Abstract
Introduction
Exposure to pain management curriculum in medical school is currently variable. This paper reports on formal prescribing education, self-perceived prescribing readiness, and prescribing practices among incoming surgical residents before and after a pain management training session.
Methods
Pre-residency survey of thirty surgical interns at a single urban medical center, followed by a repeat survey after an educational session on prescription writing and opioid abuse.
Results
Thirty-three percent of respondents had formal education on prescription writing in medical school. Median subjective preparedness to write an opioid prescription was 1.5 (range 1–10) on a 1–10 Likert scale. Ranges of morphine milligram equivalents (MME) prescribed varied from 420–2700 MME for 8 mock surgical scenarios. Post-training, median subjective preparedness increased to 3.5 (range 1–6) and prescription accuracy (the inclusion of a medication, dose, frequency, and duration) improved from 75% to 97% (p<.001). Overall, 90% of interns found the training session useful.
Conclusion
Most surgical interns were not trained in prescribing narcotics in medical school. Improved pain management curriculum is necessary to assure safe and consistent opioid prescriptions.
Introduction
According to the Centers for Disease Control and Prevention (CDC), an American dies from an opioid overdose approximately every 23 minutes.1 With opioid abuse plaguing communities across our country, regulatory agencies are finally catching up, implementing new rules and regulations to stop the opioid epidemic. In fact, just last year the Surgeon General created the TurnTheTideRx campaign to encourage all physicians to help end the opioid epidemic through more effective pain management, increased opioid abuse screening, and greater public awareness of addiction as a chronic illness.2
Beyond increased regulations, another critical tool for combatting opioid abuse is ensuring medical school and residency curriculum include prescription education to reduce opioid over-prescribing by physicians.3,4 However, despite some improvements in educational courses, studies have noted that exposure to formal pain management education in medical training continues to be variable.3–6 Additionally, in a review of pain management curriculum in medical schools in the United States, it was found that while 80 percent of medical schools offered one or more pain management education sessions, only 4 percent of medical schools required students to take one of these courses.5 This potential lack of preparedness is concerning given that surgical interns are expected to have knowledge and skills in safe and effective prescribing of medications for post-operative patients from the first day of training. Prescription-writing is a key function of surgical interns, and as a result, it’s imperative that incoming surgical interns are well-versed in prescribing opioid analgesics.
Based on current medical education and training environments, we hypothesized that the preparedness of incoming surgical interns to write opioid prescriptions would be heterogeneous. As part of an educational quality improvement project, we sought to evaluate the exposure to pain management curriculum prior to residency, assess the readiness to prescribe opioid prescriptions and determine the effect of our educational curriculum in a cohort of incoming surgical interns.
Methods
This educational quality improvement project was approved by the Institutional Review Board at Northwestern University. We surveyed 30 surgical interns amongst varying surgical subspecialties at a single urban medical center during their surgical “boot camp” orientation, which occurred in June 2016. The survey (Appendix A) assessed three separate domains: (1) self-perceived readiness to prescribe opioids; (2) relevant formal education in medical school; and (3) current beliefs regarding the appropriate opioid dose and quantity to prescribe following common surgical procedures. All surveys were voluntarily completed and anonymous. After 8 weeks, 12 surgical interns from the initial cohort attended a half hour training session on prescription writing fundamentals and opioid abuse led by a senior general surgery resident. Due to differences in surgical subspecialties in the timing of protected educational time for interns, only interns within the Department of Surgery were available for our training session and included in the follow-up survey. Immediately following the training session, this group was given the same survey they had completed during residency orientation. Additionally, this group of interns was also asked if they found the training session useful and whether they would change their prescribing practices.
Participants were asked to rank their subjective readiness to prescribe opioids for patients being discharged after surgery on a 1 to 10 Likert scale (1 was not-at-all prepared and 10 was very-well prepared). Questions regarding their formal training prior to residency included whether or not interns had education specific to prescription writing, opioid abuse and misuse, and opioid-specific (or controlled substance specific) prescription writing. Finally, interns were asked to hand write a mock discharge prescription for eight surgical procedures. The surgeries included laparoscopic cholecystectomy, laparoscopic appendectomy, open inguinal hernia repair, laparoscopic right colectomy, thyroidectomy, breast lumpectomy without sentinel lymph node biopsy, wide local excision (9 cm × 3 cm wound), and great saphenous vein ligation and stripping with microphlebectomy (10–20 stabs). Interns were prompted that they could prescribe “no opioid analgesics” or prescribe an opioid in the form of hydrocodone/acetaminophen limited to the strengths of 5/325 mg, 7.5/325 mg, or 10/325 mg. If the resident chose to prescribe an opioid, the morphine milligram equivalents (MME) of each opioid prescription were tabulated by multiplying the strength, frequency, and duration of the prescription. If essential elements of the prescription were incomplete–specifically, the type of medication, dose, frequency of administration, and duration of use–then the prescription was marked inaccurate.
Continuous variables were compared with Student’s t-test or the Kruskal-Wallis test as appropriate, categorical variables were compared with chi-square test or Fisher’s exact test as appropriate. Data was stored and managed in Microsoft Excel (Microsoft Corp, Redmond, WA) and analyses were completed in STATA version 14 (STATA Corp, College Station, TX).
Results
Pre-Residency Prescription Writing Education
When asked about medical school exposure to relevant pain management topics, 60% (N=18) of residents reported having exposure to education on opioid abuse, 40% (N=12) reported having focused education on prescription writing basics, and 33% (N=10) reported having training on opioid prescribing (Table 1).
Table 1.
Medical School Exposure to Prescription Writing, Opioid abuse and Misuse, and Opioid-Specific Prescribing
| Baseline | |||
|---|---|---|---|
| N | % | ||
| Total Interns | 30 | ||
| Medical School Exposure: | |||
| Prescription Writing | |||
| Yes | 12 | 40.0% | |
| No | 18 | 60.0% | |
| Opioid Abuse Awareness | |||
| Yes | 18 | 60.0% | |
| No | 12 | 40.0% | |
| Analgesic Prescription Practice | |||
| Yes | 10 | 33.3% | |
| No | 20 | 66.7% | |
Perceived preparedness to prescribe opioids
Incoming surgical residents reported a median readiness of 1.5 (range 1–10) to write opioid prescriptions (Figure 1). The effect of perceived opioid prescribing preparedness on prescription completeness in the pre-training cohort was evaluated by comparing participants with “low” subjective preparedness (1–3) versus those with “moderate” (4–6) and “high” preparedness (7–10). We found that those who felt moderately to highly prepared were more likely to write an accurate prescription (OR 2.09, 95% CI 1.06–4.09; p<.02). While there was a trend toward increasing preparedness among the 12 interns in the post-training group with a median score of 3.5 (range 1–6), this was not significantly different from the pre-training group (p=0.25).
Figure 1.
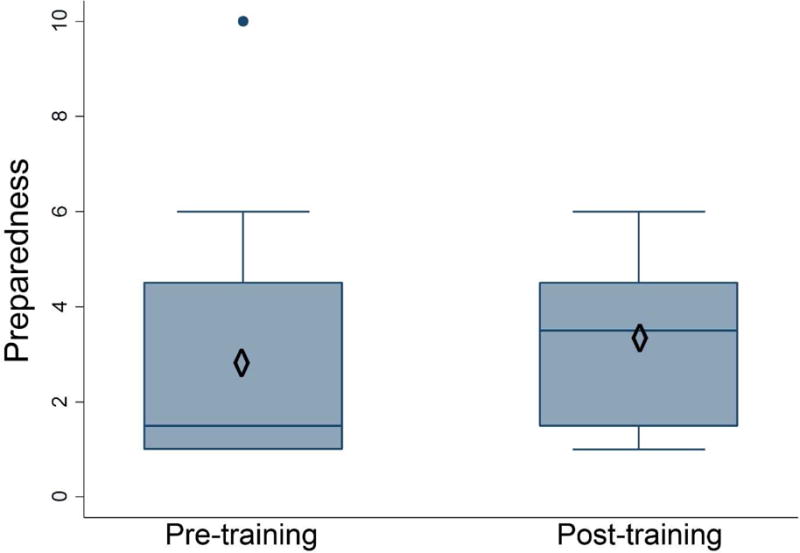
Box-and-whisker plot of subjective preparedness
Diamond: Mean
Dark Line: Median
Mock Prescriptions
There was wide variation in the number of pills and overall morphine milligram equivalents prescribed for all surgical scenarios both before and after the training session (Figure 2 and Table 2, respectively). Despite 7 % of interns reporting that they would prescribe less opioids after the training session, we noted a trend of increasing median MME for 6 procedures following the training session. We also observed a consistently wide variation in the quantity and dose of opioids prescribed for all operations. This was most prominent amongst the laparoscopic right colectomy with a range of 0 to 2700 MMEs.
Figure 2.
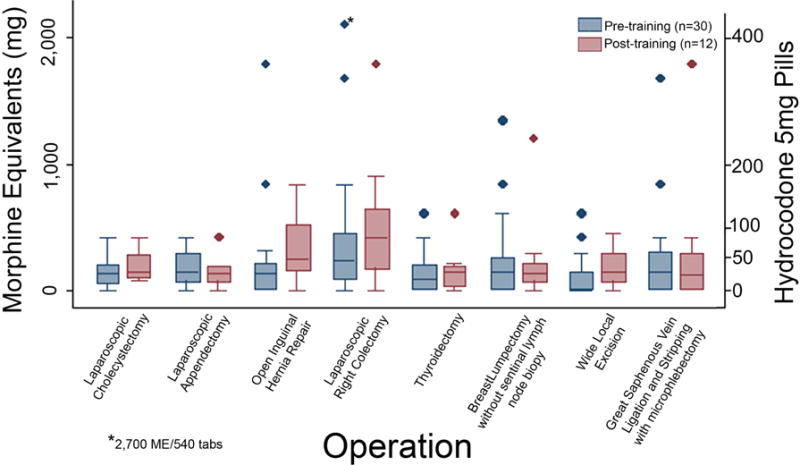
Box-and-whisker plot of Morphine Mg Equivalents (MME) prescribed for mock surgical scenarios
Table 2.
Morphine milligram equivalents (MME) prescribed for eight mock surgical scenarios.
| Operation | MME: pre-intervention (median, min, max) | MME: post-intervention median, (min, max) | P valuea |
|---|---|---|---|
| Laparoscopic cholecystectomy | 120(0–420) | 140(60–420) | 0.25 |
| Laparoscopic appendectomy | 130(0–420) | 130(0–420) | 0.87 |
| Open inguinal hernia | 120(0–1800) | 240(0–840) | 0.05 |
| Laparoscopic right colectomy | 225(0–2700) | 420(0–1800) | 0.43 |
| Thyroidectomy | 75(0–600) | 140(0–600) | 0.67 |
| Breast lumpectomy without sentinel lymph node biopsy | 140(0–1350) | 130(0–1200) | 0.97 |
| Wide local excision | 0(0 – 600) | 140(0–450) | 0.10 |
| Great saphenous vein ligation and stripping with microphlebectomy | 145(0–1680) | 1100(0–1800) | 0.90 |
Intergroup difference was tested by using Wilcoxon rank sum test.
Non-opioid analgesics were prescribed in 22% of the pre-training prescriptions compared to 14% of the post-training prescriptions (OR 0.40, 95% CI 0.20–0.81; P<0.01), despite encouraging non-opioid analgesic prescribing as part of the training session. Overall, 25% of all mock prescriptions from the pre-training cohort did not include a frequency or duration, rendering them inaccurate (Figure 3). After the training session, interns were less likely to write an inaccurate prescription, as only 3% of mock prescriptions were invalid (OR 0.10, 95% CI 0.2–0.32; p<.01).
Figure 3.
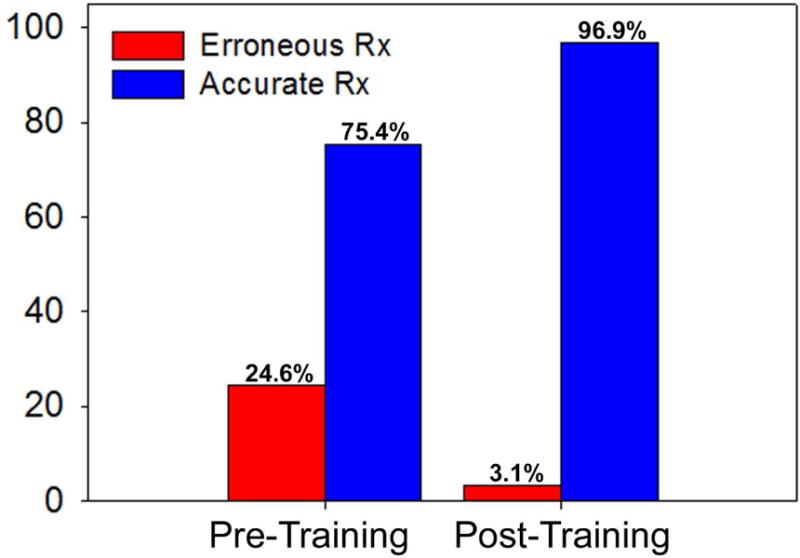
Prescription accuracy before and after intern training session
After the training session, interns were less likely to write an invalid prescription (OR 0.10, 95% CI 0.2–0.32, p<.01).
Usefulness of Training
Overall, 90% (9 of 10 responders) of the interns found the training session useful and 73% (8 of 11 responders) of the interns would have preferred for this session to be included in the pre-residency orientation. Post-training, 73% of interns felt they would prescribe fewer opioids and 27% of interns felt they would write the same dosage of opioids.
Discussion
The main purpose of this study was to determine the exposure of incoming surgical interns to pain management curriculum and their perceived readiness to prescribe opioid analgesics. The findings from this study are in line with the reported literature, with low and variable rates of formal education on general prescription-writing, opioid prescription-writing, and opioid abuse while in medical school. Not surprisingly, the perceived readiness to write opioid prescriptions for postoperative patients was low with most interns who reported that they did not feel at all prepared. Their perceived lack of readiness was confirmed by the fact that 25% of all mock prescriptions were inaccurate prior to our educational intervention.
Since incoming interns’ exposure to pain management education in medical school is limited, we would recommend residency programs integrate some formal training into their pre-residency curriculum. In our cohort, we were encouraged by the fact that after the pain management course, 90% of respondents reported the activity as useful. As a result, we have since integrated this training into the residency orientation as requested by our interns. We have also modified our curriculum to more heavily stress the beneficial use of non-opioid analgesics as adjuncts to opioid use.
In addition, it’s worth noting that other recent educational interventions have been shown to successfully alter opioid-prescribing practices.7 In a study, Hill and colleagues evaluated opioid use after 5 surgical procedures to determine prescription guidelines, in conjunction with emphasizing greater use of nonsteroidal anti-inflammatory drugs and acetaminophen, which then would be discussed with attending surgeons at their institution. After comparing prescriptions for 246 subsequent patients, they determined a 53% decrease in opioid tablets prescribed. More surprisingly, only one patient required a refill prescription. These results indicate that successful institutional change may require a top-down educational approach to be effective.
Given our initial survey findings, we implemented a training session on prescription writing and opioid abuse awareness to improve subjective preparedness and prescription accuracy, and also to decrease variability in the number of pills and strength of opioids prescribed. At this training session, the essentials of a complete prescription and data from the CDC on opioid abuse were reviewed.1 Additionally, the resident facilitator emphasized the use of multi-modal analgesic therapy with non-opioid analgesics such as nonsteroidal anti-inflammatory drugs, acetaminophen, ice packs, and epidural anesthesia when appropriate. Unfortunately, at the time of our intern training session, there were no guidelines as to the number and strength of opioid that should be discharged for standard procedures, and therefore we did not provide specific recommendations on dose or quantity. This may explain why there was no statistically significant difference between the dose and quantity of opioid prescribed by interns before versus after our intervention.
Current guidelines on the treatment of pain by the CDC and the American Society of Anesthesiologists lack data regarding the average amount of opioids consumed by patients for common surgical procedures, and our findings suggest this may be a critical element to help guide post-operative prescribing.8,9 In this vein, Gerbershagen and colleagues endorsed procedure-specific pain management as they determined that pain intensity scores were not directly correlated to the invasiveness of a procedure.10 Furthermore, multiple studies evaluating opioid use after a spectrum of surgical procedures have found that patients are consistently prescribed more opioids than they end up consuming.11–14 Therefore, we have evolved our educational intervention to serve as a mastery curriculum occurring during our pre-residency orientation boot camp that specifically will highlight the suggested strength and quantity of opioids now supported by published research.13
While the responsibility of discharge prescriptions will continue to vary among each medical center and, specifically, each surgical service, we wanted to acknowledge that young doctors are often accountable for discharge prescriptions at academic medical centers. At our institution, Interns frequently write discharge prescriptions for less complex outpatient operations into which they can scrub alone with their attending surgeons. Arguably, every interns’ prescribing practices will be influenced by their senior resident and attending surgeon, who will each have individual habits. A startling trend in our study was the almost universal increase in opiate pain medications and concomitant decrease in non-opiate adjunctive pain medication after eight weeks of clinical training and targeted education on the risks of opioid over-prescribing. This may be due to increased comfort of prescribing opioids after a brief clinical experience, or alternatively, it could be attributed to the influence of an established culture of opioid prescribing that already exists. Both the increased comfort and “established-culture” phenomenon may explain why their prescribing trends are refractory to the dedicated education session, despite the majority of residents intending to write fewer opioids. To evaluate the effect of the “established-culture” phenomenon, we are currently analyzing whether the trends in mock prescriptions among our interns mirrors actual discharge practices from the previous year.
This study has some notable limitations. As a single-institution study, the study has an evident sampling bias and results may not accurately reflect surgical residents at other institutions. Furthermore, the sub-cohort that received the training session was only part of the initial cohort, and in future educational interventions at the orientation boot camp, we plan to include all incoming surgical interns. Moreover, we recognize that low preparedness in opioid prescription-writing may not reflect readiness to use the electronic medical record (EMR) to generate a prescription, as the EMR often prompts the user to complete missing information that would otherwise render the prescription invalid. It’s understandable that eight weeks of surgical training and prescription-writing experience could have had a significant influence on the preparedness of the post-educational cohort responses and their ability to write valid prescriptions. That said, we were encouraged that the overwhelming majority of the interns found the training session helpful and felt that the additional training would have been useful during residency orientation. While our resident survey was not validated prior to distribution, we felt that it clearly highlighted a critical gap in training that we hope to bring awareness to at our institution and beyond. Lastly, we acknowledge that opioid prescribing should be determined by numerous patient-specific and perioperative variables, including but not limited to: each patient’s past medical and surgical history, previous opioid use, and individual pain tolerance. Only after thorough clinical assessment can a provider determine an appropriate discharge prescription and some of these nuances were beyond the scope of our brief educational intervention.
Conclusion
This study suggests that a majority of incoming surgical residents are not adequately prepared to write opioid prescriptions and that, even following a brief training session on appropriate opioid prescribing, a wide range in the number of pills and total morphine milligram equivalents prescribed persist. Until medical schools catch up to ensure training of this core clinical skill, we would recommend residency programs integrate prescription-writing and opioid-specific education into their pre-residency curriculum. Further research is needed to develop and evaluate training that reliably and sustainably improves knowledge and attitudes about appropriate opioid prescribing among incoming surgical residents.
Highlights.
33% (N=18) of residents had exposure to opioid prescribing education in medical school.
Incoming surgical residents reported a median readiness of 1.5 (range 1–10) to write opioid prescriptions.
Ranges of morphine milligram equivalents (MME) prescribed varied from 420–2700 MME for 8 mock surgical scenarios.
Overall, 90% of interns found the training session useful.
Acknowledgments
Work reported in this publication was partially supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number T32HL094293 in the form of partial stipend support for author MJN and NAM. The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors would also like to acknowledge Dr. Jane Holl for her assistance in critically reviewing this manuscript.
Appendix A: Prescription Questionnaire
We want to know what amount of opioid analgesics you would plan to prescribe for a variety of common surgical procedures.
For the following operations, you can answer with:
“No opioid analgesics, only non-opioid analgesics” (ie. tylenol/NSAIDs)
OR
If you would prescribe an opioid analgesic we want to know what strength, dose, frequency, and duration you would prescribe.
For ease, your opioid analgesic options at the local pharmacy are limited to:
Norco (hydrocodone/acetaminophen) in the following formulations:
5/325mg, 7.5/325mg, and 10/325mg
Doses: 1 or 2 tabs
Frequency: Q4 or Q6 hours
Duration: As many days as you feel appropriate
Laparoscopic cholecystectomy
Laparoscopic appendectomy
Unilateral open inguinal hernia repair
Laparoscopic-assisted right colectomy
Thyroidectomy
Breast lumpectomy without sentinel lymph node biopsy
Upper or lower extremity wide local excision for melanoma (length of elliptical wound is 9cm×3cm)
Unilateral great saphenous vein ligation and stripping with microphlebectomy (10–20 stabs)
The following 3 questions can be answered with a “Yes, No, or cannot recall” response:
As a medical student, did your medical school have lectures regarding the opioid crisis in the United States?
Did your medical school have lectures regarding prescription writing?
Did your medical school have lectures regarding opioid prescription writing?
-
On a scale of 1–10, 1 being unprepared and 10 being highly informed and prepared, how prepared do you feel to prescribe opioid analgesics?
(The following questions were included in the post-training survey)
Did you find the opioid abuse awareness and prescription writing review helpful? Yes or No
Would you have liked to have a similar session during your pre-residency orientation? Yes or No
Do you think your prescription writing habits will be changed after this lecture?
- How do you think your prescribing pattern will be after this lecture:
- I will prescribe more opioids
- I will prescribe the same amount of opioids
- I will prescribe fewer opioids
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. Wide-ranging online data for epidemiologic research (WONDER) Atlanta, GA: CDC, National Center for Health Statistics; 2016. http://wonder.cdc.gov Last accessed June 23, 2017. [Google Scholar]
- 2.Murthy VH. Surgeon General's Report on Alcohol, Drugs, and Health. JAMA: the journal of the American Medical Association. 2017;317:133–4. doi: 10.1001/jama.2016.18215. [DOI] [PubMed] [Google Scholar]
- 3.Chen I, Goodman B, Galicia-Castillo M, Quidgley-Nevares A, Krebs M, Gliva-McConvey G. The EVMS pain education initiative: a multifaceted approach to resident education. J Pain. 2007;8:152–60. doi: 10.1016/j.jpain.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 4.Elhwairis H, Reznich CB. An educational strategy for treating chronic, noncancer pain with opioids: a pilot test. J Pain. 2010;11:1368–75. doi: 10.1016/j.jpain.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 5.Mezei L, Murinson BB, Team JHPCD Pain education in North American medical schools. J Pain. 2011;12:1199–208. doi: 10.1016/j.jpain.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 6.Khidir H, Weiner SG. A Call for Better Opioid Prescribing Training and Education. West J Emerg Med. 2016;17:686–9. doi: 10.5811/westjem.2016.8.31204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hill MV, Stucke RS, McMahon ML, Beeman JL, Barth RJ., Jr An Educational Intervention Decreases Opioid Prescribing After General Surgical Operations. Annals of surgery. 2017 doi: 10.1097/SLA.0000000000002198. [DOI] [PubMed] [Google Scholar]
- 8.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain-United States, 2016. MMWR Recomm Rep. 2016;65:1–49. doi: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 9.American Society of Anesthesiologists Task Force on Acute Pain M. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2012;116:248–73. doi: 10.1097/ALN.0b013e31823c1030. [DOI] [PubMed] [Google Scholar]
- 10.Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013;118:934–44. doi: 10.1097/ALN.0b013e31828866b3. [DOI] [PubMed] [Google Scholar]
- 11.Mutlu I, Abubaker AO, Laskin DM. Narcotic prescribing habits and other methods of pain control by oral and maxillofacial surgeons after impacted third molar removal. J Oral Maxillofac Surg. 2013;71:1500–3. doi: 10.1016/j.joms.2013.04.031. [DOI] [PubMed] [Google Scholar]
- 12.Rodgers J, Cunningham K, Fitzgerald K, Finnerty E. Opioid consumption following outpatient upper extremity surgery. J Hand Surg Am. 2012;37:645–50. doi: 10.1016/j.jhsa.2012.01.035. [DOI] [PubMed] [Google Scholar]
- 13.Hill MV, McMahon ML, Stucke RS, Barth RJ., Jr Wide Variation and Excessive Dosage of Opioid Prescriptions for Common General Surgical Procedures. Annals of surgery. 2017;265:709–14. doi: 10.1097/SLA.0000000000001993. [DOI] [PubMed] [Google Scholar]
- 14.Bates C, Laciak R, Southwick A, Bishoff J. Overprescription of postoperative narcotics: a look at postoperative pain medication delivery, consumption and disposal in urological practice. J Urol. 2011;185:551–5. doi: 10.1016/j.juro.2010.09.088. [DOI] [PubMed] [Google Scholar]


