Introduction
Among parents’ foremost developmental concerns are cognitive delays, in particular delays in language and adaptive function. Both are features of intellectual disability (ID), or, when language is specifically affected, language disorders. Child psychiatrists will frequently encounter these conditions, particularly as they are associated with an increased risk of challenging behaviors and psychopathology. In working with affected children and their families, child psychiatrists should be prepared to identify relevant signs and symptoms, manage psychiatric comorbidities, refer to specialists for comprehensive assessment and multidisciplinary treatments, and foster family-centered care. Child psychiatrists thus play an important role in addressing the multifaceted nature of these conditions and in optimizing independence and functional outcomes.
Intellectual Disability
Intellectual disability (ID) is a neurodevelopmental disorder characterized by 3 features (1):
deficits in cognition,
deficits in adaptive function, and
onset during the developmental period.
Collective attitudes towards ID have shifted from a model of static deficiencies to a more dynamic, strength-based perspective, and “mental retardation,” the prior diagnostic term, has fallen out of favor. The introduction of “Intellectual Disability” in DSM 5 was presaged by Rosa’s Law, a 2010 federal statute requiring that intellectual disability replace mental retardation in health, legal and educational policy (P.L. 111-256). Also in contrast to DSM-IV-TR, absolute IQ cut-offs no longer define severity; mild, moderate, severe, or profound ID is now classified by level of adaptive functioning within a range of IQ scores. Adaptive functioning encompasses 3 domains:
the conceptual domain, which includes language, knowledge, and memory;
the social domain, which includes empathy, social judgment, and rule-following ability; and
the practical domain, which includes self-care, organization, and daily living skills.
Estimates of intellectual disability range between 1–3%, with a male to female ratio of 1.6:1 (2). Causes of ID include genetic abnormalities, as well as prenatal, perinatal, and postnatal environmental factors (3, 4)(Figure 1). Suspicion of ID can arise during infancy, although children under 5 years of age are typically diagnosed with global developmental delay, which requires delays in 2 or more functional domains and shows some correlation with ID. ID can be determined with greater certainty by age 5 years, when cognitive abilities become more stable. Children with less severe ID may not be diagnosed until school age, when academic demands highlight weaknesses in cognition (5). Outcomes vary depending on severity – individuals with mild ID may achieve some signs of independence, such as having a job or starting a family (6), although more severe ID requires long-term community supports for housing, occupational, and recreational activities.
Figure 1.
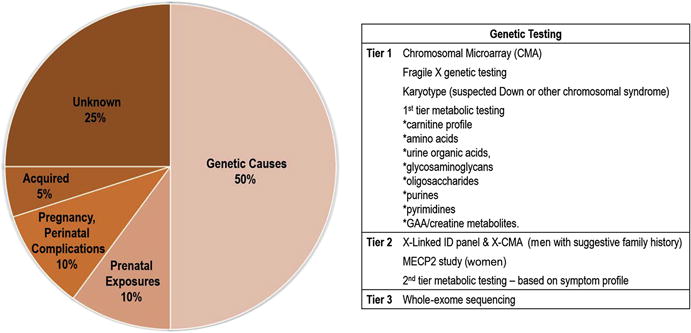
Causes of ID and their respective percentages are shown, together with a list of currently recommended genetic testing. Several non-genetic factors also lead to ID, including congenital infections, exposures to teratogens or toxins, prematurity, hypoxia, trauma, intracranial hemorrhage, central nervous system infection or malignancy, psychosocial deprivation, malnutrition, or acquired hypothyroidism.
Data from Moeschler JB, Shevell M. Comprehensive Evaluation of the Child With Intellectual Disability or Global Developmental Delays. Pediatrics 2014;134(3):e903-e918; and Pivalizza P, Lalani SR. Intellectual disability in children: Evaluation for a cause. UpToDate. Waltham, MA; 2016.
Evaluation
A comprehensive history entails a birth/prenatal history, family history, 3-generation pedigree, and information on the course and timing of delays in language, motor, social-emotional, and adaptive functioning (7). Children with ID may have a history of delays in talking, sitting up, crawling or walking; immature play and social interaction; and poor comprehension, learning, and problem solving. Screening tools, such as the Ages and Stages Questionnaire (8) can usefully clarify the extent of these concerns (see (9) for other examples). Frequent neurological comorbidities, such as seizures and motor signs (e.g., spasticity, ataxia, hypotonia), as well as developmental regression, should be assessed. Physical examination includes a complete neurological examination, measurement of head circumference, and attention to features associated with genetic syndromes, such as facial dysmorphisms and skin findings (3). A comprehensive evaluation of intellectual and adaptive functioning through neuropsychological testing is ultimately necessary for diagnosis.
Medical work-up includes testing for genetic syndromes, metabolic disorders, acquired hypothyroidism, and lead exposure (3). When a genetic syndrome or metabolic disorder is suspected, referral to a geneticist is recommended to assure the most comprehensive testing. A neurology referral is recommended for any neurologic concerns. A brain MRI is advised if microcephaly, macrocephaly, seizures, or neurologic signs are present (7, 10). Children with ID are more likely to have other medical conditions, including cataracts, vision and hearing impairments, congenital heart disease, constipation, obesity, and sleep disorders, which may prompt additional referrals. Such comorbidities not only impact overall function and quality of life, but can also increase challenging behaviors.
Differential Diagnosis
The differential diagnosis for ID includes other neurodevelopmental disorders, which can also be comorbid with ID:
Autism spectrum disorder (ASD), which exhibits a similar prevalence as ID, is characterized by impaired social communication, restricted interests, and repetitive behaviors. At least 25% of children with ASD have ID (11).
Language disorders, like ID, feature language delays. The occurrence of language delay should prompt investigation of other delays, so that ID is not overlooked.
Epilepsy may manifest with delays and regression in core developmental domains, such as language. Behaviors suggestive of epilepsy including staring spells, shaking spells, and intermittent changes in levels of consciousness with associated automatisms (e.g., blinking, lip smacking).
These potential diagnostic confounds highlight the importance of comprehensive evaluations and neuropsychological testing.
Challenging Behaviors, Comorbidity, and Management
Challenging behaviors are very common in ID and can be more strongly associated with parental stress than level of delay (12). These may include non-compliance, property destruction, tantrums, meltdowns, and physical aggression towards self or others. While challenging behaviors occur in 4–9% of typically developing children, they occur in 25% of children with ID (13). A major factor in ID stems from communication impairment, which limits the ability to express frustration and/or explain external factors or underlying physical or emotional distress. Children and adolescents with ID are also known to have higher prevalence of psychiatric disorders, including ADHD, mood disorders, anxiety disorders, and psychotic disorders (14).
The psychopharmacological evidence base is relatively limited in ID, although there is support for judicious use of medication for disruptive behaviors and psychiatric comorbidities (15, 16). Box 1 lists common medication classes, typical uses, side effects, and suggested monitoring. In preschoolers, behavioral treatment options are first-line, given their effectiveness and more frequent medication side effects in younger children. Nevertheless, when safety or ability to engage in therapy are concerns, medication may be instrumental for successful implementation of a treatment plan and reducing caregiver stress. Medication is also an element of combined therapy (medication plus behavioral management), and psychiatrists can guide the appropriate balance of behavior and medication. Low starting doses are recommended, with slow titration, along with systematic evaluation of both positive and negative effects in the context of the entire treatment plan.
Box 1. Medications for ID.
| Medications By Class | Target Behaviors | Adverse Effects | Monitoring |
| Typical Antipsychotics (e.g haloperidol, chlorpromazine) | Agitation, aggression, hyperactivity, self-injury | Extrapyramidal symptoms, tardive dyskinesia | AIMS |
| Atypical Antipsychotics (e.g risperidone, aripiprazole, olanzapine) | Irritability, aggressiveness, hyperactivity, self- injurious behavior, repetitive behaviors | Weight gain, somnolence, increased risk of diabetes, extrapyramidal symptoms, akathisia, tardive dyskinesia | Blood glucose, HbA1C, lipids AIMS |
| Mood Stabilizers (e.g., lithium, valproic acid, carbamazepine) | Mood lability, aggression, impulsivity, self-injurious behavior | Lithium: tremor, renal and thyroid toxicity, Valproate: tremor, sedation, weight gain Carbamazepine: nausea, vomiting | Renal and thyroid monitoring for lithium, liver function tests, CBC, and ammonia with valproic acid, regular drug levels for all three |
| SSRIs (e.g fluoxetine, sertraline, fluvoxamine) | Depressed mood, anxiety, self-injurious behavior, repetitive behaviors | Activation, agitation, aggression, nausea | None specific |
| Stimulants (e.g methylphenidate) | Hyperactivity, inattention, impulsivity | Loss of appetite, insomnia, depressed mood | Height, weight, vital signs |
| Alpha-agonists (e.g. clonidine, guanfacine) | Hyperactivity, inattention, impulsivity, tics | Hypotension, sedation, increased depression | Vital signs |
Abbreviations: AIMS, Abnormal Involuntary Movement Scale; CBC, complete blood count; HbA1c, hemoglobin A1c; SSRI, selective serotonin reuptake inhibitor.
Data from Handen BL, Gilchrist R. Practitioner Review: Psychopharmacology in children and adolescents with mental retardation. J Child Psychol Psychiatry 2006;47(9):871–82.
Among behavioral treatments, applied behavioral analysis (ABA) has a well-established evidence base (17). ABA attempts to modify antecedents and/or consequences of specific behaviors, either to discourage a problematic behavior or encourage an alternative behavior. Functional behavioral analyses provide detailed measurement of potential instigators of challenging behavior, such as need for attention or help, escape from demands, attempt to get what is wanted, protest, or self-stimulation (13). Behavioral planning is then tailored to a child’s behavioral profile and developmental level. In addition to ABA, parent-training approaches, e.g. Stepping Stones Triple P (18) and Parent Child Interaction Therapy (19), show evidence for improving disruptive behaviors in ID.
Promotion of Developmental Progress
Children with ID/global developmental delay benefit from intensive early intervention and multidisciplinary services (20). Federal law under the Individuals with Disability Education Act (IDEA) mandates that state-run programs identify children with disabilities and provide developmental services. Prior to age 3, families will receive an Individualized Family Service Plan (IFSP), which will implement an individualized program of services and developmental therapies. These may include speech and language therapy, occupational and physical therapy, psychological and behavioral services, medical services, nutrition counseling, assistive technology, family counseling and training, home visitation, and social services. The IFSP applies for ages 0-3 years, after which children who qualify for ongoing services are transitioned to an Individual Education Plan (IEP) with multidisciplinary preschool programming.
Language Disorders
In DSM 5, language disorders are classified as communication disorders. Communication comprises all verbal and nonverbal input used to transmit information between individuals, including language and speech. Language involves conveying information through the form, content, and function of symbolic systems according to specified rules (Figure 2). Speech is the oral production of language. Delayed talking may thus reflect disturbances in speech, language, and/or communication. Historically, language disorders have been referred to by a variety of terms, including developmental language disorders and specific language impairment. This section focuses on early childhood features of language disorders per DSM 5, which implicate language form and function (Figure 2).
Figure 2.
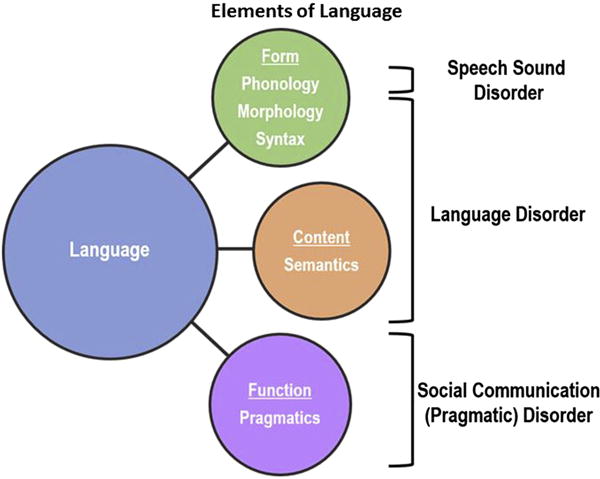
Language disorders affect one or more fundamental aspects of language: form, content, and function. Deficits may involve morphology (understanding and use of the building blocks of words), syntax (grammar), and semantics (vocabulary). Phonology, the ability to distinguish and use speech sounds appropriately, is affected in Speech Sound Disorder. Disorders of pragmatics, the use of language, are encompassed within Social Communication (Pragmatic) Disorder.
Prevalence estimates for language disorder generally range between 3 and 8% (21, 22), with a male to female ratio of 1.33:1 in an epidemiologic sample (21). Language disorders are heritable and generally appear polygenic, although some specific genetic factors, including the FOXP2 gene and linkage markers on chromosomes 3, 6, and 19, have been identified (23). Language disorders can also be acquired secondary to infection, brain injury, neglect, and abuse.
Early language difficulties are a risk factor for impaired literacy skills, memory skills, and nonverbal abilities (24, 25), although individual patterns of strengths and weaknesses in distinct aspects of language may vary over time. In some cases, “illusory recovery” occurs (26), whereby a child’s language appears to normalize, but deficits resurface with subsequent increases in demands. Additionally, rates of language growth may plateau by early adolescence, increasing the gap between children with and without language disorders (27). Receptive language impairments have worse prognoses than expressive language impairments. Deficits of comprehension are less responsive to therapy and do not resolve spontaneously; they are linked to increased likelihood of social difficulties (28), struggles with nonverbal reasoning (29), and psychiatric conditions (30).
Language Delay and “Late Talkers” vs. Language Disorder
Natural variability in language acquisition can make it challenging to assess early delays and to distinguish them from language disorders, which involve more persistent symptoms. Prevalence of late language emergence in 2-year-old children ranges between 10% and 20% (31), and males are 3 times more likely to be affected (32, 33). The majority of these children do not ultimately have language disorders (34). This “late-talkers” group may have only a few words at age 2 years, but by age 3 years matches peers in expressive language skills (34, 35).
Because only some children with late language emergence will have language disorders, assessment and management of this group has been debated. Compared to those who develop language disorders, late talkers use more communicative gestures (36), are less likely to have receptive language delay (37), and exhibit better recall of sentences on standardized testing (38). Nonetheless, toddlers and preschoolers with late language emergence should be referred to a speech/language therapist, as they may be at risk for later language and literacy difficulties (39). In the presence of associated risk factors for language disorders, such as ASD, global developmental delay, or hearing impairment, direct speech and language services are generally indicated. For children at lower risk, periodic monitoring is recommended, together with guidance for parents to provide indirect language stimulation (Box 2). If persistent delays or additional developmental concerns arise, a complete assessment and direct intervention may be warranted.
Box 2. Indirect stimulation of language competence in young children.
Responsiveness
Provide responses directly related to a child’s communication act or focus of attention.
Follow the child’s lead in play.
Discuss what the child is doing versus asking lots questions.
Language Modeling
Imitate or expand the child’s actions or words.
Rephrase what the child says in grammatically correct form.
Provide examples of using gestures and other nonverbal cues.
Reinforcement of Communication
Provide opportunities to communicate wants and choices rather than anticipate all the child’s needs.
Allow adequate time to initiate communication and respond.
Praise communication attempts.
Data from American Speech-Language-Hearing Association (n.d.). Spoken Language Disorders (Practice Portal). Available at: www.asha.org/Practice-Portal/Clinical-Topics/SpokenLanguageDisorders. Accessed Oct 1 2016.
Evaluation
The history should review not only language development and milestones, but also any other delays, challenging behaviors, mood and anxiety, and trauma which could result in developmental setbacks. In language disorders, progress is generally slow from the outset, and regression is uncommon, unlike ASD (40). Although speech delays frequently co-occur, they are not a hallmark. Box 3 provides a description of typical language milestones and clinically significant red flags. Impaired receptive and expressive language commonly co-occur, and difficulties with comprehension, in particular, are a red flag for chronic language difficulties (41). The mental status examination should note form, function, and use of language, including articulation, fluency, and tone, comprehension, the frequency and complexity of verbal communication, vocabulary, social reciprocity, and use and responsiveness to nonverbal communication, such as gestures, body language, and facial expression.
Box 3. Language Milestones and Red Flags.
| Receptive | Expressive | Receptive | Expressive | |
|---|---|---|---|---|
| 12 months | Recognizes words as symbols for objects, 3–50 words, recognizes name | First words, communicative games | Does not respond to name or gestures | No babbling, pointing, gesturing |
| 18 months | Words are understood outside context of routine games | 50–100 words, intents include requesting, answering questions, acknowledging | Does not follow 1- step directions | No “ma-ma,” “da- da,” or other names |
| 2 years | Single words for objects out of sight | 200–300 words, two- word utterances, telegraphic speech with few grammar markers, symbolic play, speech is 50% intelligible | Does not point to pictures or other body parts when named | Does not use at least 25 words |
| 2.5 years | What/who/where questions | Use of questions, early emerging grammar, narratives are primarily labels and descriptions | Does not verbally respond or nod/shake head to questions | Does not combine 2 words into unique phrases |
| 3 years | Why questions and basic spatial terms (in/on/under); simple time concepts (e.g., tomorrow) | Simple sentences, Narratives are sequences with them but no plot, speech is 75% intelligible | Does not understand prepositions or action words, does not follow 2-step instructions | Does not use at least 200 words, does not ask for things by name, repeats phrases in response to questions, unintelligible most of the time |
| 4 years | When/how questions, basic colors, shapes, sizes | Can tell a story, uses conjunctions to conjoin sentences; speech is 100% intelligible | Poor understanding of instructions or question words | Disordered speech, no 5–6 word phrases, echolalia, unintelligible most of the time |
| 5 years | Letter names and sounds; numbers and counting | Correct use of past tense, Uses conjunction words when, so, because, if; Narratives are chains with some plot | Poor understanding of instructions or question words | Unintelligible most of the time, deletes parts of words, echolalia, can’t describe short sequences of events |
| Any age | Regression or loss of milestones | |||
Data from Chapman R. Children’s language learning: An interactionist perspective. Journal of Child Psychology and Psychiatry 2000; 41:33–54; and Miller J. Assessing language production in children. Boston, MA: Allyn & Bacon; 1981.
The utility of language screeners has been deemed inconclusive (42), although in cases of clinical suspicion, screeners can help index the level of concern. Two accessible parent-report measures are the MacArthur Communicative Development Inventory (M-CDI) (43) and the Language Development Survey (LDS) (31). The M-CDI features long and short versions (requiring 20 and 5 minutes, respectively) for ages between 8 and 36 months. The LDS, which applies up to 42 months, is embedded in the Child Behavior Checklist, which conveniently queries general behavioral concerns. It is also worthwhile to screen for anomalous social development, given the association of language delay and ASD. Two of the more common brief ASD screeners are the Modified Checklist for Autism (M-CHAT), for ages 16-30 months (44), and the Social Communication Questionnaire, for ages over 4 years (45).
Medical work-up first involves ruling out hearing conditions, and referral for an audiological evaluation is an important initial step. An oral-motor evaluation should be considered if there are phonological concerns, or the child has feeding difficulties or drooling. For laboratory testing, a CBC may be considered to evaluate for anemia, which has been associated with developmental delay, as well as lead testing (46). Genetic testing is not routine, as there are no common, strongly associated genetic markers of language disorders (47), but a genetics referral is advised for features suggesting a genetic syndrome (see above). In cases of regression or concern for seizures, rapid referral to a neurologist is warranted.
Differential Diagnosis
Several conditions may present with communication difficulties in early childhood; in some cases, these may be comorbid with language disorders, so that a speech/language referral remains indicated:
Hearing impairment: As mentioned above, this possibility should be considered early in the evaluation. For children with ID and impaired language, there is a risk of reduced hearing over time, and hearing should therefore be monitored.
ID: Language delays frequently occur in ID, although only a subset of individuals ultimately shows deficiencies consistent with a language disorder. Marked language problems in individuals with ID should receive comprehensive evaluation and treatment.
ASD: Language delay and disorders are common in ASD, even when accounting for pragmatic language issues, which are universal. Consideration of ASD is important given the strong benefit of early intervention for ASD.
ADHD: Inattention and impulsivity may detract from opportunities to learn and practice language skills, particularly as related to pragmatics. Children with ADHD also have higher rates of language disorders.
Selective mutism: In this condition, poor language output manifests in specific environments, e.g., at school but not at home. Selective mutism is conceptualized as an anxiety disorder, although speech/language issues often co-occur.
Challenging Behavior and Comorbidities
Similar to children with ID, children with language disorders are at increased risk of challenging behaviors and psychiatric co-morbidities. Among children with a language disorder, 40–75% exhibit challenging behaviors (48) and 30–50% have psychiatric disorders (49, 50), most commonly ADHD, anxiety disorders, conduct disorders, and mood disorders. Conversely, research suggests that 40% of children with psychiatric diagnoses also have a language impairment (51). Work by Beitchman and colleagues showed that increased rates of psychiatric diagnoses continue up to early adulthood (52), and decreased psychiatric comorbidity was associated with special education (53).
Common challenging behaviors include both internalizing and externalizing symptoms. Hyperactivity and attentional difficulties are frequently observed (54, 55), as well as shyness, social withdrawal, and poor self-esteem (56). Socioemotional deficits may also be present, including difficulty inferring emotional reactions (57) and regulating emotions (58). As children get older, they may struggle with forming and maintaining close relationships (59), and are more likely to be bullied (60) and experience abuse (61).
Management
Psychiatrists play an important role in managing psychiatric comorbidities, as well as monitoring progress and coordinating care. In addition to making a speech/language referral, they can assist families in obtaining an evaluation for an IFSP or IEP and advocate for further services or educational accommodations. Because psychiatrists are in a position to correlate language function with psychiatric symptoms, they can provide important contextual information about the relationship between a child’s language function and associated behavioral concerns. This information may result in more appropriately structured and targeted behavioral interventions and reduce misattributions of challenging behavior (62).
Language Interventions: Principles, Approaches, and Modalities
Language intervention aim to enhance language output and comprehension, ensure access to academic content, and advance communication to the next developmental level. Principles of effective intervention include language facilitation in the context of communication; dynamic, generalizable interventions; regular assessment of response; and adaptation of treatment goals and strategies according to individual learning style, progress, and needs (63). Early intervention is recommended, as accelerated language growth tends to occur earlier vs. later in childhood (41, 64), and earlier (65) as well as longer duration of intervention have been shown to be more effective (66). A meta-analysis of speech/language therapies supported efficacy in expressive, but not receptive, language impairment, and treatments over 8 weeks showed better results (67).
Language interventions encompass a variety of approaches, treatment types, and modalities (Box 4). Therapy should be based on the child’s specific needs and learning style, as identified by standardized testing, parental concerns, and teacher input. Targets are identified and learned through drill, repetition, and carryover tracking. For preschoolers, goals will include augmenting vocabulary, conceptual understanding, and sentence variety and complexity. Associated communication targets may involve improving intelligibility and phonological awareness, as well as conversational and narrative skills. Social skills should also be emphasized, given the known interrelationship of social and language function.
Box 4. Overview of Evidence-Based Aspects of Language Interventions.
| Approach Key | Features | Comments |
|---|---|---|
| Clinician-directed *Clinician |
specifies treatment type, goals, and reinforcement | *Less
naturalistic *Maximize practice of specific targets |
| Child-directed *Clinician |
provides naturalistic opportunities for a
child response *Clinician follows the child’s lead |
*Useful when poor compliance with
clinician-directed approaches *Useful for “unassertive communicators” |
| Parent-mediated | *Parents use direct,
individualized intervention practices with their
child *Increased opportunity for language input |
*Cost
effective *Growing evidence for early intervention |
| Treatment Type | Key Features | Comments |
| Behavioral Therapies | *Use behavioral learning
principles *Increase desired behaviors *Decrease inappropriate behaviors |
*Instructional: Discrete Trial
Training *Play-based: Pivotal Response Training *Frequently used ASD and DD |
| Milieu Therapy | *Therapist elicits and reinforces
targeted responses *Naturalistic settings *Child may select topic to initiate interaction |
*Evidence in several groups: late-talkers, ASD, ID, children from high-risk and low income families |
| Relationship Based Approaches | *Promotes parent-child
interactions *Common in early intervention programs |
*Greenspan/DIR/Floortime
encourages interaction through play *Used in ASD |
| Modalities Key | Features | Comments |
| Augmentative Alternative Communication | *Supplemental methods to replace
speech *Can address impaired production or comprehension |
*Aided symbols: Picture Exchange
Communication System (PECS) and speech generating
devices *Unaided symbols: manual signs *Strong evidence in ASD & ID |
| Computer Based Instruction | *Computer programs teach language skills | *Advantage of higher number of
trials than with therapist *Example: FastForWord |
| Video Modeling | *Videos show desired
behaviors *Learners are video-taped *Practice videos are reviewed |
*Parent-mediated example: Hanen Program |
Abbreviations: DD, development delay; DIR, Developmental Individual-difference Relationship
Data from American Speech-Language-Hearing Association (n.d.). Spoken Language Disorders (Practice Portal). Available at: www.asha.org/Practice-Portal/Clinical-Topics/SpokenLanguageDisorders. Accessed Oct 1 2016.
In preschoolers with emerging language skills, parent-mediated interventions are often implemented. These confer similar benefit as direct approaches by a speech/language pathologist (67), are well-suited to language facilitation in a variety of naturalistic environments, and offer many opportunities for language input. Among therapeutic modalities, augmentative and alternative communication has accumulated a relatively large body of evidence, especially in children with developmental delays (68). Some concern has been expressed that augmentative forms of communication may replace speech entirely and therefore restrict the child’s communicative development; however, prevailing evidence suggests that augmentative communication promotes language development.
Discussion
Common Aspects of Managing ID and Language Disorders
Management of ID and language disorders shares several overarching features and principles. Because comprehensive assessments from other specialties are needed for diagnosis, sound clinical judgment must be exercised regarding referrals and following up on recommendations. The long-term impact and early emergence of these conditions is especially challenging for families; sensitivity and clarity are thus vital when delivering these diagnoses. Surveillance often occurs via a multidisciplinary team of speech and language pathologists, behavioral therapists, occupational and physical therapists, educators, social workers, and others. Maintaining clear communication and a strength-based perspective is important for implementation of therapies which promote ongoing learning and gains in adaptive function. Finally, the importance of culturally sensitive, family-centered care is increasingly emphasized. By respectfully listening to families, psychiatrists can ensure that their preferences and priorities contribute to treatment planning.
Future Directions
Although early childhood mental health and neurodevelopmental disorders are increasingly recognized, concerns remain for delays in diagnosis (69, 70). Development of improved screeners and expanded training for child psychiatrists in neurodevelopmental disorders (71) are worthwhile public health considerations to promote earlier identification and management. Further research on evidence-based treatment is also a priority, since extant literature frequently involves small samples or less rigorous study designs. Translational research in genetics, as well as neuroscience, will be important to elucidate mechanisms by which cognitive impairments interact with risk for psychopathology, thereby improving diagnostic sensitivity, treatments, and prevention.
Key Points.
-
*
Intellectual disability (ID) and language disorders are neurodevelopmental conditions arising in early childhood.
-
*
Child psychiatrists are likely to encounter children with ID and language disorders as both are strongly associated with challenging behaviors and psychopathology.
-
*
Because early intervention is associated with optimal outcomes in ID and Language Disorders, child psychiatrists must be aware of their signs and symptoms, particularly as related to delays in cognitive and adaptive function.
-
*
Optimal management of both ID and language disorders requires a multidisciplinary, team-based, and family-centered approach. Child psychiatrists play an important role on this team, given their expertise with contextualizing and treating challenging behaviors.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 2.Leonard H, Wen X. The epidemiology of mental retardation: challenges and opportunities in the new millennium. Ment Retard Dev Disabil Res Rev. 2002;8(3):117–34. doi: 10.1002/mrdd.10031. [DOI] [PubMed] [Google Scholar]
- 3.Pivalizza P, Seema L. Intellectual disability in children: Evaluation for a cause. In: Post T, editor. UpToDate. Waltham, MA: 2016. [Google Scholar]
- 4.Toth K, deLacy N, King BH. Intellectual disability. In: Dulcan MK, editor. Dulcan's textbook of child and adolescent psychiatry. 2nd 2016. [Google Scholar]
- 5.Reschly DJ. Documenting the developmental origins of mild mental retardation. Applied neuropsychology. 2009;16(2):124–34. doi: 10.1080/09084280902864469. [DOI] [PubMed] [Google Scholar]
- 6.Hall I, Strydom A, Richards M, Hardy R, Bernal J, Wadsworth M. Social outcomes in adulthood of children with intellectual impairment: evidence from a birth cohort. J Intellect Disabil Res. 2005;49(Pt 3):171–82. doi: 10.1111/j.1365-2788.2005.00636.x. [DOI] [PubMed] [Google Scholar]
- 7.Curry CJ, Stevenson RE, Aughton D, Byrne J, Carey JC, Cassidy S, et al. Evaluation of mental retardation: recommendations of a Consensus Conference: American College of Medical Genetics. American journal of medical genetics. 1997;72(4):468–77. doi: 10.1002/(sici)1096-8628(19971112)72:4<468::aid-ajmg18>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 8.Squires JPL, Bricker D. The ASQ User’s Guide for the Ages and Stages Questionnaire: A parent - completed, child monitoring system. 2nd. Baltimore, MD: Paul Brookes Publishing Comp; 1990. [Google Scholar]
- 9.Mackrides PS, Ryherd SJ. Screening for developmental delay. American family physician. 2011;84(5):544–9. [PubMed] [Google Scholar]
- 10.Moeschler JB, Shevell M. Comprehensive Evaluation of the Child With Intellectual Disability or Global Developmental Delays. Pediatrics. 2014;134(3):e903. doi: 10.1542/peds.2014-1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chakrabarti S, Fombonne E. PErvasive developmental disorders in preschool children. JAMA. 2001;285(24):3093–9. doi: 10.1001/jama.285.24.3093. [DOI] [PubMed] [Google Scholar]
- 12.Baker BL, McIntyre LL, Blacher J, Crnic K, Edelbrock C, Low C. Pre-school children with and without developmental delay: behaviour problems and parenting stress over time. J Intellect Disabil Res. 2003;47(Pt 4–5):217–30. doi: 10.1046/j.1365-2788.2003.00484.x. [DOI] [PubMed] [Google Scholar]
- 13.Harris JC. Intellectual Disability: A Guide for Families and Professionals. New York, New York: Oxford University Press; 2010. [Google Scholar]
- 14.Einfeld SL, Ellis LA, Emerson E. Comorbidity of intellectual disability and mental disorder in children and adolescents: a systematic review. Journal of intellectual & developmental disability. 2011;36(2):137–43. doi: 10.1080/13668250.2011.572548. [DOI] [PubMed] [Google Scholar]
- 15.McQuire C, Hassiotis A, Harrison B, Pilling S. Pharmacological interventions for challenging behaviour in children with intellectual disabilities: a systematic review and meta-analysis. BMC psychiatry. 2015;15:303. doi: 10.1186/s12888-015-0688-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Handen BL, Gilchrist R. Practitioner Review: Psychopharmacology in children and adolescents with mental retardation. Journal of Child Psychology and Psychiatry. 2006;47(9):871–82. doi: 10.1111/j.1469-7610.2006.01588.x. [DOI] [PubMed] [Google Scholar]
- 17.Beavers GA, Iwata BA, Lerman DC. Thirty years of research on the functional analysis of problem behavior. Journal of applied behavior analysis. 2013;46(1):1–21. doi: 10.1002/jaba.30. [DOI] [PubMed] [Google Scholar]
- 18.Tellegen CL, Sanders MR. Stepping Stones Triple P-Positive Parenting Program for children with disability: A systematic review and meta-analysis. Research in developmental disabilities. 2013;34(5):1556–71. doi: 10.1016/j.ridd.2013.01.022. [DOI] [PubMed] [Google Scholar]
- 19.Bagner DM, Eyberg SM. Parent-child interaction therapy for disruptive behavior in children with mental retardation: a randomized controlled trial. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53. 2007;36(3):418–29. doi: 10.1080/15374410701448448. [DOI] [PubMed] [Google Scholar]
- 20.Sturmey PaD Robert. Evidence-Based Practice and Intellectual Disabilities. West Sussex, UK: Wiley Blackwell; 2014. [Google Scholar]
- 21.Tomblin JB, Records NL, Buckwalter P, Zhang X, Smith E, O’Brien M. Prevalence of Specific Language Impairment in Kindergarten Children. Journal of Speech, Language, and Hearing Research. 1997;40(6):1245–60. doi: 10.1044/jslhr.4006.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Law J, Boyle J, Harris F, Harkness A, Nye C. Prevalence and natural history of primary speech and language delay: findings from a systematic review of the literature. International journal of language & communication disorders/Royal College of Speech & Language Therapists. 2000;35(2):165–88. doi: 10.1080/136828200247133. [DOI] [PubMed] [Google Scholar]
- 23.Newbury DF, Monaco AP. Genetic advances in the study of speech and language disorders. Neuron. 2010;68(2):309–20. doi: 10.1016/j.neuron.2010.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.St Clair MC, Pickles A, Durkin K, Conti-Ramsden G. A longitudinal study of behavioral, emotional and social difficulties in individuals with a history of specific language impairment (SLI) Journal of communication disorders. 2011;44(2):186–99. doi: 10.1016/j.jcomdis.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 25.Conti-Ramsden G, Durkin K, Simkin Z, Knox E. Specific language impairment and school outcomes. I: identifying and explaining variability at the end of compulsory education. International journal of language & communication disorders/Royal College of Speech & Language Therapists. 2009;44(1):15–35. doi: 10.1080/13682820801921601. [DOI] [PubMed] [Google Scholar]
- 26.Scarborough HS, Dobrich W. Development of children with early language delay. Journal of speech and hearing research. 1990;33(1):70–83. doi: 10.1044/jshr.3301.70. [DOI] [PubMed] [Google Scholar]
- 27.Rice ML. Language growth and genetics of specific language impairment. International journal of speech-language pathology. 2013;15(3):223–33. doi: 10.3109/17549507.2013.783113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clegg J, Hollis C, Mawhood L, Rutter M. Developmental language disorders–a follow-up in later adult life. Cognitive, language and psychosocial outcomes. Journal of child psychology and psychiatry, and allied disciplines. 2005;46(2):128–49. doi: 10.1111/j.1469-7610.2004.00342.x. [DOI] [PubMed] [Google Scholar]
- 29.Stothard SE, Snowling MJ, Bishop DV, Chipchase BB, Kaplan CA. Language-impaired preschoolers: a follow-up into adolescence. Journal of speech, language, and hearing research : JSLHR. 1998;41(2):407–18. doi: 10.1044/jslhr.4102.407. [DOI] [PubMed] [Google Scholar]
- 30.Snowling MJ, Bishop DV, Stothard SE, Chipchase B, Kaplan C. Psychosocial outcomes at 15 years of children with a preschool history of speech-language impairment. Journal of child psychology and psychiatry, and allied disciplines. 2006;47(8):759–65. doi: 10.1111/j.1469-7610.2006.01631.x. [DOI] [PubMed] [Google Scholar]
- 31.Rescorla L. The Language Development SurveyA Screening Tool for Delayed Language in Toddlers. Journal of Speech and Hearing Disorders. 1989;54(4):587–99. doi: 10.1044/jshd.5404.587. [DOI] [PubMed] [Google Scholar]
- 32.Zubrick SR, Taylor CL, Rice ML, Slegers DW. Late language emergence at 24 months: an epidemiological study of prevalence, predictors, and covariates. Journal of speech, language, and hearing research : JSLHR. 2007;50(6):1562–92. doi: 10.1044/1092-4388(2007/106). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roulstone S, Loader S, Northstone K, Beveridge M. The Speech and Language of Children Aged 25 Months: Descriptive Data from the Avon Longitudinal Study of Parents and Children. Early Child Development and Care. 2002;172(3):259–68. [Google Scholar]
- 34.Rescorla L. Late talkers: do good predictors of outcome exist? Developmental disabilities research reviews. 2011;17(2):141–50. doi: 10.1002/ddrr.1108. [DOI] [PubMed] [Google Scholar]
- 35.Fischel JE, Whitehurst GJ, Caulfield MB, DeBaryshe B. Language growth in children with expressive language delay. Pediatrics. 1989;83(2):218–27. [PubMed] [Google Scholar]
- 36.Thal DJ, Tobias S. Communicative Gestures in Children With Delayed Onset of Oral Expressive Vocabulary. Journal of Speech, Language, and Hearing Research. 1992;35(6):1281–9. doi: 10.1044/jshr.3506.1289. [DOI] [PubMed] [Google Scholar]
- 37.Thal D, Tobias S, Morrison D. Language and Gesture in Late TalkersA 1-Year Follow-up. Journal of Speech, Language, and Hearing Research. 1991;34(3):604–12. doi: 10.1044/jshr.3403.604. [DOI] [PubMed] [Google Scholar]
- 38.Everitt A, Hannaford P, Conti-Ramsden G. Markers for persistent specific expressive language delay in 3–4-year-olds. International journal of language & communication disorders/Royal College of Speech & Language Therapists. 2013;48(5):534–53. doi: 10.1111/1460-6984.12028. [DOI] [PubMed] [Google Scholar]
- 39.Rescorla L. Language and Reading Outcomes to Age 9 in Late-Talking Toddlers. Journal of Speech, Language, and Hearing Research. 2002;45(2):360–71. doi: 10.1044/1092-4388(2002/028). [DOI] [PubMed] [Google Scholar]
- 40.Pickles A, Simonoff E, Conti-Ramsden G, Falcaro M, Simkin Z, Charman T, et al. Loss of language in early development of autism and specific language impairment. Journal of child psychology and psychiatry, and allied disciplines. 2009;50(7):843–52. doi: 10.1111/j.1469-7610.2008.02032.x. [DOI] [PubMed] [Google Scholar]
- 41.Conti-Ramsden G, Durkin K. Language development and assessment in the preschool period. Neuropsychology review. 2012;22(4):384–401. doi: 10.1007/s11065-012-9208-z. [DOI] [PubMed] [Google Scholar]
- 42.Nelson HD, Nygren P, Walker M, Panoscha R. Screening for Speech and Language Delay in Preschool Children. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. [PubMed] [Google Scholar]
- 43.Fenson L, Dale PS, Reznick JS, Bates E, Thal DJ, Pethick SJ, et al. Variability in early communicative development. Monographs of the society for research in child development. 1994:i–185. [PubMed] [Google Scholar]
- 44.Robins DL, Fein D, Barton ML, Green JA. The Modified Checklist for Autism in Toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. Journal of autism and developmental disorders. 2001;31(2):131–44. doi: 10.1023/a:1010738829569. [DOI] [PubMed] [Google Scholar]
- 45.Berument SK, Rutter M, Lord C, Pickles A, Bailey A. Autism screening questionnaire: diagnostic validity. The British Journal of Psychiatry. 1999;175(5):444. doi: 10.1192/bjp.175.5.444. [DOI] [PubMed] [Google Scholar]
- 46.Sices L. Overview of expressive language delay (“late talking”) in young children. In: Post T, editor. UpToDate. Waltham, MA: 2016. [Google Scholar]
- 47.Bishop DV. What Causes Specific Language Impairment in Children? Current directions in psychological science. 2006;15(5):217–21. doi: 10.1111/j.1467-8721.2006.00439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stevenson J, Richman N. Behavior, language, and development in three-year-old children. Journal of autism and childhood schizophrenia. 1978;8(3):299–313. doi: 10.1007/BF01539633. [DOI] [PubMed] [Google Scholar]
- 49.Beitchman JH, Nair R, Clegg M, Ferguson B, Patel PG. Prevalence of psychiatric disorders in children with speech and language disorders. Journal of the American Academy of Child Psychiatry. 1986;25(4):528–35. doi: 10.1016/s0002-7138(10)60013-1. [DOI] [PubMed] [Google Scholar]
- 50.Baker L, Cantwell DP. A Prospective Psychiatric Follow-up of Children with Speech/Language Disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1987;26(4):546–53. doi: 10.1097/00004583-198707000-00015. [DOI] [PubMed] [Google Scholar]
- 51.Cohen NJ, Barwick MA, Horodezky NB, Vallance DD, Im N. Language, achievement, and cognitive processing in psychiatrically disturbed children with previously identified and unsuspected language impairments. Journal of child psychology and psychiatry, and allied disciplines. 1998;39(6):865–77. [PubMed] [Google Scholar]
- 52.Beitchman JH, Wilson B, Johnson CJ, Atkinson L, Young A, Adlaf E, et al. Fourteen-year follow-up of speech/language-impaired and control children: psychiatric outcome. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(1):75–82. doi: 10.1097/00004583-200101000-00019. [DOI] [PubMed] [Google Scholar]
- 53.Bao L, Brownlie EB, Beitchman JH. Mental health trajectories from adolescence to adulthood: Language disorder and other childhood and adolescent risk factors. Development and psychopathology. 2016;28(2):489–504. doi: 10.1017/S0954579415001054. [DOI] [PubMed] [Google Scholar]
- 54.Baker L, Cantwell DP. Attention deficit disorder and speech/language disorders. Comprehensive Mental Health Care. 1992;2(1):3–16. [Google Scholar]
- 55.Tirosh E, Cohen A. Language deficit with attention-deficit disorder: A prevalent comorbidity. Journal of Child Neurology. 1998;13(10):493–7. doi: 10.1177/088307389801301005. [DOI] [PubMed] [Google Scholar]
- 56.Durkin K, Conti-Ramsden G. Young people with specific language impairment: A review of social and emotional functioning in adolescence. Child Language Teaching and Therapy. 2010;26(2):105–21. [Google Scholar]
- 57.Ford JA, Milosky LM. Inferring Emotional Reactions in Social SituationsDifferences in Children With Language Impairment. Journal of Speech, Language, and Hearing Research. 2003;46(1):21–30. doi: 10.1044/1092-4388(2003/002). [DOI] [PubMed] [Google Scholar]
- 58.Fujiki M, Brinton B, Clarke D. Emotion Regulation in Children With Specific Language Impairment. Language, speech, and hearing services in schools. 2002;33(2):102–11. doi: 10.1044/0161-1461(2002/008). [DOI] [PubMed] [Google Scholar]
- 59.Wadman R, Durkin K, Conti-Ramsden G. Close relationships in adolescents with and without a history of specific language impairment. Language, speech, and hearing services in schools. 2011;42(1):41–51. doi: 10.1044/0161-1461(2010/10-0003). [DOI] [PubMed] [Google Scholar]
- 60.Hughes S. Bullying: what speech-language pathologists should know. Language, speech, and hearing services in schools. 2014;45(1):3–13. doi: 10.1044/2013_LSHSS-13-0013. [DOI] [PubMed] [Google Scholar]
- 61.Brownlie EB, Jabbar A, Beitchman J, Vida R, Atkinson L. Language impairment and sexual assault of girls and women: findings from a community sample. Journal of abnormal child psychology. 2007;35(4):618–26. doi: 10.1007/s10802-007-9117-4. [DOI] [PubMed] [Google Scholar]
- 62.Cohen NJ, Davine M, Horodezky N, Lipsett L, Isaacson L. Unsuspected language impairment in psychiatrically disturbed children: prevalence and language and behavioral characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32(3):595–603. doi: 10.1097/00004583-199305000-00016. [DOI] [PubMed] [Google Scholar]
- 63.Roth F, Worthington CK. Treatment resource manual for speech-language pathology. Clifton Park, NY: Cengage Learning; 2015. [Google Scholar]
- 64.Bishop DV, Edmundson A. Language-impaired 4-year-olds: distinguishing transient from persistent impairment. The Journal of speech and hearing disorders. 1987;52(2):156–73. doi: 10.1044/jshd.5202.156. [DOI] [PubMed] [Google Scholar]
- 65.Carter JaM. Karol Evaluation and treatment of speech and language disorders in children. In: Post T, editor. UpToDate. Waltham, MA: 2016. [Google Scholar]
- 66.Law J, Garrett Z, Nye C. Speech and language therapy interventions for children with primary speech and language delay or disorder. The Cochrane database of systematic reviews. 2003;(3):Cd004110. doi: 10.1002/14651858.CD004110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Law J, Garrett Z, Nye C. The efficacy of treatment for children with developmental speech and language delay/disorder: a meta-analysis. Journal of speech, language, and hearing research : JSLHR. 2004;47(4):924–43. doi: 10.1044/1092-4388(2004/069). [DOI] [PubMed] [Google Scholar]
- 68.Schlosser RW, Raghavendra P. Evidence-Based Practice in Augmentative and Alternative Communication. Augmentative and Alternative Communication. 2004;20(1):1–21. [Google Scholar]
- 69.Prelock PA, Hutchins T, Glascoe FP. Speech-Language Impairment: How to Identify the Most Common and Least Diagnosed Disability of Childhood. The Medscape Journal of Medicine. 2008;10(6):136. [Google Scholar]
- 70.Glascoe FP. Screening for developmental and behavioral problems. Ment Retard Dev Disabil Res Rev. 2005;11(3):173–9. doi: 10.1002/mrdd.20068. [DOI] [PubMed] [Google Scholar]
- 71.Marrus N, Veenstra-VanderWeele J, Hellings JA, Stigler KA, Szymanski L, King BH, et al. Training of child and adolescent psychiatry fellows in autism and intellectual disability. Autism. 2014;18(4):471–5. doi: 10.1177/1362361313477247. [DOI] [PMC free article] [PubMed] [Google Scholar]


