Practical Implications
Our observation confirms the critical role of the left prerolandic region in causing foreign accent syndrome (FAS) and supports the idea that FAS can be considered a syndrome due to heterogeneous etiologies.
Foreign accent syndrome (FAS) is a speech disorder that leads listeners to perceive the patient as having a foreign accent. The cardinal feature of FAS is prosody change, with variation in accent, intonation, and rhythm. Less frequently, phonetic changes with normal prosody may be detected. The composite features of patients with FAS are not characteristic of dysarthria or aphasia and partially resemble patients who have speech apraxia. Patients with FAS are often unfamiliar with the foreign language and often seem unaware of the disturbance, even though their ability to discriminate foreign accents is spared.
FAS is uncommon and seems to be ubiquitous and independent from linguistic differences, having been found across American, European, and Asiatic languages.1 After the first description by Pierre-Marie in 1907, no more than 60 patients with FAS have been described, usually related to stroke or head trauma.1 FAS often emerges during the recovery process from more severe speech disorders (mutism, aphemia, apraxia of speech, dysarthria) or nonfluent aphasias, but it may also occur as an isolated disorder without concomitant language impairment. Furthermore, FAS has been occasionally described in multiple sclerosis (MS),2 primary progressive aphasia,3 and as a developmental motor speech disorder.4 Concerning the site of lesion, the role of left prerolandic regions has been emphasized, but not all reported cases show evidence of cerebral damage, suggesting the possibility of a psychogenic nature for some patients5; in fact, the phenomenon has also been observed in psychiatric patients.6
We present a patient who developed FAS after orthotopic liver transplantation (OLT) followed by cyclosporine-induced acute encephalopathy. Speech disorders, such as mutism and speech apraxia, are occasionally seen in liver transplant patients due to immunosuppressive toxicity,7 but we are not aware of FAS previously observed in these patients.
Case history
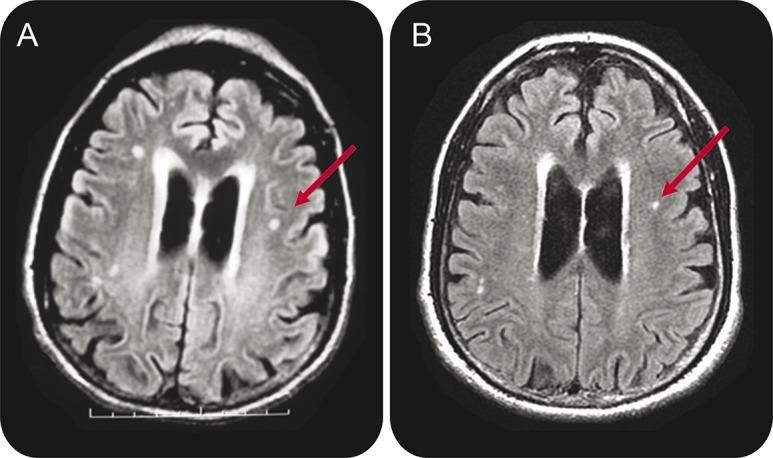
In 2003, a 59-year-old right-handed Italian man developed cyclosporine-induced mutism 1 week after OLT. Cerebral MRI showed multiple hyperintensities on T2 fluid-attenuated inversion recovery sequences in subcortical, periventricular, and semioval centers' white matter, in particular a circumscribed lesion in the left prerolandic white matter (figure, A). Two weeks after the onset of symptoms and after shifting immunosuppression to tacrolimus, the patient partially regained speech with residual dysprosody and speech apraxia, which improved with logotherapy.
Brain MRI
Figure. (A) 2003, (B) 2012. Red arrows point to the T2 fluid-attenuated inversion recovery hyperintense lesion sustaining foreign accent syndrome.
On a recent clinical examination (March 2012), the patient was cognitively and neurologically normal apart from the speech disorder. He showed dysprosody, anomalous phonetic features, and speech sound errors. In particular, his prosody was characterized by a foreign accent with German intonation, despite the fact that Italian was his native language (see the video at http://cp.neurology.org/lookup/doi/10.1212/CPJ.0000000000000145). He seemed aware of but surprised by his “new” accent. The patient is able to speak English but not German and he does not have any particular connection with German people or culture. There was no evidence of aphasia: his speech was fluent without semantic or phonemic errors or difficulty with word finding, comprehension, or naming. Writing and reading were normal. Cerebral MRI in May 2012 showed the reduction of the previously found white matter abnormalities, with unchanged left prerolandic hyperintensity (figure, B).
DISCUSSION
We report a case of FAS secondary to posttransplant cyclosporine encephalopathy. This patient is presumed to have developed FAS as a sequela of cyclosporine neurotoxicity, presenting acutely with mutism a few days after liver transplantation and developing a prosody alteration characterized by a German intonation still present 9 years after OLT.
In previously reported lesional cases of FAS due to vascular, traumatic, or demyelinating damage, the role of left prerolandic regions has been emphasized; cases with left midbrain, right hemisphere, and cerebellar damage have also been reported. It is reasonable to argue that a single cortical area is not solely responsible for causing FAS, which seems related to a dysfunction of a complex motor speech network involving multiple areas rather than to a muscular cause due to a lesion affecting the motor movement of the mouth and/or face.
In our case, MRI demonstrated that the disorder was likely produced by a cyclosporine-induced demyelinating lesion affecting left frontal subcortical white matter, similar to those seen in FAS patients with MS. Our observation confirms the critical role of the left prerolandic region in causing FAS, damaging the frontal cerebral pathways mediating motor speech planning and prosody timing, and supports the idea that FAS can be considered a syndrome due to heterogeneous etiologies.
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
The authors report no disclosures. Full disclosure form information provided by the authors is available with the full text of this article at http://cp.neurology.org/lookup/doi/10.1212/CPJ.0000000000000145.
Supplementary Material
Correspondence to: andrea.stracciari@aosp.bo.it
Funding information and disclosures are provided at the end of the article. Full disclosure form information provided by the authors is available with the full text of this article at http://cp.neurology.org/lookup/doi/10.1212/CPJ.0000000000000145.
Footnotes
Supplemental data at http://cp.neurology.org/lookup/doi/10.1212/CPJ.0000000000000145
Correspondence to: andrea.stracciari@aosp.bo.it
Funding information and disclosures are provided at the end of the article. Full disclosure form information provided by the authors is available with the full text of this article at http://cp.neurology.org/lookup/doi/10.1212/CPJ.0000000000000145.
REFERENCES
- 1.Moen I. Foreign accent syndrome: a review of contemporary explanations. Aphasiology. 2000;14:5–15. [Google Scholar]
- 2.Chanson JB, Kremer S, Blanc F, Marescaux C, Namer IJ, de Seze J. Foreign accent syndrome as a first sign of multiple sclerosis. Mult Scler. 2009;15:1123–1125. doi: 10.1177/1352458509106611. [DOI] [PubMed] [Google Scholar]
- 3.Luzzi S, Viticchi G, Piccirilli M. Foreign accent syndrome as the initial sign of primary progressive aphasia. J Neurol Neurosurg Psychiatry. 2008;79:79–81. doi: 10.1136/jnnp.2006.113365. [DOI] [PubMed] [Google Scholar]
- 4.Marien P, Verhoeven J, Wackenier P, Engelborghs S, De Deyn PP. Foreign accent syndrome as a developmental motor speech disorder. Cortex. 2009;45:870–879. doi: 10.1016/j.cortex.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 5.Van Borsel J, Janssens L, Santens P. Foreign accent syndrome: an organic disorder? J Commun Disord. 2005;38:421–429. doi: 10.1016/j.jcomdis.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Reeves RR, Burke RS, Parker JD. Characteristics of psychotic patients with foreign accent syndrome. J Neuropsychiatry Clin Neurosci. 2007;19:70–76. doi: 10.1176/jnp.2007.19.1.70. [DOI] [PubMed] [Google Scholar]
- 7.Guarino M, Stracciari A. Neuropsychiatric complications of liver transplantation. Met Brain Dis. 2001;16:3–11. doi: 10.1023/a:1011698526025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


