Abstract
It is well known that lead (Pb) produces reduced haemoglobin (Hb) levels and risk of anemia when blood lead levels (BPb) are greater than 20 µg dL−1. Two recent studies reported an increased risk of anemia in children with BPb between 10–20 µg dL−1, but few studies examined the association between Hb levels or risk of anemia and BPb under 10 µg dL−1. In the present study this association was examined using data of 140 preschool children from a larger prospective cohort study in China. Data showed that compared to children with BPb <5 µg dL−1, children with BPb between 7.5–10 µg dL−1 had significantly lower Hb levels, but there were no marked differences for other groups. A linear regression model showed a negative relationship between BPb and Hb levels after controlling for age, gender, height, weight, and iron (Fe) deficiency. This finding, although limited by a small sample size, suggests it may be important to examine Pb-induced hemosynthesis effect at concentrations less than 10 µg dL−1.
Keywords: anemia, blood lead levels, children, China, hemoglobin, preschool
Introduction
High lead (Pb) exposure levels produce a variety of adverse health effects including hematologic toxicity. Children are particularly vulnerable to environmental toxins such as Pb. Anemia has primarily been found in children, especially those living in or near Pb-contaminated areas, with a blood lead level (BPb) greater than 40 µg dL−1 (Agency for Toxic Substances and Disease Registry 2007). Schwartz et al. (1990) reported a dose–response relationship between BPb close to 25 µg dL−1 and anemia in children, and even more recently, a lower BPb range of 10–19.9 µg dL−1 was associated with severe anemia in Indian children under 3 years of age (Jain et al. 2005). This finding was then replicated in a study of Pakistan children (Shah et al. 2010), and together these studies indicated that Pb may affect hemosynthesis when BPb is below 20 µg dL−1. No apparent studies have yet examined the association between haemoglobin (Hb) levels or risk of anemia in children and BPb below 10 µg dL−1, the concern level recommended by the Center for Disease Control and Prevention (CDC). This study examined the association between BPb and Hb levels in preschool children.
Methods
Study participants
Children included in this analysis were those with both Hb and BPb data in the China Jintan Chid Cohort Study (Liu et al. 2010). This is a prospective cohort study of environmental, nutritional, and child development. Institutional review board approval was obtained from the University of Pennsylvania and the ethical committee for research at Jintan Hospital in Jintan, China. Children and parents in four preschools were invited to participate. After signing a consent form, each parent completed a baseline questionnaire about family and child characteristics.
Blood lead and hemoglobin levels
Blood was collected in lead-free tubes. BPb were measured using a graphite furnace atomic absorption spectrophotometer (instrument AA100 – Perkin-Elmer Company) and categorized as ≥ 10, 7.5–10, 5–7.5 and < 5 µg dL−1. Blood Hb concentration was measured by the 7–22 photoelectric colorimeter. According to the World Health Organization’s criteria, anemia was defined as Hb < 11 µg dL−1. Serum nutrient levels including iron (Fe) were also determined and Fe deficiency was defined as serum Fe level less than 7.5 umol.
Statistical analysis
Hemoglobin concentrations were compared using one-way analysis of variance. The association between BPb (dependent variable) and Hb (independent variable) was also examined in a linear regression model, controlling for age, gender, height, weight, and Fe deficiency. No other potential confounders were adjusted due to small sample size. All analysis was undertaken in SAS 9.2 (SAS Institute, Cary, NC). The criterion for significance was set at p < 0.05
Results
Of 140 children, more than a half were boys, and most of them are at age of 3. BPb ranged from 1.9 to 11.4 µg dL−1, with a median of 4.3 µg dL−1. Thirty-five percent children had BPb > 5 µg dL−1 (3% had BPb ≥ 10 µg dL−1 and 32% had BPb between 5–10 µg dL−1). Mean Hb concentration was 12.7 µg dL−1 (standard deviation = 0.9 µg dL−1). Three (2%) children had anemia and all of them had Fe deficiency.
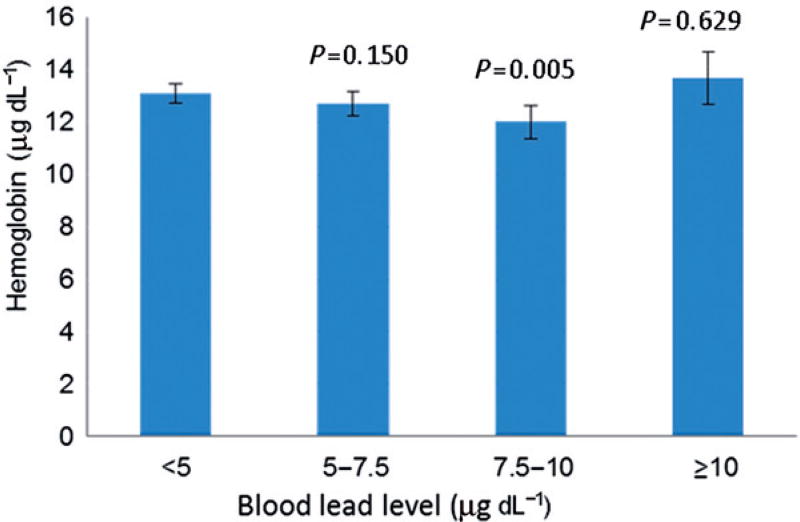
Children with BPb between 5–10 µg dL−1 had significantly higher Hb concentration than those with BPb < 5 µg dL−1 (12.5 ± 0.8 vs. 13.1 ± 0.9). Further comparisons found that a statistically significant difference existed only between children with BPb between 7.5–10 µg dL−1 (hemoglobin = 12. ± 0.5 µg dL−1) and those with lowest BPb (Figure 1). No marked differences were observed between > 10 µg dL−1 group and other groups, which may be due to small sample size. Regression analysis showed a reverse linear relationship between BPb and Hb (coefficient = −0.096, R2 = 0.08, p = 0.025) after controlling for age, gender, height, weight, and Fe deficiency (Table 1). When restricting children with BPb under 10 µg dL−1, the association became stronger, with a regression coefficient of −0.174 (p = 0.000, R2 = 0.136).
Figure 1.
Hemoglobin concentrations by blood lead level.
Notes: p values are derived from the comparisons between < 5 µg dL−1 group and other groups in one-was analysis of variance. Bars show 95% confidence intervals.
Table 1.
Linear regression of hemoglobin levels in 140 children.
| Independent variable | Coefficient | 95% CI | P value |
|---|---|---|---|
| BPb (µg dL−1) | −0.096 | −0.179–0.012 | 0.025 |
| Gender (boy vs. girl) | 0.147 | −0.153–0.448 | 0.333 |
| Age (months) | 0.446 | −0.213–1.106 | 0.182 |
| Height (cm) | 0.009 | −0.063–0.065 | 0.979 |
| Weight (kg) | 0.065 | −0.071–0.200 | 0.347 |
| Iron deficiency (yes vs. no) | −0.252 | −0.579–0.070 | 0.130 |
Notes: R2 = 0.08
Discussion
Centers for Disease Control recommended 10 µg dL−1 as a concern level for adverse health effects of Pb exposures, but a cumulative number of studies suggested that adverse health effects exist in children at BPb less than 10 µg dL−1 and even less than 5 µg dL−1 (Bellinger 2008; Lanphear et al. 2005). It is commonly agreed that there is no apparent threshold for Pb toxicity, especially for neurodevelopmental toxicity. Even with a small sample size, this pilot analysis still found that increasing BPb under the current CDC recommended limit, particularly above 7.5 µg dL−1, was associated with decreasing Hb levels, independent of Fe deficiency and other potential confounders.
Lead is known to produce anemia by inhibiting activities of hemosynthetic enzymes, particularly δ-aminolevulinic acid dehydratase (ALAD), and shortening the erythrocyte lifespan. Decreased Hb and anemia were reported among Pb-exposed workers and children living in or near Pb-polluted areas (Agency for Toxic Substances and Disease Registry 2007). More recently studies (Jain et al. 2005; Shah et al. 2010) demonstrated that Pb might produce anemia in children at levels previously thought safe, between 10–19 µg dL−1. ALAD activity inhibition can occur with BPb less than 10 µg dL−1 (Agency for Toxic Substances and Disease Registry 2007), but there were no studies examining the association between BPb under this limit and Hb levels for risk of anemia. This study showed a trend of decreasing Hb levels with increasing BPb under 10 µg dL−1, although sample size was not sufficient to examine the association between BPb and anemia. Data suggest that Pb interferes with hemosynthsis even at levels below 10 µg dL−1. However, due to small sample size and uncontrolled factors related to anemia in this study, larger studies are warranted.
Acknowledgments
Funding was provided by the National Institute of Environment Health Sciences (NIEHS, K01-ES015 877; R01-ES018858) US; The Wacker Foundation US; Jintan City Government; Jintan Hospital, China. Thanks are extended to the participating children and their families from Jintan City, and to the Jintan Cohort Study Group (Yuexian Ai, Liudi Han, Aoda Liu, and Liping Zhang). We are very grateful to the Jintan city government and the Jintan Hospital for their support and assistance.
References
- Agency for Toxic Substances and Disease Registry. Toxciological profile for lead. Atlanta, GA: US Department of Health and Human Services, Public Health Service, Agency for Toxic Substances and Disease Registry; 2007. [Google Scholar]
- Bellinger DC. Very low lead exposures and children’s neurodevelopment. Current Opinion in Pediatrics. 2008;20:172–7. doi: 10.1097/MOP.0b013e3282f4f97b. [DOI] [PubMed] [Google Scholar]
- Jain NB, Francine L, Guller U, Shankar A, Kazani S, Garshick E. Relation between blood lead levels and childhood anemia in India. American Journal of Epidemiol. 2005;161:968–73. doi: 10.1093/aje/kwi126. [DOI] [PubMed] [Google Scholar]
- Lanphear BP, Hornung R, Khoury J, Yolton K, Baghurst P, Bellinger DC, Canfield RL, et al. Low-level environmental lead exposure and children’s intellectual function: An international pooled analysis. Environmental Health Perspectives. 2005;113:894–9. doi: 10.1289/ehp.7688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, McCauley LA, Zhao Y, Zhang H, Pinto-Martin J. Cohort profile: The China Jintan child cohort study. International Journal of Epidemiology. 2010;39:668–74. doi: 10.1093/ije/dyp205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J, Landrigan PJ, Baker EL, Orenstein W, Von Lindern IH. Lead-induced anemia: Dose-response relationships and evidence for a threshold. American Journal of Public Health. 1990;80:165–8. doi: 10.2105/ajph.80.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah F, Kazi TG, Afridi HI, Baig JA, Khan S, Kolachi NF. Environmental exposure of lead and iron deficit anemia in children age ranged 1–5 years: A cross sectional study. Science Total Environment. 2010;408:5325–30. doi: 10.1016/j.scitotenv.2010.07.091. [DOI] [PubMed] [Google Scholar]