Abstract
Luteolin, a flavone, has been demonstrated to have anti-cancer properties. In the current study, the effects of luteolin on certain carcinogenesis-associated changes induced by pancreatitis, which are significant risk factors for pancreatic cancer, were investigated. Male six-week-old C57BL6 mice used in the current study were divided into three groups; the control group, acute pancreatitis group and luteolin group. Intra-peritoneal injection of cearulein was performed in the acute pancreatitis group and luteolin group to induce acute pancreatitis whereas the luteolin group received intra-peritoneal injection of luteolin. The control group received intra-peritoneal injection of normal saline. Then, the expression of SOX9, phosphorylated (p-) STAT3, p-EGFR, cytokeratin-19, Ki67 and N-cadherin were determined by immunohistochemistry. Morphological changes of acinar cells were determined by hematoxylin and eosin staining. The mRNA expression of the epithelial-mesenchymal transition markers CDH1, CDH2, Slug, Zeb1, EpCAM, ZO1, Vimentin, Snail and Twist was determined by reverse transcription-quantitative polymerase chain reaction. It was identified that luteolin inhibits the formation of tubular complexes and ectopic expression of cytokeratin-19 and luteolin also decreased proteins of SOX9, p-STAT3 and p-EGFR. In addition, luteolin inhibits proliferation and epithelial-mesenchymal transition of acinar cells induced by acute pancreatitis. As tubular complex formation and ectopic expression of cytokeratin-19 were two prominent characters of acinar-ductal metaplasia, it was concluded that luteolin inhibits acinar-ductal metaplasia induced by pancreatitis and also inhibits pancreatitis-induced proliferation and epithelial-mesenchymal transition of acinar cells. Acinar-ductal metaplasia and proliferation have close associations with pancreatic carcinogenesis. It is suggested that luteolin has potential anti-pancreatic carcinogenesis effects and merits further investigation.
Keywords: luteolin, SOX9, acinar-ductal metaplasia, epithelial-mesenchymal transition, pancreatic carcinogenesis
Introduction
Pancreatic ductal adenocarcinoma (PDAC), is a type of cancer with one of the highest rates of mortality (1). Pancreatitis, which is a significant risk factor of PDAC (2), has been identified to effectively induce initiation of PDAC in mice with K-ras oncogene (3). Acinar-ductal metaplasia (ADM) is a phenomenon that appears during pancreatitis and is characterized by the replacement of normal acinus with a ductal-like structure, which contains metaplastic acinar cells that express ductal markers, such as cytokeratin 19 (CK19) (4). Pancreatitis-induced ADM is a reversible process in normal adult mice where metaplastic acinar cells are replaced by normal acinar cells following diminishing of inflammation. However, with mutant K-ras oncogenes, acinar regeneration is blocked and metaplastic acini are driven to form pancreatic intraepithelial neoplasia (PanIN) (4), which is the most common precursor of PDAC (5). Therefore, ADM has been demonstrated to be an essential step in pancreatitis-induced, K-ras-dependent carcinogenesis of pancreatic cancer (4,6).
SRY-box 9 (SOX9) is a human motility group-box transcription factor that has been observed to regulate pancreatic exocrine and endocrine development (7). In the exocrine part of normal adult pancreas, SOX9 is expressed only in centroacinar cells and ductal cells (4). However, SOX9 is also expressed in acinar cells during pancreatitis (8). Previous studies identified that SOX9 serves a critical role in pancreatitis-induced ADM and pancreatic carcinogenesis (8–10). However, the regulation of SOX9 expression remains unclear, and further research is required in order for SOX9 to become a therapeutic target of PDAC.
In addition to the SOX9 gene, numerous other proteins and pathways were activated or upregulated during pancreatitis, and certain pathways have been demonstrated to be essential for ADM formation and pancreatic carcinogenesis. The ductal transcription factor hepatocyte nuclear factor 6 has been demonstrated to serve an important role in ADM (9). Human and mouse pancreatic lesions express abundant epidermal growth factor receptor (EGFR) and EGFR is required for ADM formation, Kras-induced PanIN formation and pancreatic carcinogenesis (11,12). Also, the downward pathways of EGFR, such as mitogen-activated protein kinase signaling and phosphatidyl inositol 3-kinase signaling, are required for PanIN formation and pancreatic carcinogenesis (13,14). Signal transducer and activator of transcription 3 (STAT3) signaling is also significantly upregulated during pancreatitis and the phosphorylation of STAT3 has been indicated to be essential for the proliferation of metaplastic acinar cells and initiation of PDAC (15–17). Other pathways including Notch signaling, canonical Wnt signaling and the Hedgehog pathway have been observed to promote ADM and pancreatic carcinogenesis (6,18,19).
Epithelial-mesenchymal transition (EMT) is a biological process in which epithelial cells transform into special cells with mesenchymal phenotypes. EMT has a close association with the metastasis of pancreatic cancer. Certain mesenchymal markers, such as zinc finger E-box binding homeobox 1 (Zeb1) and fibroblast-specific protein 1, serve as independent predictors of mortality in patients with pancreatic cancer (20,21). It has been confirmed that Kras-dependent PanIN formation and pancreatic carcinogenesis were accompanied with EMT of acinar cells, and EMT promotes dissemination of acinar cells under malignant transformation (22).
Flavonoids are the effective constituents of many herbs used in traditional Chinese medicine and have produced preventive and therapeutic effects against certain diseases (23). As a flavone widely present in various foodstuffs, plants and herbs, luteolin has been identified as one of the most potent flavonoids (24). Luteolin has been identified to exhibit numerous biological activities and therapeutic effects, including anti-inflammatory and pro-apoptotic effects, and the ability to reverse anti-neoplastic drug resistance (25–27). In a previous study, it was demonstrated that luteolin inhibits auto-phosphorylation of STAT3 and EMT of pancreatic cancer cell in vitro (28). The current study determined if luteolin inhibits certain carcinogenesis-associated pathways and proteins that were upregulated during pancreatitis. In addition, the effects of luteolin on ADM and certain other pathological changes that were essential for pancreatic carcinogenesis or metastasis were examined.
Materials and methods
Induction of acute pancreatitis and mouse treatment
Experiments were approved by the Animal Experimental Ethical Inspection of Laboratory Animal Centre, Wenzhou Medical University, Wenzhou, China (permit no. wydw2015-0128). A total of 45 male C57/BL6 mice were supplied by Laboratory Animal Centre of Wenzhou Medical University, housed in specific pathogen-free condition with constant temperature of 24°C and 12-h light/dark cycle. The mice had free access to food and water until 24 h before experiments. When mice were 6 weeks old and about 25 g, acute pancreatitis was induced by 2 sets of 6 hourly intra-peritoneal injections of cearulein (50 µg/kg; Sigma-Aldrich; Merck Millipore, Darmstadt, Germany) on alternating days. Luteolin (Chengdu Must Bio-Technology, Chengdu, China) was dissolved by DMSO at a concentration of 40 mg/ml, and then diluted by normal saline to 0.05 mg/ml. Mice were intra-peritoneally injected with luteolin daily at a dosage of 2 mg/kg. The first injection of luteolin was performed immediately subsequent to the completion of cearulein injections on the first day. The last injection of luteolin was performed on the day prior to sacrifice. The next day after finishing induction of pancreatitis was defined as day 1. Mice were sacrificed on days 1, 3 and 5 in the 9 different groups (day 1-CTRL, day 1-AP and day 1-AP+Luteolin, and so on for days 3 and 5). Each group comprised 5 mice.
Hematoxylin and eosin (H&E) staining and immunohistochemistry
Pancreas tissues were fixed overnight in 4% paraformaldehyde (Sigma-Aldrich; Merck Millipore), embedded in paraffin, cut into 4-µm-thick sections, and placed on slides. Sections were subjected to H&E and immunohistochemical staining as previously described (19,29). For H&E staining, sections were stained with hematoxylin for 4 min and with eosin for 1.5 min. For immunohistochemistry, 3–3′-diaminobenzidine tetrahydrochloride was used as a chromogen. Primary antibodies were diluted according to the instructions and were incubated overnight at 4°C (Table I). Bright-field images were acquired using a DM4000B microscope (Leica Microsystems GmbH, Wetzlar, Germany).
Table I.
Antibodies used.
| Antibody | Supplier | Catalog number | Dilution |
|---|---|---|---|
| SOX9 | Cell Signaling Technology, Inc. (Danvers, MA, USA) | 82630 | 1:400 |
| p-STAT3 | Abcam (Cambridge, UK) | Ab76315 | 1:200 |
| p-EGFR (Tyr1068) | Cell Signaling Technology, Inc. | 3777 | 1:100 |
| CK19 | Abcam | Ab52625 | 1:500 |
| Ki67 | Abcam | Ab16667 | 1:100 |
| N-cadherin | Abcam | Ab98952 | 1:1,000 |
SOX9, SRY-box 9; p-, phosphorylated; STAT3, signal transducer and activator of transcription 3; EGFR, epithelial growth factor receptor; CK19, cytokeratin 19.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Pancreas tissue was preserved in liquid nitrogen. Total RNA was extracted by tissue dissociation in TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA) according to the manufacturer's protocol. cDNA was synthesized using 1 µg of total RNA in a 20 µl final volume by reverse transcription with RevertAid RT Reverse Transcription kit (Thermo Fisher Scientific, Inc., Waltham, MA, USA). qPCR was performed with 0.3 µl of cDNA, 1.5 µl forward and reverse primers (2 µM), 1.7 µl double distilled water, and 5 µl SYBR Green Mix (Applied Biosystems; Thermo Fisher Scientific, Inc.). Expression levels were normalized using a custom primer set for GAPDH. cDNA was amplified using ABI Prism 7500 Sequence Detection System (Applied Biosystems; Thermo Fisher Scientific, Inc.). Primer sequences are listed in Table II. The thermocycling conditions were: Stage 1: 95°C, 5 min; Stage 2: 95°C, 30 sec, 60°C, 1 min, 40 cycles; melt curve: 95°C, 5 min; and, cooling at 1.6°C/sec to 60°C.
Table II.
Primers used.
| Gene | Forward (5′-3′) | Reverse (5′-3′) |
|---|---|---|
| Snail | GAGCTGCAGGACGCGTGTGT | TTGAGGACCTCGGGCGGAGG |
| Slug | TCGTCGGCAGCTCCACTCCA | CGGGGGACTTACACGCCCCA |
| Twist | AGACCCAGCGGGTCATGGCT | CTTGTCCGAGGGCAGCGTGG |
| Zeb1 | CGGTGCCAAGAACTGCTGGCA | CGGCGGTGTCTTGTTGCTGC |
| Vimentin | AATCCAAGTTTGCTGACCTCTCTGA | ACTGCACCTGTCTCCGGTACTC |
| CDH1 | AGCCCCTGCTGCCACCAGAT | CATCCAGGCCCCTGTGCAGC |
| EpCAM | GCAGGTCCAGTGTGGTACTC | GGAAGCGCTAACCCTCCTAC |
| CDH2 | GCGGGATAAAGAGCG | GGAGTCATACGGTGGC |
| ZO1 | CCACAAGCGCAGCCACAAGCTA | GCTGGGGTTGTTTCAGGCGAA |
| GAPDH | AATGGGGTGAGGCCGGTGCT | CACCCTTCAAGTGGGCCCCG |
Statistical analysis
Comparisons among multiple groups were made with a one-way analysis of variance followed by least significant difference or Dunnett's t-test. P<0.05 was considered to indicate a statistically significant difference. Results are represented as the mean ± standard error. All data presented represent at least 3 mice and represent at least three 4-µM sections unless otherwise noted.
Results
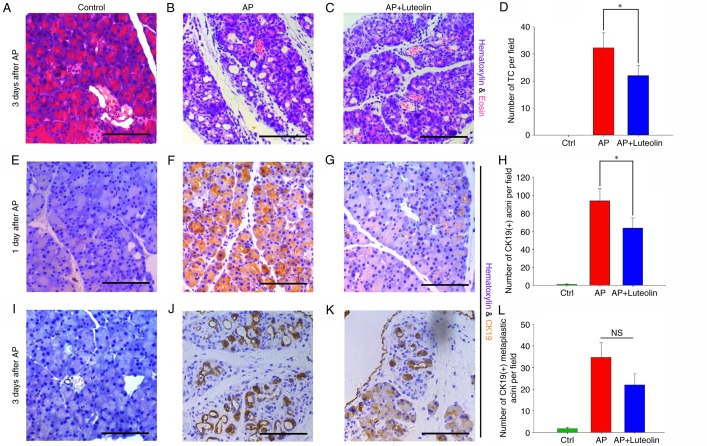
Luteolin inhibits pancreatitis-induced ADM formation
H&E staining was performed and an immunohistochemistry assay was conducted to determine whether luteolin has effects on ADM formation induced by acute pancreatitis. By H&E staining, it was identified that ADM was most evident on day 3, compared with days and day 5. A prominent change of ADM induced by acute pancreatitis was the formation of tubular complexes, which was characterized by circular arrangement of acinar cells that resembled ducts, and the tubular complexes of each field were counted (magnification, ×200) (30,31). The H&E staining slides exhibited no tubular complex in the control group (Fig. 1A), and 3 days subsequent to acute pancreatitis, this number increased to 32.27±5.58 (Fig. 1B). However, with the treatment with luteolin, 22±3.79 tubular complexes were observed per field (P<0.05) (Fig. 1C and D). This indicates that acute pancreatitis-induced the formation of tubular complexes, which was then significantly inhibited by luteolin.
Figure 1.
Luteolin inhibits pancreatitis-induced ADM formation. Hematoxylin and eosin staining of the pancreas in the (A) Ctrl, (B) AP and (C) luteolin groups on day 3. (D) Number of TC per field (magnification, ×200) in the Ctrl, AP and luteolin groups. Immunohistochemistry of CK19 in the (E) Ctrl, (F) AP and (G) luteolin groups on day 1. (H) Number of CK19(+) acini per field (×200) in the Ctrl, AP and luteolin groups on day 1. Immunohistochemistry of CK19 in the (I) Ctrl, (J) AP and (K) luteolin groups on day 3. (L) Number of CK19(+) acini per field (×200) in the Ctrl, AP and luteolin groups on day 3. *P<0.05. Scale bars, 100 µm. ADM, acinar-ductal metaplasia; Ctrl, control; AP, acute pancreatitis group; AP + luteolin, luteolin group; TC, tubular complex; NS, not significant.
To confirm luteolin's effects on ADM further, an immunohistochemistry assay was performed in order to detect ectopic expression of CK19 in acinar cells. CK19-positive acini were then counted to determine the extent of ADM. As the immunohistochemistry assay indicated, unlike tubular complexes which were clearer on day 3, CK19-positive acini rapidly appeared on day 1 and could last up to day 5. The number of CK19-positive acini were counted on days 1 and 3 to assess whether luteolin has effects on ADM. It was identified that on day 1, the number of CK19-positive acini increased from 1.13±0.45 to 93.67±13.54 per field with the injection of cearulein (P<0.05) (Fig. 1E and F), and this number decreased to 63.47±11.48 with the treatment of luteolin (P<0.05) (Fig. 1G and H). A total of 3 days subsequent to the induction of acute pancreatitis, mice which were not treated with luteolin had 34.73±6.69 CK19-positive acini per field (Fig. 1J). In mice treated with luteolin, this number decreased to 22.07±5.04 however this was not significant (P=0.072) (Fig. 1K and L). The results of H&E staining and immunohistochemistry assay both indicated that luteolin inhibits ADM induced by acute pancreatitis.
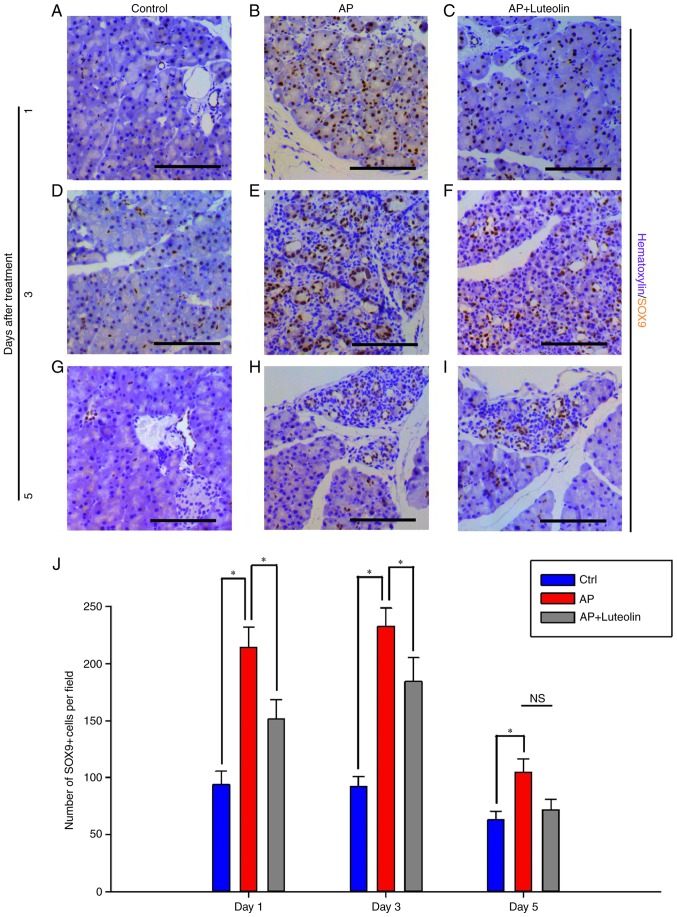
Pancreatitis-induced expression of SOX9 in acinar cells is inhibited by luteolin
Numerous kinds of transcriptional factors, such as SOX9 and HNF6, have been confirmed to be essential for ADM formation (9). In order to investigate how luteolin inhibits pancreatitis-induced ADM formation, immunohistochemistry was conducted to determine the effects of luteolin on SOX9 expression (Fig. 2). SOX9 was expressed in ductal cells and centroacinar cells alone in the normal pancreas tissues, while it was induced in acinar cells following acute pancreatitis. SOX9-positive cells increased significantly one day subsequent to pancreatitis (Fig. 2A and B). On day 1, for the control group, 93.67±11.83 of pancreatic cells per field were detected to exhibit expression of SOX9. However, for mice with acute pancreatitis, this number increased to 213.9 ±17.98 per field (P<0.05). Furthermore, when treated with luteolin, this number decreased to 151.4±16.99 (P<0.05) (Fig. 2C and J). Acute pancreatitis-induced ectopic SOX9 expression lasted up to day 3. On day 3, for mice injected with cearulein and treated with luteolin, SOX9-positive cells decreased significantly from 232.45±16.02 to 184.07±21.22 per field (P<0.05) (Fig. 2D-F and J). Luteolin also caused the decrease of SOX9-positive cells on day 5, however not significantly (P=0.112; Fig. 2G-I and J), and this is suggested to be due to the fact that ectopic SOX9 expression was almost decreased to normal levels. With the results of immunohistochemistry assay, it was concluded that luteolin inhibits acute pancreatitis-induced SOX9 expression in acinar cells, and as SOX9 is essential for ADM formation, luteolin's effects of inhibiting ADM may partly depend on the inhibition of SOX9 expression.
Figure 2.
Pancreatitis-induced expression of SOX9 in acinar cells is inhibited by luteolin. Immunohistochemistry for SOX9 in the (A) Ctrl, (B) AP and (C) luteolin groups 1 day after AP. Immunohistochemistry for SOX9 in the (D) Ctrl, (E) AP and (F) luteolin groups 3 days after AP. Immunohistochemistry for SOX9 in the (G) Ctrl, (H) AP and (I) luteolin groups 5 days after AP. (J) Number of SOX9(+) cells per field (×200) in the Ctrl, AP and luteolin groups; *P<0.05; scale bars, 100 µm. SOX9, SRY-box 9; Ctrl, control; AP, acute pancreatitis group; AP + luteolin, luteolin group; NS, not significant.
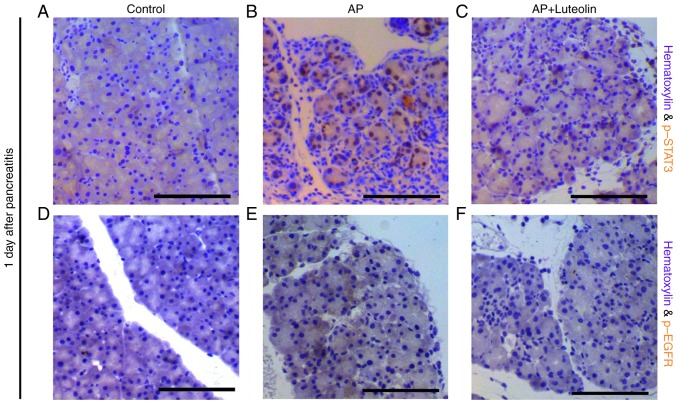
Luteolin inhibits STAT3 and EGFR signaling pathways
A number of signaling pathways have been confirmed to be essential for ADM and pancreatic carcinogenesis, including the interleukin (IL)-STAT3 pathway, EGFR-ras pathway and canonical Wnt pathway (11–13,15–18). An immunohistochemistry assay was conducted to determine the effects of luteolin on these pathways. Consistent with previous studies (15,16), p-STAT3 positive acinar cells were not observed in the exocrine part of the pancreas in the control group, however is widely observed in mice with pancreatitis on day 1 (Fig. 3A and B). However, with the treatment of luteolin, p-STAT3-positive cells decreased significantly during pancreatitis (Fig. 3C). It was also identified that pancreatitis significantly induced phosphorylation of EGFR in acinar cells (Fig. 3D and E) and with the treatment of luteolin, phosphorylation of EGFR was decreased significantly on day 1 (Fig. 3F). Therefore, not only the STAT3 pathway, however additionally the EGFR pathway were inhibited by luteolin during pancreatitis. The expression of β-catenin was determined following the treatment of luteolin. However, it seems that luteolin has no significant effect on the expression and membrane-translocation of β-catenin (data not shown). As STAT3 and EGFR signaling pathways serve a role in ADM, and the inhibition of them may contribute to luteolin's effects of inhibiting ADM formation.
Figure 3.
Luteolin inhibits STAT3 and EGFR signaling pathways. Immunohistochemistry for p-STAT3 in the (A) control, (B) AP and (C) luteolin groups 1 day after AP. Immunohistochemistry for p-EGFR in the (D) control, (E) AP and (F) luteolin groups 1 day after AP. Scale bars, 100 µm. STAT3, signal transducer and activator of transcription 3; EGFR, epithelial growth factor receptor; p-, phosphorylated; AP, acute pancreatitis group; AP + luteolin, luteolin group.
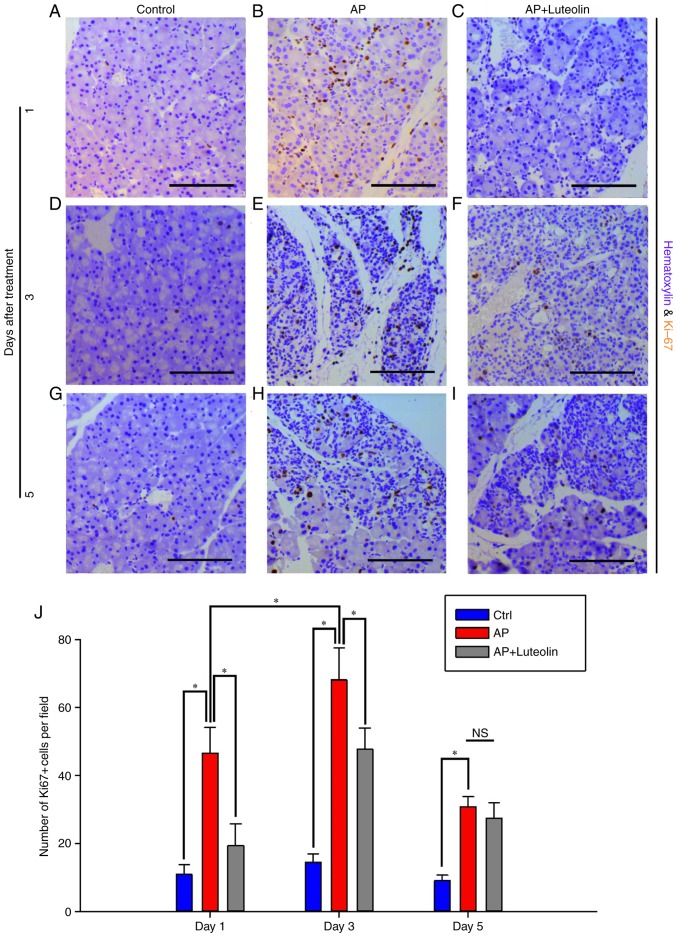
Luteolin inhibits acute pancreatitis-induced proliferation of acinar cells
It has been reported that pancreatitis-induced ADM and pancreatic carcinogenesis were accompanied with persistent proliferation of pancreatic cells (17). Cell cycle activation marker Ki67 was used to determine proliferative level of acinar cells. Few acinar cells were identified to be Ki67-positive on the control group (Fig. 4A). And frequency of Ki67-positive cells increased to 46.62±7.45 per field one day after the induction of pancreatitis (Fig. 4B). However, with the treatment of luteolin, Ki67-positive cells decreased to 19.4±6.45 per field (P<0.05; Fig. 4C). On day 3, mice on the acute pancreatitis group had 68±9.54 Ki67-positive cells per field (Fig. 4D and E). Whilst with the treatment of luteolin, this number decreased to 47.67±6.32 (P<0.05; Fig. 4F). On day 5, the number of Ki67-positive cells per field decreased from 30.8±3 to 27.43±4.52 with the treatment of luteolin (Fig. 4G-I), however it was not significant (Fig. 4J). Therefore, it was concluded that pancreatitis-induced proliferation of exocrine cells was inhibited by luteolin.
Figure 4.
Luteolin inhibits acute pancreatitis-induced proliferation of acinar cells. Immunohistochemistry for Ki67 in the (A) Ctrl, (B) AP and (C) luteolin groups 1 day after AP. Immunohistochemistry for Ki67 in the (D) Ctrl, (E) AP and (F) luteolin groups 3 days after AP. Immunohistochemistry for Ki67 in the (G) Ctrl, (H) AP and (I) luteolin groups 5 days after AP. (J) Number of Ki67(+) cells per field (×200) in the Ctrl, AP group and luteolin groups. *P<0.05, scale bars, 100 µm. Ctrl, control; AP, acute pancreatitis group; AP + luteolin, luteolin group; NS, not significant.
Transient EMT occurs on acinar cells during pancreatitis and luteolin inhibits EMT of acinar cells
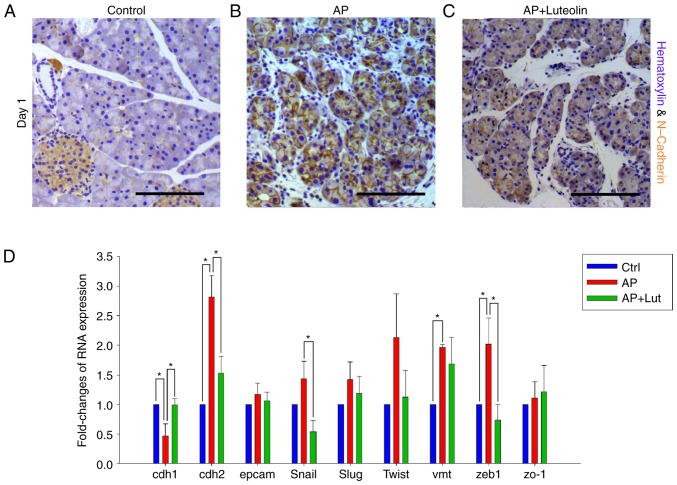
Pancreatic carcinogenesis was accompanied by EMT of acinar cells, which significantly promoted dissemination of acinar cells under malignant transition (22). Thus, it was investigated whether acute pancreatitis promotes EMT of acinar cells and if luteolin has effects on it. CDH2, which was an adhesion molecule in the membrane and a marker of mesenchyma, was chosen to indicate EMT change of acinar cells during pancreatitis. By immunohistochemistry, it was observed that CDH2 was highly expressed in islets and marginally expressed in acinar cells of normal pancreas (Fig. 5A). However, during pancreatitis, expression of CDH2 increased significantly in acinar cells on day 1 (Fig. 5B). Subsequently, the expression of CDH2 on mice treated with luteolin was established. The results indicated that pancreatitis-induced expression of CDH2 was effectively inhibited by luteolin (Fig. 5C).
Figure 5.
Transient EMT occurs on acinar cells during pancreatitis and luteolin inhibits EMT of acinar cells. (A-C) Immunohistochemistry for N-Cadherin in control group (A), acute pancreatitis group (B) and luteolin group (C) 1 day after pancreatitis. (D) Fold change in mRNA expression of CDH1, CDH2, Slug, Zeb1, EpCAM, ZO1, VMT, Snail, and Twist of pancreatic tissue. GAPDH was used as an internal control. *P<0.05; scale bars, 100 µm. EMT, epithelial-mesenchymal transition; CDH1, E-cadherin; CDH2, N-cadherin; Slug, snail family transcriptional repressor 2; Zeb1, zinc finger E-box binding homeobox 1; EpCAM, epithelial cell adhesion molecule; ZO1, zonula occludens 1; VMT, vimentin; Snail, snail family transcriptional repressor 1; Twist, twist family BHLH transcription factor 1; AP, acute pancreatitis group; AP + luteolin, luteolin group; NS, not significant.
RT-qPCR was conducted to further confirm the results. Certain EMT markers, including CDH1, CDH2, EpCAM, Snail, Slug, Twist, Vimentin, Zeb1 and ZO-1, were selected to indicate EMT change of acinar cells. As compared with the control group, the results of PCR indicated that CDH1, CDH2, Vimentin and Zeb1 changed significantly 1 day after acute pancreatitis (Fig. 5D). Changes of the four markers all indicated EMT changes to acinar cells. No marker was identified to change significantly against EMT (Fig. 5D) and compared with the acute pancreatitis group, CDH1, CDH2, Snail and Zeb1 changed significantly with the treatment of luteolin (Fig. 5D). Changes of the four markers all indicated that the EMT changes of acinar cells were reversed. No marker suggested that luteolin would promote EMT (Fig. 5D). Therefore, with the results of the immunohistochemistry assay and RT-qPCR, it was confirmed that acute pancreatitis promoted EMT of acinar cells, and this was reversed by luteolin.
Discussion
A number of pathways and proteins have been demonstrated to serve different roles in pancreatic carcinogenesis. Certain pathways and proteins are also essential for ADM formation, for example EGFR-ras pathway, IL6-STAT3 pathway, and SOX9 protein (8,11,17). These pathways and proteins are upregulated during pancreatitis, and serve as a bridge connecting pancreatitis and pancreatic cancer. Thus, pancreatitis-induced ADM formation and pancreatic carcinogenesis were blocked by inhibiting those pathways and proteins. Luteolin has been demonstrated to exhibit various anti-neoplastic properties, for example pro-apoptosis, inhibition of EMT and reversing chemotherapeutic-resistance (26–28). It has been identified to affect a number of pathways (28,29,32), and some of those pathways additionally serve roles on pancreatitis-induced ADM formation and pancreatic carcinogenesis. Thus, it was suggested that luteolin may inhibit pancreatitis-induced ADM formation. At present, the majority of studies about pancreatic carcinogenesis focused on the pathogenetic mechanisms and regulatory pathways of ADM and PDAC formation, few studies focused on interference of them with exogenous agents. The current study used luteolin, a herbal extract, to interfere with ADM by inhibiting pro-ADM pathways and proteins.
The current study identified that inflammation-associated pathways such as IL6-STAT3 and EGFR pathways were all activated on day 1 and then decreased to normal levels by day 3. It was observed that cearulein-induced inflammation of the pancreas was most prominent on day 1, compared with days 3 and 5. However, it was identified that morphological changes of acini were most prominent on day 3, not day 1. On day 3, acinar cells under ADM transformed into a more duct-like structure, accompanied by high levels of non-acinar cell infiltration. Notably, on day 3, metaplastic acini always clustered together in a lobule, single metaplastic acinus were not identified between non-ADM acini. ADM is considered as a pathological change caused by inflammation during pancreatitis (9). However, considering the difference between the time of inflammation and ADM and the characteristics of ADM on day 3, it was hypothesized that ADM may be not a pathological process directly caused by inflammation, however rather a physiological change actively mediated via acinar cells subsequent to exposure to inflammation. ADM has been regarded as a necessary step for Kras-dependent pancreatic carcinogenesis, and acinar cells under ADM exhibit increased tendency for malignant transition (8). However, it was suggested that ADM may have positive or protective effects for acinar cells during pancreatitis. Nevertheless, further study is required in order to confirm these hypotheses.
Early metastasis serves an important role in the poor prognosis of pancreatic cancer. It was reported that during the process of pancreatic carcinogenesis on mice with Kras mutation, EMT and dissemination of acinar cells precede tumor formation, and the EMT of acinar cells was promoted by pancreatitis (22). In addition, pancreatitis-induced pancreatic carcinogenesis has been observed to be accompanied by increased expression of, matrix metalloproteinase, which in turn increased the invasiveness of cancer cells (17). The present study confirmed that pancreatitis induces EMT of acinar cells. Therefore, pancreatitis not only promotes carcinogenesis of pancreatic cancer, it may also lead to acinar cells under malignant transformation becoming highly invasive. It is therefore hypothesized that pancreatic cancer cells gained invasiveness predominantly during carcinogenesis. This was different to that of the traditional view, which suggests that cancer cells gain invasiveness step by step by accumulation of mutations and stimulation of inflammation.
For two reasons, the present study suggested that luteolin could be an effective agent to inhibit pancreatic carcinogenesis. Firstly, luteolin inhibits ADM formation induced by pancreatitis. ADM gives rise to PanIN and has been confirmed as an early step in Kras-dependent pancreatic carcinogenesis (4). Furthermore, the IL6-STAT3 pathway, EGFR-ras pathway and SOX9 protein, all of which are inhibited by luteolin, serve essential roles in pancreatic carcinogenesis (8,11,12,15,16). Due to the limitation of the therapeutic methods, pancreatic cancer remains almost untreatable once it occurs. The interference of carcinogenesis in people with significant risk factors may become an important treatment for pancreatic cancer. With anti-ADM formation and anti-EMT properties, luteolin may serve an important role in anti-pancreatic cancer strategies in the future.
Acknowledgements
The current study was sponsored by grants from the National Natural Science Foundation of China (grant no. 81070372) and the Provincial Department of Construction Project (grant no. WKJ2012-2-033).
Glossary
Abbreviations
- ADM
acinar-ductal metaplasia
- CK19
cytokeratin-19
- EGFR
epithelial growth factor receptor
- EMT
epithelial-mesenchymal transition
- H&E
hematoxylin and eosin
- PanIN
pancreatic intra-epithelial neoplasia
- PDAC
pancreatic ductal adenocarcinoma
- RT-qPCR
reverse transcription-quantitative polymerase chain reaction
- STAT3
signal transducer and activator of transcription 3
References
- 1.Vincent A, Herman J, Schulick R, Hruban RH, Goggins M. Pancreatic cancer. Lancet. 2011;378:607–620. doi: 10.1016/S0140-6736(10)62307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ekbom A, McLaughlin JK, Nyrén O. Pancreatitis and the risk of pancreatic cancer. N Engl J Med. 1993;329:1502–1503. doi: 10.1056/NEJM199311113292016. [DOI] [PubMed] [Google Scholar]
- 3.Guerra C, Schuhmacher AJ, Cañamero M, Grippo PJ, Verdaguer L, Pérez-Gallego L, Dubus P, Sandgren EP, Barbacid M. Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell. 2007;11:291–302. doi: 10.1016/j.ccr.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 4.Morris JP, IV, Cano DA, Sekine S, Wang SC, Hebrok M. Beta-catenin blocks Kras-dependent reprogramming of acini into pancreatic cancer precursor lesions in mice. J Clin Invest. 2010;120:508–520. doi: 10.1172/JCI40045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hruban RH, Wilentz RE, Maitra A. Identification and analysis of precursors to invasive pancreatic cancer. Methods Mol Med. 2005;103:1–13. doi: 10.1385/1-59259-780-7:001. [DOI] [PubMed] [Google Scholar]
- 6.De La OJP, Emerson LL, Goodman JL, Froebe SC, Illum BE, Curtis AB, Murtaugh LC. Notch and Kras reprogram pancreatic acinar cells to ductal intraepithelial neoplasia; Proc Natl Acad Sci USA; 2008; pp. 18907–18912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shih HP, Kopp JL, Sandhu M, Dubois CL, Seymour PA, Grapin-Botton A, Sander M. A Notch-dependent molecular circuitry initiates pancreatic endocrine and ductal cell differentiation. Development. 2012;139:2488–2499. doi: 10.1242/dev.078634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kopp JL, von Figura G, Mayes E, Liu FF, Dubois CL, Morris JP, IV, Pan FC, Akiyama H, Wright CV, Jensen K, et al. Identification of Sox9-dependent acinar-to-ductal reprogramming as the principal mechanism for initiation of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;22:737–750. doi: 10.1016/j.ccr.2012.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prévot PP, Simion A, Grimont A, Colletti M, Khalaileh A, Van den Steen G, Sempoux C, Xu X, Roelants V, Hald J, et al. Role of the ductal transcription factors HNF6 and Sox9 in pancreatic acinar-to-ductal metaplasia. Gut. 2012;61:1723–1732. doi: 10.1136/gutjnl-2011-300266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grimont A, Pinho AV, Cowley MJ, Augereau C, Mawson A, Giry-Laterrière M, Van den Steen G, Waddell N, Pajic M, Sempoux C, et al. SOX9 regulates ERBB signalling in pancreatic cancer development. Gut. 2015;64:1790–1799. doi: 10.1136/gutjnl-2014-307075. [DOI] [PubMed] [Google Scholar]
- 11.Ardito CM, Grüner BM, Takeuchi KK, Lubeseder-Martellato C, Teichmann N, Mazur PK, Delgiorno KE, Carpenter ES, Halbrook CJ, Hall JC, et al. EGF receptor is required for KRAS-induced pancreatic tumorigenesis. Cancer Cell. 2012;22:304–317. doi: 10.1016/j.ccr.2012.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Navas C, Hernández-Porras I, Schuhmacher AJ, Sibilia M, Guerra C, Barbacid M. EGF receptor signaling is essential for k-ras oncogene-driven pancreatic ductal adenocarcinoma. Cancer Cell. 2012;22:318–330. doi: 10.1016/j.ccr.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Collins MA, Yan W, Sebolt-Leopold JS, Pasca di Magliano M. MAPK signaling is required for dedifferentiation of acinar cells and development of pancreatic intraepithelial neoplasia in mice. Gastroenterology. 2014;146:822–834.e7. doi: 10.1053/j.gastro.2013.11.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu CY, Carpenter ES, Takeuchi KK, Halbrook CJ, Peverley LV, Bien H, Hall JC, DelGiorno KE, Pal D, Song Y, et al. PI3K regulation of RAC1 is required for KRAS-induced pancreatic tumorigenesis in mice. Gastroenterology. 2014;147:1405–1416.e7. doi: 10.1053/j.gastro.2014.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corcoran RB, Contino G, Deshpande V, Tzatsos A, Conrad C, Benes CH, Levy DE, Settleman J, Engelman JA, Bardeesy N. STAT3 plays a critical role in KRAS-induced pancreatic tumorigenesis. Cancer Res. 2011;71:5020–5029. doi: 10.1158/0008-5472.CAN-11-0908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lesina M, Kurkowski MU, Ludes K, Rose-John S, Treiber M, Klöppel G, Yoshimura A, Reindl W, Sipos B, Akira S, et al. Stat3/Socs3 activation by IL-6 transsignaling promotes progression of pancreatic intraepithelial neoplasia and development of pancreatic cancer. Cancer Cell. 2011;19:456–469. doi: 10.1016/j.ccr.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 17.Fukuda A, Wang SC, Morris JP, IV, Folias AE, Liou A, Kim GE, Akira S, Boucher KM, Firpo MA, Mulvihill SJ, et al. Stat3 and MMP7 contribute to pancreatic ductal adenocarcinoma initiation and progression. Cancer Cell. 2011;19:441–455. doi: 10.1016/j.ccr.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang Y, Morris JP, IV, Yan W, Schofield HK, Gurney A, Simeone DM, Millar SE, Hoey T, Hebrok M, Pasca di Magliano M. Canonical wnt signaling is required for pancreatic carcinogenesis. Cancer Res. 2013;73:4909–4922. doi: 10.1158/0008-5472.CAN-12-4384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pasca di Magliano M, Sekine S, Ermilov A, Ferris J, Dlugosz AA, Hebrok M. Hedgehog/Ras interactions regulate early stages of pancreatic cancer. Genes Dev. 2006;20:3161–3173. doi: 10.1101/gad.1470806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brabletz S, Bajdak K, Meidhof S, Burk U, Niedermann G, Firat E, Wellner U, Dimmler A, Faller G, Schubert J, Brabletz T. The ZEB1/miR-200 feedback loop controls Notch signalling in cancer cells. EMBO J. 2011;30:770–782. doi: 10.1038/emboj.2010.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang F, Sloss C, Zhang X, Lee SW, Cusack JC. Membrane-bound heparin-binding epidermal growth factor like growth factor regulates E-cadherin expression in pancreatic carcinoma cells. Cancer Res. 2007;67:8486–8493. doi: 10.1158/0008-5472.CAN-07-0498. [DOI] [PubMed] [Google Scholar]
- 22.Rhim AD, Mirek ET, Aiello NM, Maitra A, Bailey JM, McAllister F, Reichert M, Beatty GL, Rustgi AK, Vonderheide RH, et al. EMT and dissemination precede pancreatic tumor formation. Cell. 2012;148:349–361. doi: 10.1016/j.cell.2011.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Middleton E, Jr, Kandaswami C, Theoharides TC. The effects of plant flavonoids on mammalian cells: Implications for inflammation, heart disease, and cancer. Pharmacol Rev. 2000;52:673–751. [PubMed] [Google Scholar]
- 24.Kandaswami C, Lee LT, Lee PP, Hwang JJ, Ke FC, Huang YT, Lee MT. The antitumor activities of flavonoids. In Vivo. 2005;19:895–909. [PubMed] [Google Scholar]
- 25.Jia Z, Nallasamy P, Liu D, Shah H, Li JZ, Chitrakar R, Si H, McCormick J, Zhu H, Zhen W, Li Y. Luteolin protects against vascular inflammation in mice and TNF-alpha-induced monocyte adhesion to endothelial cells via suppressing IΚBα/NF-κB signaling pathway. J Nutr Biochem. 2015;26:293–302. doi: 10.1016/j.jnutbio.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shi RX, Ong CN, Shen HM. Luteolin sensitizes tumor necrosis factor-alpha-induced apoptosis in human tumor cells. Oncogene. 2004;23:7712–7721. doi: 10.1038/sj.onc.1208046. [DOI] [PubMed] [Google Scholar]
- 27.Hong Z, Cao X, Li N, Zhang Y, Lan L, Zhou Y, Pan X, Shen L, Yin Z, Luo L. Luteolin is effective in the non-small cell lung cancer model with L858R/T790M EGF receptor mutation and erlotinib resistance. Br J Pharmacol. 2014;171:2842–2853. doi: 10.1111/bph.12610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang X, Dai S, Dai J, Xiao Y, Bai Y, Chen B, Zhou M. Luteolin decreases invasiveness, deactivates STAT3 signaling, and reverses interleukin-6 induced epithelial-mesenchymal transition and matrix metalloproteinase secretion of pancreatic cancer cells. Onco Targets Ther. 2015;8:2989–3001. doi: 10.2147/OTT.S91511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seymour PA, Freude KK, Tran MN, Mayes EE, Jensen J, Kist R, Scherer G, Sander M. SOX9 is required for maintenance of the pancreatic progenitor cell pool; Proc Natl Acad Sci USA; 2007; pp. 1865–1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rau B, Paszkowski A, Lillich S, Baumgart K, Möller P, Beger HG. Differential effects of caspase-1/interleukin-1beta-converting enzyme on acinar cell necrosis and apoptosis in severe acute experimental pancreatitis. Lab Invest. 2001;81:1001–1013. doi: 10.1038/labinvest.3780312. [DOI] [PubMed] [Google Scholar]
- 31.Reid LE, Walker NI. Acinar cell apoptosis and the origin of tubular complexes in caerulein-induced pancreatitis. Int J Exp Pathol. 1999;80:205–215. doi: 10.1046/j.1365-2613.1999.00116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bagli E, Stefaniotou M, Morbidelli L, Ziche M, Psillas K, Murphy C, Fotsis T. Luteolin inhibits vascular endothelial growth factor-induced angiogenesis: Inhibition of endothelial cell survival and proliferation by targeting phosphatidylinositol 3′-kinase activity. Cancer Res. 2004;64:7936–7946. doi: 10.1158/0008-5472.CAN-03-3104. [DOI] [PubMed] [Google Scholar]