Abstract
Background
Nosocomial infections are a major setback in the healthcare delivery system especially in developing countries due to the limited resources. The roles played by medical care equipment and work surfaces in the transmission of such organisms have inevitably contributed to the elevated mortality, morbidity and antibiotic resistances.
Methods
A total 138 samples were collected during the study from Kawolo general hospital. Swab samples were collected from various work surfaces and fomites which consisted of; beds, sink taps, infusion stands, switches, work tables and scissors. Cultures were done and the susceptibility patterns of the isolates were determined using Kirby Bauer disc diffusion method. Data was analyzed using Stata 13 and Microsoft Excel 2013 packages.
Results
A total of 44.2% (61/138) of the collected swab specimens represented the overall bacterial contamination of the sampled articles. Staphylococcus aureus and Klebsiella pneumoniae accounted for the highest bacterial contaminants constituting of 75.4% (46/61) and 11.5% (7/61) respectively. Infusion stands and patient beds were found to have the highest bacterial contamination levels both constituting 19.67% (12/61). The highest degree of transmission of organisms to patients was found to be statistically significant for patient beds with OR: 20.1 and P-value 8X10− 4. Vancomycin, ceftriaxone and ciprofloxacin were the most effective antibiotics with 100%, 80% and 80% sensitivity patterns among the isolates respectively. Multi-drug resistant (MDR) Staphylococcus aureus accounted for 52% (24/46) with 4% (1/24) classified as a possible extensively drug resistant (XDR) whereas Gram negative isolates had 27% (4/15) MDR strains out of which 50%(2/4) were classified as possible pan-drug resistant (PDR).
Conclusion
The high prevalence of bacterial contaminants in the hospital work environment is an indicator of poor or ineffective decontamination. The study findings reiterate the necessity to formulate drug usage policies and re-examine effectiveness of decontamination and sterilization practices within Kawolo general hospital. We also recommend installation of a sound Microbiology unit at the hospital to take on susceptibility testing to check on the empirical use of antibiotics as a way of reducing the rampant elevations in drug resistances.
Keywords: Nosocomial infections, Gram-positive, Gram-negative, Antimicrobial susceptibility
Background
Nosocomial infections have become increasingly an emerging threat to the health care system over the past decades. They have highly been attributed to poor disinfection, decontamination, sterilization of hospital articles as well as weak antimicrobial stewardship policies [1]. The post-operative ward in most cases harbors patients who have undergone intrusive surgical procedures like C-sections, hip replacements and tumor among others. These procedures render them highly vulnerable to sepsis from nosocomial pathogens.
Some of the consequences of this healthcare hurdle include prolonged hospital visits, increased antimicrobial resistance, and disabilities in the affected patients which greatly reduce the quality of life and productive human resource [2, 3]. As such, it is very crucial to understand the roles played by the hospital equipment and the environment in the prolonged maintenance of nosocomial infections and transmission. Whereas the hospital environment may serve as reservoirs for these organisms, their transmission to patients is mostly through hand contact [4–6].
Bacterial species have been estimated to cause the vast majority of these nosocomial infections followed by fungi and protozoa [7]. Several previous studies have ventured into isolation of nosocomial infection-causing organisms but the most often encountered species include organisms like Staphylococcus aureus, Escherichia coli, Pseudomonas aeruginosa, Klebsiella species [4, 8–10].
Emergence of multidrug-resistant organisms has further escalated this problem especially in resource deprived nations as a result of overuse, misuse and inadequate antimicrobial stewardship policies in the health management systems. The lack of hospital antimicrobial teams and strict adherence to treatment guidelines has led to the wide usage of broad spectrum and first line antibiotics thus the exacerbation of the resistance. Implications of this resistance are prolonged hospital stays and the gross economic burden incurred in treatment with consequently high morbidity and mortality rates [11–13]. Whereas this has been a major worldwide public health threat, there is very limited information about the extent of this problem in Uganda because of limited antimicrobial resistance surveillance. Therefore, this study aimed at establishing the nosocomial bacterial contaminants often found on hospital fomites, cover items and work surfaces, and their antibiotic susceptibility patterns predisposing patients to infection in the post- operative ward at Kawolo general hospital.
Methods
Study design and sampling technique
This was a cross sectional laboratory based study was carried out from June – December, 2015 at Kawolo General Hospital where a total of 138 swab specimens were collected from medical equipment which comprised of scissors, infusion stands and patient beds, and work surfaces which were composed of tables, sink taps and light switches.
Criterion followed for sample collection comprised of simple random sampling with consideration given to areas with constant hand contact. 23 swabs were collected for each mentioned article and work surface using a sterile swab moistened in normal saline from areas approximately 10 cm in diameter using standard operating procedures. The swab samples were placed tightly in well labeled swab caps and transported back immediately to the laboratory at International Health Sciences University and cultured.
Ethics approval and consent to participate
This study was approved by the research and ethics committee of International Health Sciences University, Institute of Allied Health Sciences. Permission was also granted by the Kawolo general hospital administration and the International Health Sciences University laboratories where the experiments were performed from. All ethical laws and regulations governing scientific research were promptly adhered to during the study.
Culture and isolation procedures
Upon arrival at the laboratory, the swabs were inoculated onto Blood agar and MacConkey culture media plates and incubated for 24 h at 37 °C and inspected for bacterial growth. The obtained colonies were subjected to Gram stain, hemolysis patterns on blood agar and colonial characteristics for their identification.
Biochemical tests
Biochemical tests used in the identification and isolation of the microorganisms comprised of; catalase, coagulase, motility test, TSI, urease, indole, oxidase and Simon’s Citrate agar.
Susceptibility tests
Disc diffusion method was used to assess the antibiotic susceptibility patterns of the isolates to a panel of selected antibiotics following guidelines prescribed by Clinical and Laboratory Standards Institute (CLSI 2014). All isolates were assessed using the same inocula which were standardized to 0.5 McFarland solution turbidity. The Gram-positive isolates obtained were tested against trimethoprim sulfamethoxazole (1.25/23.5 μg), penicillin (10 IU), erythromycin (15 μg), vancomycin (30 μg), cefoxtin (30 μg) and clindamycin (2 μg). Gram-negative bacterial isolates were tested with ciprofloxacin (5 μg), gentamicin (10 μg), trimethoprim sulfamethoxazole (1.25/23.5 μg), chloramphenicol (30 μg), nalidixic acid (15 μg) and ceftriaxone (30 μg).
Staphylococcus aureus (ATCC 25923), Escherichia coli (ATCC 25922) and Pseudomonas aeruginosa (ATCC 27853) were the two standard quality control strains incorporated in the study alongside the isolates.
Results
A total of 138 swabs were collected from medical care instruments and work surfaces from the post-surgical ward at Kawolo General Hospital. Among all the items sampled, 61 (44.2%) of them presented with bacterial growth. The isolates had 46 (75.4%) Gram-positive organisms all of which were Staphylococcus aureus while 15 (24.6%) were Gram-negatives that consisted of Klebsiella pneumoniae with 7(11.5%), Proteus vulgaris, Enterobacter species and Serratia merscescans representing 5(8.2%), 2(3.3%) and 1(1.6%) respectively (Fig. 1).
Fig. 1.
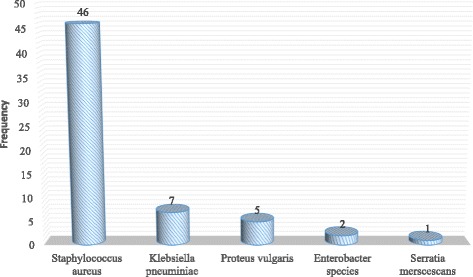
Frequency of the bacteria isolated from the swabs with bacterial growth
Bacterial distribution profile on the swabbed items
Infusion stands and patient beds were the most likely to have the highest level of bacterial contaminants both accounting for 12 swabs (19.67%) followed by tables and sinks both represented by 10 (16.39%), scissors with 9 (14.75%) and light switches with 8 (13.11%) Distribution of bacterial contaminants in each item sampled in the study was tabulated and illustrated as shown in Table 1.
Table 1.
Distribution of bacterial isolates on each respective medical item and work surface
| Isolate | Infusion stands | Patient beds | Sink taps | Tables | Scissors | Light switches | Total |
|---|---|---|---|---|---|---|---|
| Enterobacter spp | 1 | 0 | 0 | 0 | 0 | 1 | 2 |
| K. pneumoniae | 1 | 0 | 1 | 3 | 1 | 1 | 7 |
| Proteus vulgaris | 0 | 1 | 1 | 1 | 0 | 2 | 5 |
| S. merscescans | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| S. aureus | 9 | 11 | 8 | 6 | 8 | 4 | 46 |
| Total (N) | 12 | 12 | 10 | 10 | 9 | 8 | |
| Percentage | 19.67 | 19.67 | 16.39 | 16.39 | 14.75 | 13.11 |
Antibiogram profile for gram-positive isolates
Staphylococcus aureus which was the only Gram-positive bacterium isolated and was tested using an antibiotic panel consisting of: vancomycin, clindamycin, trimethoprim sulfamethoxazole, cefoxtin, erythromycin and penicillin G. The data for the susceptibility testing of Staphylococcus aureus is shown in fig. 2. Using cefoxtin as a surrogate marker, 24(52%) of Staphylococcus aureus isolates were defined as MRSA as they were resistant to Cefoxtin from which 1 isolate (4%) was defined as a possible XDR as per the guidelines provided by the CLSI 2014.
Fig. 2.
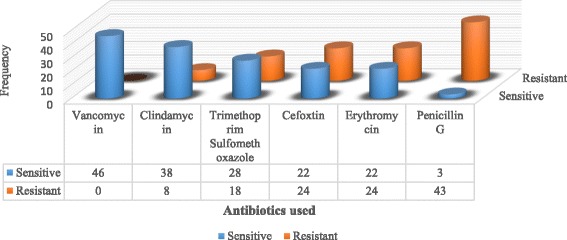
Gram-positive antimicrobial susceptibility pattern
Antibiogram profile for gram-negative isolates
Klebsiella pneumoniae 7(47%), Proteus vulgaris 5(33%), Enterobacter species 2(13%) and Serratia merscescans 1(7%) were the isolates obtained in the constituting a total of 15 isolates. These were tested against a panel of antibiotics consisting of: ciprofloxacin, ceftriaxone, gentamycin, trimethoprim sulfamethoxazole, nalidixic acid and chloramphenicol. The data for the susceptibility testing of Gram negative isolates is shown in Fig. 3. The CLSI 2014 guidelines were used to further group the Gram-negative isolates according to their resistance degrees and the study revealed that 4(27%) out of the 15 isolates were classified as MDR. Out of the 4 MDR, Klebsiella pneumoniae had 1(25%) MDR and 2(50%) being further classified as possible PDR while Proteus vulgaris accounted for the remaining 1(25%) of the MDR strains. (Table 2).
Fig. 3.
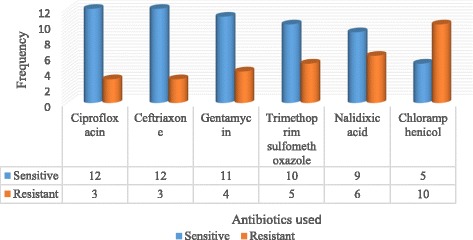
Gram-negative isolate antimicrobial susceptibility pattern
Table 2.
Classification of Gram-negative isolates according to their degree of resistance
| Isolate | Frequency | Resistance degree |
|---|---|---|
| Klebsiella pneumoniae | 2 | PDR |
| Klebsiella pneumoniae | 1 | MDR |
| Proteus vulgaris | 1 | MDR |
Discussion
The overall prevalence of bacterial contamination in the post-operative surgical ward revealed by our study was 44% (61/138) which was considerably high and capable of giving rise to nosocomial infections. Such contamination is suggestive of a variety of factors which may include; poor decontamination, poor sanitation practices, ineffective disinfectants used and ineffective sterilization of medical care articles. Different prevalences have been reported in Uganda and elsewhere in similar studies. Jinja and Mulago hospitals in Uganda reported 58.5% and 68.8% respectively [9, 10] probably because the conditions in all these health facilities are somewhat similar. Elsewhere in Nigeria, a prevalence of 47% was reported [14] whereas 85.8% was reported from a research done at Jimma university teaching hospital in Ethiopia [15]. Beyond Africa, a research performed in Taiwan reflected a prevalence of 63.5% [16] and 57% from a study carried out in 7 hospitals in Iran [6]. The data from this study indicates the articles contaminated with bacteria have an increased risk as a source for nosocomial transmission of HAIs.
Staphylococcus aureus with 75.4% (46/61) was the most prevalent bacterial contaminant isolated by our study. These results coincide with those from other studies where Staphylococcus aureus had the highest prevalence of 30.2% in a study done in Nigeria [4] and 28.4% in Cameroon [1]. Staphylococcus aureus is naturally occurring as a normal flora on human mucosa. The presence of surface proteins present in their cell walls for biofilm, evasion of host immune responses and tissue adhering abilities has enabled these organisms to survive and flourish in nature [17].
Klebsiella pneumoniae 11.5% (7/15), was the most predominant Gram-negative we isolated in our study. Isolation of such enterobacteria is highly suggestive of fecal contamination, poor personal hygiene and most especial poor hand washing practices amongst health workers and patients. The high prevalence of this organism is attributed to the presence of pili encoded by mrkD gene in Klebsiella pneumoniae that aid in adherence of the organism to host tissues during invasion and biofilm bacterial forms are 10 times more resistant to antibiotics than the uncapsulated forms [18].
Patient beds and infusion stands had the highest bacterial contamination levels of 19% (12/61) compared to the other surfaces and equipment swabbed. This is because these are some of the articles most frequently in contact with hands during patient care in any hospital setting as most authors have reported those medical workers’ hands are the most probable means of transfer [19]. In order to assess the effectiveness of the decontamination protocols used in the hospital, the research team consulted the hospital administration and found out that ordinary liquid soap and sodium hypochlorite were used for cleaning the hospital twice a day utmost which was basically done for the hospital floors. On top of that, the sterilizer for ensuring sterility of medical equipment before use was not regularly serviced. Other articles like infusion stands, work tables and beds were seldom decontaminated and yet they were found to harbor infectious organisms. There were also tales of cleaning agents occasionally running out of stock. We deduced that the persistence of the bacteria in the hospital environment could be attributed to the ineffective strength of disinfecting agents and limited frequency of decontamination. The beds are responsible for accommodating a vast number of the patients that are admitted within the post-operative ward and yet rarely or no sterilization is done to ensure their decontamination. This renders them highly exposed and most likely responsible for harboring such organisms that can later result into nosocomial infections.
Antimicrobial resistance poses one of the greatest threats to the survival of mankind. Indeed, the antimicrobial resistance review (2015) highlighted an associated global mortality of closely 700,000 deaths per annum with a projection of approximately 10 million deaths by 2050. As for the current study, vancomycin was the most effective antibiotic against Staphylococcal infections as demonstrated by our study. As such, it empirically recommended in treatment of suspected MRSA cases; however, reports of increasing vancomycin-resistant Staphylococcus aureus have been on the rise over the years. Increased resistance levels were observed for penicillin, cefoxtin and erythromycin with 93%, 48% and 48% resistances respectively. This could be attributed to the increasing overuse and misuse of antibiotics by the general population as a result of a weak health management system since they are readily available over the counter even without clinicians’ prescriptions. These same reasons can be used to explain the high frequency of MRSA that represented 52% (24/46) out of which 4% (1/24) was described as a possible XDR.
Ciprofloxacin, ceftriaxone and gentamycin with 80%, 80% and 73% sensitivities respectively were the most effective antibiotics as per our study. On the contrary, chloramphenicol and nalidixic acid with 67% and 40% resistances respectively had the least sensitivities. Increasing resistances are reflective of ready availability and prescription abuse. MDR enterobacteria accounted for 27% (4/15) out of which Klebsiella pneumoniae had 1(25%) possible PDR resistant to all the antibiotics in the drug profile. Our study findings on MDR organisms therefore coincide with many similar studies [1, 20] and call for immediate intervention to slow down this public health threat.
Among our shortcomings, our study had a small sample size which gave a small reflection about the magnitude of the challenge and we therefore recommend a nationwide similar study to get a bigger picture of this problem. Also antimicrobial susceptibility patterns were determined using phenotypic disc diffusion methods; however, we recommend whole genome sequencing for deciphering the resistome of these bacteria.
Conclusion
Our study, being the first of its kind to be done at Kawolo general hospital found out that Staphylococcus aureus and Klebsiella pneumoniae were the most predominant isolates most likely to cause HAIs. Hospital fomites have been found to harbor disease-causing microbes and are easily transmitted through hand contact from one person to another. Mutations and other various factors have aided these organisms to mount resistance towards commonly used antibiotics which has rendered treatment of infectious diseases inefficient.
There is indeed a dire need to scale up and strengthen the existing infection control strategies at Kawolo hospital, and the entire country through reassessment of the strengths and types of the decontaminants used to clean hospitals, frequency of decontamination or sterilization, good personal hygiene, and establishment of a national surveillance program to monitor and control HAIs.
Acknowledgements
We would like to recognize in a special way the financial contribution and support offered by Norah Kibuuka, Shah Mugaseth, Mawanda Allan, Bahati Akim, Komakech Christopher, Nakamwadda Brenda, and Lutaya James Kiganda.
Funding
This research was supported in part by Norah Kibuuka, Shah Mugaseth, Mawanda Allan, Bahati Akim, Komakech Christopher, and Nakamwadda Brenda.
Availability of data and materials
The dataset supporting the findings of this article is available from the corresponding author upon request.
Abbreviations
- %
Percent
- °C
Degree Celsius
- ATCC
American Type Culture Collection
- CLSI
Clinical Laboratory Standards Institute
- cm
Centimeter
- HAI
Hospital Acquired Infection
- MDR
Multi Drug Resistant
- MRSA
Methicillin Resistant Staphylococcus aureus
- OR
Odds Ratio
- PDR
Pan Drug Resistant
- TSI
Triple Sugar Iron
- XDR
Extensive Drug Resistance
Authors’ contributions
IS conceptualized the study. IS was responsible for data acquisition, analysis and interpretation. AW was involved in sample collection and performed microbiological identification of isolates. BM, GM, FS and ML performed and interpreted the drug sensitivity tests and analyzed the data. All authors critically reviewed and approved the final manuscript.
Ethics approval and consent to participate
Ethical approval for the study was attained from the research and ethics committee of International Health Sciences University, Institute of Allied Health Sciences, Kampala, Uganda. Prior to sample collection, written approval was also granted by the Kawolo General Hospital administration, Buikwe and the International Health Sciences University, microbiology laboratory where this work was carried out.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ivan Sserwadda, Phone: +256702208225, Email: ivangunz23@gmail.com.
Mathew Lukenge, Email: lukenmat@gmail.com.
Bashir Mwambi, Email: mwambibashir@yahoo.com.
Gerald Mboowa, Email: gmboowa@gmail.com.
Apollo Walusimbi, Email: apollowalusimbi@gmail.com.
Farouk Segujja, Email: frquen8@gmail.com.
References
- 1.Kihla AJ, Ngunde PJ, Mbianda SE, Nkwelang G, Ndip RN. Risk Factors for wound infection in health care facilities in Buea, Cameroon: aerobic bacterial pathogens and antibiogram of isolates. Pan African Medical Journal. 2014;18(1) [DOI] [PMC free article] [PubMed]
- 2.Jalalpour S. Effective sources of food borne illness in Iranian hospitalized patients: review article. Advances in environmental. Biology. 2013;7(11):3560–3567. [Google Scholar]
- 3.Bazira J, Boum Y, II, Sempa J, Iramiot J, Nanjebe D, Sewankambo N, Nakanjako D. Trends in antimicrobial resistance of Staphylococcus Aureus isolated from clinical samples at Mbarara regional referral Hospital in Rural Uganda. British Microbiology Research Journal. 2014;4(10):1084. doi: 10.9734/BMRJ/2014/9751. [DOI] [Google Scholar]
- 4.Muhammad UK, Isa MA, Aliyu ZM. Distribution of potential nosocomial pathogens isolated from environments of four selected hospital in Sokoto, north western Nigeria. Journal of Microbiology and Biotechnology Research. 2013;3(1):139–143. [Google Scholar]
- 5.Misgana GM, Abdissa K, Bacterial AG. Contamination of mobile phones of health care workers at Jimma University specialized hospital, Jimma, south West Ethiopia. International Journal of Infection Control. 2015 Mar 11;11(1)
- 6.Ekrami A, Kayedani A, Jahangir M, Isolation KE. Of common aerobic bacterial pathogens from the environment of seven hospitals, Ahvaz, Iran. Jundishapur Journal of Microbiology. 2011;4(2):75–82. [Google Scholar]
- 7.Bereket W, Hemalatha K, Getenet B, Wondwossen T, Solomon A, Zeynudin A, Kannan S. Update on bacterial nosocomial infections. Eur Rev Med Pharmacol Sci. 2012;16(8):1039–1044. [PubMed] [Google Scholar]
- 8.Saito Y, Kobayashi H, Uetera Y, Yasuhara H, Kajiura T, Okubo T. Microbial contamination of surgical instruments used for laparotomy. Am J Infect Control. 2014;42(1):43–47. doi: 10.1016/j.ajic.2013.06.022. [DOI] [PubMed] [Google Scholar]
- 9.Anguzu JR, Drug OD. Sensitivity patterns of bacterial isolates from septic post-operative wounds in a regional referral hospital in Uganda. Afr Health Sci. 2007;7(3) [DOI] [PMC free article] [PubMed]
- 10.Seni J, Najjuka CF, Kateete DP, Makobore P, Joloba ML, Kajumbula H, Kapesa A, Bwanga F. Antimicrobial resistance in hospitalized surgical patients: a silently emerging public health concern in Uganda. BMC research notes. 2013;6(1):298. doi: 10.1186/1756-0500-6-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mulu W, Kibru G, Beyene G, Damtie M. Postoperative nosocomial infections and antimicrobial resistance pattern of bacteria isolates among patients admitted at Felege Hiwot referral hospital, Bahirdar, Ethiopia. Ethiopian journal of health sciences. 2012;22(1):7–18. [PMC free article] [PubMed] [Google Scholar]
- 12.Messele G, Woldemedhin Y, Demissie M, Mamo K, Common GA. Causes of nosocomial infections and their susceptibility patterns in two hospitals in Addis Ababa. Ethiop J health. Biomed Sci. 2009;2(1):3–8. [Google Scholar]
- 13.Kamat US, Ferreira AM, Savio R, Motghare DD. Antimicrobial resistance among nosocomial isolates in a teaching hospital in Goa. Indian J Community Med. 2008;33(2):89. doi: 10.4103/0970-0218.40875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ochie K, Ohagwu CC. Contamination of X-ray equipment and accessories with nosocomial bacteria and the effectiveness of common disinfecting agents. African Journal of basic and applied sciences. 2009;1(1–2):31–35. [Google Scholar]
- 15.Shiferaw T, Beyene G, Kassa T, Sewunet T. Bacterial contamination, bacterial profile and antimicrobial susceptibility pattern of isolates from stethoscopes at Jimma University specialized hospital. Ann Clin Microbiol Antimicrob. 2013;12(1):39. doi: 10.1186/1476-0711-12-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen KH, Chen LR, Wang YK. Contamination of medical charts: an important source of potential infection in hospitals. PLoS One. 2014;9(2):e78512. doi: 10.1371/journal.pone.0078512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foster TJ, Geoghegan JA, Ganesh VK, Höök M. Adhesion, invasion and evasion: the many functions of the surface proteins of Staphylococcus Aureus. Nat Rev Microbiol 2014 Jan 1;12(1):49–62. [DOI] [PMC free article] [PubMed]
- 18.Bellifa S, Hassaine H, Balestrino D, Charbonnel N, Mrsquo I, Terki IK, Lachachi M, Didi W, Forestier C. Evaluation of biofilm formation of Klebsiella Pneumoniae isolated from medical devices at the University Hospital of Tlemcen, Algeria. Afr J Microbiol Res. 2013;7(49):5558–5564. doi: 10.5897/AJMR12.2331. [DOI] [Google Scholar]
- 19.Weber DJ, Anderson D, Rutala WA. The role of the surface environment in healthcare-associated infections. Curr Opin Infect Dis. 2013;26(4):338–344. doi: 10.1097/QCO.0b013e3283630f04. [DOI] [PubMed] [Google Scholar]
- 20.Abdallah EM, Ahamed F, Al-Omari AS. Antibiotic susceptibility patterns of some clinical isolates from al-Rass general hospital. International Journal of Biosciences. 2015;6(9):47–54. doi: 10.12692/ijb/6.9.47-54. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the findings of this article is available from the corresponding author upon request.


