Abstract
Background and Objectives:
Ventral hernia repair is one of the most commonly performed general surgery procedures, and minimally invasive approaches are increasingly preferred. The physiologic repair offered by the preperitoneal approach is favorable, with reduced complications, but it remains a technical challenge. The robotic platform allows for enhanced instrument flexibility and ease of operation. We conducted a retrospective review of our experience with robotic transabdominal preperitoneal repair (rTAPP) versus robotic intraperitoneal onlay mesh (rIPOM) at a tertiary care hospital in an urban setting.
Methods:
We reviewed the records of patients undergoing minimally invasive ventral hernia repair from March 2014 through March 2017. Demographics, complication rates, and operative time were compared by t test and Chi square test, as applicable.
Results:
Sixty-three patients met the criteria for inclusion in the study. Of those, 27 underwent ventral hernia repair with rIPOM and 36 with rTAPP, with no major intraoperative complications. There were no significant differences in demographics between the 2 groups in age, BMI, and sex. The difference in mean operative time was not significant (rIPOM 167.26 [SD 51.76] minutes vs rTAPP 158.84 minutes [SD 61.5]; P = .57), whereas mean console time was significantly different (rIPOM 70.88 minutes [SD 32.88] vs rTAPP 90.26 [SD 31.17]; P = .018). Postoperative complications occurred only with rIPOM and included urinary retention, seroma, and fever.
Conclusions:
rTAPP is a promising alternative to rIPOM, with reduced complications without adding significant operative time, and may allow for reduced costs.
Keywords: Intraperitoneal onlay mesh repair, Robotic ventral hernia repair, transabdominal preperitoneal hernia repair
INTRODUCTION
More than 350,000 ventral hernias are repaired annually in the United States.1 Hernia repair has progressed significantly with advances in the approach as well as the underlying principles for repair.2 For more than 25 years, laparoscopic ventral hernia repair has been used increasingly, with improved mesh overlap and lessening of postoperative complications.3 In addition, the principles regarding mesh placement are evolving and encompass findings from the repair of both inguinal and ventral hernias. The robotic intraperitoneal onlay mesh (rIPOM) procedure involves affixing the mesh to the anterior abdominal wall from inside the abdominal cavity. Although widely performed, rIPOM raises concerns about increased adhesion and seroma formation and recurrence of the hernia.4–6 To address these concerns, robotic transabdominal preperitoneal (rTAPP) creates peritoneal flaps, which allows the preperitoneal placement of the mesh and closure of the peritoneal defect over the mesh.7
The widespread adoption of preperitoneal laparoscopic ventral hernia repair has been limited by its technical difficulty, which requires maneuvers to manipulate the abdominal wall.8 Since its introduction in 2000, the robotic platform has seen improvements in ergonomics that allow easier articulation of the instruments, as opposed to the traditional laparoscopic approach. With the robotic platform, preperitoneal placement of mesh in ventral hernia repair can be performed with ease.7 The vital components of the procedure aided by the robotic platform are the creation of the preperitoneal space, the option for closure of the primary defect, and closure of the peritoneum with running sutures. rIPOM with primary closure has been associated with a reduction in recurrence and is reproducible.9–11 rTAPP may allow further improvement in this technique, with preperitoneal placement of the mesh for smaller defects and retromuscular placement for larger defects.
Current series of rTAPP ventral hernia repairs are limited by the size of patient samples. In April 2015, the technique was introduced at our institution. We report our growing experience with this procedure in a tertiary center in an urban setting.
METHODS
After institutional review board approval, a retrospective chart review identifying patients who underwent minimally invasive repair of ventral hernia was performed from March 2013 through March 2017. A total of 92 patients were identified as having ventral hernia repair. Of those, 63 were identified as undergoing rIPOM or rTAPP. Inclusion criteria were defined as patients who had undergone rIPOM or rTAPP and were followed up for 30 days after surgery. All patients were seen in the clinic, where they underwent medical optimization before the surgery. The same surgeon who assessed the patient in the clinic before the operation performed all the surgeries. Our previous approach to rTAPP and rIPOM—a double-docking method—is described in Sugiyama et al.7 We subsequently added a single-docking method, which we briefly describe below:
Step 1: the operating table is rotated left side down before the robot is docked, and the robot is docked on the patient's left side.
Step 2: after adhesiolysis is performed, blunt dissection of the peritoneal plane starts ∼5 cm from the edges of the hernia defect, ipsilateral to the ports. The peritoneal flap is created in a superior-to-inferior fashion.
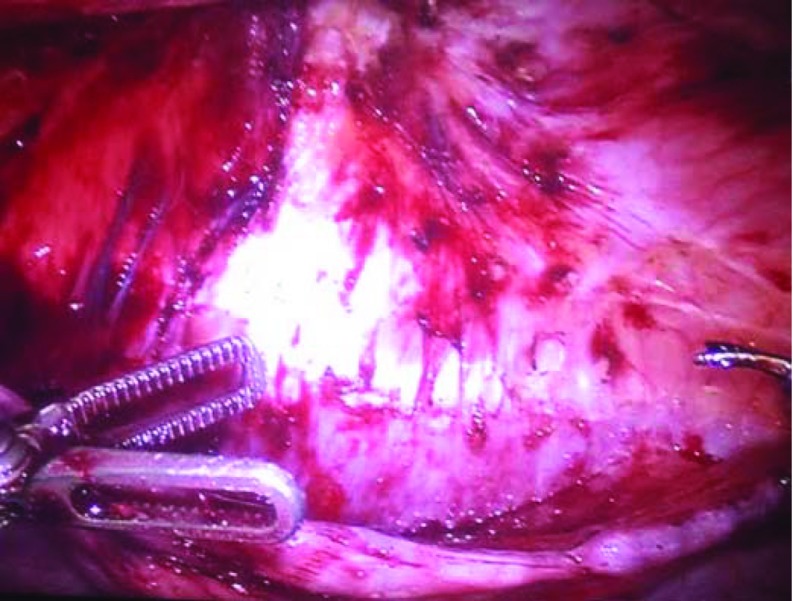
Step 3: once a large peritoneal flap is created, the hernia defect is closed with running V-Loc sutures (Medtronics, Minneapolis Minnesota, USA) (Figure 1).
Figure 1.
Dissection of peritoneal flap after reduction of the hernia sac.
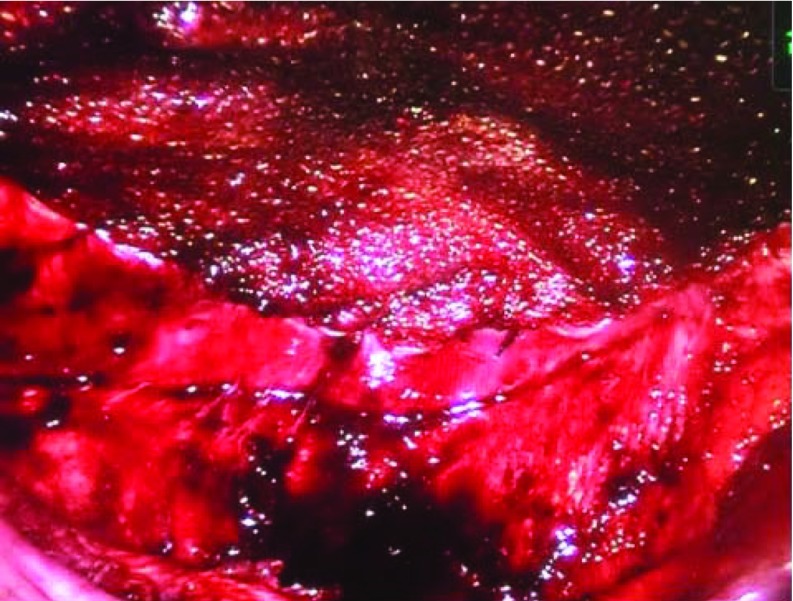
Step 4: a polypropylene mesh is placed in the preperitoneal space (Figure 2).
Figure 2.
Preperitoneal placement of the mesh.
Step 5: the mesh is circumferentially secured to the posterior sheath with running V-Loc sutures.
Step 6: the peritoneal flaps are closed to cover the mesh completely (Figure 3).
Figure 3.
Closure of the peritoneum over the mesh.
Cumulative operative and console times were recorded for each procedure. Only patients who came to the clinic for follow-up 30 days after the surgery were included in the study. Postoperative outcome variables were hernia recurrence, hematoma or seroma, urinary retention, and fever. Outcomes were analyzed by Fisher's exact test. Preoperative factors are listed in Table 1 and were also analyzed with Fisher's exact test. Results were considered statistically significant at P < .05. The age, BMI, and ASA score of each patient were included in the perioperative data collected during the procedure. Quantitative continuous operative risk variables were operative and console times. Results were analyzed with Student's t test. Categorical variables included ASA score, which was analyzed with the Chi square test.
Table 1.
Characteristics of Patients Undergoing Robotic Ventral Hernia Repair
| Characteristics* | Robotic IPOM (n = 27) | Robotic TAPP (n = 36) | P |
|---|---|---|---|
| Age, mean years (SD) | 45.6 (13.1) | 44.3 (13.3) | .71 |
| Sex | |||
| Male | 5 (18.6) | 12 (33.3) | .25 |
| Female | 22 (81.4) | 24 (66.7) | |
| BMI, mean kg/m2 (SD) | 31.8 (9.6) | 31.0 (6.4) | .75 |
| Race | |||
| Black | 21 (77.8) | 31 (86.1) | |
| White | 2 (7.4) | 0 | |
| Hispanic | 3 (11.1) | 5 (13.9) | |
| Other | 1 (3.7) | 0 | |
| Discharged to home | 19 (70.3) | 27 (75.0) | .68 |
| Preoperative risk factors, % | |||
| Smoking | 13.4 | 19.8 | .16 |
| Alcohol use | 13.9 | 21.9 | .088 |
| Drug abuse | 1.6 | 5.2 | .083 |
| Diabetes mellitus | 21.1 | 23.4 | .65 |
| Coronary artery disease | 6.8 | 5.3 | .61 |
| Hypertension | 46.0 | 30.9 | .015 |
| Hyperlipidemia | 16.0 | 12.8 | .48 |
| Asthma | 12.2 | 14.9 | .52 |
| Chronic obstructive pulmonary disease | 2.6 | 0.0 | .11 |
| Chronic kidney disease | 2.6 | 3.2 | .79 |
| End stage renal disease | 1.1 | 3.2 | .20 |
| Hepatitis C | 0.5 | 0.0 | .48 |
| HIV | 0.5 | 1.1 | .61 |
| Hernia size, mean cm (SD) | 3.40 (1.51) | 3.98 (2.61) | .32 |
| Open conversion, % | 0 | 0 | — |
| 30-day readmission, % | 3.7 | 4.2 | .83 |
Unless otherwise specified, data are expressed as number of patients (percentage of patients in total group).
*Missing data are not included in calculations.
RESULTS
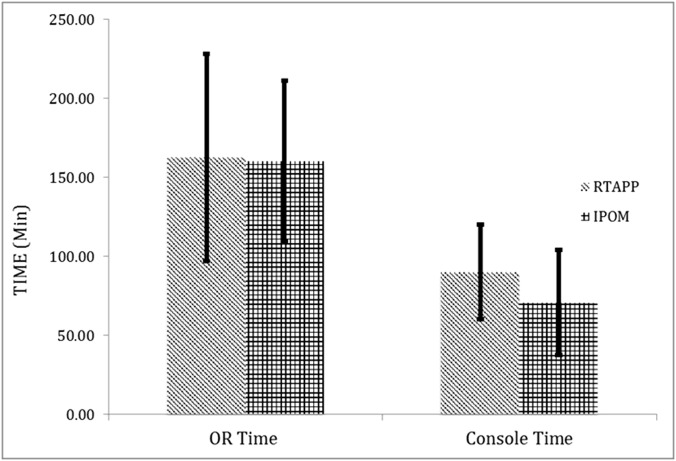
Sixty-three patients met the inclusion criteria. Of those, 36 (57.1%) underwent rTAPP and 27 (42.9%) underwent rIPOM. Hernia size was measured as the largest diameter of solo ventral hernias. Swiss cheese defects were not included in the calculation. The mean hernia size was 3.40 cm (SD 1.54) for rIPOM versus 3.98 cm (SD 2.61) for rTAPP (P = .32). There were no major intraoperative complications or conversions to open surgery. The mean operative time for rTAPP was 158.84 min (SD 61.5) versus 167.26 (SD 51.76) minutes for rIPOM (P = .57). Operative time for rTAPP was significantly longer, with an average console time of 90.26 min (SD 31.17) versus 70.88 min (SD 32.88) for rIPOM (P = .018), (Figure 4). Controlling for perioperative factors such as age, BMI, and sex showed no significant differences between the 2 groups (Table 1). In terms of postoperative outcomes, recorded postoperative complications were urinary retention and readmission within 30 days for fever of unknown source, hematoma, seroma, and urinary retention. The rTAPP group had 1 patient with a postoperative hematoma and another readmission which was not related to a post operative complication compared to the rIPOM group in which 3 patients had postoperative fever, hematoma or seroma formation, or urinary retention.
Figure 4.
Graph above shows no statistical difference between operative time between rTAPP and rIPOM, however a statistical difference is shown between rTAPP and rIPOM in terms of console time.
DISCUSSION
The use of rTAPP in the repair of ventral hernias is evolving. We describe our early experience in an urban teaching hospital. Increased experience with the robotic platform in ventral hernia repair is not likely to lead to major intraoperative complications or to conversions to open. Concerns about rTAPP include increased operative time; however, in our study, the time difference between the 2 procedures was not significant for total operative time. There was a significant increase in console time for rTAPP over rIPOM, which we ascribe to the time required for dissection of the peritoneal flaps before placement of the mesh. We suspect that, with increasing experience with rTAPP, the console time will become comparable with that of rIPOM.
Although the overall complication rate was minimal, it did not differ significantly at the 30-day postoperative follow-up, which was consistent with a prospective study performed by Sarli et al.6 However, in another study, Prasad et al5 found that complication rates were significantly different, favoring rTAPP over rIPOM. Additional possible complications not encountered in our cohort included chronic pain, infection, and fistula formation. Although the mechanisms for these complications are yet to be understood, animal models suggest that areas of injured peritoneum are associated with more adhesions to mesh.12 This finding further supports that covering the mesh with peritoneum is physiologically favorable.
We have noted several pitfalls during our experience. Sometimes we are left with small defects in the peritoneum that can be closed with absorbable sutures. Alternatively, these findings may facilitate future studies of reduction of inflammatory reaction with engineered mesh types and coating to reduce complications in rIPOM, although current animal studies show only reduction, not elimination, of adhesions.13,14 This possibility translates to potential cost efficacy of rTAPP, as rIPOM repair requires use of specifically engineered mesh products to reduce adhesions versus polypropylene mesh for rTAPP.
In this early series, limitations include factors that could not be standardized in a retrospective study. One of these limitations was that rIPOM and rTAPP were used for smaller abdominal wall defects. Oviedo et al15 looked at endoscopic component separation using the robotic platform for rTAPP and rIPOM in repairing larger hernia defects. The results of their study, showed no increase in operative time between the 2 groups. However, there was a difference in console time, as found in our study. Hernia defects ranged from 3 to 12 cm. Another limitation could be seen in surgeon preference and experience with the technique. Future prospective studies comparing rTAPP and rIPOM are warranted to address the limitations and examination of associated costs, controls for hernia size, and patient-centered outcomes, such as pain and time to return to work.
CONCLUSION
In our retrospective review, rTAPP was found to be a technically feasible procedure that is a promising addition to a surgeon's armamentarium for the repair of ventral hernias. Further studies to examine learning curves will determine whether the difference in operative times between rTAPP and rIPOM will persist over time.
Contributor Information
Michael Kennedy, Department of Surgery, Downstate Medical Center, State University of New York, Brooklyn, New York, USA..
Kaylene Barrera, Department of Surgery, Downstate Medical Center, State University of New York, Brooklyn, New York, USA..
Andrew Akcelik, Downstate School of Medicine, State University of New York, Brooklyn, New York, USA..
Yohannes Constable, Downstate School of Medicine, State University of New York, Brooklyn, New York, USA..
Michael Smith, Department of Surgery, Vanderbilt University Medical Center, Nashville, Tennessee, USA..
Paul Chung, Coney Island Hospital, Brooklyn, New York, USA..
Gainosuke Sugiyama, Hofstra Northwell School of Medicine, Hempstead, New York, USA..
References:
- 1. Jacob BP, Ramshaw B. Technique: laparoscopic ventral/incisional hernia repair, in Sages Manual of Hernia Repair. New York: Springer; 2013:340. [Google Scholar]
- 2. Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias: nine years of experience with 850 consecutive hernias. Ann Surg. 2003;283:391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bingener J, Buck L, Richards M, Michalek J, Schwesinger W, Kenneth S. Long-term outcomes in laparoscopic vs open ventral hernia repair. Arch Surg. 2007;142:562–567. [DOI] [PubMed] [Google Scholar]
- 4. Farmer L, Ayoub M, Warejcka D, Southerland S, Freeman A, Solis M. Adhesion formation after intraperitoneal and extraperitoneal implantation of polypropylene mesh. Am Surg. 1998;64:144–146. [PubMed] [Google Scholar]
- 5. Prasad P, Tantia O, Patle NM, Khanna S, Sen B. Laparoscopic ventral hernia repair: a comparative study of transabdominal preperitoneal versus intraperitoneal onlay mesh repair. J Laparoendosc Adv Surg Tech. 2011;21:477–483. [DOI] [PubMed] [Google Scholar]
- 6. Sarli L, Pietra N, Choua O, Costi R, Cattaneo G. Laparoscopic hernia repair: a prospective comparison of TAPP and IPOM techniques. Surg Laparosc Endosc. 1997;7:472–476. [PubMed] [Google Scholar]
- 7. Sugiyama G, Chivukula S, Chung PJ, Alfonso A. Robot-assisted transabdominal preperitoneal ventral hernia repair. JSLS. 2015. Oct-Dec; 19(4): e2015.00092; DOI: 10.4293/JSLS.2015.00092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Martín Cartes JA, Morales JM, Suárez Grau JM. Basic concepts in laparoscopic hernia repair. In: Advances in Laparoscopy of Abdominal Wall Hernia, London, Springer, 2014:37–51. [Google Scholar]
- 9. Wennergren JE, Askenasy EP, Greenberg JA. Laparoscopic ventral hernia repair with primary closure versus no primary closure of the defect: potential benefits of the robotic technology. Int J Med Robot. 2015;11:120–125. [DOI] [PubMed] [Google Scholar]
- 10. Clapp ML, Hicks SC, Awad SS, Liang MK. Trans-cutaneous closure of central defects (TCCD) in laparoscopic ventral hernia repair (LVHR). World J Surg. 2013;37:42–51. [DOI] [PubMed] [Google Scholar]
- 11. Gonzalez A, Escobar E, Romero R. Robotic-assisted ventral hernia repair: multicenter evaluation of clinical outcomes. Surg Endosc. 2017;31:1342–1349. [DOI] [PubMed] [Google Scholar]
- 12. Winny M, Grethe L, Maegel L. Impairment of the peritoneal surface as a decisive factor for intestinal adhesions in intraperitoneal onlay mesh surgery: introducing a new rat model. Int J Med Sci. 2016;13:108–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. D'Amore L, Ceci F, Mattia S, Fabbi M, Negro P, Gossetti F. Adhesion prevention in ventral hernia repair: an experimental study comparing three lightweight porous meshes recommended for intraperitoneal use. Hernia. 2017;21:115–123. [DOI] [PubMed] [Google Scholar]
- 14. Schreinemacher MH, van Barneveld KW, Dikmans RE, Gijbels MJ, Greve JW, Bouvy ND. Coated meshes for hernia repair provide comparable intraperitoneal adhesion prevention. Surg Endosc. 2013;27:4202–4209. [DOI] [PubMed] [Google Scholar]
- 15. Oviedo R, Robertson JC, Desai AS. Robotic ventral hernia repair and endoscopic component separation: outcomes. JSLS. 2017;21(3):e2017.00055. DOI: 10.4293/JSLS.2017.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]