Abstract
Fasted or weight-category athletes manage their training under strict diet conditions that could impair the stress-recovery balance and result in acute or chronic fatigue. However, to date, no validated biomarker are available to quantify this phenomena. The aim of this study was to assess the validity of a specific index combining plasma albumin and weight change to detect nutrition-related risks of fatigue increase and under-performance in athletes experiencing particular nutritional conditions.
An athlete's nutrition risk index (ANRI) equation, based on data from lightweight and heavyweight rowers, was developed using relationship between plasma albumin concentrations combined to weight changes with sport performance and overtraining scores and was tested by odds ratio for failure. The accuracy and sensitivity of this former specific equation was subsequently tested on runners observing the Ramadan-fasting as well as on boxers after a short weight-loss period.
Independently of training and performance, lightweight rowers presented lower nutritional parameters than heavyweight (albumin: 37.4 ± 2.7 vs 39.9 ± 1.8 g·L−1, P < 0.05; weight state: 94.5 ± 1.8 vs 99.9 ± 0.9%, P < 0.01). In lightweight, ANRI was related with overtraining score (R2 = 0.21, P < 0.01), risks for failure in competition were enhanced when ANRI increased (OR:2.5, P = 0.03). Relationship of ANRI with overtraining score tended to be also significant in runners (R2 = 0.32, P = 0.06) but not in boxers (P = 0.4).
Albumin concentrations combined to weight loss appeared relevant to delineate nutrition-related risks of fatigue and/or competitive failure associated with mid-term diets (about 30 days) as observed in rowers and Ramadan-fasted runners. ANRI may benefit to athletes monitoring by delineating effects of their weight loss program.
Keywords: Albumin, Weight loss, Physical conditioning
Highlights
-
•
Albumin or weight loss, alone, are not related with fatigue scores.
-
•
A combination of albumin and weight loss can highlight nutritional risk of fatigue.
-
•
A specific and valuable athlete's nutrition risk index can be built.
-
•
Risks for failure in competition increase when ANRI increases in rowers and runners.
1. Introduction
The nutrition status can be considered as the regulation of a homeostatic process which allowing to keep the body at a constant state with respect to physiological functions and with optimal energy stores. However, there are several situations characterized by an impairment of this equilibrium (i.e. linked to a decrease in nutrients intake or a high increase of nutrient expenditure) which usually lead to malnutrition. That is classically observed in patients with protein energy malnutrition (like elderly people) or in intensive care unit patients [1]. For these patients, some indexes were developed to set protein energy malnutrition diagnosis and to assess nutritional status [2]. These markers are well validated and extensively used in clinical practice for their reliability to predict patients' outcome. Although largely underestimated, athletes' population, because of its high daily energy expenditure, may be also at risk of malnutrition [3]. Hence, despite the benefic effects of regular exercise on health, marked increases of physical training may be associated with physiological systems alterations (i.e.: muscular damages; metabolic pathways impairments; dysimmunity) [4], [5], [6]. Although nutrition plays an important role in the recovery of the exercise-induced physiological stress, trained individuals frequently present imbalance between caloric intake and expenditure [7]. Finally, over their competitive period, athletes competing in weight classes have to combine reduced diet with strenuous training that could result in energy homeostasis imbalance increasing their risks for underperformance and alterations of the immune systems [8], [9], [10].
It could be obviously assumed that tool classically used in malnourished patients are not appropriate to discriminate a possible impairment of nutritional status in athletes [2], [11]. The nutritional risk index (NRI) has been reported to accurately determine nutrition-related risks in hospitalized young and aged patients, and to describe nutritional status in healthy subjects [12], [13], [14], [15]. However, to our knowledge, there is no tool to evaluate the nutritional status of athletes [2], [16]. This lack of specific tools for the monitoring of athletes nutritional status should be related to the specific situations associated with this particular population [17]: i) high variability of training and competition context, ii) variability of diet duration and type, iii) difficulty to determine parameters as outcomes of nutritional status, iv) difficulty to collect and analyze biological parameters in the sport competitive context, and v) inadequacy of the body mass index, which is usually > to 25 or 30 in strength conditioned athletes.
The aim of this study was to develop a new index called athlete's NRI (ANRI: developed from NRI) to detect nutrition-related risks of failure in athletes experiencing particular nutritional conditions.
2. Materials and methods
An ANRI equation, based on data from lightweight rowers, was developed using relationship between plasma albumin concentrations combined with weight changes and overtraining scores, and was tested by odds ratio for failure. The accuracy and sensitivity of this former specific equation was therefore tested on two confirmation groups: runners observing the Ramadan-fasting and boxers after a weight loss period. In the three groups, blood samples, weight and overtraining questionnaires were collected in similar conditions at the beginning of the diet (weight) and onset of the sport event (rowers and boxers) or end of the Ramadan fast (runners; blood samples, weight, overtraining questionnaires). Results of NRI and ANRI were also compared to absolute and relative performance indicators.
2.1. Subjects
Men rowers competing at the similar sport level were recruited for the study, they competed as lightweight rowers (LW; n = 23; 23.6 ± 0.8 years old) having to achieve a weight limit or as heavyweight rowers (HW; n = 22; 24.2 ± 1.1 years old) without weight limit. LW were observed after a weight loss diet period of 33.4 ± 4.3 days preceding a national level multi-races competition (three races for each subjects). All the rowers competed in similar boats (coxless pairs) providing methodological advantages: i) reduced delays between races and unique classification scale; ii) limit for the average weight was 70 kg for the crew (72.5 max individually) increasing weight losses when compared to single scull or ergometer races; iii) coxless pairs described individual performance compared to other crew boats.
Groups of Ramadan-fasted runners and boxers were also recruited to test the equation developed based on LW rowers. Eight middle-distance runners participated in the study (25.0 ± 1.3 years old), they were trained for 8.2 ± 0.6 h per week during the study. Runners observed the Ramadan-fasting, abstaining from food and liquids from approximately 05.00 to 19.00 h for 30 days [18]. Eight elite boxers composed the third group (21.4 ± 1.4 years old) and were trained for 7.4 ± 1.6 h during the study. Boxers observed a 10 days pre-competitive weight loss diet to achieve individual weight limit. After explaining the risks and benefits of the study, subjects gave their written informed consent to participate in the study which was carried out according to the ethical guidelines of the University of Paris Descartes-Cochin (Paris, France).
2.2. Nutritional risk index and nutritional status
The NRI was calculated as previously described using albumin serum concentrations and weight state:
| NRI = [1.519 × albumin (g·L−1)] + [0.417 (weight state)] [13]. |
In line with previous studies on NRI [12], [13], [14] we set actual weight/usual weight = 1 when actual weight exceeded usual weight.
Based on previous studies, 4 grades of nutrition-related risk have been defined: 1-major risk (NRI < 82), 2-moderate risk (NRI: 82 to 92), 3-low risk (NRI: 92 to 97.5), and 4-no risk (NRI>: 97.5) [14].
The specific ANRI equation was calculated using the relationship between rowers plasma albumin concentrations combined with weight changes and overtraining scores:
| ANRI = [−0.7915 × albumin (g·L−1)] − [1.2810 (weight state)] + 169.85. |
Weight state was calculated using comparison of the weight at the competition onset (rowers and boxers) or fast end (runners) with usual weight recorded at the beginning of the diet [weight state = (actual weight/usual weight × 100)]. In the morning and fasted state, body weight was measured using a floor scale (Mettler–Toledo floor scale, France). Body mass index (BMI) was calculated from the ratio of weight (in kg) by height squared (in meters), the individual height being declared by subjects.
2.3. Overtraining and performance
Overtraining score, absolute performance and performance classes were used as outcomes of the athletes' nutritional status.
The risk of overtraining was assessed using the valid and reliable questionnaire of the French Society for Sports Medicine that was composed of a list of 54 items selected among the reported clinical manifestations of the syndrome that requires an answered response of ‘‘yes” or ‘‘no” by the athletes [19]. The positive items determined a score (called overtraining score) used to classify athletes, a score higher than 20 suggesting possibly-overtrained athletes [19], [20].
In rowers, the mean velocity achieved during the third and last race (2000-m long) of the competition was accounted as the absolute performance and was expressed relatively to the best international performance in coxless pair for LW and HW rowers to allow weight categories comparisons.
Two hours before the first race, rowers were asked to declare which final competition ranking will be considered as success and which one will be considered failure according to their own training and to adversary. Comparison between the actual final ranking and the declared success/failure rankings determined two performance classes: success or failure.
In runners, before and after the Ramadan-fasting, subjects performed an incremental exercise to exhaustion on a standard athletic track (400 m) for determining their maximal aerobic velocity (MAV), by using the University of Montreal Track Test [21]. MAV and its changes with fasting period were respectively assumed as absolute and relative performance indicators.
In boxers, total scoring points performed in a single-elimination boxing tournament were recorded as absolute performance.
2.4. Blood sampling and analyses
Blood samples were collected with subjects at rest and in post-absorptive condition (last meal at least 2.5 h before blood collection).
In rowers, blood samples were collected 1–2 h before their first race, to respect their comfort in these conditions, capillary blood samples of ∼50 μL drawn at the fingertip inducing the use of a specific method to analyze plasma albumin concentrations. Plasma albumin concentrations were determined by Fourier-transform infrared (FT-IR) spectrometry according to the methods previously described [22], [23] and using the analysis compartment of a Tensor-27 spectrometer equipped with a HTS-XT autosampler (Bruker, Germany). A 2 cm−1 spectral resolution was used for 32 co-added scans in transmission mode for triplicate measurements and averaged.
In runners and boxers, venous blood (20 mL) was sampled from an antecubital vein. From this sampling, 10 mL of blood was sampled on EDTA anticoagulant for plasma. After clotting, the samples were stored at −20 °C for subsequent determinations. Albumin concentrations were measured using commercial colorimetric methods (Biomerieux, Boehringer Mannheim, France). All samples were analyzed in triplicate.
2.5. Statistics
Results of LW and HW rowers were compared using non parametric Mann–Whitney test for quantitative variables and chi-square tests for qualitative variables. Relationships between different diet outcomes and between anthropometrical data were assessed by linear regression (Kendall rank correlation) and were calculated for rowers, runners and boxers. We assessed if NRI or ANRI were independently associated with overtraining score value, performance parameters and success-failure results by multiple linear regression and multiple logistic regression when appropriate (NRI and ANRI were independent variables and the three outcomes were dependent variables). Quantitative variables are expressed as mean ± standard deviation and qualitative variables as number and percentage. R software (version 3.0.2, R Foundation for Statistical Computing, Vienna, Austria) was used for the analysis. All tests were two-sided and level significance was set at P < 0.05.
3. Results
Weight and anthropometric results, nutritional parameters and overtraining scores were presented in Table 1. Bodyweight and weight state differed between LW and HW rowers (both case, P < 0.0001). Runners and boxers also lost weight over the diet period (both case, P < 0.001).
Table 1.
Nutritional results and overtraining scores for lightweight rowers group (LW, n = 23), heavyweight rowers (HW, n = 22), Ramadan fasted runners (n = 8) and boxers with competitive weight limits (n = 8).
| LW rowers | HW rowers | Runners | Boxers | |
|---|---|---|---|---|
| Weight (kg) | 69.1 ± 1.6 | 79.8 ± 6.9a | 63.9 ± 6.8 | 68.4 ± 10.4 |
| Weight state (%) | 94.5 ± 1.8 | 99.9 ± 0.9a | 97.0 ± 1.8 | 95.4 ± 1.9 |
| Body mass index (kg·m−2) | 22.0 ± 0.9 | 23.2 ± 1.6 | 20.7 ± 0.9 | 22.2 ± 2.2 |
| Albumin (g·L−1) | 37.4 ± 2.8 | 39.9 ± 1.8a | 44.8 ± 3.7 | 48.8 ± 3.7 |
| Nutritional risk index | 96.2 ± 4.2 | 102.2 ± 2.9a | 108.7 ± 5.2 | 116.0 ± 5.7 |
| Athletes nutritional risk index | 19.1 ± 2.8 | 10.09 ± 2.2a | 9.96 ± 2.3 | 6.65 ± 4.1 |
| Overtraining score | 19.1 ± 4.4 | 18.5 ± 3.3 | 16.3 ± 4.6 | 12.1 ± 5.2 |
Significant differences between LW and HW.
LW rowers presented lower albumin plasma concentrations than HW (P = 0.001), with concentrations appearing below the normal ranges (37–46 g·L−1) in 10 LW rowers. 2 runners and 5 boxers presented serum albumin concentrations above the normal range.
No difference was observed between LW and HW rowers for performance classes (P = 0.7; success or failure). Relative velocity slightly differed according to category (94.3 ± 2.6% in LW rowers vs 93.0 ± 1.8 in HW, P = 0.07). MAV in runners decreased over the Ramadan fast (20.7 ± 0.4 km·h−1 before Ramadan onset vs 19.9 ± 0.4 at Ramadan end, P = 0.004).
Similar overtraining scores were observed between LW and HW rowers (P = 0.6) with seven LW and five HW rowers overreaching 20 positive responses (limit for suspected overtraining state), 2 runners and 2 boxers overreached the total of 20 positive responses. Total recorded points in boxers event was 113.6 ± 39.4.
LW subjects presented significantly lower NRI than HW, with NRI results describing a LW group with “low risk” when HW rowers were without any risk. Among the LW group, five rowers were placed in the “moderate risk” category.
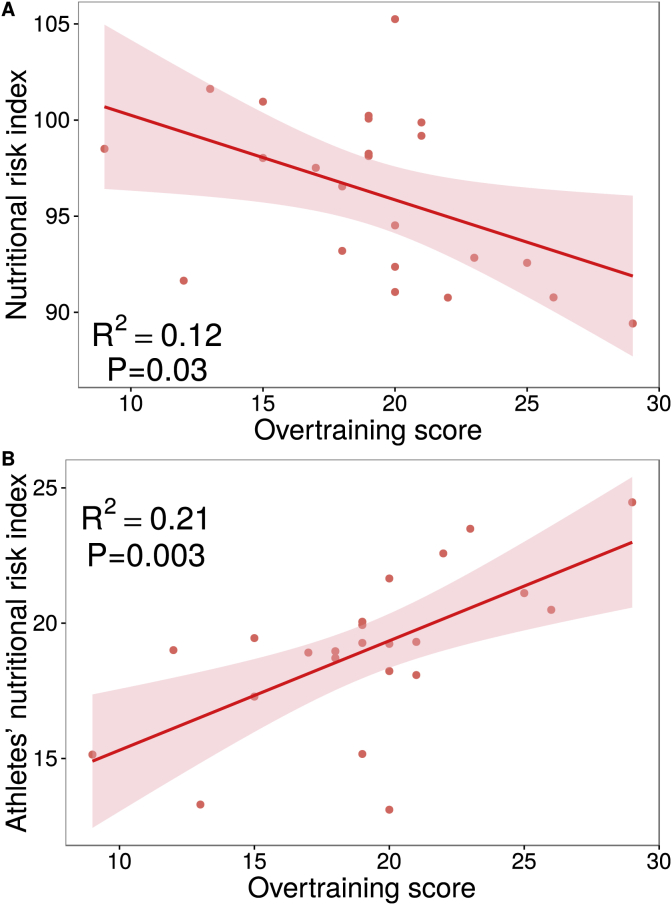
In LW, NRI was correlated with overtraining score, even adjusted on diet duration (both case, P = 0.03). Multiple linear regression analysis reported that ANRI were not related with relative velocity in LW (P of overall F statistic = 0.2) and in HW (P of overall F statistic = 0.6), nor with overtraining score in HW (P of overall F statistic = 0.6) but correlation was found with overtraining score in LW (even when adjusted for diet duration, P = 0.003; Fig. 1).
Fig. 1.
Relationships of nutritional risk index (A) and athletes' nutritional risk index (B) with overtraining scores in lightweight rowers.
Risks for rowers failure in competition were lowered when NRI increased and, because ANRI calculations were based on overtraining score, the risk of failure was increased when ANRI increased (Table 2).
Table 2.
Rowers groups odds ratio for failure in rowing competition. Heavyweight (HW) n = 22 and lightweight (LW) n = 23.
| HW |
LW |
|||||
|---|---|---|---|---|---|---|
| Crude OR (CI 95%) | P | Crude OR (CI 95%) | P | |||
| Nutritional risk index | 0.90 | (0.64–1.27) | 0.5 | 0.72 | (0.52–0.99) | 0.04 |
| Athletes' nutritional risk index | 3.20 | (0.21–49.5) | 0.4 | 2.53 | (1.09–5.89) | 0.03 |
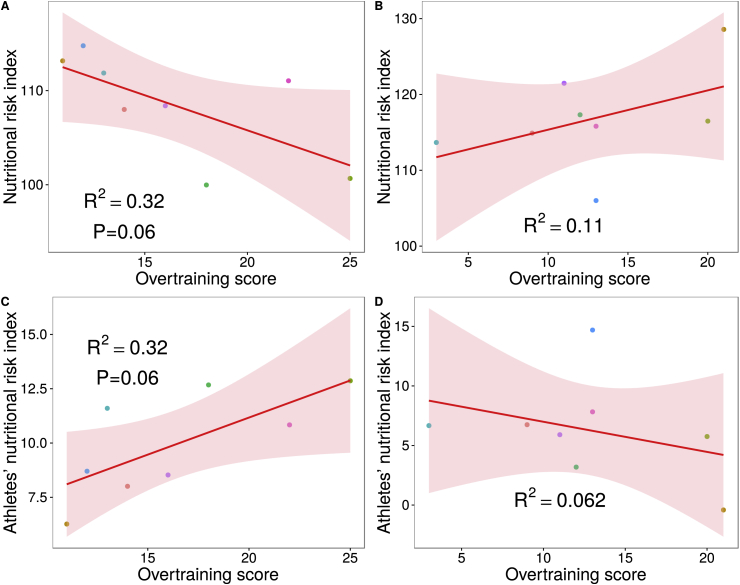
In runners, overtraining scores appeared almost statistically related with NRI and ANRI (P = 0.06) (Fig. 2A and C). In boxers, no relationship was observed for NRI and ANRI (Fig. 2B and D) with overtraining scores. NRI and ANRI were not related with performance parameters (P of overall F statistic > 0.1).
Fig. 2.
Relationships of nutritional risk index and athletes' nutritional risk index with overtraining scores in Ramadan fasted runners (A, C) and in boxers (B, D).
When observed independently, no relationships between albumin concentrations, weight, BMI and weight state with overtraining score and performance parameters was found significant in rowers, runners and boxers (P of overall F statistic > 0.1).
4. Discussion
It is largely recognized that evaluation of nutritional status is of major importance as predictive marker for patient's outcome. For this purpose, some indicators were developed (like NRI) and assessed for general population. However, it appears that the general tool is not necessarily appropriate to a given sub-population. This is in line with the nutritional recommendations which are specific for each population (i.e. elderly, babies, pregnant women, athletes etc.). In this way, it was developed the Geriatric NRI (called GNRI) devoted to elderly population [15], it seems logical to propose a specific nutritional marker for athletes. The present study is the first to describe relationships of combined anthropometrical and biochemical parameters with risks of fatigue and/or failure in LW rowers and Ramadan fasted runners. Utilization of NRI for athletes competing in weight categories singularly differed from that of surgical or elderly populations with the major risk being the overtraining state associated to physiological and psychological troubles [24], [25].
When applying NRI equation and previously published grades of nutrition-related risks in rowers, 22% were described with moderate risks, 39% with low risks and the remainder without risks. Conversely, runners and boxers could be considered without risks. ANRI specific calculations based on LW rowers provided more accurate fit of actual overtraining scores and odds ratio appeared significant for ANRI to detect risk of failure. Relationship was also observed between ANRI and overtraining scores in runners but not in boxers. The ANRI equation described lower variability in predictions and error of estimates when applying this latter specific index. These results, associated with the large differences between the populations used to conceive the original NRI and ANRI, supported the use of an athlete's specific index.
Some differences between rowers, runners and boxers may be of importance to understand the relevance. One of the constituting parameter of ANRI was the weight loss which has been previously reported to have reduced effects on performance when lower than 5% of previous body weight, but assumed to markedly lower fitness and performance when higher than 10% (8–9). In our study, weight state described changes higher than 5% in rowers (54% of the total group), boxers (37.5% of the total group) but not in runners (only 12.5%). None of our subjects achieved the critical value of 10% body weight loss. In some rapid weight loss strategies, main part of the loss could originate from water loss [8], [26]. Such strategies were not likely to occur in a diet lasting 30-day as observed in rowers and runners but could have been used in boxers [27], [28]. Short term diet of boxers may involve water loss with dehydration inducing the higher albumin concentrations measured. This result suggested that according to possible dehydration in dieted athletes, plasma volume change should therefore be controlled. Based on clinical practice, we could assume that albumin concentrations below 35 g·L−1 suggested moderate denutrition and below 30 g·L−1 a severe denutrition [29], [30]. Albumin concentrations appeared lower in LW rowers than in HW and in the normal range in runners and boxers. Lower albumin concentrations in LW rowers could be due to the repeated exercises of the training program associated with reduced food intakes. According to serum albumin half-life (20 days), the 33 days of LW rowers' diet may be sufficient to reduce albumin concentrations as it was observed in 26% of the group with concentrations below 35 g·L−1. Mid-term duration was also observed in Ramadan fast without resulting in low albumin concentrations. This could be due to the design of the Ramadan which is an intermittent fasting period without searching for weight loss. However, it is well known that albumin may be influenced by many factors (i.e. inflammation, exercise, etc) and confirm that this marker used alone is not suitable for athletes to detect protein-energy malnutrition. However, in inflamed patients, decrease in plasma albumin is rather linked to extravasations due to vessel dilation [31] than to a decrease of synthesis [32] and this factor could be excluded in athletes.
Consequently, when considered separately albumin or weight state were not related with overtraining scores underlining the high combined influence of albumin concentrations and weight state to delineate the rowers and runners nutritional status. Similarly to previous studies, no relationship appeared between nutritional parameters (NRI, ANRI, albumin and weight state) and sport performance suggesting that the diet influence on sport performances remain difficult to measure [24], [28], [29].
5. Conclusions
Therefore, the present study highlights a new valuable way to monitor athletes' nutritional status according to risks endured when competing under-pressure of body weight or social norms. Albumin concentrations combined to weight loss appears relevant to delineate nutrition-related risks of fatigue and/or competitive failure when diets were conducted in mid to long term periods. We assumed that ANRI may benefit to athletes monitoring by delineating the effects of their weight loss program. Obviously, further studies remain required to test our ANRI equation in larger populations.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
None of the authors had any financial or personal relations with people or organizations that could have inappropriately influenced their work. The corresponding author states that he had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Acknowledgements
Authors thank the rowers, runners and boxers who participated to the study.
References
- 1.McClave S.A., Mitoraj T.E., Thielmeier K.A., Greenburg R.A. Differentiating subtypes (hypoalbuminemic vs marasmic) of protein-calorie malnutrition: incidence and clinical significance in a university hospital setting. J. Parenter. Enter. Nutr. 1992;16:337–342. doi: 10.1177/0148607192016004337. [DOI] [PubMed] [Google Scholar]
- 2.Kondrup J., Allison S.P., Elia M., Vellas B., Plauth M. Educational and clinical practice committee, European society of parenteral and Enteral nutrition (ESPEN), ESPEN guidelines for nutrition screening 2002. Clin. Nutr. Edinb. Scotl. 2003;22:415–421. doi: 10.1016/s0261-5614(03)00098-0. [DOI] [PubMed] [Google Scholar]
- 3.Booth F.W., Roberts C.K. Linking performance and chronic disease risk: indices of physical performance are surrogates for health. Br. J. Sports Med. 2008;42:950–952. doi: 10.1136/bjsm.2008.052589. [DOI] [PubMed] [Google Scholar]
- 4.Venkatraman J.T., Pendergast D.R. Effect of dietary intake on immune function in athletes. Sports Med. Auckl. N. Z. 2002;32:323–337. doi: 10.2165/00007256-200232050-00004. [DOI] [PubMed] [Google Scholar]
- 5.Petibois C., Cazorla G., Poortmans J.-R., Déléris G. Biochemical aspects of overtraining in endurance sports: the metabolism alteration process syndrome. Sports Med. Auckl. N. Z. 2003;33:83–94. doi: 10.2165/00007256-200333020-00001. [DOI] [PubMed] [Google Scholar]
- 6.Cheung K., Hume P., Maxwell L. Delayed onset muscle soreness: treatment strategies and performance factors. Sports Med. Auckl. N. Z. 2003;33:145–164. doi: 10.2165/00007256-200333020-00005. [DOI] [PubMed] [Google Scholar]
- 7.Thompson J.L., Manore M.M., Skinner J.S., Ravussin E., Spraul M. Daily energy expenditure in male endurance athletes with differing energy intakes. Med. Sci. Sports Exerc. 1995;27:347–354. [PubMed] [Google Scholar]
- 8.Fogelholm M. Effects of bodyweight reduction on sports performance. Sports Med. Auckl. N. Z. 1994;18:249–267. doi: 10.2165/00007256-199418040-00004. [DOI] [PubMed] [Google Scholar]
- 9.Brownell K.D., Steen S.N., Wilmore J.H. Weight regulation practices in athletes: analysis of metabolic and health effects. Med. Sci. Sports Exerc. 1987;19:546–556. [PubMed] [Google Scholar]
- 10.Degoutte F., Jouanel P., Bègue R.J., Colombier M., Lac G., Pequignot J.M. Food restriction, performance, biochemical, psychological, and endocrine changes in judo athletes. Int. J. Sports Med. 2006;27:9–18. doi: 10.1055/s-2005-837505. [DOI] [PubMed] [Google Scholar]
- 11.Hasselmann M., Alix E. Tools and procedures for screening for malnutrition and its associated in risks in hospital. Nutr. Clin. Metab. 2003;17:218–226. [Google Scholar]
- 12.Buzby G.P., Knox L.S., Crosby L.O., Eisenberg J.M., Haakenson C.M., McNeal G.E. Study protocol: a randomized clinical trial of total parenteral nutrition in malnourished surgical patients. Am. J. Clin. Nutr. 1988;47:366–381. doi: 10.1093/ajcn/47.2.366. [DOI] [PubMed] [Google Scholar]
- 13.Buzby G.P., Williford W.O., Peterson O.L., Crosby L.O., Page C.P., Reinhardt G.F. A randomized clinical trial of total parenteral nutrition in malnourished surgical patients: the rationale and impact of previous clinical trials and pilot study on protocol design. Am. J. Clin. Nutr. 1988;47:357–365. doi: 10.1093/ajcn/47.2.357. [DOI] [PubMed] [Google Scholar]
- 14.Naber T.H., de Bree A., Schermer T.R., Bakkeren J., Bär B., de Wild G. Specificity of indexes of malnutrition when applied to apparently healthy people: the effect of age. Am. J. Clin. Nutr. 1997;65:1721–1725. doi: 10.1093/ajcn/65.6.1721. [DOI] [PubMed] [Google Scholar]
- 15.Bouillanne O., Morineau G., Dupont C., Coulombel I., Vincent J.-P., Nicolis I. Geriatric nutritional risk index: a new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 2005;82:777–783. doi: 10.1093/ajcn/82.4.777. [DOI] [PubMed] [Google Scholar]
- 16.Loucks A.B. Energy balance and body composition in sports and exercise. J. Sports Sci. 2004;22:1–14. doi: 10.1080/0264041031000140518. [DOI] [PubMed] [Google Scholar]
- 17.Khodaee M., Olewinski L., Shadgan B., Kiningham R.R. Rapid weight loss in sports with weight classes. Curr. Sports Med. Rep. 2015;14:435–441. doi: 10.1249/JSR.0000000000000206. [DOI] [PubMed] [Google Scholar]
- 18.Chennaoui M., Desgorces F., Drogou C., Boudjemaa B., Tomaszewski A., Depiesse F. Effects of Ramadan fasting on physical performance and metabolic, hormonal, and inflammatory parameters in middle-distance runners. Appl. Physiol. Nutr. Metab. Physiol. 2009;34:587–594. doi: 10.1139/H09-014. [DOI] [PubMed] [Google Scholar]
- 19.Brun J.-F. The overtraining: to a system of evaluation usable by routine examination. Sci. Sports. 2003;18:282–286. [Google Scholar]
- 20.Varlet-Marie E., Maso F., Lac G., Brun J.-F. Hemorheological disturbances in the overtraining syndrome. Clin. Hemorheol. Microcirc. 2004;30:211–218. [PubMed] [Google Scholar]
- 21.Léger L., Boucher R. An indirect continuous running multistage field test: the Université de Montréal track test. Can. J. Appl. Sport Sci. 1980;5:77–84. [PubMed] [Google Scholar]
- 22.Petibois C., Cazorla G., Cassaigne A., Déléris G. Plasma protein contents determined by Fourier-transform infrared spectrometry. Clin. Chem. 2001;47:730–738. [PubMed] [Google Scholar]
- 23.Petibois C., Melin A.M., Perromat A., Cazorla G., Déléris G. Glucose and lactate concentration determination on single microsamples by Fourier-transform infrared spectroscopy. J. Lab. Clin. Med. 2000;135:210–215. doi: 10.1067/mlc.2000.104460. [DOI] [PubMed] [Google Scholar]
- 24.Eichner E.R. Overtraining: consequences and prevention. J. Sports Sci. 1995;13 Spec No:S41–S48. doi: 10.1080/02640419508732276. [DOI] [PubMed] [Google Scholar]
- 25.Koral J., Dosseville F. Combination of gradual and rapid weight loss: effects on physical performance and psychological state of elite judo athletes. J. Sports Sci. 2009;27:115–120. doi: 10.1080/02640410802413214. [DOI] [PubMed] [Google Scholar]
- 26.Artioli G.G., Gualano B., Franchini E., Scagliusi F.B., Takesian M., Fuchs M. Prevalence, magnitude, and methods of rapid weight loss among judo competitors. Med. Sci. Sports Exerc. 2010;42:436–442. doi: 10.1249/MSS.0b013e3181ba8055. [DOI] [PubMed] [Google Scholar]
- 27.Hall C.J., Lane A.M. Effects of rapid weight loss on mood and performance among amateur boxers. Br. J. Sports Med. 2001;35:390–395. doi: 10.1136/bjsm.35.6.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morton J.P., Robertson C., Sutton L., MacLaren D.P.M. Making the weight: a case study from professional boxing. Int. J. Sport Nutr. Exerc. Metab. 2010;20:80–85. doi: 10.1123/ijsnem.20.1.80. [DOI] [PubMed] [Google Scholar]
- 29.Ballmer P.E. Causes and mechanisms of hypoalbuminaemia. Clin. Nutr. Edinb. Scotl. 2001;20:271–273. doi: 10.1054/clnu.2001.0439. [DOI] [PubMed] [Google Scholar]
- 30.Walberg J.L., Leidy M.K., Sturgill D.J., Hinkle D.E., Ritchey S.J., Sebolt D.R. Macronutrient content of a hypoenergy diet affects nitrogen retention and muscle function in weight lifters. Int. J. Sports Med. 1988;9:261–266. doi: 10.1055/s-2007-1025018. [DOI] [PubMed] [Google Scholar]
- 31.Ruot B., Papet I., Bechereau F., Denis P., Buffiere C., Gimonet J. Increased albumin plasma efflux contributes to hypoalbuminemia only during early phase of sepsis in rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2003;284:R707–R713. doi: 10.1152/ajpregu.00483.2002. [DOI] [PubMed] [Google Scholar]
- 32.Mansoor O., Bazin J.E., Beaufrère B., Schoeffler P. Catabolic aspects of cranial trauma. Ann. Fr. 1998;17:180–185. doi: 10.1016/s0750-7658(98)80072-5. [DOI] [PubMed] [Google Scholar]