Abstract
Objective/Background
There is a widespread belief that moderate-to-vigorous-intensity physical activity (MVPA) declines markedly in adolescence, particularly in girls. This belief has led to substantial research and policy effort aimed at reducing the perceived decline in MVPA during adolescence. The main aim of this review is to critically examine the belief that MVPA declines during adolescence.
Methods
Review of evidence from studies with objective measures of physical activity, systematic reviews of longitudinal studies, insights from recent longitudinal studies, and evidence from the International Children's Accelerometry Database (ICAD).
Results
Existing systematic review evidence, four recent longitudinal studies from England, and ICAD data all failed to support the hypothesis that MVPA declines particularly markedly during adolescence, or that an MVPA decline begins at adolescence, or that declines in MVPA during adolescence are greater in girls than in boys. Systematic reviews, longitudinal studies, and ICAD data in fact suggest that MVPA begins to decline, and sedentary behavior begins to increase, from around the age of school entry. Recent longitudinal studies also suggest that increasing sedentary behavior during adolescence displaces light-intensity physical activity. An emerging body of evidence from longitudinal studies that use trajectory analysis is providing important new insights into marked between-individual differences in the trajectories of MVPA across childhood and adolescence.
Conclusion
Although gaps in the evidence remain, particularly from low- to middle-income countries, and additional longitudinal studies are required, this review suggests that efforts to promote and/or maintain MVPA should begin well before adolescence.
Keywords: Adolescent, Child, Exercise, Longitudinal study, Physical activity, Sedentary behavior
Introduction
There is now a substantial amount of evidence, reviewed systematically and appraised critically, that physical activity influences health during childhood and adolescence.1, 2 Moreover, higher moderate-to-vigorous-intensity physical activity (MVPA) during childhood and adolescence has benefits beyond health. For example, recent evidence suggests that higher habitual MVPA can produce meaningful improvements in academic attainment in childhood and adolescence.3, 4, 5
Physical activity recommendations for school-age children and adolescents are evidence based and harmonized internationally (Appendix 1). The recommendation in relation to a minimum of 60 minutes of MVPA daily has received most attention, and is the focus of child and adolescent public health surveillance of physical activity. The other two physical activity recommendations are for vigorous-intensity physical activity (VPA), and for activities to promote muscle and bone health and flexibility (Appendix 1). Although these latter recommendations are important, they have generally received less attention (e.g., in research and in public health surveillance) than the recommendation for MVPA. Internationally, levels of MVPA among adolescents are typically much lower than recommended: as few as 20% of 13–15-year-olds globally appear to meet the MVPA recommendation.6 Levels of adherence to the recommendations in relation to VPA and activities to promote muscle and bone health and flexibility are less well-known because of the lack of surveillance of these behaviors.7, 8
It is generally accepted that there is a marked decline in MVPA during adolescence, and the decline is usually believed to be much more marked in girls than in boys. In the UK, for example, much policy and research efforts have been based on the concept that MVPA declines dramatically during adolescence, with the concept that adolescents, particularly adolescent girls, are a high-risk group for low MVPA.9, 10, 11 Globally, international surveillance programs for MVPA also focus on adolescents.6 There has been a tendency among researchers and policymakers in physical activity and health domains to assume that levels of MVPA among children are relatively high, or at least adequate, and that low MVPA is a problem that emerges in adolescence.9, 10, 11
The view that MVPA declines dramatically during adolescence has been extremely influential and is very well-established, but it is worth considering how evidence based the belief is. This work, a review of objectively measured evidence, aims to: (1) critique the belief that declines in MVPA begin in adolescence; (2) consider very recent evidence from longitudinal studies on the existence and extent of MVPA declines during adolescence; and (3) suggest new approaches to understanding the timing and magnitude of changes in MVPA across childhood and adolescence.
Methods
This work is a critique based on objectively measured physical activity evidence derived from recent systematic reviews of longitudinal studies of changes in MVPA and sedentary behavior, a synthesis of longitudinal studies published after the most recent systematic reviews, and a consideration of insights from the International Children’s Accelerometry Database (ICAD).12
Results
Systematic review evidence on declines in MVPA during adolescence
The most recent systematic review of declines in physical activity (not specifically MVPA) during adolescence was carried out by Dumith et al.13 Their work has been highly cited as evidence that MVPA declines during adolescence, and it reviewed 26 eligible longitudinal studies (with at least 2 measures of physical activity). Of the 26 eligible studies, 22 were based on questionnaire measures of change, three of which used pedometers, and only two were based on accelerometry. Most (16/26) of the eligible studies were from the United States, most (16/26) completed data collection before the year 2000, and the representativeness (or otherwise) of the samples in the eligible studies was usually unclear.13
Although the systematic review by Dumith et al13 is a very useful and thorough summary of the evidence base in the area, numerous substantial limitations in the evidence base should be noted. First, the small number of accelerometer studies means that there was in fact almost no longitudinal evidence on the magnitude of declines in MVPA in that review, with accelerometry necessary to have high confidence in the amount and intensity of physical activity.14 Second, the evidence base is arguably of limited generalizability globally given the dominance of studies from high-income countries, the United States in particular. Third, the dominance of studies with only two time points limits our understanding of the timing of changes in MVPA—an improved understanding of the timing and rate of changes in MVPA will require longitudinal studies with multiple measurement time points. In addition, the limited evidence across both childhood and adolescence revealed by Dumith et al13 makes it impossible to determine whether age-related declines in MVPA either began during adolescence or increased during adolescence.
An additional difficulty with the review by Dumith et al13 is that the evidence base is now so old that it may have reduced generalizability to contemporary populations. Recent and rapid societal changes, notably changes in transportation, in education, and in the technology now widely available to children and adolescents,15 might have changed the timing and/or magnitude of declines in MVPA during adolescence quite markedly in recent years. For example, many new screen-based sedentary behaviors have become popular with young children, and exposure to screen-based sedentary behavior has probably increased substantially in early childhood.16 Although the impact of these changes on physical activity is unclear, any increase in sedentary time must displace some combination of sleep, light-intensity physical activity, and/or MVPA. There is another difficulty with older evidence that applies particularly to settings where the environment has become more obesogenic: there is emerging, though not yet conclusive, evidence17, 18, 19 that obesity, and possibly overweight, will reduce MVPA. Prevalence of overweight and obesity is generally higher than in the past, and the body fat content of nonoverweight and nonobese children appears to have been going up.20, 21 In addition, in recent longitudinal studies of children, body mass index z score tends to increase with age, across the distribution of body mass index z score, and not just in the overweight and obese children.17 These population-wide changes in body composition predict that MVPA levels of children now will be lower than in even the recent past.
In summary, the lack of good evidence identified by Dumith et al13 means that there can be little or no confidence in changes in either the amount or timing of MVPA across adolescence at present. The review also provides little or no confidence in the view that MVPA declines begin during adolescence. A brief review of more recent longitudinal studies of changes in MVPA during adolescence, published after the review by Dumith et al,13 is given in the following sections.
Review of recent longitudinal studies of changes in MVPA during adolescence
Four studies of accelerometer-measured longitudinal changes in MVPA (each with 2 measurement time points) in English adolescents were published after the review by Dumith et al.13 Two of the cohort studies took place in South-West England and changes were measured using an ActiGraph accelerometer (ActiGraph, Pensacola, Florida, USA), though with different accelerometer cutoff points: Harding et al22 (n = 363) found no significant changes in MVPA in either boys or girls, born in the mid–late 1990s, between the ages of 12 and 15 years; Mitchell et al23 (n = 5436) found negligible changes in MVPA in both sexes between the ages of 12 and 16 years in a cohort born in the early 1990s.
In a smaller cohort study by Corder et al24 in the South-East of England, changes in physical activity of 480 participants who had been born in the late 1990s were measured using an ActiGraph accelerometer at the age of 10 years and were followed up to age 14 years. Corder et al24 reported small declines in MVPA in both sexes over the 4-year period; the declines were slightly but significantly more marked in boys than in girls. In another smaller cohort study in the South-East of England, with baseline measures taken when participants were aged 15 years (n = 144; born in the early 1990s), longitudinal declines in accelerometer-measured MVPA were small but statistically significant in both sexes between 15 and 17 years of age, with slightly greater declines in boys than in girls.25
In summary, all these four recently published longitudinal studies of objectively measured changes in MVPA during adolescence from England do not support the view that marked declines in MVPA occur during adolescence nor the common view that declines in MVPA during adolescence are more marked in girls than in boys. In fact, this emerging evidence from longitudinal studies suggests that declines in MVPA, where they occur, might be greatest in those groups with highest baseline MVPA (and so are likely to be greater in boys than in girls).25
One notable contrast to the recent evidence from longitudinal accelerometry studies summarized here is the study by Nader et al.26 Their study reported a phenomenal decline, of over 4 h/d, in MVPA between age 9–10 years and 15–16 years in the United States. This magnitude of change is almost certainly an artifact of the accelerometer cutoff points used to define MVPA at the different ages.14, 25
Evidence on increases in sedentary behavior across childhood and adolescence
One great advantage of longitudinal accelerometry studies of the kind described earlier is that they can provide a unique insight into the relationships between changes in sedentary behavior, light-intensity physical activity, and MVPA with age. Sedentary behavior and physical activity are generally regarded as distinct variables, so that an individual can theoretically be both active (i.e., have sufficient MVPA) and sedentary (i.e., with excess sedentary time). A recent review of largely cross-sectional studies (most of which used subjective measurement methods) found that there was limited evidence of displacement of MVPA by sedentary behavior.27 However, the recent longitudinal accelerometry studies from England described earlier show that the increased amount of time spent in sedentary activities as adolescence proceeds displaces physical activity (particularly light-intensity physical activity),22, 23 and may also displace sleep.25
Tanaka et al28 recently reported a systematic review of longitudinal studies of changes in accelerometer-measured sedentary behavior in children and adolescents. They found 10 eligible studies, most from high-income Western countries, and most with measures at only two time points. In all of the eligible studies, which measured changes after the age of school entry, sedentary behavior increased over time, by an average of 25–30 min/d/y.28 While the review by Tanaka et al28 found gaps and limitations in the evidence base, it supports the view that sedentary behavior typically increases from early–mid childhood,28 and this must be displacing physical activity and/or sleep.
Insights from the ICAD
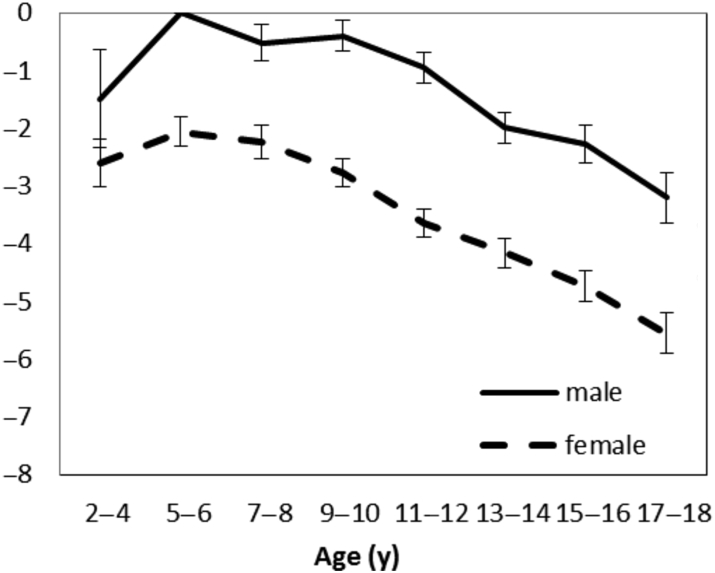
The ICAD12 has, by standardizing and pooling accelerometer-measured MVPA from up to 21 studies (of well over 20,000 individuals), provided a number of important insights into levels, correlates, and consequences of variation in MVPA during childhood and adolescence. In the context of providing an understanding of change in MVPA, the ICAD has limitations, in part because most of the individual data sets are cross sectional. Despite these limitations, recent evidence from pooled ICAD data12 quite clearly predicts that declines in the total volume of physical activity, light-intensity physical activity, and MVPA occur across childhood and adolescence, beginning around the time of school entry in both sexes, with no obviously marked declines in MVPA during adolescence. Changes in MVPA with age across the ICAD data set are summarized in Figure 1.
Figure 1.
Percentage decline in moderate-to-vigorous-intensity physical activity by age group across childhood and adolescence from the ICAD data.12Note. From “Objectively measured physical activity and sedentary time in youth: the International Children’s Accelerometry Database (ICAD),” by A. Cooper, A. Goodman, A.S. Page, et al., 2015, Int J Behav Nutr Phys Act. 12, p. 113.
Large-scale data-pooling studies of this kind can also be helpful in providing evidence on why, as well as when, declines in MVPA occur. For example, the extent to which declines in MVPA might be inherent (biological) rather than external (environmental) has been debated.29, 30 The ICAD data demonstrate substantial variation in MVPA between studies/environments, providing support for the view that environment (in the widest sense: policy, built, cultural) is important, and might either increase or decrease changes in MVPA, which are mediated by any underlying biological processes.12
Insights from the Iowa Bone Development Study
An improved understanding of the timing and magnitude of changes in MVPA will require longitudinal studies, using objective measures, which span both childhood and adolescence and have multiple measurement points (rather than the standard 2 time points common in the literature to date13, 28). Such evidence is very scarce,13 but available from the Iowa Bone Development Study,31 which has data on a cohort born in the early 1990s in the United States, with up to seven accelerometer-measured MVPA between the age of 5 and 19 years. Data from the Iowa Bone Development Study support the view that MVPA declines across childhood and adolescence in both sexes, and these declines do not develop at or during adolescence.
The large number of MVPA measures made in the Iowa Bone Development Study also provide an important insight into between-individual variation in both the timing of changes in MVPA and the magnitude of changes in MVPA. Changes in MVPA over time are often considered in an overly simplistic way, tending to make the implicit assumption that all or most individuals follow the same trajectory of change over time.9, 10, 11 The multiple measures of MVPA in the Iowa Study permit trajectory analysis, identifying subgroups within the population with very different timing and/or magnitude of change in MVPA across adolescence. These between-group differences in timing and magnitude of MVPA in the Iowa cohort are surprisingly marked, identifying a subgroup with stable MVPA across childhood and adolescence, a subgroup with low and steadily declining MVPA, and a subgroup with high initial MVPA in early childhood and with a dramatically declining MVPA from that point.31 Such marked differences in the trajectory of MVPA across childhood and adolescence represent a challenge for the prevention of MVPA decline, however, greater awareness of the existence of these different trajectories and evidence on the determinants of the trajectories should permit much more evidence-informed prevention in future.31 In summary, recent longitudinal studies that have used accelerometry suggest that it is time for a more nuanced view of age-related changes in MVPA across childhood and adolescence.
Translation of evidence on changes in MVPA into policy
Despite the low quality, small quantity, and limited generalizability of the evidence, there appears to be great and widespread confidence in the belief that MVPA declines markedly during adolescence. In Scotland, for example, cross-sectional data from nationally representative surveys of physical activity are available across childhood and adolescence, and these appear to show that levels of MVPA are very high in childhood, declining markedly in adolescence, particularly in girls.9, 10, 11 The apparent decline in MVPA during adolescence has been used as the basis of physical activity policy in Scotland for many years, which targets adolescents, particularly girls.9, 10, 11 The concept of decline in MVPA during adolescence has led to many research studentships and grants aimed at understanding why MVPA declines during adolescence. The Scottish survey data, which show the apparent decline in MVPA, are not without problems however, quite apart from the recent evidence summarized earlier. The only validation study of Scottish survey methodology to date has shown that the method of physical activity measurement used grossly overestimated MVPA during childhood, by an average of 2 h/d, and has no association with accelerometer-measured MVPA.32 In addition, the main national survey in Scotland (Scottish Health Survey) is cross sectional rather than longitudinal, and the erroneous data on MVPA it produced lead not just to an overestimation of MVPA, but also generated spurious differences in physical activity (e.g., between UK nations, between children and adolescents of high vs. low socioeconomic status), which are not supported by accelerometry studies.14, 33, 34, 35 In summary, much of the physical activity policy in Scotland, and probably in other countries, is not as evidence based as it may appear to be, because the evidence on which it is based is misleading.
The Active Healthy Kids Global Alliance (http://www.activehealthykids.org) is a new international effort that aims to build capacity in physical activity and health globally, to improve surveillance of child and adolescent physical activity nationally and internationally, and in turn to improve national and international physical activity policy.8 In Scotland, the Active Healthy Kids Scotland Report Card (http://www.activehealthykidsscotland.co.uk) is an attempt to highlight limitations in physical activity surveillance, so that future surveillance and policy will be much more evidence informed.36 As noted earlier, recent longitudinal studies with accelerometer-based measures are providing new insights into age-related changes in MVPA. Future evidence-based policy, in Scotland and globally, should therefore be based on much better evidence (objective measurement and longitudinal designs) than in the past, and should be able to take advantage of increasing global capacity in physical activity and health.
Gaps in the evidence globally
This review highlights the need for more longitudinal studies of changes in MVPA, with objective measures made at multiple time points, and which cross childhood and adolescence. Such studies are required urgently, even for high-income countries. The summaries of recent evidence presented here highlight the fact that nearly all of the available longitudinal evidence currently is from high-income or Western countries only. Low MVPA appears to be a global problem for adolescents,6 and requires a more global response, but research from many low- and middle-income countries is lacking,6 and this should be a high priority. A recent global consensus on priorities for physical activity and health among children and adolescents globally37 highlighted that the top priority was identifying interventions to improve MVPA, but more evidence on the magnitude and timing of age-related declines in MVPA globally would provide a sound basis for such future interventions. New research funding efforts will be required to undertake the new longitudinal studies that are needed so urgently.
Conclusion
This review suggests that there is little or no sound evidence to support the view that MVPA begins to decline in early adolescence, or the view that MVPA declines particularly markedly during adolescence, or the view that declines in MVPA during adolescence are more substantive in girls than in boys. It now seems much more likely that MVPA declines and sedentary behavior increases, in both sexes, from around the age of school entry. These suggestions should be tested by future longitudinal studies that use objective measures of physical activity and sedentary behavior. Future studies should be global because low MVPA is now a global problem.6, 8
Conflicts of interest
The author has no conflicts of interest relevant to this article.
Funding/support
No financial or grant support was received for this work.
Appendix 1. Physical activity recommendations for school-age children and adolescents.7
-
•
Accumulate at least 60 minutes, preferably more, of moderate-to-vigorous-intensity physical activity on a daily basis.
-
•
Incorporate vigorous-intensity activities on at least 3 d/wk.
-
•
Include activities that strengthen muscles and bones, and promote flexibility, on at least 3 d/wk.
Note. From “The pandemic of low physical activity in children and adolescents,” by J.J. Reilly, 2015, Aspetar Sports Med J., 4, p. 234–238.
References
- 1.Timmons B.W., Leblanc A.G., Carson V. Systematic review of physical activity and health in the early years (aged 0–4 years) Appl Physiol Nutr Metab. 2012;37:773–792. doi: 10.1139/h2012-070. [DOI] [PubMed] [Google Scholar]
- 2.Janssen I., Leblanc A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Booth J.N., Leary S.D., Joinson C. Associations between objectively measured physical activity and academic attainment in adolescents from a UK cohort. Br J Sports Med. 2014;48:265–270. doi: 10.1136/bjsports-2013-092334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Donnelly J.E., Greene J.L., Gibson C.A. Physical Activity Across the Curriculum (PAAC): A randomized controlled trial to promote physical activity and diminish overweight and obesity in elementary school children. Prev Med. 2009;49:336–341. doi: 10.1016/j.ypmed.2009.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davis C.L., Tomporowski P.D., Boyle C.A. Effect of aerobic exercise on overweight children’s cognitive function: RCT. Res Q Exerc Sport. 2007;78:510–519. doi: 10.1080/02701367.2007.10599450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hallal P.C., Andersen L.B., Bull F.C. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 7.Reilly J.J. The pandemic of low physical activity in children and adolescents. Aspetar Sports Med J. 2015;4:234–238. [Google Scholar]
- 8.Tremblay M.S., Gray C.E., Akinroye K. Physical activity of children: A global matrix of grades comparing 15 countries. J Phys Act Health. 2014;11(Suppl 1):S113–S125. doi: 10.1123/jpah.2014-0177. [DOI] [PubMed] [Google Scholar]
- 9.Scottish Health Survey 2014 (SHeS). Available from: www.scotland.gov.uk/Topics/Statistics/Browse/Health/scottish-health-survey. Accessed 31.03.16.
- 10.Let's Make Scotland More Active: Five-Year Review of a Strategy for Physical Activity. Available from: www.healthscotland.com/uploads/documents/9159-1150-HS%20PA%5yr%20Review%20Final.pdf Accessed 17.08.13.
- 11.Murray A., Calderwood C., O'Connor N. Scotland's progress in putting policy about physical activity into practice. Br J Sports Med. 2016;50:320–321. doi: 10.1136/bjsports-2015-095744. [DOI] [PubMed] [Google Scholar]
- 12.Cooper A., Goodman A., Page A.S. Objectively measured physical activity and sedentary time in youth: The International Children's Accelerometry Database (ICAD) Int J Behav Nutr Phys Act. 2015;12:113. doi: 10.1186/s12966-015-0274-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dumith S.C., Gigante D.P., Domingues M.R. Physical activity change during adolescence: A systematic review and a pooled analysis. Int J Epidemiol. 2011;40:685–698. doi: 10.1093/ije/dyq272. [DOI] [PubMed] [Google Scholar]
- 14.Reilly J.J., Penpraze V., Hislop J. Objective measurement of physical activity and sedentary behaviour: Review with new data. Arch Dis Child. 2008;93:614–619. doi: 10.1136/adc.2007.133272. [DOI] [PubMed] [Google Scholar]
- 15.Pratt M., Sarmiento O.L., Montes F. The implications of megatrends in information and communication technology and transportation for changes in global physical activity. Lancet. 2012;380:282–293. doi: 10.1016/S0140-6736(12)60736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Christakis D.A. Interactive media use at younger than the age of 2 years: time to rethink the American Academy of Pediatrics guideline? JAMA Pediatr. 2014;168:399–400. doi: 10.1001/jamapediatrics.2013.5081. [DOI] [PubMed] [Google Scholar]
- 17.Basterfield L., Adamson A.J., Frary J.K. Longitudinal study of physical activity and sedentary behavior in children. Pediatrics. 2011;127:e24–e30. doi: 10.1542/peds.2010-1935. [DOI] [PubMed] [Google Scholar]
- 18.Hughes A.R., Stewart L., Chapple J. Randomized, controlled trial of a best-practice individualized behavioral program for treatment of childhood overweight: Scottish Childhood Overweight Treatment Trial (SCOTT) Pediatrics. 2008;121:e539–e546. doi: 10.1542/peds.2007-1786. [DOI] [PubMed] [Google Scholar]
- 19.Bauman A.E., Reis R.S., Sallis J.F. Correlates of physical activity: Why are some people physically active and others not? Lancet. 2012;380:258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 20.Wells J.C., Coward W.A., Cole T.J. The contribution of fat and fat-free tissue to body mass index in contemporary children and the reference child. Int J Obes Relat Metab Disord. 2002;10:1323–1328. doi: 10.1038/sj.ijo.0802077. [DOI] [PubMed] [Google Scholar]
- 21.Ruxton C.H.S., Reilly J.J., Kirk T.R. Body composition of healthy 7- and 8-year-old children and a comparison with the ‘reference child’. Int J Obes (Lond) 1999;23:1276–1281. doi: 10.1038/sj.ijo.0801067. [DOI] [PubMed] [Google Scholar]
- 22.Harding S.K., Page A.S., Falconer C. Longitudinal changes in sedentary time and physical activity during adolescence. Int J Behav Nutr Phys Act. 2015;12:44. doi: 10.1186/s12966-015-0204-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell J.A., Pate R.R., Dowda M. A prospective study of sedentary behavior in a large cohort of youth. Med Sci Sports Exerc. 2012;44:1081–1087. doi: 10.1249/MSS.0b013e3182446c65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Corder K., Sharp S.J., Atkin A.J. Change in objectively measured physical activity during the transition to adolescence. Br J Sports Med. 2015;49:730–736. doi: 10.1136/bjsports-2013-093190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Collings P.J., Wijndaele K., Corder K. Magnitude and determinants of change in objectively-measured physical activity, sedentary time and sleep duration from ages 15 to 17.5y in UK adolescents: the ROOTS study. Int J Behav Nutr Phys Act. 2015;12:61. doi: 10.1186/s12966-015-0222-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nader P.R., Bradley R.H., Houts R.M. Moderate-to-vigorous physical activity from ages 9 to 15 years. JAMA. 2008;300:295–305. doi: 10.1001/jama.300.3.295. [DOI] [PubMed] [Google Scholar]
- 27.Pearson N., Braithwaite R.E., Biddle S.J. Associations between sedentary behaviour and physical activity in children and adolescents: A meta-analysis. Obes Rev. 2014;15:666–675. doi: 10.1111/obr.12188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tanaka C., Reilly J.J., Huang W.Y. Longitudinal changes in objectively measured sedentary behaviour and their relationship with adiposity in children and adolescents: Systematic review and evidence appraisal. Obes Rev. 2014;15:791–803. doi: 10.1111/obr.12195. [DOI] [PubMed] [Google Scholar]
- 29.Wilkin T.J. Can we modulate physical activity in children? No. Int J Obes (Lond) 2011;35:1270–1276. doi: 10.1038/ijo.2011.163. [DOI] [PubMed] [Google Scholar]
- 30.Reilly J.J. Can we modulate physical activity in children? Int J Obes (Lond) 2011;35:1266–1269. doi: 10.1038/ijo.2011.62. [DOI] [PubMed] [Google Scholar]
- 31.Kwon S., Janz K.F., Letuchy E.M. Developmental trajectories of physical activity, sports, and television viewing during childhood to young adulthood: Iowa Bone Development Study. JAMA Pediatr. 2015;169:666–672. doi: 10.1001/jamapediatrics.2015.0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Basterfield L., Adamson A.J., Parkinson K.N. Surveillance of physical activity in the UK is flawed: validation of the Health Survey for England physical activity questionnaire. Arch Dis Child. 2008;93:1054–1058. doi: 10.1136/adc.2007.135905. [DOI] [PubMed] [Google Scholar]
- 33.World Health Organization Europe . World Health Organization; Geneva, Switzerland: 2015. United Kingdom of Great Britain and Northern Ireland Physical Activity Factsheet. [Google Scholar]
- 34.British Heart Foundation. Physical Activity Statistics 2015. Available from: www.bhf.org.uk [Accessed 31 Mar 2016].
- 35.UK Association for Physical Education. Health Position Paper 2015. www.afpe.org.uk/advocacy-a-leadership/afpe-policy-statements/health Accessed 29.03.16.
- 36.Reilly J.J., Dick S., McNeill G. Results from Scotland's 2013 Report Card on Physical Activity for Children and Youth. J Phys Act Health. 2014;11(Suppl 1):S93–S97. doi: 10.1123/jpah.2014-0183. [DOI] [PubMed] [Google Scholar]
- 37.Gillis L., Tomkinson G., Olds T. Research priorities in child and adolescent physical activity and sedentary behaviour: a global perspective using a twin-panel Delphi procedure. Int J Behav Nutr Phys Act. 2013;10:112. doi: 10.1186/1479-5868-10-112. [DOI] [PMC free article] [PubMed] [Google Scholar]