neuroendocrine cells in the lung and intestine. Levels are usually undetectable in healthy individuals but increase in response to systemic inflammation. Cytokines typically associated with bacterial infection enhance PCT release, whereas interferons, which are more often associated with viral infections, inhibit PCT release.69, 70 Thus, much interest has been directed at PCT as a potential biomarker for bacterial disease.
Among 532 hospitalized children enrolled in the CDC EPIC study, a PCT cutoff value of 0.25 ng/mL demonstrated a sensitivity of 85% and specificity of 45% for CAP caused by typical bacterial pathogens.71 The study also found that higher PCT levels were associated with more severe disease. Multiple studies have shown utility in using PCT levels to guide antibiotic initiation and duration.71, 72, 73, 74, 75, 76
Biomarker studies using transcriptomics show promise for enhancing diagnostic capabilities by using host responses to identify possible pathogens and study disease severity.77, 78, 79, 80 Transcriptomics uses gene expression profiling to measure the activity or expression of thousands of genes at once, thereby creating a global picture of cellular activity. Profiles of peripheral blood leukocytes in patients with lower respiratory tract infection can accurately distinguish influenza viral infection from bacterial infection and predict disease severity.81 Host transcriptional profiling has also been shown useful in distinguishing symptomatic rhinovirus infection from incidental detection in children.80 These promising studies will likely add much to the understanding of pneumonia etiology and outcomes, although much work remains prior to translating these new technologies to the bedside.
Prediction of Outcomes
Several prognostic models are available for adults with pneumonia,82, 83 and their application has been shown to contribute to improved outcomes. Unfortunately, no analogous models have been validated in children, a recognized key knowledge gap.7 Recently, Williams and colleagues84 derived 3 prognostic models to identify risk for severe outcomes among children with CAP; each model demonstrated good predictive accuracy (concordance index 0.78–0.81). In that study, extremes of age, vital signs, chest indrawing, and radiographic infiltrate pattern ranked among the most important predictors of disease outcomes. Although these models require further validation, their use could reduce variability and improve care for children with pneumonia.
Treatment
Although viruses are a major cause of childhood pneumonia, a majority of children with pneumonia receive antibiotics. Pneumonia is associated with more antibiotic use in US pediatric hospitals than any other condition.85 When antibiotics are indicated, amoxicillin or ampicillin is recommended as first-line therapy in most children7 (Table 3 ). Prior to release of the national guideline, however, broader-spectrum third-generation cephalosporins and macrolides were commonly used.
Table 3.
Empiric antimicrobial strategies for pediatric community-acquired pneumonia
| Population | Bacterial Pneumonia | Atypical Pneumonia | |
|---|---|---|---|
| Outpatient | |||
| Neonates — 3 mo | |||
| Preschool (<5 y) | Preferred | Amoxicillin | Azithromycin |
| Alternative(s) | Amoxiciilin/clavulanate | Clarithromycin or erythromycin | |
| 5–17 y | Preferred | Amoxicillin | Azithromycin |
| Alternative(s) | Amoxicillin/clavulanate | Clarithromycin or erythromycin Doxycycline if >7 y | |
| Inpatient | |||
| Neonates | Preferred | Ampicillin + gentamicin | N/A |
| Alternative(s) | Ampicillin + cefotaxime | ||
| 1–3 mo | Preferred | Cefotaxime | N/A |
| Alternative(s) | Azithromycin if suspect C trachomatis or B pertussis | ||
| 3 mo–17 y, fully immunized, local epidemiology indicates low prevalence of penicillin nonsusceptible Streptococcus pneumoniae | Preferred | Ampicillin or penicillin G | Azithromycin |
| Alternative(s) | Ceftriaxone or cefotaxime Antistaphylococcal coverage for suspected S aureus, including clindamycin or vancomycin in methicillin-resistant S aureus–prevalent regions | Clarithromycin or erythromycin Doxycycline if >7 y Levofloxacin for those who have reached skeletal maturity | |
| 3 mo–17 y, not fully immunized, or local epidemiology indicates moderate to high prevalence of penicillin nonsusceptible Streptococcus pneumoniae | Preferred | Ceftriaxone or cefotaxime | Azithromycin |
| Alternative(s) | Levofloxacin Antistaphylococcal coverage for suspected S aureus, including clindamycin or vancomycin in methicillin-resistant S aureus–prevalent regions |
Clarithromycin or erythromycin Doxycycline if >7 y Levofloxacin for those who have reached skeletal maturity | |
Adapted from Bradley JS, Byington CL, Shah SS, et al. Empiric therapy for pediatric community-acquired pneumonia (CAP). The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis 2011;53:e34. Table 7; with permission.
To date, the impact of the national guideline on prescribing has been mixed. Approximately 4 years after guideline publication, penicillin use increased approximately 27.6% and cephalosporin use decreased approximately 27.8% across 48 tertiary care children’s hospitals in the United States, although substantial variability was noted across institutions.86 Similar variability persists in the outpatient setting.87 Antimicrobial stewardship programs, local clinical practice guidelines, and quality improvement methods all play important roles in raising awareness of these recommendations and reducing unnecessary and inappropriate antibiotic use.86, 88, 89
Current practices for treatment of uncomplicated CAP generally use 7-day to 10-day antibiotic courses, although 2 large pediatric randomized controlled studies are currently evaluating the safety and efficacy of shorter courses of antibiotics, a United Kingdom community-acquired pneumonia study (CAP-IT) and the US phase IV double-blind, placebo-controlled, randomized trial Short Course Outpatient Therapy of Community Acquired Pneumonia (SCOUT-CAP).90, 91
Consideration of alternative etiologies, such as S aureus, is warranted in children with severe or rapidly progressive disease, extensive local complications, or poor treatment response. S aureus is an uncommon cause of CAP, detected in only 1% of children hospitalized with pneumonia.4 Thus, to preserve the effectiveness of antistaphylococcal antibiotics, care must be taken when considering when to use these agents empirically, and efforts to de-escalate therapy whenever possible should be emphasized.
Although M pneumoniae is a frequent cause of CAP in children, it is impossible to reliably distinguish this pathogen from other common causes of pneumonia. Questions regarding the utility of currently available PCR tests for M pneumoniae, as outlined previously, further complicate treatment considerations. Moreover, azithromycin use is associated with the development of multidrug resistance.92, 93 Perhaps the most important consideration governing when to use macrolide therapy, however, is that currently available studies have failed to consistently demonstrate their benefit in children with pneumonia.94
Summary
Despite advances in recent years, CAP continues to cause significant morbidity and mortality and poses diagnostic and therapeutic challenges. Vaccination against Haemophilus influenzae type b and Streptococcus pneumoniae has greatly reduced invasive disease rates caused by these pathogens, and the introduction of molecular diagnostics has highlighted the important role that respiratory viruses play in disease pathogenesis while also introducing new challenges. This updated understanding brings into question whether all children with CAP would benefit from antibiotic therapy, and if so, which therapies might be most effective. Limitations of current diagnostics, however, impede advances toward addressing these important questions. Biomarkers and host responses to infection are current areas of intense study that may facilitate a deeper understanding of pneumonia etiology and disease outcomes. As this important work progresses, future epidemiologic studies using state-of-the-art diagnostics will continue to serve an important role in informing understanding of the changing epidemiology of CAP.
Acknowledgments
The authors thank Kathryn Edwards, MD, and Ritu Banerjee, MD, PhD, Vanderbilt University Medical Center, for their critical review and input during article preparation.
Footnotes
Disclosures: The authors have no relevant financial disclosures.
References
- 1.Harris M., Clark J., Coote N. British thoracic society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax. 2011;66(Suppl 2):ii1–ii23. doi: 10.1136/thoraxjnl-2011-200598. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization, 2016. Fact Sheet – Pneumonia. Available at: http://www.who.int/mediacentre/factsheets/fs331/en/. Accessed November 22, 2017.
- 3.Kronman M.P., Hersh A.L., Feng R. Ambulatory visit rates and antibiotic prescribing for children with pneumonia, 1994-2007. Pediatrics. 2011;127(3):411–418. doi: 10.1542/peds.2010-2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jain S., Williams D.J., Arnold S.R. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372(9):835–845. doi: 10.1056/NEJMoa1405870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee G.E., Lorch S.A., Sheffler-Collins S. National hospitalization trends for pediatric pneumonia and associated complications. Pediatrics. 2010;126(2):204–213. doi: 10.1542/peds.2009-3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Healthcare Cost and Utilization Project (HCUP). HCUP Kids’ Inpatient Database (KID) 2009; Available at: http://hcup-us.ahrq.gov/kidsoverview.jsp. Accessed June 28, 2017.
- 7.Bradley J.S., Byington C.L., Shah S.S. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the pediatric infectious diseases society and the infectious diseases society of America. Clin Infect Dis. 2011;53(7):e25–e76. doi: 10.1093/cid/cir531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Novack V., Avnon L.S., Smolyakov A. Disagreement in the interpretation of chest radiographs among specialists and clinical outcomes of patients hospitalized with suspected pneumonia. Eur J Intern Med. 2006;17(1):43–47. doi: 10.1016/j.ejim.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 9.Shah V.P., Tunik M.G., Tsung J.W. Prospective evaluation of point-of-care ultrasonography for the diagnosis of pneumonia in children and young adults. JAMA Pediatr. 2013;167(2):119–125. doi: 10.1001/2013.jamapediatrics.107. [DOI] [PubMed] [Google Scholar]
- 10.Copetti R., Cattarossi L. Ultrasound diagnosis of pneumonia in children. Radiol Med. 2008;113(2):190–198. doi: 10.1007/s11547-008-0247-8. [DOI] [PubMed] [Google Scholar]
- 11.Pereda M.A., Chavez M.A., Hooper-Miele C.C. Lung ultrasound for the diagnosis of pneumonia in children: a meta-analysis. Pediatrics. 2015;135(4):714–722. doi: 10.1542/peds.2014-2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boursiani C., Tsolia M., Koumanidou C. Lung ultrasound as first-line examination for the diagnosis of community-acquired pneumonia in children. Pediatr Emerg Care. 2017;33(1):62–66. doi: 10.1097/PEC.0000000000000969. [DOI] [PubMed] [Google Scholar]
- 13.Claes A.S., Clapuyt P., Menten R. Performance of chest ultrasound in pediatric pneumonia. Eur J Radiol. 2017;88:82–87. doi: 10.1016/j.ejrad.2016.12.032. [DOI] [PubMed] [Google Scholar]
- 14.Juven T., Mertsola J., Waris M. Etiology of community-acquired pneumonia in 254 hospitalized children. Pediatr Infect Dis J. 2000;19(4):293–298. doi: 10.1097/00006454-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Michelow I.C., Olsen K., Lozano J. Epidemiology and clinical characteristics of community-acquired pneumonia in hospitalized children. Pediatrics. 2004;113(4):701–707. doi: 10.1542/peds.113.4.701. [DOI] [PubMed] [Google Scholar]
- 16.Wubbel L., Muniz L., Ahmed A. Etiology and treatment of community-acquired pneumonia in ambulatory children. Pediatr Infect Dis J. 1999;18(2):98–104. doi: 10.1097/00006454-199902000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Claesson B.A., Trollfors B., Brolin I. Etiology of community-acquired pneumonia in children based on antibody responses to bacterial and viral antigens. Pediatr Infect Dis J. 1989;8(12):856–862. doi: 10.1097/00006454-198912000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Heiskanen-Kosma T., Korppi M., Jokinen C. Etiology of childhood pneumonia: serologic results of a prospective, population-based study. Pediatr Infect Dis J. 1998;17(11):986–991. doi: 10.1097/00006454-199811000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Hicks L.A., Harrison L.H., Flannery B. Incidence of pneumococcal disease due to non-pneumococcal conjugate vaccine (PCV7) serotypes in the United States during the era of widespread PCV7 vaccination, 1998-2004. J Infect Dis. 2007;196(9):1346–1354. doi: 10.1086/521626. [DOI] [PubMed] [Google Scholar]
- 20.Grijalva C.G., Nuorti J.P., Arbogast P.G. Decline in pneumonia admissions after routine childhood immunisation with pneumococcal conjugate vaccine in the USA: a time-series analysis. Lancet. 2007;369(9568):1179–1186. doi: 10.1016/S0140-6736(07)60564-9. [DOI] [PubMed] [Google Scholar]
- 21.Moore M.R., Gertz R.E., Jr., Woodbury R.L. Population snapshot of emergent Streptococcus pneumoniae serotype 19A in the United States, 2005. J Infect Dis. 2008;197(7):1016–1027. doi: 10.1086/528996. [DOI] [PubMed] [Google Scholar]
- 22.Olarte L., Barson W.J., Barson R.M. Pneumococcal pneumonia requiring hospitalization in us children in the 13-valent pneumococcal conjugate vaccine era. Clin Infect Dis. 2017;64(12):1699–1704. doi: 10.1093/cid/cix115. [DOI] [PubMed] [Google Scholar]
- 23.Campbell S.G., Marrie T.J., Anstey R. The contribution of blood cultures to the clinical management of adult patients admitted to the hospital with community-acquired pneumonia: a prospective observational study. Chest. 2003;123(4):1142–1150. doi: 10.1378/chest.123.4.1142. [DOI] [PubMed] [Google Scholar]
- 24.Hickey R.W., Bowman M.J., Smith G.A. Utility of blood cultures in pediatric patients found to have pneumonia in the emergency department. Ann Emerg Med. 1996;27(6):721–725. doi: 10.1016/s0196-0644(96)70189-0. [DOI] [PubMed] [Google Scholar]
- 25.Myers A.L., Hall M., Williams D.J. Prevalence of bacteremia in hospitalized pediatric patients with community-acquired pneumonia. Pediatr Infect Dis J. 2013;32(7):736–740. doi: 10.1097/INF.0b013e318290bf63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shah S.S., Dugan M.H., Bell L.M. Blood cultures in the emergency department evaluation of childhood pneumonia. Pediatr Infect Dis J. 2011;30(6):475–479. doi: 10.1097/INF.0b013e31820a5adb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iroh Tam P.Y., Bernstein E., Ma X. Blood culture in evaluation of pediatric community-acquired pneumonia: a systematic review and meta-analysis. Hosp Pediatr. 2015;5(6):324–336. doi: 10.1542/hpeds.2014-0138. [DOI] [PubMed] [Google Scholar]
- 28.Blaschke A.J., Heyrend C., Byington C.L. Molecular analysis improves pathogen identification and epidemiologic study of pediatric parapneumonic empyema. Pediatr Infect Dis J. 2011;30(4):289–294. doi: 10.1097/INF.0b013e3182002d14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dien Bard J., McElvania TeKippe E. Diagnosis of bloodstream infections in children. J Clin Microbiol. 2016;54(6):1418–1424. doi: 10.1128/JCM.02919-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Self W.H., Speroff T., Grijalva C.G. Reducing blood culture contamination in the emergency department: an interrupted time series quality improvement study. Acad Emerg Med. 2013;20(1):89–97. doi: 10.1111/acem.12057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hall R.T., Domenico H.J., Self W.H. Reducing the blood culture contamination rate in a pediatric emergency department and subsequent cost savings. Pediatrics. 2013;131(1):e292–e297. doi: 10.1542/peds.2012-1030. [DOI] [PubMed] [Google Scholar]
- 32.Driscoll A.J., Deloria Knoll M., Hammitt L.L. The effect of antibiotic exposure and specimen volume on the detection of bacterial pathogens in children with pneumonia. Clin Infect Dis. 2017;64(suppl_3):S368–S377. doi: 10.1093/cid/cix101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harris A.M., Bramley A.M., Jain S. Influence of antibiotics on the detection of bacteria by culture-based and culture-independent diagnostic tests in patients hospitalized with community-acquired pneumonia. Open Forum Infect Dis. 2017;4(1):ofx014. doi: 10.1093/ofid/ofx014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Isaacman D.J., Karasic R.B., Reynolds E.A. Effect of number of blood cultures and volume of blood on detection of bacteremia in children. J Pediatr. 1996;128(2):190–195. doi: 10.1016/s0022-3476(96)70388-8. [DOI] [PubMed] [Google Scholar]
- 35.Gonsalves W.I., Cornish N., Moore M. Effects of volume and site of blood draw on blood culture results. J Clin Microbiol. 2009;47(11):3482–3485. doi: 10.1128/JCM.02107-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berkley J.A., Lowe B.S., Mwangi I. Bacteremia among children admitted to a rural hospital in Kenya. N Engl J Med. 2005;352(1):39–47. doi: 10.1056/NEJMoa040275. [DOI] [PubMed] [Google Scholar]
- 37.Connell T.G., Rele M., Cowley D. How reliable is a negative blood culture result? Volume of blood submitted for culture in routine practice in a children's hospital. Pediatrics. 2007;119(5):891–896. doi: 10.1542/peds.2006-0440. [DOI] [PubMed] [Google Scholar]
- 38.Byington C.L., Spencer L.Y., Johnson T.A. An epidemiological investigation of a sustained high rate of pediatric parapneumonic empyema: risk factors and microbiological associations. Clin Infect Dis. 2002;34(4):434–440. doi: 10.1086/338460. [DOI] [PubMed] [Google Scholar]
- 39.Hoff S.J., Neblett W.W., Edwards K.M. Parapneumonic empyema in children: decortication hastens recovery in patients with severe pleural infections. Pediatr Infect Dis J. 1991;10(3):194–199. [PubMed] [Google Scholar]
- 40.Picard E., Joseph L., Goldberg S. Predictive factors of morbidity in childhood parapneumonic effusion-associated pneumonia: a retrospective study. Pediatr Infect Dis J. 2010;29(9):840–843. doi: 10.1097/INF.0b013e3181dd1fc4. [DOI] [PubMed] [Google Scholar]
- 41.Brownback K.R., Thomas L.A., Simpson S.Q. Role of bronchoalveolar lavage in the diagnosis of pulmonary infiltrates in immunocompromised patients. Curr Opin Infect Dis. 2014;27(4):322–328. doi: 10.1097/QCO.0000000000000072. [DOI] [PubMed] [Google Scholar]
- 42.Thea D.M., Seidenberg P., Park D.E. Limited utility of polymerase chain reaction in induced sputum specimens for determining the causes of childhood pneumonia in resource-poor settings: findings from the Pneumonia Etiology Research for Child Health (PERCH) Study. Clin Infect Dis. 2017;64(suppl_3):S289–S300. doi: 10.1093/cid/cix098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Murdoch D.R., Morpeth S.C., Hammitt L.L. The diagnostic utility of induced sputum microscopy and culture in childhood pneumonia. Clin Infect Dis. 2017;64(suppl_3):S280–S288. doi: 10.1093/cid/cix090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Murdoch D.R., Laing R.T., Mills G.D. Evaluation of a rapid immunochromatographic test for detection of Streptococcus pneumoniae antigen in urine samples from adults with community-acquired pneumonia. J Clin Microbiol. 2001;39(10):3495–3498. doi: 10.1128/JCM.39.10.3495-3498.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dowell S.F., Garman R.L., Liu G. Evaluation of Binax NOW, an assay for the detection of pneumococcal antigen in urine samples, performed among pediatric patients. Clin Infect Dis. 2001;32(5):824–825. doi: 10.1086/319205. [DOI] [PubMed] [Google Scholar]
- 46.Pride M.W., Huijts S.M., Wu K. Validation of an immunodiagnostic assay for detection of 13 Streptococcus pneumoniae serotype-specific polysaccharides in human urine. Clin Vaccine Immunol. 2012;19(8):1131–1141. doi: 10.1128/CVI.00064-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Resti M., Micheli A., Moriondo M. Comparison of the effect of antibiotic treatment on the possibility of diagnosing invasive pneumococcal disease by culture or molecular methods: a prospective, observational study of children and adolescents with proven pneumococcal infection. Clin Ther. 2009;31(6):1266–1273. doi: 10.1016/j.clinthera.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 48.Clark J.E. Determining the microbiological cause of a chest infection. Arch Dis Child. 2015;100(2):193–197. doi: 10.1136/archdischild-2013-305742. [DOI] [PubMed] [Google Scholar]
- 49.Morpeth S.C., Deloria Knoll M., Scott J.A.G. Detection of pneumococcal DNA in blood by polymerase chain reaction for diagnosing pneumococcal pneumonia in young children from low- and middle-income countries. Clin Infect Dis. 2017;64(suppl_3):S347–S356. doi: 10.1093/cid/cix145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Azzari C., Cortimiglia M., Moriondo M. Pneumococcal DNA is not detectable in the blood of healthy carrier children by real-time PCR targeting the lytA gene. J Med Microbiol. 2011;60(Pt 6):710–714. doi: 10.1099/jmm.0.028357-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Abdullahi O., Nyiro J., Lewa P. The descriptive epidemiology of Streptococcus pneumoniae and Haemophilus influenzae nasopharyngeal carriage in children and adults in Kilifi district, Kenya. Pediatr Infect Dis J. 2008;27(1):59–64. doi: 10.1097/INF.0b013e31814da70c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Spuesens E.B., Fraaij P.L., Visser E.G. Carriage of Mycoplasma pneumoniae in the upper respiratory tract of symptomatic and asymptomatic children: an observational study. PLoS Med. 2013;10(5):e1001444. doi: 10.1371/journal.pmed.1001444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Self W.H., Williams D.J., Zhu Y. Respiratory viral detection in children and adults: comparing asymptomatic controls and patients with community-acquired pneumonia. J Infect Dis. 2016;213(4):584–591. doi: 10.1093/infdis/jiv323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jansen R.R., Wieringa J., Koekkoek S.M. Frequent detection of respiratory viruses without symptoms: toward defining clinically relevant cutoff values. J Clin Microbiol. 2011;49(7):2631–2636. doi: 10.1128/JCM.02094-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ampofo K., Bender J., Sheng X. Seasonal invasive pneumococcal disease in children: role of preceding respiratory viral infection. Pediatrics. 2008;122(2):229–237. doi: 10.1542/peds.2007-3192. [DOI] [PubMed] [Google Scholar]
- 56.Peltola V.T., McCullers J.A. Respiratory viruses predisposing to bacterial infections: role of neuraminidase. Pediatr Infect Dis J. 2004;23(1 Suppl):S87–S97. doi: 10.1097/01.inf.0000108197.81270.35. [DOI] [PubMed] [Google Scholar]
- 57.Fiore A.E., Iverson C., Messmer T. Outbreak of pneumonia in a long-term care facility: antecedent human parainfluenza virus 1 infection may predispose to bacterial pneumonia. J Am Geriatr Soc. 1998;46(9):1112–1117. doi: 10.1111/j.1532-5415.1998.tb06649.x. [DOI] [PubMed] [Google Scholar]
- 58.Randolph A.G., Vaughn F., Sullivan R. Critically ill children during the 2009-2010 influenza pandemic in the United States. Pediatrics. 2011;128(6):e1450–e1458. doi: 10.1542/peds.2011-0774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nguyen T., Kyle U.G., Jaimon N. Coinfection with Staphylococcus aureus increases risk of severe coagulopathy in critically ill children with influenza A (H1N1) virus infection. Crit Care Med. 2012;40(12):3246–3250. doi: 10.1097/CCM.0b013e318260c7f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Voiriot G., Visseaux B., Cohen J. Viral-bacterial coinfection affects the presentation and alters the prognosis of severe community-acquired pneumonia. Crit Care. 2016;20(1):375. doi: 10.1186/s13054-016-1517-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McCullers J.A. Insights into the interaction between influenza virus and pneumococcus. Clin Microbiol Rev. 2006;19(3):571–582. doi: 10.1128/CMR.00058-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dawood F.S., Chaves S.S., Perez A. Complications and associated bacterial coinfections among children hospitalized with seasonal or pandemic influenza, United States, 2003-2010. J Infect Dis. 2014;209(5):686–694. doi: 10.1093/infdis/jit473. [DOI] [PubMed] [Google Scholar]
- 63.Nohynek H., Valkeila E., Leinonen M. Erythrocyte sedimentation rate, white blood cell count and serum C-reactive protein in assessing etiologic diagnosis of acute lower respiratory infections in children. Pediatr Infect Dis J. 1995;14(6):484–490. doi: 10.1097/00006454-199506000-00004. [DOI] [PubMed] [Google Scholar]
- 64.Berg A.S., Inchley C.S., Fjaerli H.O. Clinical features and inflammatory markers in pediatric pneumonia: a prospective study. Eur J Pediatr. 2017;176(5):629–638. doi: 10.1007/s00431-017-2887-y. [DOI] [PubMed] [Google Scholar]
- 65.Hoshina T., Nanishi E., Kanno S. The utility of biomarkers in differentiating bacterial from non-bacterial lower respiratory tract infection in hospitalized children: difference of the diagnostic performance between acute pneumonia and bronchitis. J Infect Chemother. 2014;20(10):616–620. doi: 10.1016/j.jiac.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 66.Van den Bruel A., Thompson M.J., Haj-Hassan T. Diagnostic value of laboratory tests in identifying serious infections in febrile children: systematic review. BMJ. 2011;342:d3082. doi: 10.1136/bmj.d3082. [DOI] [PubMed] [Google Scholar]
- 67.Higdon M.M., Le T., O'Brien K.L. Association of C-reactive protein with bacterial and respiratory syncytial virus-associated pneumonia among children aged <5 years in the PERCH study. Clin Infect Dis. 2017;64(suppl_3):S378–S386. doi: 10.1093/cid/cix150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Flood R.G., Badik J., Aronoff S.C. The utility of serum C-reactive protein in differentiating bacterial from nonbacterial pneumonia in children: a meta-analysis of 1230 children. Pediatr Infect Dis J. 2008;27(2):95–99. doi: 10.1097/INF.0b013e318157aced. [DOI] [PubMed] [Google Scholar]
- 69.Gilbert D.N. Procalcitonin as a biomarker in respiratory tract infection. Clin Infect Dis. 2011;52(Suppl 4):S346–S350. doi: 10.1093/cid/cir050. [DOI] [PubMed] [Google Scholar]
- 70.Linscheid P., Seboek D., Nylen E.S. In vitro and in vivo calcitonin I gene expression in parenchymal cells: a novel product of human adipose tissue. Endocrinology. 2003;144(12):5578–5584. doi: 10.1210/en.2003-0854. [DOI] [PubMed] [Google Scholar]
- 71.Stockmann C., Ampofo K., Killpack J. Procalcitonin accurately identifies hospitalized children with low risk of bacterial community-acquired pneumonia. J Pediatric Infect Dis Soc. 2017 doi: 10.1093/jpids/piw091. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Christ-Crain M., Jaccard-Stolz D., Bingisser R. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet. 2004;363(9409):600–607. doi: 10.1016/S0140-6736(04)15591-8. [DOI] [PubMed] [Google Scholar]
- 73.Bouadma L., Luyt C.E., Tubach F. Use of procalcitonin to reduce patients' exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet. 2010;375(9713):463–474. doi: 10.1016/S0140-6736(09)61879-1. [DOI] [PubMed] [Google Scholar]
- 74.Schuetz P., Briel M., Christ-Crain M. Procalcitonin to guide initiation and duration of antibiotic treatment in acute respiratory infections: an individual patient data meta-analysis. Clin Infect Dis. 2012;55(5):651–662. doi: 10.1093/cid/cis464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Baer G., Baumann P., Buettcher M. Procalcitonin guidance to reduce antibiotic treatment of lower respiratory tract infection in children and adolescents (ProPAED): a randomized controlled trial. PLoS One. 2013;8(8):e68419. doi: 10.1371/journal.pone.0068419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Esposito S., Tagliabue C., Picciolli I. Procalcitonin measurements for guiding antibiotic treatment in pediatric pneumonia. Respir Med. 2011;105(12):1939–1945. doi: 10.1016/j.rmed.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 77.Mejias A., Dimo B., Suarez N.M. Whole blood gene expression profiles to assess pathogenesis and disease severity in infants with respiratory syncytial virus infection. Plos Med. 2013;10(11):e1001549. doi: 10.1371/journal.pmed.1001549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Suarez N.M., Bunsow E., Falsey A.R. Superiority of transcriptional profiling over procalcitonin for distinguishing bacterial from viral lower respiratory tract infections in hospitalized adults. J Infect Dis. 2015;212(2):213–222. doi: 10.1093/infdis/jiv047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mahajan P., Kuppermann N., Mejias A. Association of RNA biosignatures with bacterial infections in febrile infants aged 60 days or younger. JAMA. 2016;316(8):846–857. doi: 10.1001/jama.2016.9207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Heinonen S., Jartti T., Garcia C. Rhinovirus detection in symptomatic and asymptomatic children: value of host transcriptome analysis. Am J Respir Crit Care Med. 2016;193(7):772–782. doi: 10.1164/rccm.201504-0749OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ramilo O., Allman W., Chung W. Gene expression patterns in blood leukocytes discriminate patients with acute infections. Blood. 2007;109(5):2066–2077. doi: 10.1182/blood-2006-02-002477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fine M.J., Auble T.E., Yealy D.M. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336(4):243–250. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 83.Charles P.G., Wolfe R., Whitby M. SMART-COP: a tool for predicting the need for intensive respiratory or vasopressor support in community-acquired pneumonia. Clin Infect Dis. 2008;47(3):375–384. doi: 10.1086/589754. [DOI] [PubMed] [Google Scholar]
- 84.Williams D.J., Zhu Y., Grijalva C.G. Predicting severe pneumonia outcomes in children. Pediatrics. 2016;138(4) doi: 10.1542/peds.2016-1019. [pii:e20161019] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gerber J.S., Kronman M.P., Ross R.K. Identifying targets for antimicrobial stewardship in children's hospitals. Infect Control Hosp Epidemiol. 2013;34(12):1252–1258. doi: 10.1086/673982. [DOI] [PubMed] [Google Scholar]
- 86.Williams D.J., Hall M., Gerber J.S. Impact of a national guideline on antibiotic selection for hospitalized pneumonia. Pediatrics. 2017;139(4) doi: 10.1542/peds.2016-3231. [pii:e20163231] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Handy L.K., Bryan M., Gerber J.S. Variability in antibiotic prescribing for community-acquired pneumonia. Pediatrics. 2017;139(4) doi: 10.1542/peds.2016-2331. [pii:e20162331] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Smith M.J., Kong M., Cambon A. Effectiveness of antimicrobial guidelines for community-acquired pneumonia in children. Pediatrics. 2012;129(5):e1326–e1333. doi: 10.1542/peds.2011-2412. [DOI] [PubMed] [Google Scholar]
- 89.Ambroggio L., Thomson J., Murtagh Kurowski E. Quality improvement methods increase appropriate antibiotic prescribing for childhood pneumonia. Pediatrics. 2013;131(5):e1623–e1631. doi: 10.1542/peds.2012-2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.CAP-IT: Efficacy, safety and impact on antimicrobial resistance of duration and dose of amoxicillin treatment for young children with Community-Acquired Pneumonia (CAP): A randomised controlled trial. 2017; Available at: https://www.capitstudy.org.uk/. Accessed June 28, 2017. [DOI] [PMC free article] [PubMed]
- 91.A Phase IV Double-Blind, Placebo-Controlled, Randomized Trial to Evaluate Short Course vs. Standard Course Outpatient Therapy of Community Acquired Pneumonia in Children (SCOUT-CAP). 2017; https://clinicaltrials.gov/ct2/show/NCT02891915. Accessed June 28, 2017.
- 92.Hicks L.A., Chien Y.W., Taylor T.H., Jr., Active Bacterial Core Surveillance Team Outpatient antibiotic prescribing and nonsusceptible Streptococcus pneumoniae in the United States, 1996-2003. Clin Infect Dis. 2011;53(7):631–639. doi: 10.1093/cid/cir443. [DOI] [PubMed] [Google Scholar]
- 93.Spuesens E.B., Meyer Sauteur P.M., Vink C. Mycoplasma pneumoniae infections–does treatment help? J Infect. 2014;69(Suppl 1):S42–S46. doi: 10.1016/j.jinf.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 94.Biondi E., McCulloh R., Alverson B. Treatment of mycoplasma pneumonia: a systematic review. Pediatrics. 2014;133(6):1081–1090. doi: 10.1542/peds.2013-3729. [DOI] [PubMed] [Google Scholar]