Abstract
Studies in urban informal settlements show widespread inappropriate infant and young child feeding (IYCF) practices and high rates of food insecurity. This study assessed the association between household food security and IYCF practices in two urban informal settlements in Nairobi, Kenya. The study adopted a longitudinal design that involved a census sample of 1110 children less than 12 months of age and their mothers aged between 12 and 49 years. A questionnaire was used to collect information on: IYCF practices and household food security. Logistic regression was used to determine the association between food insecurity and IYFC practices. The findings showed high household food insecurity; only 19.5% of the households were food secure based on Household Insecurity Access Score. Infant feeding practices were inappropriate: 76% attained minimum meal frequency; 41% of the children attained a minimum dietary diversity; and 27% attained minimum acceptable diet. With the exception of the minimum meal frequency, infants living in food secure households were significantly more likely to achieve appropriate infant feeding practices than those in food insecure households: minimum meal frequency (adjusted odds ratio (AOR) = 1.26, P=0.530); minimum dietary diversity (AOR = 1.84, P=0.046) and minimum acceptable diet (AOR = 2.35, P=0.008). The study adds to the existing body of knowledge by demonstrating an association between household food security and infant feeding practices in low-income settings. The findings imply that interventions aimed at improving infant feeding practices and ultimately nutritional status need to also focus on improving household food security.
Keywords: complementary feeding, household food security, infant feeding practices, urban informal settlements
Introduction
In East Africa, undernutrition is a major problem with close to 50% of young children being stunted.1 In Kenya, 26% of children under 5 years have stunted growth, 11% are underweight and 4% are wasted according to the 2014 Kenya Demographic and Health Survey (KDHS). This is an improvement from 2008 when stunting was at 35%, underweight at 16% and wasting at 7%.2 In the urban informal settlements (UIS) levels of stunting have remained persistently high, higher than national levels according to studies carried out from 2008 to 2015, but levels for underweight and wasting are comparable with the national levels. Examples are: Kibera where rates for stunting, underweight and wasting are 47, 11.8 and 2.6%,3 and Korogocho and Viwandani, where rates are 46, 11 and 2.5%.4 This situation in Kenyan UIS is not unique, similar a stunting rate of 46% has been reported in IS in India.5 A comparative analysis of health status carried out among IS and non-IS, and rural and urban populations in Bangladesh, Kenya, Egypt and India reported that children in UIS had much poorer health outcomes than children in all other residential domains.6
Appropriate infant and young child feeding (IYCF) practices, which include breastfeeding and complementary feeding, play a major role in the healthy growth and development of children, and help to reduce under-nutrition.7–10 The 2013 Lancet series on Maternal and Child Nutrition reports that sub-optimal breastfeeding results in an increased risk for mortality in the first 2 years of life.11 Black et al. (2008) reported that sub-optimal breastfeeding was responsible for 14 million child deaths and 44 million disability-adjusted life years (DALYs) (10% of DALYs in children younger than 5 years). The indicators of complementary feeding include; time of initiation of complementary foods; frequency of feeding of complementary feeding and minimum acceptable diet – a composite indicator that includes appropriate frequency of feeding and minimum dietary diversity.12 It is recommended that children be introduced to solid and semi-solid foods at the age of 6 months. For the minimum dietary diversity, it is recommended that children aged 6–23 months be fed foods from four or more food groups out of seven groups daily. In addition, it is recommended that children should receive solid, semi-solid or soft food the minimum number of times or more; two times for breastfed children 6–8 months old, three times for those aged 9–23 months and four times for non-breastfed children aged 6–23 months.12 However, the recommendation seems not to be met in the Kenyan context as only about two in 10 children aged 6–23 months consume the minimum acceptable diet, which is a composite indicator that considers both food diversity and frequency.13
Non-adherence to WHO IYCF guidelines or sub-optimal infant feeding practices has been reported in UIS.14,15 For instance, in Korogocho and Viwandani in Nairobi, Kenya, only 2% of the infants <6 months of age are exclusively breastfed.16 In Korogocho, only 15.4% of the children 6–23 months old attained a minimum acceptable diet in 2013.15 Factors associated with sub-optimal breastfeeding include poverty, early and single motherhood, poor knowledge about breastfeeding, and myths and misconceptions.17,18
Globally, food and nutrition insecurity remains a major challenge. According to the Food and Agriculture Organization (FAO) hunger indicator, it is estimated that between the years 2010 and 2012, 870 million people (about 12.5% of global population) were undernourished, with the majority of them in developing countries and 234 million in sub-Saharan Africa.19 In Kenya, more than 10 million people (almost a third of the Kenyan population) suffer from chronic food insecurity and poor nutrition.20 In Kenya’s urban poor, only one household in five is food secure;21,22 which means that only a small percentage of the population have physical and economic access to sufficient, safe and nutritious food to meet their dietary needs and food preferences for an active and healthy life. In the UIS negative coping strategies are widely used to address food insecurity, including reducing the number of meals, reducing food variety and quality, scavenging and eating street foods.22
While household food insecurity is prevalent in these settings, a few studies have explored the linkage between household food security and IYCF practices. In rural Bangladesh, better household food security status was reported to be associated with poor IYCF practices among children between three and 6 months old but was associated with better practices during the second half of infancy.5 Separate studies carried out in Ghana and Bangladesh reported that children in food secure households were significantly more likely to receive a minimum acceptable diet than those in food insecure households.9,23 In Kenya, there is paucity of data on the influence of household food security on IYCF practices. One study, however, conducted in Viwandani and Korogocho in Nairobi reported that maternal perception of food insecurity negatively affected breastfeeding.17 About 72% of the urban population in Africa lives in slums,24 which are characterized by food insecurity and poor IYCF practices. With the increasing urbanization and natural growth, more households are likely to end up in slums aggravating the problem of food insecurity and inappropriate feeding practices among the poor. This emphasizes the need to investigate how household food insecurity among low-income urban dwellers influences infant feeding practices. UIS present unique challenges with regards to child health, nutrition and survival including lack of social amenities, high unemployment, overcrowding, insecurity and social fragmentation6,25–27 and with increasing urbanization, the problem of food insecurity and malnutrition in UIS are likely to increase unless special efforts are put in place to mitigate the problem. Therefore, bridging the information gap on the association between food insecurity and IYCF practices in a local context is necessary to guide future interventions such as nutrition-sensitive strategies aimed at improving the nutritional status and the overall health of children in urban poor households. The aim of this study was to assess the association between household food security and infant feeding practices in Korogocho and Viwandani UIS in Nairobi County, Kenya.
Methodology
Research design
This study was embedded within a larger study the Maternal Infant and Young Child Nutrition (MIYCN)28 by the African Population and Health Research Center (APHRC). The study was a cluster randomized controlled trial conducted in two urban informal settlements in Nairobi and involved a census sample of 1101 and follow-up of the women during pregnancy, and a follow-up of the mother–child pairs after birth till the end of the child’s infancy.28 The sample size determination for the main study was calculated taking into consideration the cluster randomized study design.28
This paper presents information on the association of household food security and IYCF practices for the participating households that was not a core objective of the MIYCN study but used household food security and IYCF practices data that was collected in the larger study.
Study setting
The MIYCN study was carried out in two informal settlements in Nairobi: Korogocho and Viwandani, nested within the Nairobi Urban Health and Demographic Surveillance System (NUHDSS) operated by APHRC. The NUHDSS covers around 65,000 individuals in 24,000 households in Korogocho and Viwandani urban informal settlements and it involves a systematic recording of vital demographic events three times a year, since 2003.29 The two settlements are densely populated and are characterized by poor housing, lack of basic infrastructure, insecurity, high unemployment rates, poor availability and accessibility of health services and poor health indicators.30
Data collection procedures
Researcher-administered structured questionnaires were used to collect data on household food security at baseline and IYCF practices postpartum. The questionnaires were also used to collect information on morbidity and immunization status of the infants and demographic and socio-economic characteristics of the mothers. The information on infant feeding practices was collected every 2 months at the household level.
Study variables
This study assessed the association of household food security and infant feeding practices in the study area. The outcome variables were infant feeding practices measured using the WHO indicators.12 The indicators were: exclusive breastfeeding (EBF) for the first 6 months; time of initiation of complementary feeding; minimum dietary diversity, minimum frequency of feeding and minimum acceptable diet. The indicator for the correct timing of initiation of complementary feeding was the percentage of infants 6–8 months who ate solid or semi-solid foods The minimum dietary diversity was determined by the percentage of children 6–23 months old who ate foods from a minimum of four food groups and also the mean dietary score from the following seven groups of food (grains, roots and tubers; legumes and nuts; dairy products (milk, yogurt and cheese); flesh foods (meat, fish, poultry and liver/organ meats); eggs; vitamin A rich fruits and vegetables and other fruits and vegetables. Minimum meal frequency was established for the proportion of breastfed infants 6–11 months of age who received solid, semi-solid, or soft foods and for non-breastfed infants 6–11 months (but also received milk feeds). The indicator for minimum meal frequency is two times for breastfed infants 6–8 months old, three times for breastfed children 9–11 months old and four times for non-breastfed children 6–11 months old. Meals include both meals and snacks (other than trivial amounts <15 g). Minimum acceptable diet was worked out as those infants who received the minimum meal frequency and the minimum dietary diversity. Complementary feeding practices were determined based on maternal 24 h recalls.
The main independent variable was household food security computed using the Household Food Insecurity Access Score method.31 A set of nine questions that relate to three different domains of food insecurity (access) were used to calculate the score (i) anxiety and uncertainty about the household food supply with regards to whether one worried that the household would not have enough to eat; (ii) insufficient quality in terms of variety and preferences of the type of food the household accessed; and (iii) insufficient food intake in terms of reducing quantity of food eaten in a meal and number of meals. Each of the nine questions was asked with a recall period of 4 weeks to address the three domains with the answers ranging from never having experienced conditions related to food insecurity, experiencing them rarely, sometimes or often. Households that experienced none of the food insecurity condition or just rarely experienced worry was defined as food secure. Mildly food insecure households worried about not having enough food sometimes or often, and/or was unable to eat preferred foods, and/or eat a more monotonous diet than desired and/or some foods considered undesirable, but only rarely. Moderately food insecure households sacrificed quality more frequently, by eating monotonous diets or undesirable foods sometimes or often, and/or had started to cut back on quantity by reducing the size of meals or number of meals, rarely or sometimes. Severely food insecure households were those that resorted to cutting back on meal size or number of meals often, and/or experienced any of the three most severe conditions. Any household that experienced one of the three most severe conditions (running out of food, going to bed hungry, or going a whole day and night without eating) was considered as severely food insecure.31
Data analysis
Descriptive statistics (frequencies and proportions) were used to summarize both the outcome of interest and the independent variables. χ2 tests for independence were used to test association between household food insecurity and independent variables. Logistic regression models (bivariate and multivariate) were used to assess the association between household food security and independent variables. All tests were done at 95% confidence level. All data management and analysis were conducted using STATA version 13.1. The following variables were controlled in the multivariate analysis: marital status, religion, mother’s age, parity, residence, mother’s occupation, education level, household size, place of delivery, whether the household were in the intervention or control groups, sex and morbidity status of the index child.
Ethical considerations
Ethical approval for the main study was granted to APHRC by the Kenya Medical Research Institute Ethics Review Committee reference number KEMRI/RES/7/3/1. The investigators upheld the fundamental principles regarding research on human subjects: respect for persons, beneficence and justice. Informed consent was sought from the respondents following full disclosure regarding the study before interviews were conducted while proxy consent for children was obtained from their mothers. Data were collected electronically and for confidentiality, passwords only known to the research team were used to access the data.
Results
Characteristics of the study population
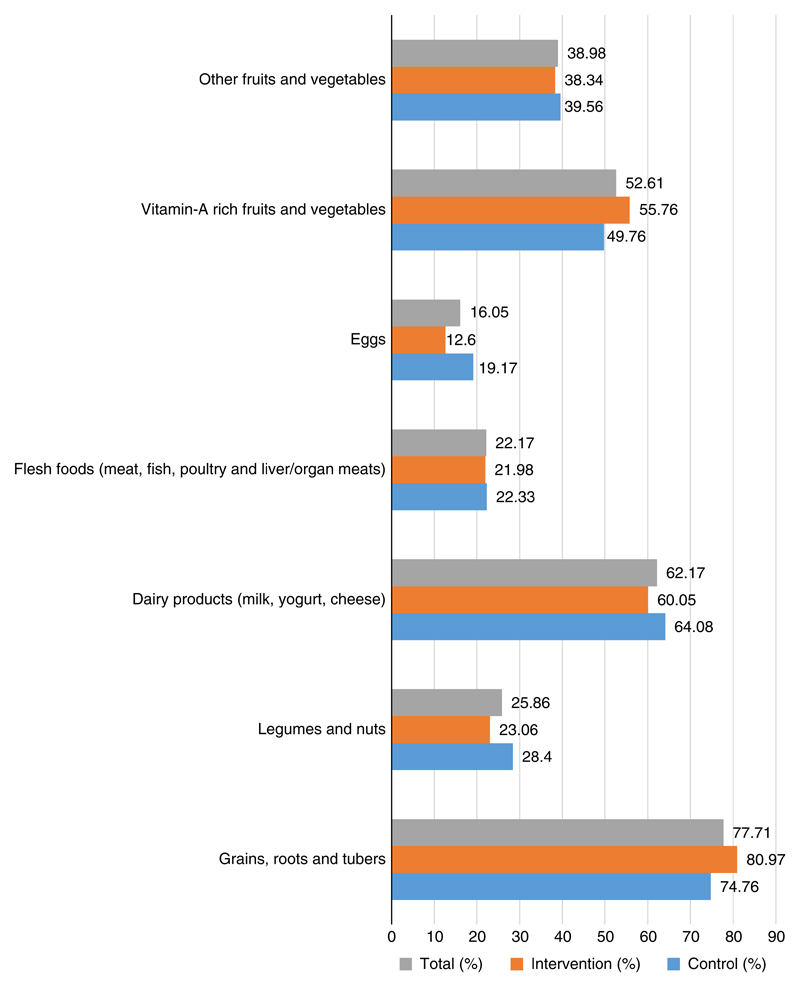
A total of close to 1500 mothers were recruited, some mothers were lost to follow-up and 1101 mothers were followed up after pregnancy until 12 months postpartum. The youngest mother was 14 and the oldest 45 years old. Majority of the mothers (83.7%) were either married or living together with a partner and 82.1% at least had primary education. About a third of the mothers were either employed, self-employed or casual labourers (Table 1). The majority of the children (84.2%) had been initiated to breastfeeding on time and the EBF rate was 60.4% (Table 2). Nearly all infants 6–8 months old (97%) had received solid, semi-solid or soft foods. The majority (76.3%) of the children aged 6–11 months attained a minimum meal frequency. Grains, roots and tubers were consumed by 78.3% of the children, 26.1% consumed legumes and nuts while 62.6% consumed dairy products. The consumption of animal foods was low as only 22.4% consumed flesh foods and only 16.1% consumed eggs. Vitamin A-rich fruits and vegetables were consumed by 52.7 and 39% consumed other fruits and vegetables Fig. 1; 41% of children aged 6–11 months attained the minimum dietary diversity while approximately a third of the children (27%) achieved the minimum acceptable diet (Table 2). Households reported using various coping strategies in the 4 weeks preceding the interview (Table 3). The most frequently used strategies related to not eating preferred foods and eating limited variety of foods whilst about 50% of the households reported that a member of the household ate a fewer number meals in a day because food was not enough.
Table 1. Socio-demographic characteristics.
| Factor | Control (%) |
Intervention (%) |
Total (%) |
P-value |
|---|---|---|---|---|
| Mother’s age | ||||
| 14–20 | 27.0 | 30.0 | 28.4 | 0.219 |
| 21–24 | 30.7 | 30.9 | 30.8 | |
| 25–29 | 23.6 | 25.2 | 24.3 | |
| 30–45 | 17.5 | 12.4 | 15.1 | |
| Missing | 1.2 | 1.5 | 1.4 | |
| Marital status | ||||
| Not in a union | 15.3 | 17.4 | 16.3 | 0.639 |
| In a union | 84.8 | 82.4 | 83.7 | |
| Missing | 0.0 | 0.2 | 0.1 | |
| Religion | ||||
| Christian | 90.6 | 91.0 | 90.8 | 0.569 |
| Muslim | 7.3 | 4.6 | 6.0 | |
| Missing | 2.1 | 4.4 | 3.2 | |
| Education | ||||
| Less than primary | 19.4 | 16.2 | 17.9 | 0.624 |
| Primary school | 56.2 | 54.0 | 55.1 | |
| Secondary school | 22.2 | 25.6 | 23.8 | |
| Missing | 2.3 | 4.2 | 3.2 | |
| Parity | ||||
| 1 | 36.6 | 41.6 | 39.0 | 0.247 |
| 2 | 30.7 | 31.5 | 31.1 | |
| 3 | 32.8 | 26.9 | 30.0 | |
| Mother’s occupation at baseline | ||||
| Not working | 71.8 | 67.0 | 69.5 | 0.300 |
| Working | 25.8 | 28.8 | 27.3 | |
| Missing | 2.4 | 4.2 | 3.3 | |
| Mother’s occupation at follow-up | ||||
| Not working | 89.8 | 83.8 | 86.9 | 0.097 |
| Working | 7.8 | 14.9 | 11.2 | |
| Missing | 2.4 | 1.3 | 1.9 | |
| Ethnicity of the person | ||||
| Kikuyu | 20.3 | 24.6 | 22.3 | 0.876 |
| Luhya | 15.9 | 13.6 | 14.8 | |
| Luo | 11.4 | 15.5 | 13.4 | |
| Kamba | 16.3 | 15.3 | 15.8 | |
| Other | 14.2 | 13.6 | 13.9 | |
| Missing | 21.8 | 17.6 | 19.8 | |
| Place of delivery | ||||
| Home | 4.0 | 5.3 | 4.6 | 0.295 |
| Health facility | 92.6 | 92.0 | 92.3 | |
| Missing | 3.5 | 2.7 | 3.1 | |
| Wealth index | ||||
| Poorest | 25.0 | 24.4 | 24.7 | 0.820 |
| Middle | 19.2 | 22.1 | 20.6 | |
| Least poor | 20.3 | 25.8 | 22.9 | |
| Missing | 3.5 | 27.7 | 31.8 | |
| Child’s sex | ||||
| Male | 52.2 | 49.6 | 51.0 | 0.135 |
| Female | 46.3 | 49.1 | 47.6 | |
| Missing | 1.6 | 1.3 | 1.5 | |
| n | 577 | 524 | 1101 | |
Table 2. Feeding practices.
| Indicator | Control (%) | Intervention (%) | Total (%) | P-value |
|---|---|---|---|---|
| Introduction of solid, semi-solid or soft foods (6–8 months) (n = 699) | 95.6 | 98.5 | 97.0 | 0.117 |
| Minimum dietary diversity (6–11 months) (n = 737) | 42.9 | 38.9 | 41.0 | 0.600 |
| Timely initiation of breastfeeding (n = 1101) | 83.6 | 84.8 | 84.2 | 0.677 |
| % EBF at 6 months (n = 1101) | 59.7 | 61.2 | 60.4 | 0.863 |
| Children ever breastfed | 100.0 | 99.8 | 99.9 | 0.370 |
| Minimum meal frequency (6–11 months) (n = 785) | 74.0 | 80.7 | 77.2 | 0.057 |
| Minimum acceptable diet (6–11 months) (n = 785) | 26.5 | 27.6 | 27.0 | 0.862 |
EBF, exclusive breastfeeding.
Fig. 1.
Food groups consumed.
Table 3. Household food insecurity access-related conditions.
| Household food insecurity | Control (%) |
Intervention (%) |
Total (%) |
P-value |
|---|---|---|---|---|
| Worry that household would not have enough food | ||||
| Never | 44.1 | 49.2 | 46.5 | 0.489 |
| Rarely | 18.8 | 15.9 | 17.4 | |
| Sometimes | 23.1 | 26.5 | 24.7 | |
| Often | 14.1 | 8.5 | 11.4 | |
| Household member not able to eat preferred food because of a lack of resources | ||||
| Never | 32.2 | 28.6 | 30.5 | 0.652 |
| Rarely | 17.2 | 19.7 | 18.4 | |
| Sometimes | 32.8 | 38.4 | 35.5 | |
| Often | 17.8 | 13.4 | 15.7 | |
| Household member had to eat a limited variety of foods due to lack of resources | ||||
| Never | 37.1 | 33.3 | 35.3 | 0.759 |
| Rarely | 17.2 | 19.7 | 18.4 | |
| Sometimes | 30.7 | 34.1 | 32.3 | |
| Often | 15.0 | 12.9 | 14.0 | |
| Household member ate food that was not preferred because of a lack in resources | ||||
| Never | 32.4 | 29.2 | 30.9 | 0.794 |
| Rarely | 20.5 | 21.2 | 20.8 | |
| Sometimes | 33.2 | 37.3 | 35.2 | |
| Often | 13.9 | 12.3 | 13.1 | |
| Household member ate a smaller meal because there was not enough food | ||||
| Never | 45.5 | 45.1 | 45.3 | 0.892 |
| Rarely | 20.9 | 23.5 | 22.2 | |
| Sometimes | 25.6 | 24.2 | 24.9 | |
| Often | 8.0 | 7.2 | 7.6 | |
| Household member ate fewer numbers of meals/day because food not enough | ||||
| Never | 49.0 | 48.7 | 48.9 | 0.603 |
| Rarely | 20.1 | 25.0 | 22.5 | |
| Sometimes | 22.7 | 21.2 | 22.0 | |
| Often | 8.2 | 5.1 | 6.7 | |
| Past 4 weeks there was ever no food in household because of lack resources | ||||
| Never | 72.5 | 79.2 | 75.7 | 0.365 |
| Rarely | 13.5 | 10.6 | 12.1 | |
| Sometimes | 11.9 | 9.1 | 10.6 | |
| Often | 2.2 | 1.1 | 1.6 | |
| Household member slept hungry because there was not enough food | ||||
| Never | 82.2 | 87.7 | 84.9 | 0.229 |
| Rarely | 9.8 | 8.9 | 9.4 | |
| Sometimes | 6.5 | 2.3 | 4.5 | |
| Often | 1.6 | 1.1 | 1.3 | |
| Past 4 weeks household member go day and night without eating because food not enough | ||||
| Never | 91.0 | 92.4 | 91.7 | 0.657 |
| Rarely | 5.5 | 4.9 | 5.2 | |
| Sometimes | 2.5 | 2.5 | 2.5 | |
| Often | 1.0 | 0.2 | 0.6 | |
| n | 512 | 472 | 984 |
Tables 4–6 summarises findings from regression analysis. Infants living in food secure households were 104% (AOR = 2.04, P=0.019) significantly more likely to be exclusively breastfed up to 6 months of age compared with infants from households that are food insecure (Table 4). Infants living in food secure households were 77% (AOR = 0.23, P=0.013) significantly less likely to be initiated to complementary feeding timely compared with infants from households that are food insecure (Table 5). Infants living in food secure households were 84% (AOR = 1.84, P=0.046) significantly more likely to have a diverse diet compared with infants from households that are food insecure. Infants living in food secure households were 26% (AOR = 1.26, P=0.530) more likely to have high frequency of feeding compared with infants from households that are food insecure but the results were not significant. Infants living in food secure households were 135% (AOR = 2.35, P=0.008) significantly more likely to have minimum acceptance diet compared with infants from food insecure households (Table 6).
Table 4. Unadjusted and adjusted logistic regression for relationship between exclusive breastfeeding at 6 and household food security controlling for other factors.
| Factors | uAOR (95% CI) | P-value | AOR (95% CI) | P-value |
|---|---|---|---|---|
| Food security | ||||
| Food insecure | 1.00 (1.00; 1.00) | 1.00 (1.00; 1.00) | ||
| Food secure | 1.28 (0.87; 1.87) | 0.205 | 2.04 (1.13; 3.71) | 0.019 |
| Sex | ||||
| Male | 1.00 (1.00; 1.00) | 1.00 (1.00; 1.00) | ||
| Female | 0.84 (0.62; 1.12) | 0.236 | 0.69 (0.44; 1.07) | 0.099 |
| Intervention | ||||
| Control | 1.00 (1.00; 1.00) | 1.00 (1.00; 1.00) | ||
| Intervention | 1.02 (0.76; 1.38) | 0.883 | 1.64 (1.04; 2.57) | 0.032 |
| Mothers occupation | ||||
| Not working | 1.00 (1.00; 1.00) | 1.00 (1.00; 1.00) | ||
| Working | 0.69 (0.50; 0.95) | 0.024 | 0.65 (0.39; 1.07) | 0.090 |
| Place of residence | ||||
| Korogocho | 1.00 (1.00; 1.00) | 1.00 (1.00; 1.00) | ||
| Viwandani | 0.37 (0.27; 0.51) | 0.000 | 0.13 (0.06; 0.29) | 0.000 |
uAOR, unadjusted odds ratio; AOR, adjusted odds ratio.
Controlled for socio economic status, marital, mother’s age, religion, education, parity, ethnicity, health facility, birth weight.
Table 6. Unadjusted and adjusted logistic regression for relationship between minimum acceptable diet and household food security controlling for other factors.
| Factors | uAOR (95% CI) | P-value | AOR (95% CI) | P-value |
|---|---|---|---|---|
| Food security | ||||
| Food insecure | 1.00 (1.00; 1.00) | 1.00 (0.00; 0.00) | ||
| Food secure | 1.11 (0.73; 1.68) | 0.626 | 2.35 (1.26; 4.39) | 0.008 |
| Health facility birth | ||||
| No | 1.00 (0.00; 0.00) | 1.00 (0.00; 0.00) | ||
| Yes | 0.63 (0.30; 1.35) | 0.235 | 0.28 (0.07; 1.11) | 0.070 |
| Place of residence | ||||
| Korogocho | 1.00 (0.00; 0.00) | 1.00 (0.00; 0.00) | ||
| Viwandani | 0.84 (0.60; 1.18) | 0.312 | 0.45 (0.22; 0.93) | 0.030 |
uAOR, unadjusted odds ratio; AOR, adjusted odds ratio.
Controlled for sex, birth weight, intervention, socio economic status, marital status, mother age, religion, education, parity, occupation, ethnicity.
Table 5. Unadjusted and adjusted logistic regression for relationship between age of initiation of complimentary feeding and household food security controlling for other factors.
| Factors | uAOR (95% CI) | P-value | AOR (95% CI) | P-value |
|---|---|---|---|---|
| Food security | ||||
| Food insecure | 1.00 (1.00; 1.00) | 1.00 (0.00; 0.00) | ||
| Food secure | 0.62 (0.23; 1.62) | 0.328 | 0.23 (0.07; 0.73) | 0.013 |
| Sex | ||||
| Male | 1.00 (0.00; 0.00) | 1.00 (0.00; 0.00) | ||
| Female | 0.36 (0.14; 0.94) | 0.036 | 0.39 (0.13; 1.13) | 0.084 |
| Place of residence | ||||
| Korogocho | 1.00 (0.00; 0.00) | 1.00 (0.00; 0.00) | ||
| Viwandani | 5.81 (1.93; 17.49) | 0.002 | 5.22 (1.46; 18.68) | 0.011 |
uAOR, unadjusted odds ratio; AOR, adjusted odds ratio.
Controlled for intervention, marital, mother’s age, education, parity, occupation, health facility delivery.
Discussion
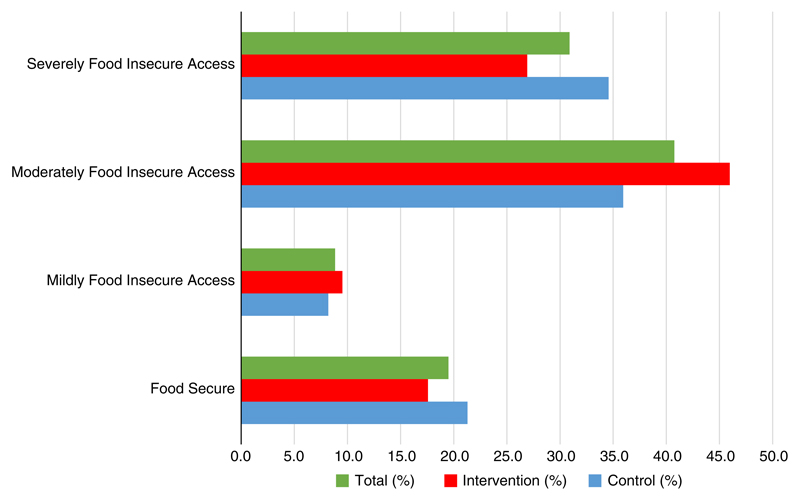
Our study assessed the association between household food security and infant feeding practices in two urban informal settlements in sub-Saharan Africa. The findings confirm that there is high household food insecurity as only 19.5% of the households in the study sample were food secure. The findings are similar to those of other studies conducted in Kenya and elsewhere.21,22,32,33
As a whole, the findings revealed inappropriate feeding practices among the infants living in the limited resource settings. Breastfeeding has many benefits for both the mother and child as it contains all the nutrients an infant needs in the first 6 months of life.34 While the exclusive breastfeeding rate in this study was comparable with the national rate of 61% (KDHS 2014) it implies that 40% of infants were not exclusively breastfed, and hence missed the associated benefits. However, rates have improved after intervention implemented following a study done in the same community by Kimani-Murage et al., in 2011 that reported exclusive breastfeeding rates of 2%.
In terms of complementary feeding, nearly all the children (97%) 6–8 months of age in this study had been introduced to solid, semi-solid or soft foods between 6 and 8 months implying timely introduction of complementary feeding. This rate is relevant because infant needs for energy and micronutrients start to exceed what is provided by breast milk at 6 months.35 and is comparable with the rate of 100% found in a prior study in Korogocho,15 but higher than those reported in Ethiopia and India at 79.7 and 77.5%, respectively.36,37
In the present study, the majority of the children (76.3%) attained the minimum meal frequency; this is similar to findings in informal settlements in Nairobi.15 But <50% of the children achieved minimum dietary diversity, implying that while the majority received meals at the appropriate frequency these were limited in the variety of foods offered. Also, as has been shown in other low resource settings, consumption of animal foods was very low, as <25% of children consumed flesh foods (meat, fish, poultry and liver/organ meats), and only 26.1% consumed eggs. In this respect, our findings were similar to the 2013 study in Korogocho.15 In contrast, the present study found that the majority of children aged 6–11 months (80%) consumed foods made from grains, roots and tubers. The low dietary diversity found may be attributable to the high poverty level and limited income available to purchase foods, as reducing the variety of foods consumed is one of the coping strategies adopted in the face of food insecurity. A study in the same setting on coping strategies among urban poor in 2014 reported that food accounted for 52% of the total spending in households, and that among a variety of coping strategies the one most frequently used was reduction in food consumption.38
The minimum acceptable diet indicator combines standards of dietary diversity and feeding frequency by breastfeeding status and consumption of milk feeds for children who are not breastfed. The indicator provides a useful way to track progress and simultaneously improve the key quality and quantity dimensions of children’s diets. The low percentage of children who achieved the minimum acceptable diet is comparable with the reports of Joshi et al. in rural India, and Korir in Kenya.15,39 Prior studies from Kenya report varying rates; and while the rate in the current study is slightly higher than national rates reported for Kenya (21%),40 it is much lower than that found in the Nairobi informal settlements in 2014 (54.8%).41 One of the factors that may be contributing to inappropriate IYCF practices in these low resource settings is household food security and yet there is paucity of data on the relationship between the two.
This study is one of the few that have investigated how household food security is associated with infant feeding practices. The findings showed an association between infant feeding practices and food security, as infants living in food secure households were significantly more likely to achieve appropriate infant feeding practices than those in food insecure households. Two other studies conducted in rural Bangladesh5,9 and Ghana23 reported similar findings. Saha et al. reported that better household food security status was associated with better infant feeding practices for children 6–12 months of age and Owais et al. that the odds of receiving a minimally acceptable diet for infants in most food secure households was higher than for infants living in least food secure huseholds.The Ghana study also reported that the provision of adequate child diet is threatened at times when there is no food to eat at all.
In conclusion, the present study adds to the body of knowledge on infant feeding that household food security is associated with infant feeding practices in low-income settings. The findings imply that interventions aimed at improving IYCF practices and consequently nutritional status need to take into consideration the issue of food security. This means that interventions to improve child nutritional status in resource-limited settings should consider multidisciplinary approaches engaging nutrition-sensitive interventions to improve household food security (Fig. 2).
Fig. 2.
Household food security status.
Acknowledgements
The authors thank the APHRC Research Staff for their technical support in the design and implementation of the study. They are particularly grateful to Dr Alex Ezeh and Dr Catherine Kyobutungi for their contribution to the study design and Fredrick Wekesah, Milka Wanjohi and Peterrock Muriuki for their contribution to the data collection. The authors would also like to highly thank Prof. Paula Griffiths of Loughborough University, Prof. Nyovani Madise of the University of Southampton and Prof. Rachel Musoke of Nairobi University for their technical support during the design and implementation of the study. They are grateful to the Unit of Nutrition and Dietetics and the Unit of Community Health Services of the Ministry of Health, Kenya, for their guidance in the design of the project and their continued support of the implementation of the project. They would also like to thank UNICEF, Concern World Wide, Makadara and Embakasi sub-County Health Management Teams, the National Maternal Infant and Young Child Nutrition Steering Committee, the Urban Nutrition Working Group, and the Nutrition Information Working Group, among other agencies/NGOs/groups for their contribution to the design and/or implementation of the project. The authors are also highly indebted to the study participants and data collection and management teams.
Financial Support
This study was funded by the Wellcome Trust, Grant # 097146/Z/11/Z. The authors also acknowledge core funding for APHRC from The William and Flora Hewlett Foundation and the Swedish International Cooperation Agency (SIDA); and funding for the NUHDSS from the Bill and Melinda Gates Foundation.
Footnotes
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the Kenya Medical Research Institute Ethics Review Committee reference number KEMRI/RES/7/3/1.
References
- 1.United Nations Standing Committee on Nutrition. United Nations Standing Committee on Nutrition (SACN) Sixth report on the world nutrition situation: progress in nutrition. 2010 Retrieved 4 August 2015 from https://www.unscn.org/files/Publications/RWNS6/report/SCN_report.pdf.
- 2.National Bureau of Statistics-Kenya, ICF International 2014. KDHS key findings. Rockville, Maryland, USA: KNBS and ICF International; 2015. Retrieved 11 August 2015 from https://www.dhsprogram.com/pubs/pdf/SR227/SR227.pdf. [Google Scholar]
- 3.Olack B, Burke H, Cosmas L, et al. Nutritional status of under-five children living in an informal urban settlement in Nairobi, Kenya. J Health Popul Nutr. 2011;29:357. doi: 10.3329/jhpn.v29i4.8451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kimani-Murage E, Muthuri SK, Oti SO, et al. Evidence of a double burden of malnutrition in urban poor settings in Nairobi, Kenya. PLoS One. 2015;10 doi: 10.1371/journal.pone.0129943. Retrieved 11 August 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saha KK, Frongillo EA, Alam DS, et al. Household food security is associated with infant feeding practices in rural Bangladesh. J Nutr. 2008;138:1383–1390. doi: 10.1093/jn/138.7.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mberu BU, Haregu TN, Kyobutungi C, Ezeh AC. Health and health-related indicators in slum, rural, and urbancommunities: a comparative analysis. Glob Health Action. 2016;9:33163. doi: 10.3402/gha.v9.33163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kramer MS, Kakuma R. The Optimal Duration of Exclusive Breastfeeding. In: Pickering LK, Morrow AL, Ruiz-Palacios GM, Schanler RJ, editors. Protecting Infants through Human Milk. Advances in Experimental Medicine and Biology. Springer; Boston, MA: 2004. [Google Scholar]
- 8.Onyango AW, Esrey SA, Kramer MS. Continued breastfeeding and child growth in the second year of life: a prospective cohort study in western Kenya. Lancet. 1999;354:2041–2045. doi: 10.1016/S0140-6736(99)02168-6. [DOI] [PubMed] [Google Scholar]
- 9.Owais A, Kleinbaum D, Suchdev P, et al. Household food security and infant feeding practices in rural Bangladesh (378.1) FASEB J. 2014;28(Suppl. 1):378–381. doi: 10.1017/S1368980015003195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO. Nutrition – WHO|Regional Office for Africa. 2015 Retrieved 13 August 2015 from http://www.afro.who.int/en/clusters-a-programmes/hpr/food-safety-and-nutrition-fan/programme-components/nutrition.html.
- 11.Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet (London, England) 2013;382:427–451. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 12.WHO. Indicators for assessing infant and young child feeding practices: conclusions of a consensus meeting held 6–8 November 2007. 2007 Retrieved 27 July 2016 from http://apps.who.int/iris/bitstream/10665/43895/1/9789241596664_eng.pdf.
- 13.Kenya National Bureau of Statistics, Ministry of Health, National AIDS Control Council, Kenya Medical Research Institute, National Council for Population and Development. Kenya demographic and health survey: key indicators report 2014. 2015 Retrieved 11 August 2015 from http://dhsprogram.com/pubs/pdf/PR55/PR55.pdf.
- 14.Fotso JC, Madise N, Baschieri A, et al. Child growth in urban deprived settings: Does household poverty status matter? At which stage of child development? Health Place. 2012;18:375–384. doi: 10.1016/j.healthplace.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Korir JK. Determinants of complementary feeding practices and nutritional status of children 6–23 months old in Korogocho slum, Nairobi County, Kenya. 2013 Retrieved 11 August 2015 from http://etd-library.ku.ac.ke/handle/123456789/9419.
- 16.Kimani-Murage E, Madise NJ, Fotso J-C, et al. Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi Kenya. BMC Public Health. 2011;11:396. doi: 10.1186/1471-2458-11-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kimani-Murage E, Wekesah F, Wanjohi M, et al. Factors affecting actualisation of the WHO breastfeeding recommendations in urban poor settings in Kenya: breastfeeding challenges in urban poor settings. Matern Child Nutr. 2014;11:314–332. doi: 10.1111/mcn.12161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ochola SA. Evaluation of two counseling strategies improving exclusive breastfeeding among HIV-negative mothers in Kibera Slum, Nairobi, Kenya : a randomized controlled trial. Stellenbosch: Stellenbosch University; 2008. [Internet]. Retrieved 1 November 2017 from http://scholar.sun.ac.za/handle/10019.1/1460. [Google Scholar]
- 19.FAO, WFP, IFAD. The State of Food Insecurity in the World. FAO; ROME: 2012. [Google Scholar]
- 20.Agricultural Sector Coordination Unit (ASCU) National Food and Nutrition security policy. Agricultural Sector Coordination Unit (ASCU); Nairobi: 2011. [Google Scholar]
- 21.Faye O, Baschieri A, Falkingham J, Muindi K. Hunger and food insecurity in Nairobi’s slums: an assessment using IRT models. J Urban Heal. 2011;88:235–255. doi: 10.1007/s11524-010-9521-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kimani-Murage E, Schofield L, Wekesah F, et al. Vulnerability to food insecurity in urban slums: experiences from Nairobi, Kenya. J Urban Heal. 2014;91:1098–1113. doi: 10.1007/s11524-014-9894-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agbadi P, Urke HB, Mittelmark MB. Household food security and adequacy of child diet in the food insecure region north in Ghana. PLoS One. 2017;12:e0177377. doi: 10.1371/journal.pone.0177377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garvelink W, Wedding K. Nutrition and food security in the city|Center for Strategic and International Studies. 2013 Retrieved 2 August 2015 from http://csis.org/publication/nutrition-and-food-security-city.
- 25.Lamba D. The forgotten half; environmental health in Nairobi’s poverty areas. Environ Urban. 1994;6:164–173. [Google Scholar]
- 26.African Population and Health Research Center. Population and Health Dynamics in Nairobi’s Informal Settlements: report of the Nairobi cross-sectional slums survey (NCSS) 2012. APHRC; 2014. [Google Scholar]
- 27.African Population and Health Research Center. Population and health dynamics in Nairobi’s informal settlements: report of the Nairobi cross-sectional slums survey (NCSS) 2000. 2002 Retrieved 4 October 2017 from http://aphrc.org/wp-content/uploads/2014/08/Population-and-Health-Dynamics-in-Nairobi%E2%80%99s-Informal-Settlements.pdf.
- 28.Kimani-Murage E, Kyobutungi C, Ezeh AC, et al. Effectiveness of personalised, home-based nutritional counselling on infant feeding practices, morbidity and nutritional outcomes among infants in Nairobi slums: study protocol for a cluster randomised controlled trial. Trials. 2013;14:445. doi: 10.1186/1745-6215-14-445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beguy D, Elung’ata P, Mberu B, et al. Health & demographic surveillance system profile: the Nairobi Urban Health and Demographic Surveillance System (NUHDSS) Int J Epidemiol. 2015;44:462–471. doi: 10.1093/ije/dyu251. [DOI] [PubMed] [Google Scholar]
- 30.Emina J, Beguy D, Zulu EM, et al. Monitoring of health and demographic outcomes in poor urban settlements: evidence from the nairobi urban health and demographic surveillance system. J Urban Health. 2011;88(Suppl. 2):200–218. doi: 10.1007/s11524-011-9594-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide. Food Nutr Tech Assist Proj Acad Educ Dev. 2007 http://www.fao.org/fileadmin/user_upload/eufao-fsi4dm/doc-training/hfias.pdf. [Google Scholar]
- 32.Agarwal S, Sethi V, Gupta P, et al. Experiential household food insecurity in an urban underserved slum of North India. Food Secur. 2009;1:239–250. [Google Scholar]
- 33.Maitra C, Rao DP. Poverty–food security Nexus: evidence from a survey of urban slum dwellers in Kolkata. World Dev. 2015;72:308–325. [Google Scholar]
- 34.WHO. WHO|Early Initiation of Breastfeeding. WHO; 2016. Retrieved 22 November 2016 from http://www.who.int/elena/titles/early_breastfeeding/en/. [Google Scholar]
- 35.WHO. Indicators for assessing infant and young child feeding practices. Young. 2007;2007:1–19. [Google Scholar]
- 36.Ergib M, Ashenafi S, Semaw F, Fisaha H. Magnitude and factors associated with appropriate complementary feeding among mothers having children 6-23 months-of-age in Northern Ethiopia; A Community-Based Cross-Sectional Study. Journal of Food and Nutrition Sciences. 2014;2:36–42. [Google Scholar]
- 37.Rao S, Swathi P, Unnikrishnan B, Hegde A. Study of complementary feeding practices among mothers of children aged six months to two years – a study from coastal south India. The Australasian Medical Journal. 2011;4:252–257. doi: 10.4066/AMJ.2011.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amendah DD, Buigut S, Mohamed S. Coping strategies among urban poor: evidence from Nairobi, Kenya. PLoS One. 2014;9:e83428. doi: 10.1371/journal.pone.0083428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Joshi N, Agho KE, Dibley MJ, Senarath U, Tiwari K. Determinants of inappropriate complementary feeding practices in young children in Nepal: secondary data analysis of Demographic and Health Survey 2006. Matern Child Nutr. 2012;8(Suppl. 1):45–59. doi: 10.1111/j.1740-8709.2011.00384.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kenya National Bureau of Statistics (KNBS); ICF Macro. Kenya Demographic and Health Survey 2014. Heal (San Francisco) 2014. pp. 1–314. [Google Scholar]
- 41.Concern Worldwide Kenya. Integrated health and nutrition baseline survey in the Nairobi slums Nairobi County. 2014 Retrieved 15 May 2017 from http://www.nutritionhealth.or.ke/wp-content/uploads/Downloads/Nairobi Slums MNCH KPC Final Report.pdf.