Abstract
Elevated C-reactive protein (CRP) in association with hyperinsulinemia is a significant risk factor for cardiovascular diseases and that plays a key role in the development of the PCOS. We evaluated serum CRP level, before and after metformin therapy in obese women with polycystic ovarian syndrome (PCOS). Thirty five obese women with PCOS [BMI=28,2±1,84kg/m2, aged 20-35 years] were studied. Patients received metformin orally the dose of 850 mg per day. The patients were carefully interviewed, clinically examined, and laboratory tested to eliminate conditions, probable to provoke an inflammatory response which was an exclusion criterion. Subjects were excluded if there was clinical or electrocardiographic evidence of coronary artery disease, a family history of coronary artery disease, a history of smoking, or concurrent oestrogen, antihypertensive, or lipid lowering medication. At all patients we determined CRP, insulin, C-peptide, luteinising hormone, follicle stimulating hormone, oestradiol, testosterone, prolactin, TSh, T3, T4, glucose, fibrinogen and lipid profile, before and after metformin treatment. Mean serum C-RP levels significantly decreased after metformin treatment ((6,37±1,72 vs. 1,67±0,73 mg/l; p<0,05). Level of insulin reduced for 37% after metfromin treatment (234±68 vs. 148±39μmol/l). Total cholesterol and low-density lipoprotein cholesterol levels decreased as well. Mean total testosterone levels decreased after metformin treatment too (3,21±0,91, vs. 2,31±0,72 nmol/l). Elevated serum CRP level significantly correlated to the hyperinsulinaemia (r=0,54). Metformin therapy in PCOS women reduces CRP level, hyperinsulinaemia and cardiovascular risk.
Keywords: C-reactive protein, hyperinsulinaemia, PCOS, metformin
INTRODUCTION
Insulin resistance and compensatory hyperinsu-linaemia have been consistently documented in lean and obese women with PCOS. Increased activity of plasminogen activation inhibitor-I and C-re-active protein (CRP) associated with increased cardiovascular risk in PCOS (1). This increased cardiovascular risk is probably the result, in part, of the metabolic disturbance associated with PCOS. Dyslipidae-mia, diabetes, and obesity are all potent cardiovascular risk factors that tend to cluster in women with PCOS. In recent years, interest has grown in novel biochemical and biophysical markers of cardiovascular risk. C reactive protein (CRP) has been shown to be a good predictor of vascular events. In addition to being a marker of inflammation, there is evidence that CRP may have a direct role in atherogenesis via adhesion molecule expression, complement activation, and mediation of low density lipoprotein (LDL) uptake by macrophages (2). Elevated CRP in association with hyperinsulinemia is a significant risk factor for cardiovascular diseases and that plays a key role in the development of the PCOS (3). Amenorrhoea, polycystic ovaries, hirsutism, high fasting insulin and high testosterone concentrations characterize polycistic ovary syndrome (PCOS).
OBJECTIVE
We aimed to evaluate the effect of metformin on serum CRP levels as marker of cardiovascular risk in obese PCOS women.
PATIENTS AND METHODS
Thirty five premenopausal, obese women with PCOS [BMI=28,2±1,84kg/m2, aged 20-35 years] were studied. Patients received metformin orally the dose of 850 mg per day. The patients were carefully interviewed, clinically examined, and laboratory tested to eliminate conditions probable to provoke an inflammatory response which was an exclusion criterion. PCOS was defined as an ovarian ultrasound diagnosis, with a history of menstrual disturbance (amenorrhoea/oligomenor-rhoea), in association with raised serum testosterone and luteinising hormone, and a low or normal follicle stimulating hormone. Subjects were excluded if there was clinical or electrocardiographic evidence of coronary artery disease, a family history of coronary artery disease, a history of smoking, or concurrent oestrogen, antihypertensive, or lipid lowering medication. At all patients we determined CRP, basal insulin, basal C-peptide, luteinising hormone, follicle stimulating hormone, oestradiol, testosterone, prolactin, TSh, T3, T4, glucose, fibrinogen and lipid profile, before and after metformin treatment. Serum CRP levels were measured with immunometric assay, level of insulin were measured with RIA. Student’s T-test, percen-tile and correlation was reformed in statistical analysis.
RESULTS
After one year of metformin treatment, mean serum CRP levels significantly decreased (6,37 ± 1,72 vs. 1,67 ± 0,73 mg/l; p<0,05), Figure 1. Basal insulin levels reduced for 37% after metfromin treatment (234±68 vs. 148±39μmol/l) Figure 2. Total cholesterol and low-density lipoprotein cholesterol levels decreased as well (Figure 3). Mean total testosterone levels decreased after metformin treatment too (3,21±0,91, vs. 2,31±0,72nmol/ l), Figure 4. Elevated serum CRP level significantly correlated to the hyperinsulinaemia (r=0,54), Figure 5.
FIGURE 1.
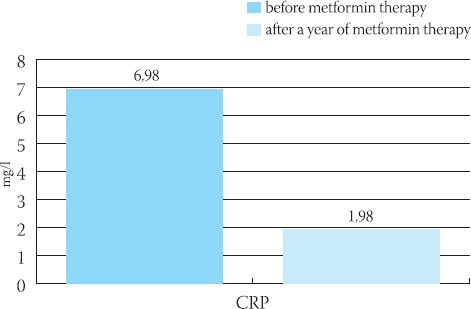
Decreasing of CRP levels after metformin treatment in PCOS women (p<0,05)
FIGURE 2.
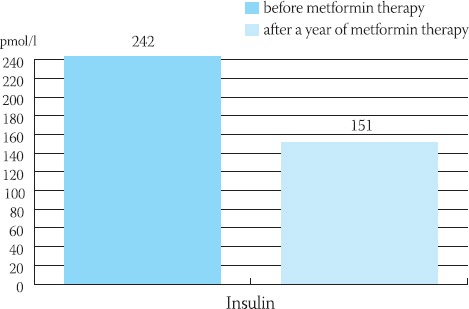
Decreasing of insulin levels after metformin treatment in PCOS women (37%)
FIGURE 3.
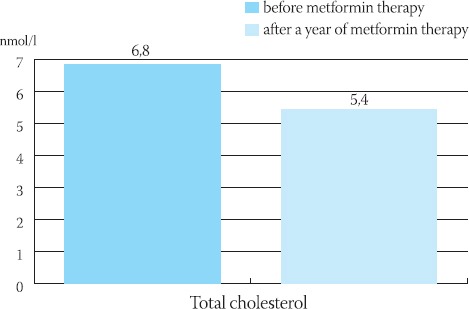
Decreasing of cholesterol levels after metformin treatment in PCOS women
FIGURE 4.
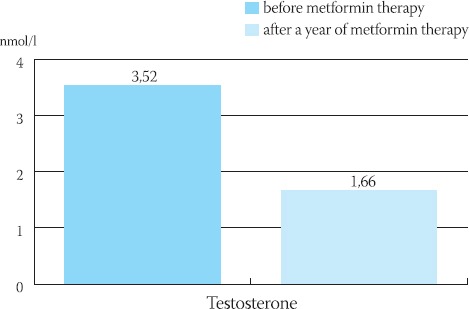
Decreasing of testosteron levels after metformin treatment in PCOS women
FIGURE 5.
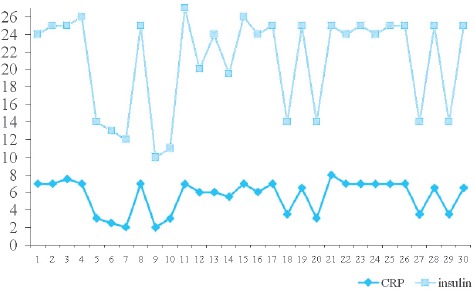
The correlation between CRP and insulin in PCOS women (r=0,54)
DISCUSSION
C-reactive protein (CRP) is associated with insulin resistance and as such increases both risk of development of diabetes type 2 and cardiovascular risk. Ibáñez and colleagues suggest a possible synergistic effect of obesity, insulin resistance and diabetes mellitus on the chronic low-level inflammation, which may play a crucial role in the pathogenesis of atherosclerosis and the possibility that CRP may be a novel therapeutic target (4). Low grade chronic inflammation as reflected by increased C-reactive protein (CRP) concentrations independently predicts those at risk for coronary heart disease (CHD) and type 2 diabetes in women with polycystic ovarian syndrome (5). Yudkin and colleagues have shown that CRP concentrations measured using a highly sensitive assay are significantly increased in women with PCOS relative to those in healthy women with normal menstrual rhythm and normal androgen levels after correction for BMI. In keeping with previous data, they also noted that CRP concentrations in both PCOS women correlated with the degree of obesity and inversely with insulin sensitivity (6), although not with total testosterone concentrations. Adipose tissue-derived cytokine expression (tumor necrosis factor-α and interleukin-6) may be an important contributor to low grade chronic inflammation. In other words, accumulation of visceral adipose tissue may be a key factor underpinning features of the metabolic syndrome and of low grade chronic inflammation. These combined observations would also explain the correlation of insulin sensitivity to CRP, as recently noted by Festa and colleagues (7). Larger, randomized, placebo-controlled trials are now needed to examine the potential impact of met-formin in PCOS women. Metformin has been proved to be active as a pro-ovulatory compound even in the presence of normal fasting insulin (8), which suggests a direct action of this drug at the ovarian level. Metfor-min has recently been shown to reduce serum C-reac-tive protein (CRP) levels in women with PCOS (9).
CONCLUSION
Metformin therapy reduces CRP level, hyperinsulinaemia and cardiovascular risk in PCOS women. The decrease of serum CRP levels during metformin therapy is in accordance with the known beneficial metabolic effects of this drug and suggests that CRP or other inflammation parameters could be used as markers of treatment efficiency in women with PCOS.
REFERENCES
- 1.Sampson M, Kong C, Patel A, Unwin R, Jacobs H.S. Ambulatory blood pressure profiles and plasminogen activator inhibitor (PAI-1) activity in lean women with and without the polycystic ovary syndrome. Clin. Endocrinol. 1996;45:623–629. doi: 10.1046/j.1365-2265.1996.00863.x. [DOI] [PubMed] [Google Scholar]
- 2.Blake G.J, Ridker P.M. Inflammatory bio-markers and cardiovascular risk prediction. J. Intern. Med. 2002;252:283–294. doi: 10.1046/j.1365-2796.2002.01019.x. [DOI] [PubMed] [Google Scholar]
- 3.Boulman N, Levy Y, Leiba R, Shachar S, Linn R, Zinder O, Blumenfeld Z. Increased C-reactive protein levels in the polycystic ovary syndrome: A marker of cardiovascular disease. J. Clin. En-docrinol. Metab. 2004;89(5):2160–2165. doi: 10.1210/jc.2003-031096. [DOI] [PubMed] [Google Scholar]
- 4.Ibáñez L, Valls C, De Zegher F. Low-dose flutamide-met-formin (Flu-Met) with an oral contraceptive is a therapeutic option for women with hyperinsulinaemic hyperandrogenism. Human Reproduction. 2006;21(2):451–456. doi: 10.1093/humrep/dei329. [DOI] [PubMed] [Google Scholar]
- 5.Kelly C. J, Lyall H, Petne J.R, Gould G.W, M.C, Connell J, Sat-tar N. Low grade chronic inflammation in women with polycys-tic ovarian syndrome. J Clin. Endocrinol. Metabol. 2001;86(6):2453–2455. doi: 10.1210/jcem.86.6.7580. [DOI] [PubMed] [Google Scholar]
- 6.Yudkin J.S, Stehouwer C.D, Emeis J.J, Coppack S.W. C-Reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue? Arterioscler. Thromb. Vasc. Biol. 1999;19:972–978. doi: 10.1161/01.atv.19.4.972. [DOI] [PubMed] [Google Scholar]
- 7.Festa A, D’Agostino R.J, Howard G, Mykkänen L, Tracy R.P, Haflner S.M. Chronic subclinical inflammation as part of the insulin resistance syndrome: The Insulin Resistance Atherosclerosis Study (IRAS) Circulation. 2000;102:42–47. doi: 10.1161/01.cir.102.1.42. [DOI] [PubMed] [Google Scholar]
- 8.Sattar N, Hopkinson Z.E, Greer I.A. Insulin-sensitising agents in polycystic-ovary syndrome. Lancet. 1998;354:305–307. doi: 10.1016/S0140-6736(05)78345-8. [DOI] [PubMed] [Google Scholar]
- 9.Morin-Papunen L, Rautio K, Ruokonen A, Hedberg P, Puukka M, Tapanainen J.S. Metformin reduces serum C-reactive protein levels in women with polycystic ovary syndrome. J. Chn. Endocri-nol. Metab. 2003;88:4649–4654. doi: 10.1210/jc.2002-021688. [DOI] [PubMed] [Google Scholar]


