Abstract
Background and aims
The selective removal of tattoos and benign cutaneous pigmented lesions with laser energy evolved rapidly with the development of the nanosecond-domain Q-switched laser (ns-laser). Recently, however, a series of picosecond-domain lasers (ps-lasers) with pulsewidths less than 1 ns has become commercially available, enabling more efficient and faster removal of pigmented lesions in the field of dermatologic laser surgery.
Rationale behind the ps-laser
The efficacy of the ns-laser depended on the theory of selective photothermolysis, whereby an extremely short pulse width was delivered less than the thermal relaxation time (TRT) of a target. At sub-ns pulsewidths, i.e. in the ps-domain, this efficacy is dramatically extended through defeating the stress relaxation time (SRT) of a target allowing for even more effective pigment destruction with even less damage to the surrounding normal tissue. This will be discussed in detail.
Clinical applications
The ps-laser has been reported as achieving tattoo removal in fewer sessions than the ns-laser, with less in the way of unwanted side effects. Tattoos recalcitrant to ns-laser treatment have responded well to the ps-laser, and although true ‘color blindness’ is not yet completely achieved with the ps-domain pulses currently available, multicolored tattoos have also responded very favorably. The ability to limit damage precisely to the pigment target gives greater efficacy in treatment of epidermal lesions with less induction of post-inflammatory hyperpigmentation in the PIH-susceptible Asian skin, and dermal melanocytosis also respond very well to ps-laser treatment. Illustrative clinical examples from the author's experience are given.
Conclusions
Current ps-lasers could be a revolutionary advance for laser tattoo removal but may be less effective for some specific aesthetic indications such as melasma and other cosmetic procedures. Manufacturers must make an effort to reduce the current comparatively long ps-domain pulsewidths to deliver a ‘true’ ps-domain laser, with more basic studies also being required to allow expansion of the safe and effective use of the ps-laser outside of tattoo removal.
Keywords: tattoo, Q-switched laser, picosecond laser, photothermal reaction, photoacoustic reaction
Introduction
The background behind the appearance of picosecond lasers
The history of the evolution of short pulsed lasers: For the treatment of cutaneous pigmented lesions, two types of laser emission mode may be used. One is continuous wave lasers (CWL), and the other is the pulsed laser (PL). If the purpose of the treatment is to vaporize or ablate living tissue from the surface of the target, the distinction between the two could be small. However, if a selective destruction of a certain structure were the purpose, the use of a PL would be advantageous. According to the theory of selective photothermolysis proposed by Anderson and Parrish, two conditions are required to selectively destroy a target: 1). The laser energy must be at a wavelength which is highly absorbed by the target relative to the surrounding normal tissue; and 2: The pulse duration used must be shorter than the time it takes for heat to escape through conduction.
Based on this theory, three types of laser have been realized which enabled dramatic improvements in clinical results in the treatment of pigmented targets. Firstly is the pulsed dye laser which targets the hemoglobin in dermal capillaries. The wavelength in the vicinity of 590 nm and a pulse duration of 0.5∼3 ms, made possible the treatment of port-wine stains and telangiectasia. Secondly are the nanosecond Q-switched lasers (ns-lasers) selectively targeting pigmented lesions including tattoo pigments and dermal melanocytosis. The ns-domain Q-switched ruby laser (QSRL/694 nm, 20 ns), the Q-switched alexandrite laser (QSAL/755 nm, 50 ns) and the Q-switched Nd:YAG laser (QSYL/1064 nm, 5∼10 ns) are 3 PLs that made the treatment of tattoos and difficult dermal melanocytic lesions such as nevus of Ota, possible. Thirdly are the various long-pulsed hair removal lasers, such as the alexandrite (755 nm), diode (810/940 nm) and Nd:YAG (1064 nm) used at pulse durations ranging from 2∼100 msec. These made it possible for near permanent epilation through selective destruction of hair follicles. The clinical application of these 3 types of PLs secured the position of lasers in the field of dermatologic surgery.
The establishment and limitations of nano-second Q switched lasers: During the period from 1990 to 1994, the clinical application of these lasers came in succession and their efficacies were reported 2–4). Prior to this period, lasers were thought to be capable of treating lesions limited to the skin surface and it came as a surprise to everyone that lasers were in fact capable of selectively destroying intra-dermal pigments such as tattoo pigments. These lasers spread throughout the world quickly and the efficacy of laser tattoo removal became a proven fact. In Asian countries where dermal melanocytosis such as nevus of Ota are prevalent, the efficacy of lasers for not only dermal melanocytosis but also for epidermal lesions such as solar lentigines, secured the role of lasers as the king of treatment for benign cutaneous pigmented lesions 5). Presently the three types of Q-switched lasers, the QSRL, QSAL and QSYL, are considered the definitive treatment method for tattoos and dermal melanocytosis and as for the treatment of regular nevus of Ota and acquired dermal melanocytosis, complete clearance is expected within a number of treatments. However, in the treatment of tattoos, although lasers are effective in most cases, there are examples where numerous treatments are required, where specific colors resist treatment or where disturbing pigmentary changes follow laser irradiation 6, 7) and methods to improve these phenomena were eagerly sought after.
Clinical application of picosecond lasers: The possibility of improving the clinical results for tattoo removal by creating lasers with pulse widths in the order of less than 1 ns (1.0 ns =10−9 s) was reported relatively early on in the late 1990s with an experimental laboratory-based ps-laser 8). However, in the subsequent 15 years, no similar ps-laser hardware became commercially available. Only recently, based on newly developed cavity technology, lasers such as the PicoSure (755 nm/750 ps) was released by Cynosure Inc. in 2012, followed by enLIGHTen (1064 nm, 532 nm/750 ps) by Cutera Inc. and PicoWay (1064 nm, 532 nm/450 ps, 375 ps) by Syneron Candela Inc. in 2013. Presently a variety of laser manufacturers are marketing ps-lasers. These ps-lasers are superior regarding the removal of tattoos compared to the ns-domain Q switched lasers 9), and removal of previously difficult tattoo colors 10–12) with less hyperpigmentation 13) has also been reported. On the other hand, the treatment of dermal melanocytosis and other pigmented nevi as well as cosmetic laser procedures has been attempted but to date, few definitive and conclusive studies have been reported.
Theoretical background of picosecond lasers
Thermal lock-in (Thermal relaxation theory)
The thermal relaxation theory is based on the following proven phenomenon. If a certain structure is heated to a certain temperature, heat escapes to the surrounding tissue through heat conduction and if the heating takes place over a longer period, heat escapes while the structure is being heated and thus the temperature rise of the target structure is limited. Such a condition is called heat diffusion (Fig. 1 (a)). However if the structure is heated in a very short exposure time, the temperature rises quickly since there is no time for the heat to diffuse. This condition is called thermal lock-in (Fig. 1 (b)) 14, 15). Once thermal lock-in is achieved selective thermal destruction of the structure becomes possible. Whether or not thermal lock-in is achieved depends on the temporal threshold of the structure which is called the coefficient of thermal relaxation, or more simply, the thermal relaxation time (TRT), and the TRT depends on the absorption coefficient and heat diffusion coefficient of the structure.
Fig. 1.
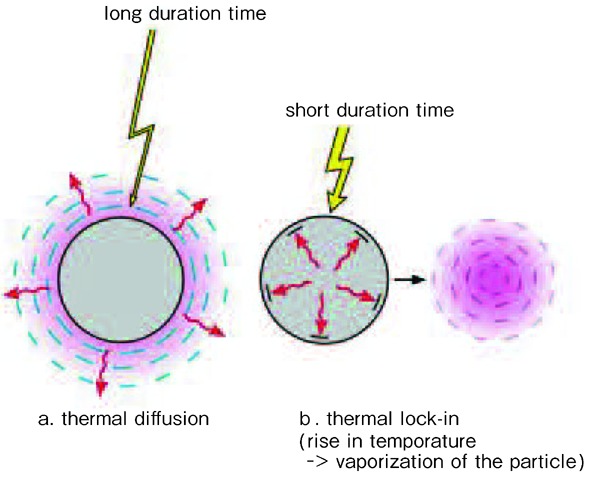
Mechanism of thermal lock-in. (Reproduced with permission from reference #14) (a) Thermal diffusion: Thermal infusion with a long period of time results in thermal diffusion. (b) Thermal lock-in: Thermal infusion within a short time results in thermal lock-in causing rise in temperature and vaporization of particle.
Stress lock-in (Stress relaxation time theory):
In tattoo removal using the ns-domain Q switched lasers, it is argued that the pulse duration of the laser is shorter than the thermal relaxation time of the tattoo pigments and thus thermal lock-in is achieved. However at the same time, another important phenomenon called stress lock-in must be taken into consideration.
Stress relaxation can be explained simply as follows. When a certain particle is heated, thermal expansion of the particle occurs. The expansion diffuses to the surrounding tissue as vibration which is called stress diffusion (Fig. 2 (a)). When a particle is heated within an extremely short period of time, the stress generated within the particle has not enough time to diffuse and stress lock-in is achieved, 14, 15) and if the generated stress is high enough, fracture of the particle occurs. This is analogous to the thermal lock-in and extreme temperature rise in the thermal relaxation theory. The temporal threshold of the particle for stress lock-in to occur, the stress relaxation time (SRT), for tattoo pigments is thought to be slightly shorter than 1 ns. Therefore in tattoo removal using ns-domain Q-switched lasers, stress lock-in is not achieved since the pulse width of the lasers is longer than the stress relaxation time of the tattoo pigments. However when a ps-laser is used which can defeat the SRT, stress lock-in is achieved.
Fig. 2.
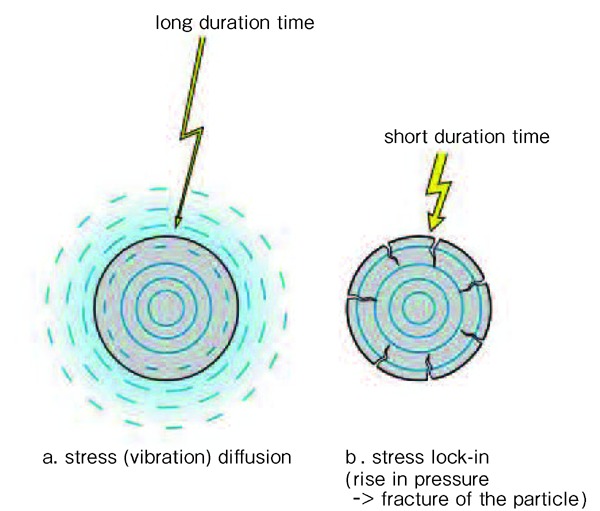
Mechanism of stress lock-in. ( Reproduced with permission from reference #14). (a) Stress diffusion: Mechanical stress generated with a long period of time results in stress (vibration) diffusion. (b) Stress lock-in: Mechanical stress generated within a very short period of time results in stress lock-in causing rise in pressure and fracture of the particle.
The different reactions comparing a ps-laser to an ns-laser can be summed up as follows. When an ns-domain Q-switched laser is used, the major reaction which takes place is photothermolysis through a photothermal reaction, with a very small photomechanical effect. However when a ps-laser is used, stress lock-in occurs and the major reaction involves the photoacoustic destruction of the particle, with a minor photothermal component. Therefore more efficient and effective destruction of the particle becomes possible. Also, since heat generation through light absorbance decreases, color dependence for the reactions decreases as well. It is anticipated that the less heat generation will lead to less heat induced complications such as discoloration of the tattoo. Such tendencies have already been seen in some clinical settings but have yet to be confirmed comprehensively.
Clinical indications for picosecond lasers
Tattoos
The higher efficacy of the ps- laser compared to the ns-laser in removal of tattoos is gaining wider recognition. The author has been using a ps-domain alexandrite laser clinically (Pico-Alex: 755 nm/550–750 ps), the PicoSure system from Cynosure Inc., since February of 2014, and a ps-domain Nd:YAG (Pico-YAG: 1064, 532 nm/450, 350 ps) also PicoWay from Syneron Candela Inc., since May of 2015. The impression given to the author by these ps-lasers has been that they are far more effective for tattoo removal compared to the ns-domain Q-switched lasers (QSRL, QSYL, QSAL). For the removal of black pigmented tattoos the picosecond lasers are more than twice as effective (meaning that less than half the number of treatments are required to completely remove the tattoo) and are several times more effective in removal of multi-colored tattoos, compared to the ns-domain Q-switched lasers. Please refer to the following cases.
Case 1. 28-year-old male patient. Tattoo on the forearm (Fig. 3 (a)) Two months after 4 treatments using the Pico-Alex, the tattoo has been almost completely removed (Fig. 3 (b)). Several more treatments would most likely have been required if a ns-domain Q-switched laser had been used.
Fig. 3.

Case 1, tattoo on the forearm. (a) Before treatment, (b) Two months after 4 times treatment by Pico-Alex. (For interpretation of the references to color in this figure legend, the reader is refered to the web version of this article.)
Case 2. 41-year-old male patient. Tattoo on the back (Fig. 4 (a)). Two months after 1 treatment using QSYL + 5 treatments using Pico-Alex. The tattoo pigments were almost completely removed with transient cutaneous hyperpigmentation remaining (Fig. 4 (b)). The hyperpigmentation could be expected to resolve spontaneously in roughly a year. Several more treatments would probably have been required if a ns-domain Q-switched laser had been used.
Fig. 4.

Case 2, tattoo on the back. (a) Before treatment, (b) Two months after 1 time QSYL treatment and 5 times Pico-Alex treatment. (For interpretation of the references to color in this figure legend, the reader is refered to the web version of this article.)
Case 3. 25-year-old female patient. Tattoo on the chest (Fig. 5 (a)). Two months after a single treatment with Pico-Alex. The blue and purple pigments were completely removed (Fig. 5 (b)). As seen in this case the Pico-Alex is extremely effective for the removal of blue and purple pigments. Such a swift and complete removal would most probably be impossible when using ns-domain Q switched lasers.
Fig. 5.
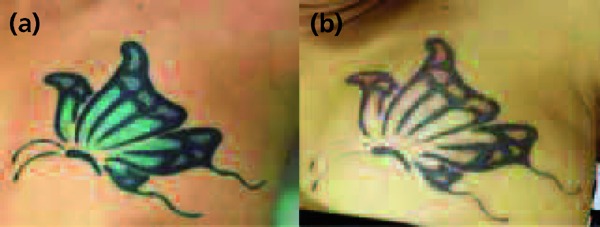
Case 3, tattoo on the chest. (a) Before treatment, (b) Two months after 1 time Pico -Alex treatment. (For interpretation of the references to color in this figure legend, the reader is refered to the web version of this article.)
Case 4. 35-year-old female patient. Tattoo on the upper arm (Fig. 6 (a)). This multi-colored tattoo would be considered extremely difficult to remove completely using a ns-domain Q switched laser. After 3 treatments with Pico-Alex (Fig. 6 (b)), all colors were effectively removed but the blue and purple pigments were most effectively removed. After 5 treatments with Pico-Alex (Fig. 6 (c)), the tattoo was being progressively removed but red and yellow pigments still remained. One treatment with Pico-YAG (532 nm) was added and dramatic removal of these colors was observed (Fig. 6 (d)). Further treatments are being planned following the resolution of the cutaneous hyperpigmentation.
Fig. 6.
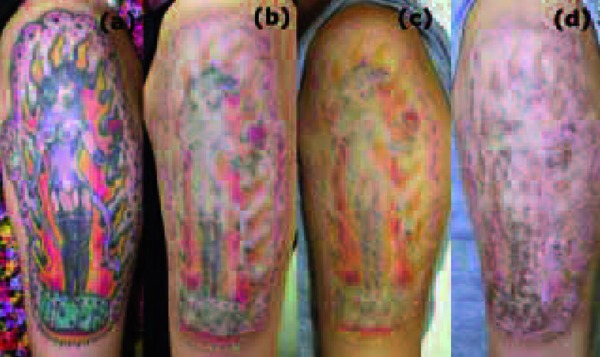
Case 4, tattoo on the upper arm. (a) Before treatment, (b) After 3 times treatment by Pico-Alex, (c) After 5 times treatment by Pico-Alex, (d) One month after five Pico-Alex plus one Pico-YAG (532) treatment. (For interpretation of the references to color in this figure legend, the reader is refered to the web version of this article.)
Dermal melanocytosis
Since ps-lasers are capable of destroying the melanosomes of dermal melanocytes in a similar manner to ns-domain Q switched lasers, it is easy to assume that ps-lasers would be effective for the treatment of dermal melanocytosis. Case reports have been presented at various academic meetings but no large scale comprehensive study has been published in the literature. The author assumes that ps-lasers would be just as effective for the treatment of dermal melanocytosis as the ns-lasers but further studies are warranted. If it were to be proven that treatment for dermal melanocytosis with ps-lasers could be more effective than ns-lasers, it would be a revolutionary advance.
Case 5. 2-year-old male patient. Nevus of Ota of the left cheek (Fig. 7 (a)). Four months after a single treatment with Pico-Alex, the color of the nevus haddramatically faded (Fig. 7 (b)) but similar results might have been achieved with a ns-domain Q switched laser.
Fig. 7.
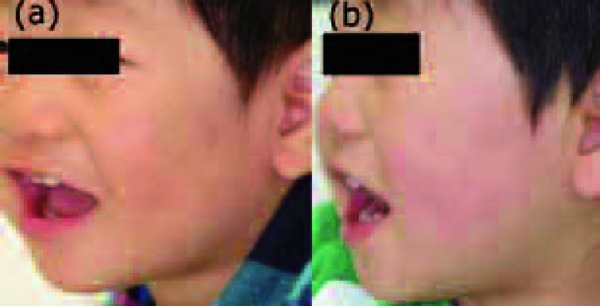
Case 5, Nevus of Ota on the left cheek. (a) Before treatment, (b) Four months after one treatment by Pico-Alex. (For interpretation of the references to color in this figure legend, the reader is refered to the web version of this article.)
Case 6. 2-year-old male patient. Ectopic Mongolian spot of the chest and left upper limb. From the dark color of the nevus, spontaneous resolution was considered unlikely and laser treatment was started (Fig. 8 (a)). A QSRL was used to treat the shoulder and upper limb region while the Pico-Alex system was used to treat the chest region. Four months after laser irradiation (Fig. 8 (b)). In the QSRL treated region, the distinctive hyperpigmentation and transient exacerbation of the nevus could be observed while at the Pico-Alex treated region, the skin color had returned to its original hue. Even at this point the difference in treatment effect was obvious. However what is important is how to interpret the difference. One way would be to think that the difference relies solely on the different lasers used, while another way would be to think that the treatment parameters for the QSRL may have been sub-optimum. Another different interpretation would be to take into consideration the speed and/or mechanism of elimination of post-treatment color pigments. At this point, no conclusion can be reached and further studies are warranted.
Fig. 8.
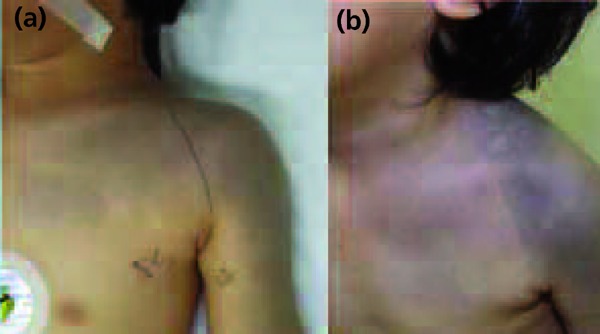
Case 6, ectopic mongolian spot on the chest and upper extremity. (a) Before treatment, (b) Four months after one treatment by Pico- Alex (chest) and QSRL (arm). (For interpretation of the references to color in this figure legend, the reader is refered to the web version of this article.)
Solar lentigines
There is a consensus on the efficacy of ns-domain Q-switched lasers for the treatment of senile lentigines and ephelides, or so called solar lentigines. Of course the efficacy of picosecond lasers is anticipated to be just as good. Case reports at various academic meetings have been seen sporadically but no comprehensive study has been performed. Whether a single high fluence treatment or multiple low fluence treatments would be better has not yet been elucidated.
Case 7. 47-year-old, female patient. Solar lentigo of the right cheek (Fig. 9 (a)). Pico-Alex was applied at 3.5 J/cm2. The lesion whitened immediately after laser irradiation (Fig. 9 (b)) and formed a dark brown eschar which exfoliated after 10 days and the lentigo was completely eradicated (Fig. 9 (c)). At one month posttreatment (Fig. 9 (d)), there was some marginal pigmentation but was blending in with the surrounding skin. This course is almost identical to that seen when lentigines are treated with a QSRL. Based on this, it could be suggested that the Pico-Alex could be used with similar efficacy to the QSRL.
Fig. 9.
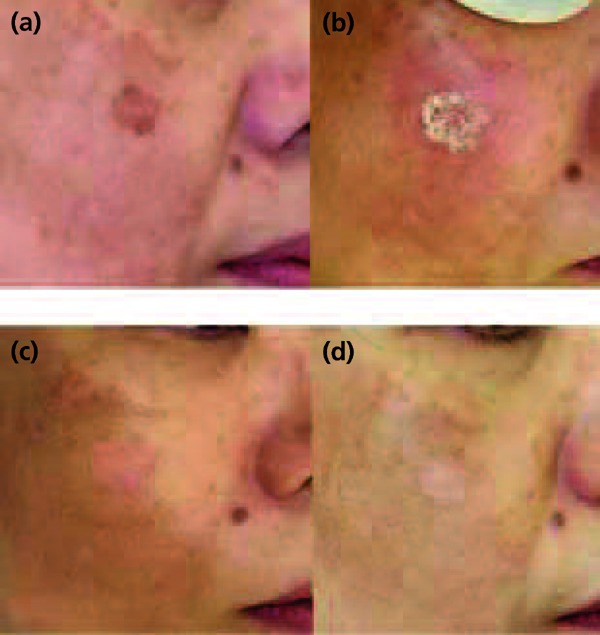
Case 7, solar lentigo on the right cheek. (a) Before treatment, (b) Immediately after treatment, the lesion shows immediate whitening phenomenon. (c) Ten days after treatment, the pigment of the lesion was removed. (d) One months after treatment, the lesion keeps white with subtle marginal hyperpigmentation. (For interpretation of the references to color in this figure legend, the reader is refered to the web version of this article.)
Case 8. 47-year-old female patient. This patient came to the clinic wanting to receive cosmetic treatment of the whole face (Fig. 10 (a)). Spot irradiation with Pico-Alex at a fluence of 3 J/cm2 was administered on the disseminated lentigines while laser irradiation at a low fluence of 0.4 J/cm2 was administered over the rest of the face. This low fluence treatment was performed twice, one month apart. This treatment regimen causes minimal crusting, requires no dressing and does not interfere with normal daily activities: it is thus well accepted by patients. One month after the second treatment (Fig. 10 (b)). The number and darkness of the pigmented lesions were reduced significantly. Repeated low fluence treatments with ps-lasers should be studied with caution. The usage of ps-lasers to treat so called senile flecks can be considered effective, however the efficacy of repeated low fluence treatment for acquired dermal melanocytosis remains to be determined. Also, questions such as whether or not melasma treatment with repeated low fluence ps-laser treatment could produce the same results as laser toning (repeated low fluence QSYL treatment) or could cause similar severe complications, remain to be answered.
Fig. 10.
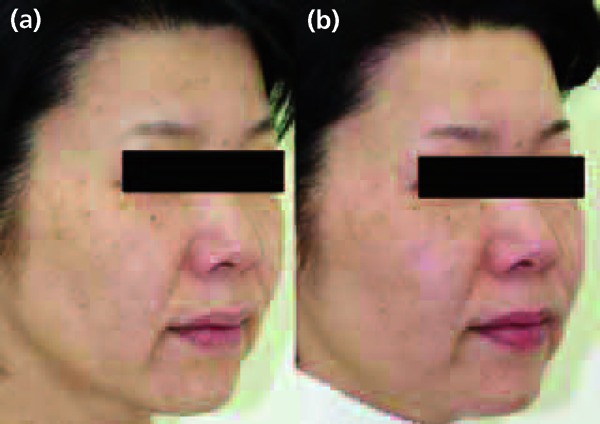
Case 8, disseminated solar lentigines on the face. (a) Before treatment, (b) One months after 2 times treatment using Pico-Alex with middle fluence at pigment spot and with low fluence on the whole face. (For interpretation of the references to color in this figure legend, the reader is refered to the web version of this article.)
Rejuvenation treatment such as for wrinkles
There is a trend toward the use of picosecond lasers for treatment of sagging skin, open pores and general facial rejuvenation. There are some who state that in combination with a special handpiece delivering an array of focused microbeams, which gives a similar effect as a fractional laser, high cosmetic result can be attained with ps-lasers. Among cosmetic dermatologists of the United States, Asia and Oceania this trend is growing. However, reports with high evidence levels are non-existent and it can be said that premature anticipation and financial needs are pushing this trend. Before promoting any rejuvenation treatment, basic studies should be performed.
Problems and future prospects
Deepening of the theoretical background of laser tattoo removal
It can be said with certainty that ps-lasers are more effective tattoo removal laser devices compared to ns-lasers. The efficacy of the SRT theory and photoacoustic reactions are being seen in actual clinical practice. However some questions still remain.
Firstly, even though we know that ps-lasers are better than ns-lasers, we do not know exactly what pulse width is best fit for tattoo removal. From clinical experience using the Pico-Alex, the author's impression is that 550 ps is better suited for tattoo removal than 750 ps in general. However there are cases where the outcome was the opposite. In almost all cases, ps-lasers were superior to ns-lasers but there was a single case where a ns-laser more effectively removed tattoo pigments than the ps-lasers. In the future, femtosecond lasers (fs-lasers) with r pulse widths orders of magnitude shorter pulse width than the ps-laser may be developed for clinical application. The question remains the same. What pulse width is best suited for which types of tattoos? Studies on this subject are strongly warranted.
Secondly, there is the question of color dependency. It was originally thought that since ps-lasers rely heavily on the photoacoustic reaction for their therapeutic effect, the removal of tattoo pigments would be color independent where all colors would be removed at the same rate. However in actual practice, although color dependence is smaller than ns-lasers, color dependence still exists 15). (Please refer to Case 4). This is because we have not yet been given a ‘true’ ps-laser. The current shortest pulse width is 350 ps, and that is still 0.35 ns. When we get down to single digit ps pulse widths, then we may well see true color independence. Studies on the subject of the color of the tattoo pigment and types of lasers to be used are warranted.
Thirdly there is the question of color changes and shifts in tattoos. It is known that in certain tattoos color changes and shifts occur after ns-laser irradiation which can make the tattoo more conspicuous than before the treatment. The ps-laser which relies more on a photoacoustic rather than a photothermal reaction, is anticipated to have relatively less color changes and shifts than ns-lasers. From the author's experience there was a case of a skin-colored cosmetic tattoo where a color change was seen after treatment with a ns-laser. Subsequent picosecond laser treatment removed the tattoo without any further color changes. On the other hand, the author has experienced cases where color changes occurred regardless of the laser type used. Studies on this subject are also required. It is clear that the ps-laser has definitely advanced laser tattoo removal but it is equally clear that an even deeper understanding of the theoretical background behind laser tattoo removal is necessary.
Ps-lasers used as a no-downtime cosmetic device
From the previous discussions, it can be said that ps-lasers are highly effective for the removal of tattoos. Recently there is a trend toward applying ps-lasers as a cosmetic device with no associated patient downtime. Presently there are numerous devices on the market which advertise their capability to treat a patient without the need for post-treatment dressing or limit the patient's social activities (referred to as no downtime) for a cosmetic procedure. However scientific evidence supporting the efficacy of such devices is generally sparse and in most cases over-rated expectations are driving such a trend. The author believes that the ps-laser is at a state of balance as to whether or not its application for ‘no-down time’ cosmetic procedures can be supported by scientific evidence.
Indications for the treatment of melasma
Lasers with pulse widths of a few nanoseconds are capable of destroying melanosomes with minimum collateral damage to the melanocytes and surrounding tissue. It was from this fact that repeated low fluence treatment with QSYL (Laser Toning: LT) was born, developed for the treatment of the problematic condition of chronic over-abundance of melanin in the skin, melasma. While LT sessions are being given, the melanin decreases and at first LT may seem to be effective but in many cases soon after the treatment is terminated melasma recurs, and in some cases there is a rebound effect resulting in patches of pigment which are darker than before the treatment. LT is also known to cause intractable punctuate leukoderma 17). LT seems to have passed its peak of popularity which means that treatment of melasma with the ps-laser may well be coming next. It could be argued that the ps-laser with its shorter pulse width will have the same or higher efficacy in decreasing the amount of melanin than LT with the ns-laser. However since the basic mechanism of treatment differs from LT in that there is more of a photomechanical than a photothermal effect, the risk of complications already associated with LT may increase depending on the method of use of the ps-laser. The author stresses that careful and comprehensive clinical trials must be performed before picosecond lasers are used for the treatment of melasma in the general public, particularly in Asian patients with Fitzpatrick skin types III and above 18).
Conclusions
This paper has reviewed the background behind the appearance of the ps-laser, the clinical application, present problems and future prospects in the field of dermatology for ps-lasers. The ps-laser is a revolutionary advance for laser tattoo removal but may be a less effective device in other indications such as those currently being treated with the numerous no-down time cosmetic devices present in the market: The same applies for ps-laser treatments of melasma and other cosmetic procedures. Basic studies must be performed before trying to expand sales of the devices, in addition to a much deeper understanding of the theoretical laser/tissue interaction specific to the ps-laser.
[Acknowledgements]
Editor's Note: This paper was originally published in Japanese in The Journal of Japan Society for Laser Surgery and Medicine, Vol.37-4: 440–446, 2016, and has been specially translated for inclusion in Laser Therapy as an English Original Article.
Disclosure of conflicts of interests
No conflicts of interests exist.
References
- 1: Anderson RR, Parrish JA. Selective photothermolysis: Precise microsurgery by selective absorption of pulsed radiation. Science 1983;220: 524-27. [DOI] [PubMed] [Google Scholar]
- 2: Scheibner A, Kenny G, et al. A superior method of tattoo removal using the Q-switched ruby laser. J Dermatol Surg Oncol 1990;16: 1091-8. [DOI] [PubMed] [Google Scholar]
- 3: Kilmer SL, Anderson RR. Clinical use of the Q-switched ruby and the Q-switched Nd:YAG (1064nm and 532nm) lasers for treatment of tattoos. J Dermatol Surg Oncol, 1993; 19: 330-88. [DOI] [PubMed] [Google Scholar]
- 4: Fitzpatrick RE, Goldman MP. Tattoo removal using the alexandrite laser. Arch Dermatol 1994; 130: 1508-14. [PubMed] [Google Scholar]
- 5: Kasai K. Tattoo. Introduction to Q switched laser treatment. Kasai K. Bunkodo; 2008; 86-97. [Google Scholar]
- 6: Peach AH, Thomas K, Kenealy J. Colour shift following tattoo removal with Q-switched Nd-YAG laser (1064/532). Br J Plast Surg 1999; 52: 482-7. [DOI] [PubMed] [Google Scholar]
- 7: Ross EV, Yashar S, et al. Tattoo darkening and nonresponse after laser treatment: a possible role for titanium dioxide. Arch Dermatol 2001; 137: 33-7. [DOI] [PubMed] [Google Scholar]
- 8: Ross V, Naseef G, et al. Comparison of responses of tattoos to picosecond and nanosecond Q-switched neodymium: YAG lasers. Arch Dermatol 1998; 132: 167-71. [DOI] [PubMed] [Google Scholar]
- 9: Saedi N, Metelitsa A, et al. Treatment of tattoos with a picosecond alexandrite laser: a prospective trial. Arch Dermatol 2012; 148: 1360-3. [DOI] [PubMed] [Google Scholar]
- 10: Brauer JA, Reddy KK, et al. Successful and rapid treatment of blue and green tattoo pigment with a novel picosecond laser. Arch Dermatol 2012; 148:820-3. [DOI] [PubMed] [Google Scholar]
- 11: Alabdulrazzaq H, Brauer JA, et al. Clearance of yellow tattoo ink with a novel 532-nm picoseconds laser. Lasers Surg Med 2015; 47: 285-8. [DOI] [PubMed] [Google Scholar]
- 12: Bernstein EF, Schomacker KT, et al. A novel dual-wavelength, Nd:YAG, picosecond-domain laser safely and effectively removes multicolor tattoos. Lasers Surg Med, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13: Bae YC, Alabdulrazzaq H, et al. Successful treatment of paradoxical darkening. Lasers Surg Med, 2016. [DOI] [PubMed] [Google Scholar]
- 14: Hazama H, Awazu K. Mechanism and principle of laser treatment in dermatology: Light-tissue interaction. In Pearls and problems of laser dermatology. Edit Watanabe S, et al. Nankodo; 2013; 2-12. [Google Scholar]
- 15: Kasai K. Laser treatment of tattoos. Pepars 2016; 111: 114-121, 2016. [Google Scholar]
- 16: Kasai K. Danger of low fluence Q switched Nd:YAG laser treatment for melasma-so called “laser toning”. J Japan Soc Laser Surg Med 2016; 36: 430-435. [Google Scholar]
- 17: Kasai K. Melasma. In Treatment of Pigmented Lesions 2nd ed. Kasai K. Bunkodo; 2015; 121-172. [Google Scholar]
- 18: Kasai K. Treatment strategy of melasma: The importance of conservative treatment taking into consideration of the essential qualities of melasma. Pepars 2016; 110: 73-78. [Google Scholar]


