Abstract
Adults with intellectual disabilities (ID) often live a sedentary lifestyle and have higher rates of overweight and obesity. The purpose of this report is to describe the design and methods of a multi-component physical activity (PA) intervention program that aims to increase PA levels in adults with ID who live in group homes. The study employed a multi-component delayed treatment control group design involving adults with ID who lived in two group homes. Interventions included 30 exercise sessions in groups over a 10-week period and three educational lessons based on social cognitive theory that aimed to improve self-efficacy and social support for PA in the participants. In addition, staff training in exercise and advice on institutional PA policies were provided to the caregivers working in the group homes. Outcome measures on three aspects were collected: (1) physical fitness, (2) PA as assessed by an ActiGraph accelerometer, and (3) self-efficacy and social support for PA. Our major objective was to develop the intervention protocol, and the successful completion of this study will provide valuable evidence on how to promote active lifestyles in adults with ID.
Keywords: Adults, Intellectual disabilities, Physical activity intervention
Introduction
Adults with intellectual disabilities (ID) have low levels of physical activity (PA) and high levels of sedentary behavior.1 It is well documented that adults with ID tend to have higher rates of morbidity and mortality associated with hypoactive diseases,2 low fitness levels and high obesity rate1, 3 when compared with the general population. PA is an important factor in improving health outcomes because of its association with reduced risk of heart diseases, hypertension, cancer, diabetes, and obesity.4 The World Health Organization (2010) recommends that adults aged 18–64 should do at least 150 minutes of moderate-intensity aerobic PA throughout the week.5 However, most studies in adults with ID have found that this population subgroup has very low PA levels. In a review paper, researchers found that only 17.5–33.0% of individuals with ID engaged in the recommended amount of PA.6 Past studies determined the steps taken by adults with ID in Hong Kong and concluded that they led sedentary lifestyles.7, 8
Because of the well documented low PA levels and high overweight and obesity rates of adults with ID, researchers have advocated for an urgent need in offering health promotion and PA intervention programs for such adults.6, 9, 10 However, there is a paucity of studies on interventions that aim to improve PA among adults with ID. For example, only 11 relevant studies were included in a published scoping review that focused on PA promotion.6 A recent review found only six PA intervention studies targeting adults with ID that met the inclusion criteria.9 Nevertheless, Heller et al.6 concluded that there was some evidence that community-based PA and exercise programs for adults with ID improved physical fitness (e.g., lower body mass index) and had psychosocial benefits (e.g., better attitude towards PA, improved life satisfaction). Similar conclusions were drawn from a more recent review on lifestyle interventions for youths with ID that revealed successful changes in weight, body mass index, and fat mass.11 More specifically, a meta-analysis showed a moderate effect (0.41) of exercise programs on individuals with ID.12 The subgroup analysis in this meta-analysis further indicated that the effectiveness of exercise interventions were more profound in improving cardiovascular fitness, balance and self-esteem. As suggested by the previous review,6 future studies on PA interventions for adults with ID should address the issues of staff training, knowledge and motivation of people with ID, formulate ways to increase organizational capabilities to promote healthy behaviors, and use representative samples with objective measures of PA. Furthermore, the addition of a resistance training component seemed to be beneficial for improving strength, balance and flexibility among adults with mild to moderate ID.13
Developing effective PA intervention requires better understanding of the factors that either facilitate or prohibit PA participation in this population. By using focus group interviews, researchers have identified barriers for older people with mild to moderate ID; multitude variables including social support (from staff and peers), adequate self-efficacy, and physical environment factors (such as transportation) have certain impacts on PA participation.14 These findings are in line with what the social cognitive theory (SCT) has postulated.15 Originating in psychology, SCT posits a reciprocal relationship between individual, environment and behavior; self-efficacy is the core construct in the theory. In accordance with this theory, two sets of beliefs are implicated in behavioral change. Firstly, they need beliefs about the desired behavior; that habituated behaviors are appropriately reinforced and that any consequence associated with the desired behavior is rewarded. Secondly, there needs to be beliefs about themselves in relation to the behavior—that they have the necessary capabilities to perform the desired behavior as well as the confidence to successfully perform that behavior.16 The theory has been widely applied in behavioral interventions (including those that aim to increase PA) in the general population; however, the application of SCT in people with ID is very limited. Recently, one study reported a theory (mainly the SCT)-driven intervention protocol for promoting PA among seniors with ID.17 Various behavioral techniques were applied in developing the interventions, e.g., tailoring, education, and modeling. Its effectiveness remains unknown.
According to data published in January 2015, there were 71,000–101,000 people with ID in Hong Kong, representing a prevalence rate of 1.0–1.4% for ID.18 Adults with ID may live independently in the community, with family members at home, or in residential group homes (e.g., supported hostel) within the Department of Social Welfare system with services provided and managed by non-governmental agencies. To our knowledge, there are a very limited number of studies related to the PA of adults with ID in Hong Kong. Local scholars have conducted studies of youth with fundamental skill development problems and children with ID and with cerebral palsy,19 and studies that examined PA levels of children attending special schools.20 Intervention programs have been reported for young children in special school21 and for adults with ID.7 However, Chan’s study7 only provided a 12-week period of PA education to the experimental group that aimed to improve their PA levels during out-of-work hours and had no exercise intervention component. Therefore, the purpose of the present paper was to describe the design and methods of a multi-component PA intervention program for adults with ID who lived in group homes.
Methods
Study design
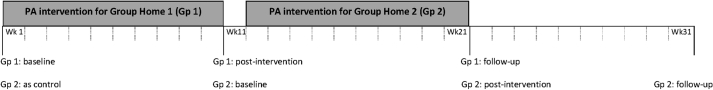
This study used a delayed treatment control group design consisting of a multi-component PA intervention program. The intervention program lasted for 10 weeks. After participants from the first group home completed the program, intervention was then provided to participants from the second group home who formed the delayed treatment control group. Participants in the delayed treatment control group were asked to carry on with their normal daily routines, while PA intervention was provided to participants from the first group home.
Participants
Adults with ID who were residents from two selected group homes that pair with shelter workshops offering at least 30 residential places were recruited as participants. Inclusion criteria were: (1) aged 18–55 years; (2) either mildly or moderately mentally handicapped (information provided by the group homes, and degree of mental handicap was diagnosed before or at the age of 18; http://www.lwb.gov.hk/eng/advisory/rac/rpp_report.htm); (3) have the ability to understand basic information about the intervention and to give consent; and (4) be able to participate in aerobic exercises involving mostly walking. Exclusion criteria were: (1) presence of contraindications to participating in exercise programs as advised by the service provider or care staff including those with a variety of other physical disorders (such as congenital heart defects and cerebral palsy), or judged to be at risk of self-harm by the service provider or care staff, such as being autistic; and (2) any known chronic diseases that may prevent them from participating in exercise, including those who are wheelchair bound.
Ethics approval for conducting the study was obtained from Hong Kong Baptist University’s Human Ethics Committee and from the directors of the two selected group homes. Informed consent forms were distributed to the parents or guardians of all eligible residents of the group homes.
Sample size calculation
Based on previous data from a 6-minute walk test13 and moderate-to-vigorous physical activity (MVPA) assessed by an ActiGraph accelerometer,22 taking α = 0.05 and 1 – β = 0.80, the calculated sample size per site by power analysis is between 7 (r = 0.9) and 23 (r = 0.5) for the 6-minute walk test and 6 (r = 0.9) and 14 (r = 0.5) for PA data. Therefore, the decision was to recruit at least 30 participants from each group home. A total of 62 participants were included.
PA intervention contents
Intervention contents consisted of three components: exercise program in a group, SCT-based educational program, and staff training for caregivers of the two group homes. All intervention contents were reviewed and evaluated by the research team prior to implementation.
Exercise program. The focus of the exercise program was a gradual increase in intensity from light to moderate during the 10-week intervention period. Three supervised group exercise sessions per week were provided. The intervention format was similar to that in previous studies.23, 24 The exercise program consisted of five lesson plans, each to be implemented in exercise sessions of 2 consecutive weeks. The design of the lesson plans followed program guidelines.25 Also, the exercise intensity of the first 12 sessions of the program (based on the first two lesson plans) was of light intensity while the latter part of the exercise program (based on the 3rd, 4th and 5th lesson plans) had gradual increments of moderate intensity (e.g., single leg and double leg jumps; squat exercise). The format of the 60-minute exercise session included 5 minutes of warm-up, 35–40 minutes of light-to-moderate intensity aerobic exercises, 5–10 minutes of light weight training exercises incorporated into the aerobic exercises, and 5–10 minutes of stretching and cool-down. The aerobic exercises consisted of rhythmic and continuous walking or running movements involving large muscles. The weight training exercises involved the use of foams (e.g., hitting targets for 30 seconds placed at over standing height positions) and sand-filled bottles (e.g., arm curl exercise) for training of upper body muscle groups and the use of one’s own body weight for training of lower body muscle groups (e.g., squat exercise). Participants took turns in doing the aerobic and weight training exercises so that they had adequate resting time in between the exercises. The exercise sessions were led by an exercise instructor who has a physical education teacher diploma with sport coaching experience and experience in working with adults with ID. The exercise sessions were assisted by two to three university student helpers and a staff member from the group homes. Study participants from each hostel were divided into two exercise groups and the group size ranged from 15 to 17. To assess whether participants showed any gradual increase in percent time spent engaging in MVPA in the exercise program, participants wore the ActiGraph accelerometers during three exercise sessions held in the first week and during alternate weeks.
Educational program. The second component of intervention consisted of three sessions of 1-hour educational lessons based on SCT that focused on behavioral change strategies delivered to the participants in the intervention group. The educational content focused on increasing participants’ self-efficacy and their ability to seek social support with teaching materials adapted from Bodde et al. (Table 1)22 and the Exercise and Nutrition Health Education Curriculum for Adults with Developmental Disabilities.26 Under the SCT model, self-efficacy and social support are important features for behavioral change. Self-efficacy is the confidence a person has in his/her ability to perform a behavior (i.e., to exercise), including the confidence to overcome barriers to performing the behavior. Following Bodde et al.’s model,22 pictures and videos were used to teach skills of doing exercises. Another aspect of the educational component was to increase participants’ ability to seek social support for PA by teaching strategies such as seeking friends to encourage one another to do exercise. Verbal encouragement was given to the participants to increase walking, stretching, and light weight training exercises during their own free time.
Table 1.
The targeted constructs in the SCT and the intervention components.
| Target construct according to SCT | Change objectives | Relevant behavior change components |
|---|---|---|
| Self-efficacy | Adults with ID think they are able to perform PA | • Setting progressive goals in exercise program • Providing model demonstration during exercise program |
| Attitude | Adults with ID enjoy participating in PA | • Selecting exercise types according to the preference of the participants |
| Behavioral reward | Adults with ID feel stimulated and supported by others to perform PA | • Prompt giving of rewards and praise for any attempt at performing PA during exercise program • Presenting of certificate to participants who attended at least 80% of the exercise program • Providing feedback on participants’ progress during the education program |
| Social support | Adults with ID feel safe and comfortable to perform PA | • Providing adequate knowledge (e.g., safety, how to seek help from others) through the education program • Strengthening the knowledge and skills of staff at the residential group homes through staff training |
Staff training program. The intervention included a staff training component. As social support can be provided by the staff of the group homes, the content of the 2-hour staff training session included increasing cognitive awareness of the importance of providing physical activities to the residents, the use of behavioral change strategies in promoting physically active lifestyles, and the practical skills needed to lead physical exercises.27, 28 Lastly, advice on the institutional policies with regard to the promotion of PA was given to the personnel of the group homes.
Outcome assessment
Measurements were taken at baseline (week 0), post-intervention (week 11), and at the 10-week follow-up. The assessment time points are shown in Figure 1.
Figure 1.
Assessment time points.
Physical fitness variables. Body weight, body height, body mass index, and waist and hip circumferences were measured. Estimated percent body fat was assessed with a body fat analyzer (TBF-410 Body Composition Analyzer; Tanita Corp., Tokyo, Japan). To assess aerobic fitness, the 25-meter 6-minute walk test29 was conducted; the test has been shown to have validity and reliability for adults with ID.30 The sit-and-reach test and arm curl test were conducted to assess flexibility and upper arm muscular endurance.
Physical activity measure. PA levels were assessed with an accelerometer (wGT3X-BT Activity Monitor; ActiGraph LLC, Pensacola, FL, USA). Accelerometers have been used extensively in PA studies of the general population and in PA studies of children with ID31 and adults with ID.32, 33 In this study, accelerometer data were collected for a minimum of 3 consecutive week days and a maximum of 8 days at baseline, post-intervention, and at the 10-week follow-up. (Participants who stayed at the hostel on the weekends wore the accelerometer consecutively for 8 days while those who left for home at the weekends wore the accelerometer only during the week days they were in the hostel.) At the beginning of each measurement day, the selected participant wore an elastic belt holding the ActiGraph Activity Monitor around his/her waist. The group home staff or carer was asked to remind the participant to wear the monitor during waking hours, with the exception of bath time and bedtime. Data that included more than 60 minutes of zero recordings in a day without any recorded explanation were treated as non-usable data. Only usable data of counts per minute with a minimum of 3 week days for each participant were analyzed. Data were set by 1-minute epochs and were categorized as minutes spent in light-, moderate- or vigorous-intensity PA according to the cut-off counts per minute.34
Psychosocial variables. Two scales developed by Peterson et al.35—the self-efficacy (SE) and social support (SS) scales—were used; they have been shown to have good psychometric properties in examining SE and SS constructs in adults with ID. The SE scale contains six items. The SS scale consists of three subscales: (1) family support (7 items); (2) staff support (6 items); and roommate support (5 items). These items were translated into Chinese using forward–backward translation procedures. The scale characteristics of content validity and reliability using Cronbach’s alpha were determined.
Intervention fidelity
Intervention fidelity is defined as the extent to which a program adheres to its program theory.36 It was reflected by the following indices: (1) attendance rate of the exercise program; (2) score (from 1 to 5) given by the staff of the group homes about the effort made by each of the intervention participants during the last exercise session in each week and during the education sessions. The content of the exercise program was evaluated by a rater (one of the researchers) who determined the percentage of matching between the lesson plan content and actual implementation.
Data analysis
Data were inputted into IBM SPSS Statistics for Windows, Version 24.0 (IBM Corp., Armonk, NY, USA) for statistical analyses. A 2×2 ANOVA with an independent factor of group home (intervention vs. control) and a repeated factor of pre-test and post-test was computed separately for each of the measured variables of physical fitness, PA levels, and self-efficacy and social support for PA. A repeated one-way ANOVA was determined by each intervention group for pre-test, post-test, and follow-up test separately for all the measured variables. The level of significance was set at 0.05.
Results
Our major objective was to develop an intervention protocol and describe the study design. Hence, no results are given.
Discussion
The study participants were selected from two group homes with each hostel having a sheltered workshop located in the same building. All participants worked at the sheltered workshop from 9 a.m. to 4 p.m. on weekdays. At work, they spent the majority of their time in a sitting position performing tasks such as putting on product labels. After work, they stayed at the hostels, mostly engaged in sedentary activities such as watching television. During weekends and public holidays, only 26% of participants remained at the hostel; the rest spent their time at home with family. Hence, our study aimed to increase participants’ PA on weekdays by implementing a multi-component PA intervention program because it would have been extremely difficult for the research team to follow and track PA levels on the weekends when participants were in their home environment.
In our multi-component intervention, we offered group exercise sessions, educational lessons and staff training. The strengths of our research design lie in three aspects. First, exercise sessions involving new lesson plans were observed to ensure that lessons followed the curriculum. Second, we offered interactive educational lessons with graphic prompts and questions to convey and consolidate the importance of seeking social support in doing PA. The educational content was SCT-based by adopting similar approaches as those described in previous studies.22, 37, 38, 39 Third, staff were involved in the implementation of the intervention, with at least one staff member being present in the exercise sessions. Also, staff training was provided.28 On the other hand, there were some limitations: this study was not a randomized controlled trial due to practical difficulties; we could not collect accelerometer data on the weekends for those participants who did not stay at the hostel on the weekends due to budget concerns. Since little is known about how to design appropriate and acceptable interventions for people with ID,9 our major objective was to develop an intervention protocol which will provide valuable insight for the design of PA intervention programs for this population.
Conflicts of interest
All contributing authors declare that they have no conflicts of interest.
Funding/support
The project was funded by the university’s Faculty Research Grant to the first author as the chief investigator (FRG2/14-15/062).
References
- 1.Draheim C.C., Williams D.P., McCubbin J.A. Prevalence of physical inactivity and recommended physical activity in community-based adults with mental retardation. Ment Retard. 2002;40:436–444. doi: 10.1352/0047-6765(2002)040<0436:POPIAR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Sutherland G., Couch M.A., Iacono T. Health issues for adults with developmental disability. Res Dev Disabil. 2002;23:422–445. doi: 10.1016/s0891-4222(02)00143-9. [DOI] [PubMed] [Google Scholar]
- 3.Grondhuis S.N., Aman M.G. Overweight and obesity in youth with developmental disabilities: a call to action. J Intellect Disabil Res. 2014;58:787–799. doi: 10.1111/jir.12090. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services (USDHHS) USDHHS; Atlanta, GA: 1996. Physical Activity and Health: A Report of the Surgeon General. [Google Scholar]
- 5.World Health Organization . WHO; Geneva: 2010. Global Recommendations on Physical Activity for Health. [PubMed] [Google Scholar]
- 6.Heller T., McCubbin J.A., Drum C. Physical activity and nutrition health promotion interventions: what is working for people with intellectual disabilities? Intellect Dev Disabil. 2011;49:26–36. doi: 10.1352/1934-9556-49.1.26. [DOI] [PubMed] [Google Scholar]
- 7.Chan S.Y. Hong Kong Baptist University; Hong Kong: 2014. Social Cognitive Theory Based PA Intervention Targeting Non-working Time PA of Workers with Intellectual Disabilities. [Google Scholar]
- 8.Chan H.T., Chow B.C. Physical activity of working adults with intellectual disabilities. In: Chen S.H., Fung S.K., editors. Contemporary Trends, Research, Teaching and Coaching in Adapted Physical Activity. Hong Kong Institute of Education; Hong Kong: 2013. pp. 1–9. [Google Scholar]
- 9.Brooker K., van Dooren K., McPherson L. A systematic review of interventions aiming to improve involvement in physical activity among adults with intellectual disability. J Phys Act Health. 2015;12:434–444. doi: 10.1123/jpah.2013-0014. [DOI] [PubMed] [Google Scholar]
- 10.Spanos D., Melville C.A., Hankey C.R. Weight management interventions in adults with intellectual disabilities and obesity: a systematic review of the evidence. Nutr J. 2013;12:132. doi: 10.1186/1475-2891-12-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maiano C., Normand C.L., Aime A. Lifestyle interventions targeting changes in body weight and composition among youth with an intellectual disability: a systematic review. Res Dev Disabil. 2014;35:1914–1926. doi: 10.1016/j.ridd.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 12.Shin I.S., Park E.Y. Meta-analysis of the effect of exercise programs for individuals with intellectual disabilities. Res Dev Disabil. 2012;33:1937–1947. doi: 10.1016/j.ridd.2012.05.019. [DOI] [PubMed] [Google Scholar]
- 13.Oviedo G.R., Guerra-Balic M., Baynard T. Effects of aerobic, resistance and balance training in adults with intellectual disabilities. Res Dev Disabil. 2014;35:2624–2634. doi: 10.1016/j.ridd.2014.06.025. [DOI] [PubMed] [Google Scholar]
- 14.van Schijndel-Speet M., Evenhuis H.M., van Wijck R. Facilitators and barriers to physical activity as perceived by older adults with intellectual disability. Intellect Dev Disabil. 2014;52:175–186. doi: 10.1352/1934-9556-52.3.175. [DOI] [PubMed] [Google Scholar]
- 15.Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13:623–649. [Google Scholar]
- 16.Heller T., Hsieh K., Rimmer J.H. Attitudinal and psychosocial outcomes of a fitness and health education program on adults with down syndrome. Am J Ment Retard. 2004;109:175–185. doi: 10.1352/0895-8017(2004)109<175:AAPOOA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.van Schijndel-Speet M., Evenhuis H.M., van Empelen P. Development and evaluation of a structured programme for promoting physical activity among seniors with intellectual disabilities: a study protocol for a cluster randomized trial. BMC Public Health. 2013;13:746. doi: 10.1186/1471-2458-13-746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Census and Statistics Department, HKSAR . Census and Statistics Department of the HKSAR; Hong Kong: January 2015. Persons with disabilities and chronic diseases in Hong Kong. Hong Kong Monthly Digest of Statistics. [Google Scholar]
- 19.Capio C.M., Sit C.H.P., Eguia K.F. Fundamental movement skills training to promote physical activity in children with and without disability: a pilot study. J Sport Health Sci. 2015;4:235–243. [Google Scholar]
- 20.Sit C.H., McKenzie T.L., Cerin E. Physical activity for children in special school environment. Hong Kong Med J. 2013;19(Suppl 4):42–44. [PubMed] [Google Scholar]
- 21.Choi P.H., Cheung S.Y. Effects of an 8-week structured physical activity program on psychosocial behaviors of children with intellectual disabilities. Adapt Phys Activ Q. 2016;33:1–14. doi: 10.1123/APAQ.2014-0213. [DOI] [PubMed] [Google Scholar]
- 22.Bodde A.E., Seo D.C., Frey G.C. The effect of a designed health education intervention on physical activity knowledge and participation of adults with intellectual disabilities. Am J Health Promot. 2012;26:313–316. doi: 10.4278/ajhp.100408-ARB-112. [DOI] [PubMed] [Google Scholar]
- 23.Ordonez F.J., Rosety M., Rosety-Rodriguez M. Influence of 12-week exercise training on fat mass percentage in adolescents with Down syndrome. Med Sci Monit. 2006;12:CR416–CR419. [PubMed] [Google Scholar]
- 24.Rimmer J.H., Heller T., Wang E. Improvements in physical fitness in adults with Down syndrome. Am J Ment Retard. 2004;109:165–174. doi: 10.1352/0895-8017(2004)109<165:IIPFIA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Winnick J.P. Human Kinetics; Champaign, IL: 2011. Adapted Physical Education and Sport. [Google Scholar]
- 26.Heller T., Marks B., Sisirak J. 3rd ed. University of Illinois at Chicago; Chicago, IL: 2006. Exercise and Nutrition Health Education Curriculum for Adults with Developmental Disabilities. [Google Scholar]
- 27.Draheim C.C. Cardiovascular disease prevalence and risk factors of persons with mental retardation. Ment Retard Dev Disabil Res Rev. 2006;12:3–12. doi: 10.1002/mrdd.20095. [DOI] [PubMed] [Google Scholar]
- 28.Prashner V.P., Janicki M.P. Blackwell Publishing; Oxford, UK: 2002. Physical Health of Adults with Intellectual Disabilities. [Google Scholar]
- 29.Elmahgoub S.S., Van de Velde A., Peersman W. Reproducibility, validity and predictors of six-minute walk test in overweight and obese adolescents with intellectual disability. Disabil Rehabil. 2012;34:846–851. doi: 10.3109/09638288.2011.623757. [DOI] [PubMed] [Google Scholar]
- 30.Nasuti G., Stuart-Hill L., Temple V.A. The six-minute walk test for adults with intellectual disability: a study of validity and reliability. J Intellect Dev Disabil. 2013;38:31–38. doi: 10.3109/13668250.2012.748885. [DOI] [PubMed] [Google Scholar]
- 31.Pan C.Y., Frey G.C. Physical activity patterns in youth with autism spectrum disorders. J Autism Dev Disord. 2006;36:597–606. doi: 10.1007/s10803-006-0101-6. [DOI] [PubMed] [Google Scholar]
- 32.Frey G.C. Comparison of physical activity levels between adults with and without mental retardation. J Phys Act Health. 2004;1:235–245. [Google Scholar]
- 33.Temple V.A., Anderson C., Walkley J.W. Physical activity levels of individuals living in a supported hostel. J Intellect Dev Disabil. 2000;25:327–341. [Google Scholar]
- 34.Freedson P.S., Melanson E., Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 35.Peterson J.J., Peterson N.A., Lowe J.B. Promoting leisure physical activity participation among adults with intellectual disabilities: validation on self-efficacy and social support scales. J Appl Res Intellect Disabil. 2009;22:487–497. [Google Scholar]
- 36.Fraser M.W. Oxford University Press; Oxford, UK: 2009. Intervention Research: Developing Social Programs. [Google Scholar]
- 37.Ewing G., McDermott S., Thomas-Koger M. Evaluation of a cardiovascular health program for participants with mental retardation and normal learners. Health Educ Behav. 2004;31:77–87. doi: 10.1177/1090198103259162. [DOI] [PubMed] [Google Scholar]
- 38.Mann J., Zhou H., McDermott S. Healthy behavior change of adults with mental retardation: attendance in a health promotion program. Am J Ment Retard. 2006;111:62–73. doi: 10.1352/0895-8017(2006)111[62:HBCOAW]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 39.Melville C.A., Boyle S., Miller S. An open study of the effectiveness of a multi-component weight-loss intervention for adults with intellectual disabilities and obesity. Br J Nutr. 2011;105:1553–1562. doi: 10.1017/S0007114510005362. [DOI] [PubMed] [Google Scholar]